6 Development and structure of corneal epithelium and stroma
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
116 Terms
What embryologic tissue is all cornea derived from?
Ectoderm
ectoderm divides into
ocular surface ectoderm and neuroectoderm
How does the back/dorsal part of the embryo become part of the ocular system?
Dorsolateral parts (neural crest cells) become migratory and go towards eye (first wave → corneal endothelium, second → stroma)
What forms first, cornea or lens+retina?
lens+retina
What is the first part of the cornea to form?
epithelium
How are the migratory cells that make the corneal endothelium from epithelium cells?
Started epithelium (part of neural crest), delaminated from neural crest, became mesenchymal and migrated under corneal epithelium, and become endothelium (a type of epithelium again)
Is endothelium an epithelial tissue?
Yes
What develops after primitive corneal endothelium is formed?
primitive stroma
When is primitive stroma formed, is there increase or decrease in thickness?
initially swells, then decreases in thickness
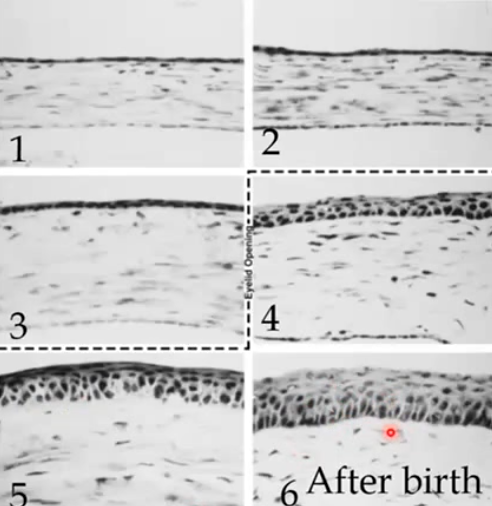
Describe corneal epithelium thickening in development
2 rounds of corneal epithelium thickening
when eye lids first start to open, mid-gestation/in utero → 4 cells thick
immediately after birth, by 6 months (4-6 cells)
What is produced with the first round of corneal epithelium thickening when eye lids first start to open?
production of BM and anchoring complexes to primitive stroma (hemidesmosomes)
Is cornea thickest at beginning, middle, or end of development?
middle - swells in utero, then stroma is reduced beginning in utero and continuing through birth
What is in the ECM of stroma that makes it thicken? What is the significance?
hyaluronan (produced by neural crest cells that will become keratocytes); binds water
What causes the corneal endothelium to undergo compaction after swelling?
hyaluronan broken down and keratocytes switch to making different ECM → lamellae
endothelial pumps begin to function → dehydration
In what direction does corneal stroma mature (water content reduced as hyaluronan ECM→ collagen fibril ECM)?
posterior (from endothelium) to anterior
What is the principle GAG/polysaccharide in primary corneal stroma?
Hyaluronic Acid / Hyaluronan
What is hyaluronan made by?
primitive corneal endothelium and keratoblasts
What provides a substrate for further ocular crest cell migration into the stroma?
large amounts of hyaluronan
What breaks down hyaluronan?
hyaluronidase, produced by primitive keratocytes
What happens during maturation of corneal endothelium?
tight junctions form to limit paracellular water transport
production of endothelial pump proteins
stroma decreases water content by moving water/ions across endothelium into aqueous humor
Does cornea become transparent in utero or after birth?
in utero
Temporal order of cornea stroma development in 4 main steps
Mesenchymal (ocular neural crest) cells migrate beneath corneal epithelium, forms primitive endothelium and keratoblasts
After primary migration, keratoblasts produce hyaluronan and thick primary stroma (and primitive endo produces DM)
Second wave of mesenchymal cells become keratoblasts
Dehydration/Compaction/organization
When does cornea reach adult size?
about 2 years of age
T or F, changing size of cornea changes ocular power
T
What decreases in cornea with age?
keratocyte number, corneal nerve fibers, endothelial cell density
What increases in cornea with age?
Epithelial BM thickness
stiffness/strength of stroma
DM
impaired wound healing
What is arcus senilis?
deposits of (cholesteryl ester-rich) lipid particles, derived from LDLs, phospholipids, and TGs
Does arcus senilis affect vision?
not typically, not in visual axis
corneal stroma is made of lamellae of __ ← __ ← __
collagen fibrils; collagen molecule (triple helix of alpha peptide chains); amino acid chain with tripeptide sequences
What are the three amino acids that make up the sequence of chains that form triple helix of collagen fibrils
glycine, proline, hydroxyproline
multiple collagen fibers make up
lamellae (large broad sheet)
Which has smaller fibril diameter, corneal stroma or Bowman’s?
Bowman’s
What has wider collagen fibrils, central or peripheral?
peripheral
Which has more interfibrillar space, central or peripheral cornea?
peripheral
What about the collagen fibrils promotes transparency?
regular size and spacing of them
How are collagen fibrils arranged in Bowman’s layer?
interweaving of thinner fibers, not lamellae
How are collagen fibrils arranged in anterior 1/3 of stroma proper?
interwoven lamellar structures
How are collagen fibrils arranged in posterior 2/3 stroma?
orthagonal arrangement of lamellae (more 90 and 45 degree angles)
What provides mechanical strength for the cornea?
arrangement of collagen fibrils, more interweaving towards Bowman’s
What causes peripheral cornea to be thicker than central?
number of lamellae (500 peripheral, 250-300 central)
Which is better in withstanding forces, anterior or posterior cornea? Why?
anterior; lamellae less organized
is keratoconus usually uni- or bilateral?
Bilateral
What is keratoconus?
bilateral, progressive thinning and ectasia of cornea → blurred vision from irregular astigmatism
Keratoconus is an example of a cornea __, where the cornea thins and bulges
cornea ectasia
T or F, LASIK can cause corneal ectasia
T, taking some cornea away affects biomechanical strength of the tissue
post-LASIK ectasia
mechanical failure from weakened structure and interlamellar slippage (fewer lamellae in area of ectasia)
T or F, all lamellae in the peripheral corneal stroma are organized orthogonal to each other
F, but MOST are (nasal/temporal and inf/superior)
What causes the cornea to bulge out more and have a steeper curvature than the sclera?
annulus of collagen around the cornea
Functions of the annulus of collagen around the cornea
promote curvature of cornea, provide mechanical strength
What are the two categories that the 13 known types of collagens in the cornea are divided into?
fibril forming type (73%) and non fibril forming (27%)
What types of collagen are classified as fibril forming?
I and V
What types of collagen are classified as non fibril forming?
VI and FACIT
FACIT
Fibril Associated Collagens with Interrupted Triple helices (XII, XIV)
Function of non fibril forming type collagen
bridge together fibrils, lamellae for structure
What type collagen is found most abundantly in fibrils?
Type I (much more than V)
What determines how large the diameter of fibrils is?
ratios of Type I and V collagen
More type V collagen means a larger or smaller fibril diameter?
smaller diameter
Which has a thinner fibril diameter size, Bowman’s or corneal stroma?
Bowman’s
Which has less type V collagen, Bowman’s or corneal stroma?
stroma
Why does more type V → smaller fibril diameter?
Type V has a kinked morphology, so it’s harder to add more collagen to the fibril
What causes the “banded” pattern of collagen fibrils
they are quarter staggered
What would removal of type 14 (FACIT) collagen result in?
larger collagen fibril diameter
What is Ehlers-Danlos syndrome caused by?
affecting genes for collagen I and V → disruptions in CT proteins, and/or genes for lysyl hydroxylase (ECM proteins and intracellular processes)
Presentations of Ehlers-Danlos syndrome
Skin hyperextensibility
Delayed wound healing
Joint hypermobility
Corneal complications (thinner, stromal folding, keratoconus)
Functions of Type VI collagen
binds corneal lamellae and other types of collagen together
What type of collagen is nonbanded and beaded?
Type VI
Keratocyte function
production of collagen fibrils and ECM, including during injury
turnover of stromal ECM by producing enzymes that break ECM down, and building it back up again
What makes collagen that make up the corneal stroma?
keratocytes
What are keratoblasts?
secrete collagen in development, before becoming mature keratocytes
What makes up the largest component of the corneal stroma’s dry weight? Second largest?
Collagen, keratocytes
Does density of keratocytes increase or decrease with age?
decrease
__ are 10% of corneal stromal volume
keratocytes
Keratocytes have a __ organization
radial (whorl like)
Are keratocytes more dense in anterior or posterior stroma?
anterior
How are fibrous collagen fibrils made by keratocytes?
translation into rough ER
Enzymes prolyl hydroxylase and lysyl hydroxylase in ER add hydroxyl groups to prolines and lysines
Glycosylation in ER (add saccharide units to collagen peptide)
Sulfide bonding between propeptide sequences → triple helix formation
→ golgi → vesicle → procollagen peptidase activity → cleaves N/C terminal peptides that don’t make it into helix → secreted from cell
Lysyl oxidase (assemble helical tropocollagen structures into collagen)
Function of procollagen peptidase
cleaves ends of procollagen that doesn’t make it into the helix
What is lysyl oxidase?
extracellular enzyme that helps assemble helical structures into collagen fibrils
What parts of collagen fibril formation happen inside the keratocytes? Outside the cell?
Inside keratocytes: individual subunits translated, hydroxylated, glycosylated, form triple helix with sulfide bonds, and are cleaved by procollagen peptidase
Outside the cell, lysyl oxidase (secreted by cell) assembles fibrils
What step of fibrous collagen fibril formation requires ascorbic acid (vitamin C)?
first step of prolyl hydroxylase and lysyl hydroxylase activity
What are fibripositors?
long cytoplasmic extensions that surround nascent fibrils and deposit them into forming lamellae
What assembles collagen and is a long cytoplasmic extension of keratocytes?
fibripositors
2 categories of collagen fibril maturation
Cross-link maturation
Glycation
What categories are within cross-link maturation?
Enzymatic: divalent cross-linking (lysyl oxidase)
Non-enzymatic: trivalent cross-linking
What is glycation?
a category of maturation where sugar residue bridges collagen fibrils together
What is the result of collagen fibril maturation over time?
increase in corneal stiffness → stronger/tougher fibrils
T or F, excessive collagen fibril glycation and cross-link maturation would result in a flexible corneal stroma
F, would cause tissue to be brittle, more prone to fracture
Describe divalent crosslinking
enzymatic maturation, lysyl oxidase links 2 tropocollagen (tripeptides) by adding a hydroxyl group on lysine to create an aldehyde (very reactive, likely to form covalent bonds with neighboring lysine)
Describe trivalent crosslinking
non-enzymatic maturation, spontaneous racemization/isomerization of functional groups linking 3 tropocollagens (tripeptides)
What amino acids are affected by trivalent crosslinking?
glycine and aspartic acid
Difference between cross-linking maturation and glycation?
cross-linking just modifies and bridges the existing peptides, while glycation uses a reducing sugar (glucose) molecule
T or F, glycation only bridges peptides within the same tropocollagen
F, cross-links all peptides! Within same tropocollagen, between neighboring ones in the same fibril, and different fibrils
T or F, glycation is typically irreversible
T
What are the products of pathological glycation?
Advanced-glycation end products (AGE)
What are Advanced-glycation end products (AGE)?
They form naturally with age (or pathologically with hyperglycemia) from glycation within collagens lipids, other proteins
What collagen molecules are more likely to be AGE products?
long lasting ones, like in the corneal stroma (and other ocular tissues)
Why is a diabetic eye more prone to corneal injury and worse at wound healing?
Excessive glycation → cross-linkage of tropocollagens → stiffness/brittleness of tissue when force is applied → prone to injury, migration of immune cells and keratocytes inhibited by stiff surroundings
How can progression of ectasia (like keratoconus) be prevented?
Use UVA-Riboflavin (UV light-activated sugar) to stimulate cross-linking of lysine in corneal collagen, increasing mechanical strength of cornea
What are the proteins associated with polysaccharides that decorate the outside of fibrils and function as spacer molecules between collagen fibrils?
proteoglycans
What are the four main protein cores of proteoglycans?
Decorin, Lumican, Keratocan, Mimecan
What are GAGs?
highly negatively charged long polysaccharide chains consisting of disaccharide subunits