Psychopathology & Mental Health Exam #4
1/134
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
135 Terms
what are personality disorders?
personality refers to traits that are fairly stable over time. often expressed (and measured) in terms of interpersonal relationships (social motivation, emotional expression, views of self and others).
five factors model of personality (big 5)
OCEAN: neuroticism (expression of negative emotion), extraversion (interest in interacting with others), openness (willingness to consider other perspectives), agreeableness, conscientiousness.
personality disorders
enduring patterns of perceiving, relating to, and thinking about the environment and oneself that cause impairment/distress, presumably evident by adolescence and stable over the adult lifespan, vary from a lot of other disorders in the sense that they often don't cause personal distress or impairment, but rather cause other people distress, lso vary in the sense that other disorders are ego-dystonic.
ego-dystonic
dissonant with person's self image, personal distress, discomfort with one's symptoms
ego-syntonic
consistent with person's self image, they do not generally bother the person. ex: someone with narcissism isn't going to be upset by the fact that they think they're better than everyone else, but they might be upset by the fact that they don't have many friends (not the symptom, but the consequence)
why care about personality disorders?
significant impairment in one’s life, risk factor for other mental disorders, treatment implications.
history of personality disorders
in previous versions of the DSM, personality disorders were Axis II and separate from other disorders (Axis I). that said, they weren’t always separable, which led to diagnostic confusion. some axis I disorders are very stable and some personality disorders are treatable.
assessment and treatment of personality disorders
difficult to assess and treat, tremendous overlap among categories, not clear that they are culturally universal, little research.
classification of personality disorders
DSM-5 uses a categorical model (you either have a PD or you don’t, criteria for 9 disorders).
advantages of PD categorical classification
familiar and convenient, ease in communication, consistent with clinical diagnoses.
disadvantages of PD categorical classification
low inter-rater reliability, very high comorbidity, high overlap among symptom criteria, some not based on a theoretical model, ambiguity occurs regarding presence vs. absence of symptoms, most commonly diagnosed personality disorder is PD-NOS (not otherwise specified).
dimensional model of personality traits
not currently used, but people think it will be in the future. looks at a continuum of normal to abnormal personality. various dimensional models exist.
advantages of dimensional classification of PD
theoretical basis, retention of information, flexible (different cutoffs for different needs, but not arbitrary), resolution of a variety of classification dilemmas.
disadvantages of dimensional classification of PD
less familiar, lacks clinical application
clusters of personality disorders
cluster A: all of these share similarities with schizophrenia and can proceed the onset of psychosis.
cluster B: erratic, dramatic, emotional behavior
cluster C: anxious, fearful, avoidant
cluster A PDs
paranoid PD, schizoid PD, schizotypal PD
cluster A PD prevalence and course
.5-4.9%, gender difference (males more likely than females)
paranoid PD
distrust or suspicious of others and self-blameless. pervasive, extreme mistrust, often hostile, perceives others’ motives as malevolent.
paranoid PD criteria
4 or more of symptoms:
suspects others are exploiting, harming, or deceiving him or her
doubts the loyalty or trustworthiness of friends or associates
reluctant to confide in others
reads hidden demeaning or threatening meanings
persistently bears grudges
perceives attacks and is quick to react angrily or to counterattack
recurrently suspects sexual partner of cheating
paranoid PD associated features
usually difficult to get along with
suspicious and hostility
hyper vigilant for potential threats
excessive need for self-sufficiency
often controlling, rigid, and critical
involved in legal disputes
paranoid PD treatment
unlikely to be sought, but usually involves a trusting environment
schizoid PD
impaired social relationships, inability and lack of desire. little expression of emotion. aloof, cold. detached from social relationships. restricted range of emotions. not distressed by lack of social contact.
schizoid PD criteria
4 or more symptoms:
neither desires nor enjoys close relationships
almost always chooses solitary activities
has little interest in having sexual experiences with another person
takes pleasure in a few activities
lacks close friends or confidants
appears indifferent to others' praise or criticism
shows emotional coldness, detachment, or flattened affectivity
schizoid PD treatment
unlikely to seek treatment, long-term prognosis is not very optimistic.
schizotypal PD
discomfort with close relationships, peculiar thought patterns, odd perception and speech, peculiar behavior, socially isolated, cognitive or perceptual distortions, but not hallucinations
schizotypal PD criteria
5 or more symptoms:
ideas of reference (think that something is out to get them that isn't, but not delusions or held in firm conviction)
odd beliefs or magical thinking that influence behavior and are inconsistent with cultural norms
Unusual perceptual experiences (hearing your name being murmured, feeling presence of a dead relative, different from hallucinations)
Odd thinking and speech (idiosyncratic speech, incoherent, vague, apply concepts in unusual ways
Suspiciousness or paranoid ideation
Inappropriate or constructed affect
Behavior or appearance that is odd, eccentric, or peculiar (not washing hair, wearing mismatchy clothes)
Lack of close friends of confidants
Excessive social anxiety that does not diminish with familiarity
schizotypal PD treatment
most do not seek treatment, medication (antipsychotics, SSRIs)
therapy: supportive, psychoeducational treatment. Insight oriented therapy does not appear to be effective
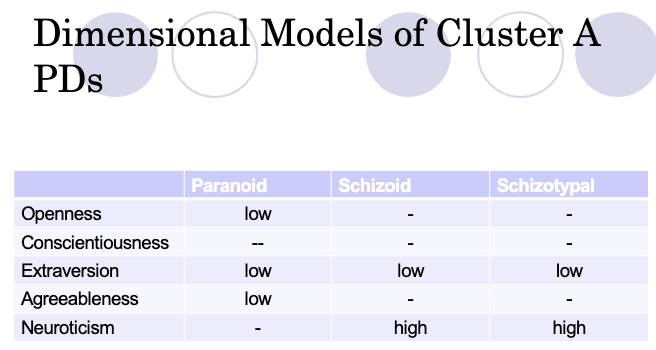
dimensional model of cluster A PDs
cluster B PDs
erratic, dramatic, emotional behavior.
narcissistic PD, antisocial PD, histrionic PD, borderline PD
narcissistic PD
pervasive pattern of grandiosity (in fantasy or behavior), need for admiration, and lack of empathy. preoccupation with own achievements.
narcissistic PD criteria
Five or more of the following:
Grandiose sense of self-importance
Preoccupied with fantasies of unlimited success, power, brilliance, beauty, or ideal love
Believes that he or she is "special" and unique
Requires excessive admiration
Sense of entitlement
Interpersonally exploitative
Lacks empathy-- unwilling to recognize or identify with the feelings and needs of others
Often envious of other or believes others are envious of them
Shows arrogant, haughty behaviors or attitudes (annoyed with incompetence)
narcissistic PD associated features
vulnerable self-esteem, care deeply about their own self-perception, relationship impairments
narcissistic PD comorbidities
bipolar disorder, substance use disorder, major depressive disorder. other cluster B PDs.
narcissistic PD prevalence and etiology
up to 6.2%, linked to poor parenting, more common in men, difficulties adjusting to onset of limitations inherent to aging
narcissistic PD treatment
talk therapy (psychotherapy).
antisocial PD
a pervasive pattern of disregard for and violation of the rights of others.
antisocial PD criteria
Repeatedly breaks the law
Deceitfulness
Impulsivity/failure to plan ahead
Irritability or aggressiveness
Reckless disregard for the safety of self or others
Consistent irresponsibility
Lack of remorse
At least 18
Evidence of conduct disorder before age 15
conduct disorder
Pattern of violating basic rights of others and/or major societal norms
Aggressive to people and animals,
Destruction of property
Deceitfulness or theft
Serious rule violation
psychopathy and ASPD
a related diagnostic category: deceitful, lacks empathy, and incapable of learning from experience
Not in the DSM-5, captures a subset of people with ASPD, strong emphasis on emotional and interpersonal traits, better predictor of recidivism
ASPD blurs criminality. How is antisocial pd different than criminality?
antisocial PD prevalence and course
3% men, 1% women, higher in samples that are economically disadvantaged. may burnout after age 40; life course persistent, person's options become narrowed, limited range of behavioral skills, ensnared by consequences of earlier behaviors
histrionic PD
Pervasive pattern of excessive emotionality and attention seeking behavior (self-centered, vain)
histrionic PD criteria
Five or more of the following:
Is uncomfortable if not the center of attention
Often inappropriately sexually seductive or provocative
Rapidly shifting and shallow expressions of emotions
Consistently uses physical appearance to draw attention
Speech is excessively impressionistic and lacking is detail
Self-dramatization, theatricality, and exaggerated emotion
Is suggestible
Considers relationships to be more intimate than they are
histrionic PD associated features
may have difficulty with emotional intimacy, act out roles, alienate others, crave novelty, stimulation and excitement
histrionic PD comorbidity
suicidality
histrionic PD prevalence
2-3%, more common in women.
borderline PD
Pervasive pattern of instability in personal relationships, self-image, and affects, and marked impulsivity.
borderline PD criteria
Five or more of the following
Frantic efforts to avoid abandonment (threatens suicide if you break up with them)
Pattern of unstable and intense personal relationships
Identity disturbance
Self-damaging impulsivity
Recurrent suicidal behavior, gestures, threats
Reccurent suicidal behavior, gestures, threats of self-mutilating behaviors
4-9% commit suicide
Self harm is not the same as a desire to die
Reasons for self-harm: make someone feel something
Affective instability
Chronic feelings of emptiness
Inappropriate, intense anger, or difficulty controlling anger
Transient, stress-related paranoid ideation or severe dissociation
borderline PD associated features
pattern of undermining themselves, may feel more secure with transient object
borderline PD etiology
childhood maltreatment (elevated of sexual assault for girls).
borderline PD prevalence and comorbidities
2%, comorbid with mood disorders (depression, bulimia, substance use disorders), gender distribution: slightly higher in women
borderline PD treatment
difficult, medicinal (antipsychotics, antidepressants, anticonvulsants, lithium), DBT has the strongest support for being effective in the treatment of BP (reorganizes BPD as a disorder of dysregulation).
cluster C PDs
anxious, fearful, or avoidant.
avoidant PD, dependent PD, obsessive-compulsive PD
avoidant PD
Pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation occurring in a range of situations
avoidant PD criteria
four or more of the following:
avoids work activities that involve significant interpersonal contact, because of fears of criticism, disapproval, or rejection
is unwilling to get involved with people unless certain of being liked
shows restraint within intimate relationships because of the fear of being shamed or ridiculed
preoccupied with social criticism or rejection
is inhibited in new interpersonal situations because of feelings of inadequacy
views self as socially inept, personally unappealing, or inferior to others
is unusually reluctant to take personal risks or to engage in any new activities because they may prove embarrassing
avoidant PD associated features
shy, timid, lonely, hyper vigilant, often target of ridicule, low self-esteem and hypersensitivity to rejection, may fantasize about idealized relationships,
avoidant PD prevalence and course
1.2%-4%, equally common in men and women, related to generalized social phobia, same condition, more severe? often starts in infancy or childhood, some evidence for remission over life
dependent PD
A pervasive and excessive need to be taken care of that leads to submissive and often clinging behavior and fears of separation
dependent PD criteria
Five or more of the following:
Needs an excessive amount of advice and reassurance from others to make everyday decisions
Needs others to assume responsibility for most major areas of their life
has difficulty expressing disagreement with others
has difficulty initiating projects
goes to excessive lengths to obtain nurturance and support from others
feels uncomfortable or helpless when alone because of exaggerated fear of being unable to care for themself
urgently seeks another relationship
is unrealistically preoccupied with fears of being left to take care of themself
dependent PD associated features
pessimism and self-doubt, may avoid positions of responsibility
dependent PD prevalence and etiology
.3-2%, equal gender distribution, may be linked to neglect and disruptions in attachment patterns.
obsessive-compulsive PD
preoccupation with orderliness, perfectionism, and mental and interpersonal control.
obsessive-compulsive PD criteria
four or more of the following:
is preoccupied with details and organization to the extent that the major point of the activity is lost
shows perfectionism that interferes with task completion
is excessively devoted to work and productivity to the exclusion of leisure activities and friendships
is over conscientious, scrupulous, and inflexible about values
is unable to discard worn out or worthless objects
is reluctant to delegate tasks or to work with others unless they submit to exactly his way of doing things
adopts a miserly spending style toward both self and others
shows rigidity and stubbornness
obsessive-compulsive PD
may be preoccupied with logic, difficulty prioritizing tasks, prone to be upset if they cant control a situation, relationships may have formal quality
obsessive-compulsive PD comorbidities
anxiety disorders
obsessive-compulsive PD prevalence
2-8%
Autistic disorder (classic autism) central symptoms
impaired social interaction, impaired communication, restrictive and repetitive behaviors, interests or actions.
Autistic disorder (classic autism) and social interaction
marked impairment in nonverbal behaviors
absence of developmentally appropriate peer relations
lack of spontaneous seeking of enjoyment, interests activities
lack of social or emotional reciprocity
Autistic disorder (classic autism) and impaired communication
delay or total lack of spoken language
impairment in conversation
stereotyped or repetitive language
lack of make-believe or social imitative play
Autistic disorder (classic autism) and restrictive and repetitive behaviors, interests, or actions
preoccupations with patterns of interest
inflexible adherence to routine
stereotyped or repetitive motor mannerisms
preoccupation with parts of objects (ex. wheels of a toy car)
Autistic disorder (classic autism) associated features
reduced eye contact — in study where they asked kids with ASD to look at fans and faces, they better-encoded fans
self-injury: one of the most dangerous difficulties of autism, should not be misinterpreted as suicidal behavior
savant performance: an exceptional ability in a highly specialized area of functioning. no adequate theory for savant performance. note: not common —> 70% of kids with autism have intellectual disabilities according to DSM-5 (IQ lower than 70)
DSM-IV criteria for Autistic disorder
6+ symptoms: impairment in social interaction (at least 2), impairment in communication (at least 1), restricted and repetitive behaviors, interests, and activities (at least 1).
delays or abnormal functioning in one before age 3: social interaction, language used in social communication, symbolic/imaginative play.
autistic disorder (classic autism) assessment
autism diagnostic observation schedule (DOS). standardized behavioral observation and coding
autistic disorder (classic autism) DMS-4 course/prognosis
early signs are subtle. some symptoms have early onset in school-aged kids, developmental gains common.
prognosis is generally poor for classic autism, 1/3 achieve partial independence as adults.
autistic disorder (classic autism) prevalence
large increases in diagnoses (criteria broadened). 3-4 more common among boys than girls, occurs in all demographics
autistic disorder (classic autism) etiology
initially people thought that parents of kids with autism were smarter than average (what really was happening was that parents who were more aware of signs initially were seeking treatment, and happened to be more educated) —> not related to education levels
vaccines don't cause autism!
is asperger’s disorder in the DSM-5?
NO
asperger’s disorder central symptoms
impaired social interaction, restrictive, repetitive, behaviors, interests, or activities.
DSM-4 criteria for asperger’s
no significant delays in language, cognitive development, self-help skills, adaptive behaviors (other than social interaction), curiosity about environment.
DSM-5 ASD central symptoms
impairment in social interaction, restricted and repetitive behaviors, interests, or actions
ASD and impaired social interaction
marked impairment in nonverbal behaviors, absence of developmentally appropriate peer relations, lack of social or emotional reciprocity.
ASD and restrictive and repetitive interests, behaviors, and actions
highly restricted fixated interests, inflexible adherence to routine, stereotyped or repetitive motor mannerisms, hyper or hyporeactivity to sensory input.
additional criteria for ASD
symptoms must be present in early developmental period, symptoms cause impairment.
asperger’s and ASD specifiers
with or without accompanying intellectual impairment, With or without accompanying language impairment, associated with known medical or genetic condition or environmental factor
asperger’s and ASD risk factors
advanced parental age (older father especially), low birth weight, exposure to certain meds in utero. 37-90% heritability estimates
asperger’s and ASD treatment
medications not effective for core symptoms. Interventions focus on enhancing daily living, communication, and social skills, and reducing undesirable behaviors. applied behavior analysis
ASD prevalence
1% of the population, increased diagnoses, 4x more common in boys, some concern about girls being undiagnosed.
applied behavior analysis
Intensive behavior modification using operant conditioning techniques, therapists focus on treating the specific symptoms of autism. 1st goal is to identify very specific target behaviors, 2nd goal is to gain control over these behaviors using reinforcement and punishment
developmental approach to childhood psychopathology
definitions of “normal” depend on age. classification of many childhood disorders rests on our knowledge of normal childhood behavior.
externalizing disorders
children who have problems in conforming to expected norms. kids with externalizing disorders are more likely to receive treatment.
key features of externalizing disorders
norms violated at a younger age than is typical, importance of age of onset. rule violations, negativity, impulsivity, hyperactivity, attention deficits
early childhood irritability
clinically significant levels, role of dysregulated tantrums, moderately stable, has clinical and predictive validity.
callous behaviors
reliably assessed, coherent developmental patterns, predictive utility
types of conduct problems

ADHD
attention deficit hyperactivity disorder. persistent pattern of inattention and/or hyperactivity.
inattention: careless mistakes, easily distracted, forgetful, difficulty organizing tasks.
hyperactivity and impulsivity: fidgets, unable to stay in seat, talks excessively, interrupts other.
DSM-5 criteria: for at least 6 months, need greater than or equal to 6 symptoms of inattention or hyperactivity and impulsivity. several symptoms must be present before the age of 12 in at least two settings. must cause impairment.
social problems in kids with ADHD
impairments in relationships with peers, teachers, and parents.
ODD
oppositional defiance disorder. a pattern of angry/irritable mood, argumentative/defiant behavior or vindictiveness. need greater than or equal to 5 symptoms over 6+ months (with at least one person who isn’t a sibling). associated with distress for self or others OR causes significant impairment. cannot occur exclusively during psychotic, substance use, or mood disorder.
conduct disorder
a repetitive pattern of violating basic rights of others and/or major societal norms of: aggression to people and animals, destruction of property, deceitfulness or theft, serious rule violation. over 12 months need greater than or equal to 3 symptoms across 4 categories. must cause impairment. for those over 18 yrs of age, criteria for ASPD are not met.
prevalence and course of externalizing disorders
19% lifetime prevalence rate for adolescents. boys have 2-10x higher rates, prevalence declines with age.
ADHD epidemiology
most diagnosed ages 7-9. more common among boys than girls. lifetime prevalence: 3-10% of American children, 1-5% European children.