Community Pharmacy - Pharmacist in practice
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
What is the framework that covers the different services a community pharmacy can deliver?
Community pharmacy contractual framework - CPCF
What is the service type that pharmacies must provide to meet their pharmacy contractual framework?
Essential services
What is the service type that pharmacies can provide if specified training requirements have been met?
Advanced services
What are the 3 phases in NMS?
Recruitment, intervention and follow up
What was the previous service that has now been incorporated into pharmacy first, relating to consultations?
Community pharmacist consultation service
What are the 3 parts of pharmacy first?
Clinical pathways consultations, urgent repeat medicine supply, minor illnesses
What are the 7 conditions included in the clinical pathways part of pharmacy first currently?
Sinusitis, sore throat, acute otitis media, infected insect bites, impetigo, shingles, uncomplicated UTI in women
How many PGDs and protocols are in place with pharmacy first’s clinical pathways?
23 PGDs, 1 protocol
What part of the clinical pathways consultation cannot be provided from distance-selling pharmacist?
Acute otitis media
What is the legal framework which allows certain healthcare professionals to sell, supply and/administer POM to groups of patients that fit specified criteria without the need for a prescription?
PGD - Patient group directions
What are examples of PGDs?
Vaccinations, emergency hormonal contraception, treating STDs, emergency treatment by paramedics
What are examples of healthcare professionals that can supply POMs under PGDs?
Chiropodists and podiatrists, nurses and midwives, orthoptists and prosthetists, physiotherapists, dental hygienists and therapists, occupational therapists, paramedics, radiographers, dieticians, optometrists, pharmacists, speech and language therapists
What must be declared for individual practitioners using PGDs?
Must be named and ensure they are fully competent and trained
What information must PGDs include?
name of authority to which it applies
Date the PGD comes into force, date it expires
Description of medicines covered
Clinical conditions covered
When to seek further advice and arrangements for referral
Exclusion criteria
Appropriate dosage and max total dosage, quantity, form, strength, route and frequency of admin, minimu/maximum period over which it should be administered
Relevant warnings, including potential adverse reactions
Details of any follow-up action
Statement of records to be kept
Who should produce and sign a PGD?
Senior doctor/dentist, senior pharmacist and representative of authorising authority
What do black triangle drugs mean?
Drugs marked as subject to more frequent monitoring
What property must medicines have to be placed on a PGD?
Must have a product license but use itself can be off-label
What medicines and products are excluded from use on a PGD?
Appliances, dressings, medical devices, radiopharmaceuticals, abortifacients, unlicensed medicines
What medicines may be allowed on a PGD after special consideration?
Schedule 2 drugs e.g., morphine and diamorphine if not for treating addiction
Midazolam
Schedule 4 part 1 medicine that isn’t in parenteral form for treating addiction
Schedule 5 controlled drugs
Antimicrobials - providing regular review occurs and local microbiologist is contacted
What must be given for medicines supplied under pGD?
Must be in original packaging to ensure patient eceives a PIL
Where will most pharmacies make you make an entry for auditing purposes after supply for a PGD?
Patient medical record - PMR
What does the minor ailments scheme do?
Pharmacists can claim for payment for giving advice or treatment OTC for certain conditions
What information does the referral from the minor ailments service contain?
Basic information about the patient - pharmacist must interview the pt and explore the conditon further
What is key to rule out when undertaking the minor illness consultation?
Red flag symptoms!
What resource should pharmacists check to ensure a correct diagnosis and treatment is made for minor ailments?
NICE CKS
What is NOT reimbursed in the minor ailments service?
Medication sold OTC - sold at pharmacy’s retail price
What statement should be given to the patient at the end of a minor ailments consultation?
Safety net - if symptoms do not improve, come back or seek advice from GP
How can minor ailments referrals/other pharmacy first referrals be accessed online?
Via PharmOutcomes
What is the website to report adverse drug reactions to?
Yellow Card Scheme
What is an emergency supply?
Pharmacist supplies medication when there is an urgent need and a charge can be taken from the pt to cover the cost of the medication
How does the urgent supply service compare to a normal emergency supply?
External healthcare provider refers the pt to the pharmacy for an urgent request, charging the pt usual Levy charge/exempt if pt is usually exempt
Where is the token sent to for reimbursement of the pharmacy first urgent supply service?
NHSBSA
What type of service is the discharge medicines service?
Essential - all pharmacies must provide it!
What is the purpose of the discharge medicines service?
Improve patients adherence with medicines and reduce the risk of harm if pt uses medicines inappropriately
What is one key source of error in collating an accurate medication history?
When patients transferred between care
What will pharmacies receive after a patient has been discharged?
Discharge summary detailing medicines the patient is now on and changes that have been made
What role do hospital pharmacists have in DMS?
Initial referral into the service
What role do general practice pharmacists have in DMS?
Have an in depth discussion with the pt in the form of a structured medication review
What are the 3 steps in DMS?
Community pharmacy receives the referral, community receives the first prescription following discharge, community pharmacy checks patients understanding
What stages of DMS must a pharmacist be involved?
Stage 2 and 3
What is the system allowing prescribers to send NHS prescriptions directly to a pharmacy electronically for dispensing?
Electronic prescription service
What is the name of the division of NHSBSA where prescriptions are submitted for payment once the pt has collected their medication?
prescription pricing division
What is the NHS spine?
The central system that prescribers send prescriptions on where pharmacies can download them from
What legal requirements do EPS prescriptions not show?
Prescribers signature as sending it via the spine shows it has been confirmed
What is the name of the electronic dispensing token form that is used to submit payment?
FP10DT
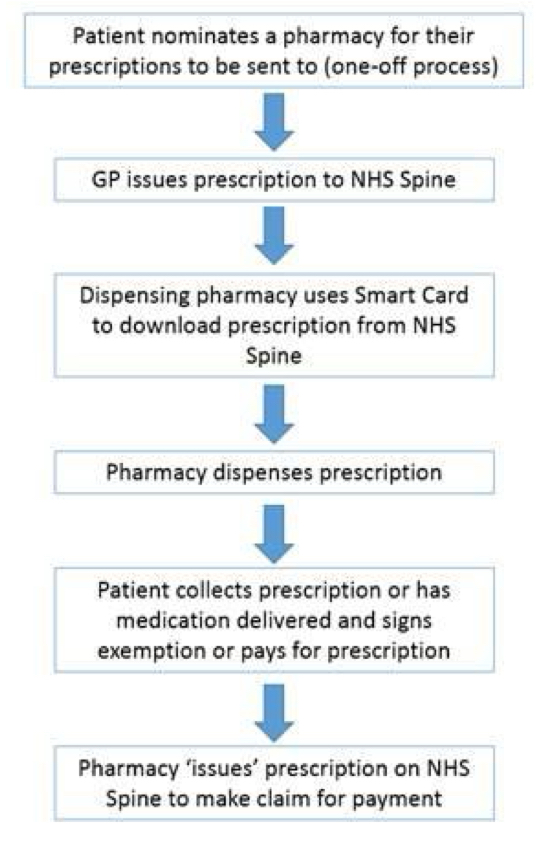
What is a diagram showing the key stages in the EPS process?
What is the name of the process where a patient chooses which pharmacy they want their electronic prescriptions to be sent to?
Nomination
How can patients nominate a pharmacy?
Contacts GP or pharmacy to ask them to nominate their EPS through the NHS spine
What must be given for a patient to be nominated to a pharmacy?
Patients consent!
What safeguards can be put in place to prevent abuse of the nomination system?
Allow pts to request paper FP10 prescriptions to take to a different pharmacy to pharmacy holding EPS nomination
Regulations for EPS to prevent GPs persuading patients to choose a particular pharmacy
Regulations prevent pharmacies from incentivising patients to nominate their pharmacy
What is needed to access the NHS spine and approved systems e.g., NHS EPS Prescription tracker, national care record service?
NHS Smartcard
What is the repeating dispensing service?
A prescriber issues a batch of prescriptions - 6-12 months at a time and the dispensing of these are managed in the pharmacy
What are the expectations of repeat dispensing in the pharmacy?
Dispense repeat dispensing Rx issued by GP
Ensure each repeat supply is required
Seek to ascertain there is no reason why the pt should be referred back to the GP
What is issued alongside paper repeat dispensing prescriptions?
Repeat authorising form - legally signed prescription
What does the repeating authorising form contain?
Standard info required of an NHS Rx alongside number of issues required and dispensing interval, with RA annotation
What will the RD form contain instead of the prescribers signature?
State number of batch issue and total number of forms issued e.g., 1 out of 6
How long are RD forms legal for?
Can be 12 months from appropriate date
When should each RD form be sent to the PPD?
Every month
When should the RA form be sent to the PPD?
At the end of the month in which the final RD from the batch has been dispensed - month where batch issue was stopped by GP
What happens with electronic repeat dispensing?
NO Ra form issued - each prescription loaded to the spine and the initial issue counts as GPs authorisation
What can be issued for electronic repeat dispensing to reassure the pt they have a prescription?
Repeatable prescription authorising token
What must pharmacies do with electronic repeat dispensing forms to download the next prescription from the batch?
Issue and claim each RD form
When is it possible to issue multiple prescriptions from the RD batch?
If patient is going on holiday IF batch issues are not post-dated
What should happen if the pharmacy doesn’t have an item on an EPS form and has not been dispensed?
Return Rx to the spine and provide the token to the patient
What should happen if the pharmacy has 2 of 3 items on an EPS form and 2 have been fully dispensed, one partially dispensed?
patient will need prescription from GP, inform them about you not being able to issue the full supply, endorse the script for the quantity actually dispensed
What should happen if there is only 1 item on the Rx and has been part dispensed, but was dated 7 months prior?
Prescription will have expired and new needs requesting