Kin 315-Ch.8: Physical Growth, Maturation, & Aging
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
39 Terms
Changes to Individual Constraints are influenced by
A combination of factors:
Genetic: drive orderly and sequenced pattern of growth and aging
Extrinsic: examples would be nutrition and disease
Universality
patterns across all humans
Variability
individual differences
Developmentally Appropriate
motor tasks that are achievable by a given range of ages and abilities
Educators/therapists should make sure tasks are
Embryonic Development: Timeline
Conception to 8 weeks
Conception: male and female sex cells fuse together
Embryonic Development: Differentiation of Cells
1st stage of embryonic development
forms tissues and organs
differentiation: cells become specialized, form specific tissues and organs
by the time the embryo implants into the uterus, it is several hundred cells in size
Embryonic Development: 4 Weeks
2nd stage of embryonic development
Limbs formed
Embryonic Development: 8 Weeks
final stage of embryonic development
human form noticeable
eyes, ears, nose, mouth, fingers, toes
Fetal Development: Timeline
8 weeks to birth
further growth and cell differentiation of the fetus, leading to functional capacity
Fetal Development: Continued Growth via…
Hyperplasia
increase in cell #
Hypertrophy
increase in cell size
Cephalocaudal
one of the directions of development in fetal development
head to toe
head, facial structures —> upper body —> lower body
Proximodistal
one of the directions of development in fetal development
near to far
trunk —> proximal limb parts —> distal limb parts
Plasticity
part of fetal development
the capability to take on new function
ex: if some cells in a system are damaged, the other cells can work to perform the role of the damaged cells
cells in the CNS have a high degree of this
Fetal Nourishment
Placenta: where O2 and nutrients diffuse between fetal and maternal blood
place of CO2 and waste products exchange
Maternal health status affects fetus
if in low supply, mother and fetus compete for these resources
Low birth-weight: infants are at greater risk of disease, infection, and death in the weeks after birth than normal-weight infants
Abnormal Prenatal Development
Source can be:
Genetic: inherited, may be immediately apparent or remain undetected until well into postnatal growth
Extrinsic: drugs and chemicals in mother’s bloodstream, viruses, excessive pressure applied to mother’s abdomen
Types:
Congenital (present at birth; due to either genetic or extrinsic factors)
Non-congenital
Abnormal Prenatal Development: Genetic Causes
Dominant disorders: defective gene from one parent
Recessive disorders: defective gene from each parent
Gene mutation: could be spontaneous or from irradiation, environmental toxins, etc.
Mutation of egg or sperm cell (not necessarily inherited)
Abnormal Prenatal Development: Effects on Growth/Maturation
Variable in appearance and severity
malformation of limb, organ
deformation of body part
mental problems
visual impairment
body systems dysfunction
Many are obvious at birth, but some do not appear until later
Abnormal Fetal Development: Example of Genetic Disability
Down Syndrome (aka Trisomy 21)
chromosomal anomaly
usually an egg and sperm have 23 chromosomes; after fertilization an embryo ends up with a complete set of 46 chromosomes
sometimes an egg or sperm cell keeps both chromosome 21s, so the embryo has an extra chromosome 21
Abnormal Fetal Development: Example of Abnormal Development Due to Extrinsic Factors
Fetal alcohol syndrome
occurs when mother consumes alcohol when pregnant
Abnormal Development: External Causes
Nourishment
Physical environment
Teratogen: drug/chemical agent that causes abnormal prenatal development; can be from too much/too little of substance; delivered through nourishment system
effects depend on when the fetus was exposed (critical periods) and the amount of substance
example: too little folic acid (B vitamin)—needed for spinal development, too little could lead to spina bifida (incomplete neural development)
TLDR: external factors can be diet/medications, environment, and conditions/diseases
Abnormal Fetal Development: Harmful Environmental Factors
Placenta screens some substances (ex: large viruses) but not all harmful things
Pressure (could also include internal pressure from other fetus in utero)
Temperature: extreme internal temp (ex: when mother has high fever or hypothermia)
X Rays
Gamma Rays
Atmospheric Pressure (ex: hypoxia aka O2 deficiency)
Pollutants (environmental such as air pollution and secondhand smoke)
Other (smoke, alcohol, drugs, raw food, etc.)
Timing is important—ex) Rubella virus is most dangerous if fetus is exposed during the critical period (first four weeks) of pregnancy
Most vulnerable: tissues undergoing rapid development at time of exposure
Postnatal Development: Growth Pattern
Sigmoid (s-shaped: sigmoid is the Greek letter for S)
Postnatal Development: Timing of Spurts vs. Steady Periods
Generally universal
Varies among individuals
Differs between the sexes
usually rapid growth (height and weight) after birth (aka during infancy), steady growth during childhood, rapid growth during early adolescence, and a leveling/tapering off
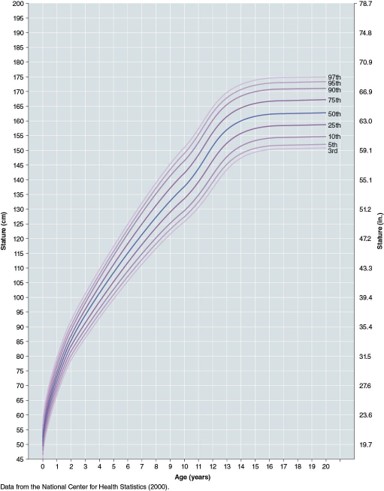
Height (General)
Sigmoid pattern
Although a normal growth curve is always sigmoid, the timing of a particular individual’s spurts and steady growth periods is likely to vary from the average
Long growth period of males contributes to absolute height differences
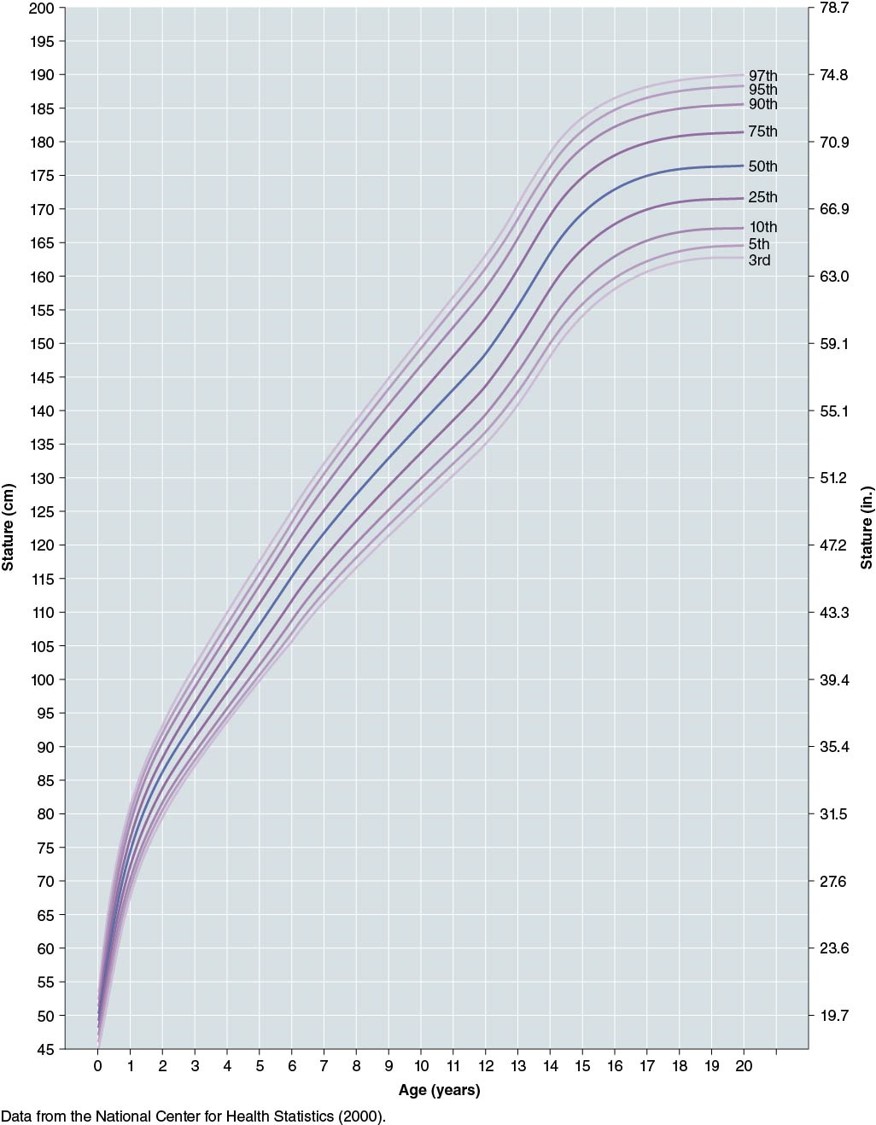
Height (Boys)
Peak Height Velocity: 13.5-14 yr
Growth:
tapers off ~17 yrs
ends ~ 18 yrs
Height Curve for boys 0-20 years old
Note the 2 steep slopes first:
~0-1 yr
~12-14 yr
This shows:
Universality (general shape of the curve)
Variability (percentiles)
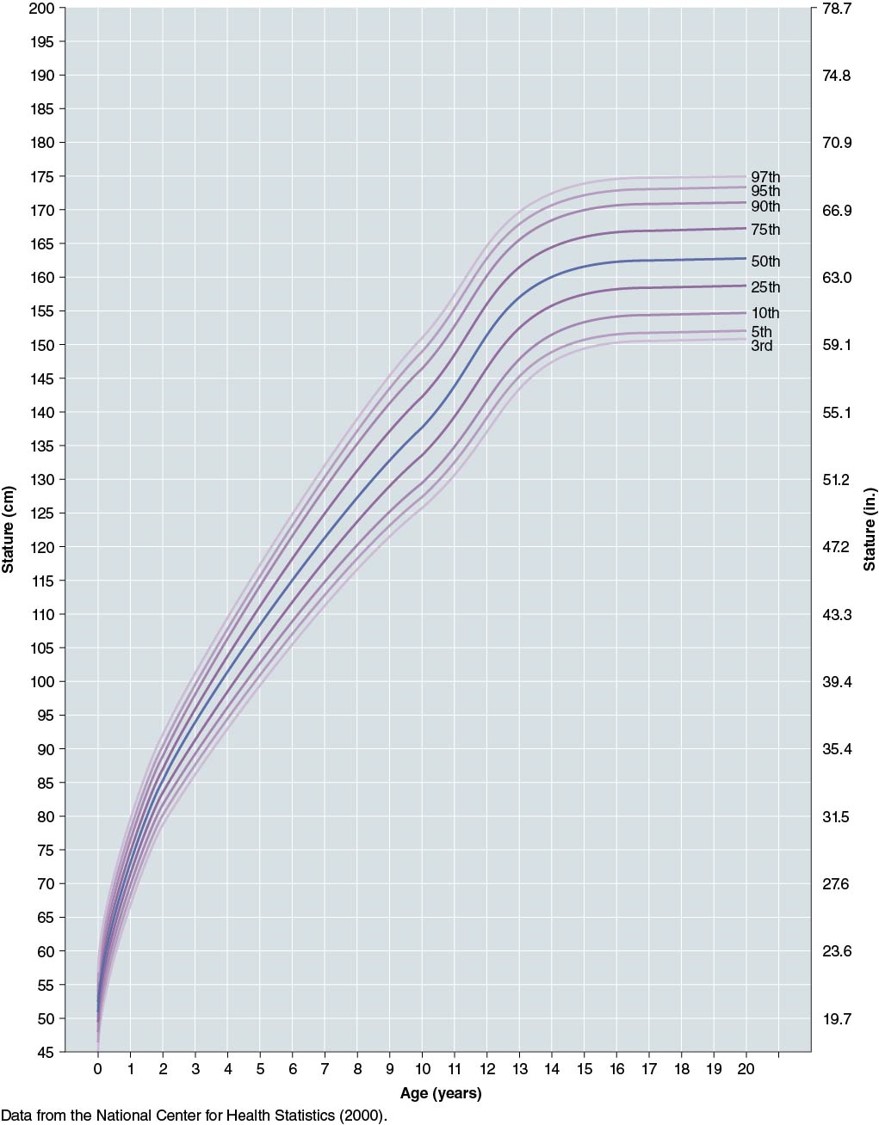
Height (Girls)
Peak Height Velocity: 11.5-12 yr
Growth:
tapers off ~14 yrs
ends ~ 16 yrs
Height Curve for girls 0-20 years old
Note the 2 steep slopes first:
~0-1 yr
~10-12 yr
This shows:
Universality (general shape of the curve)
Variability (percentiles: aka timing and steepness of segments of the curve are specific to the individual)
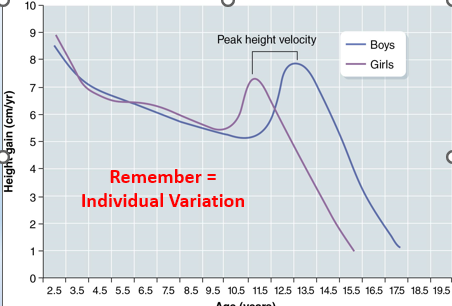
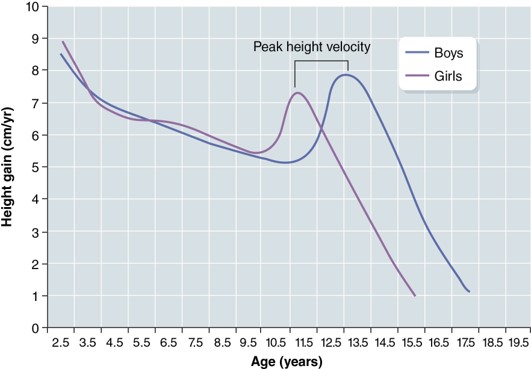
Height: Velocity Curves
After age 2 the rate of growth slows until the adolescent growth spurt. Note the ages at peak height velocity
Longer period of greater rate of growing for boys = absolute height differences
Note: males have about 2 more years of growth than females
Boys peak height velocity is somewhat faster than that of girls
9cm/yr vs. 8cm/yr
Girls begin their adolescent growth spurt when they are about 9, whereas boys begin theirs at about 11 (these are age group averages)
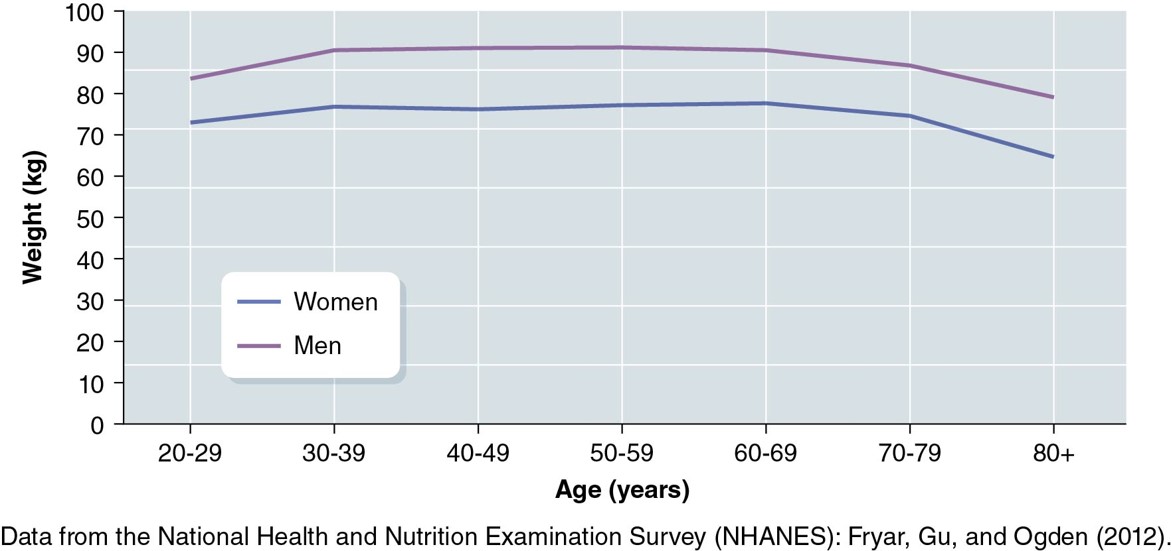
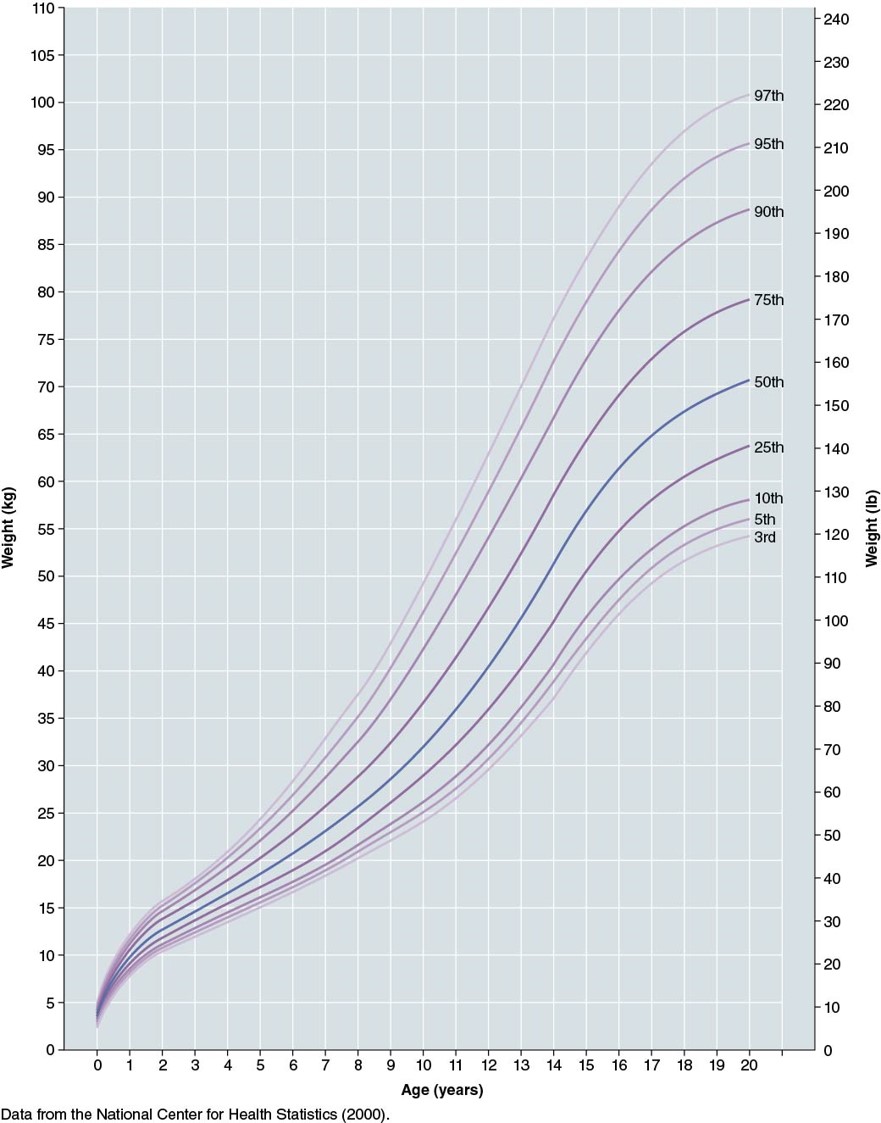
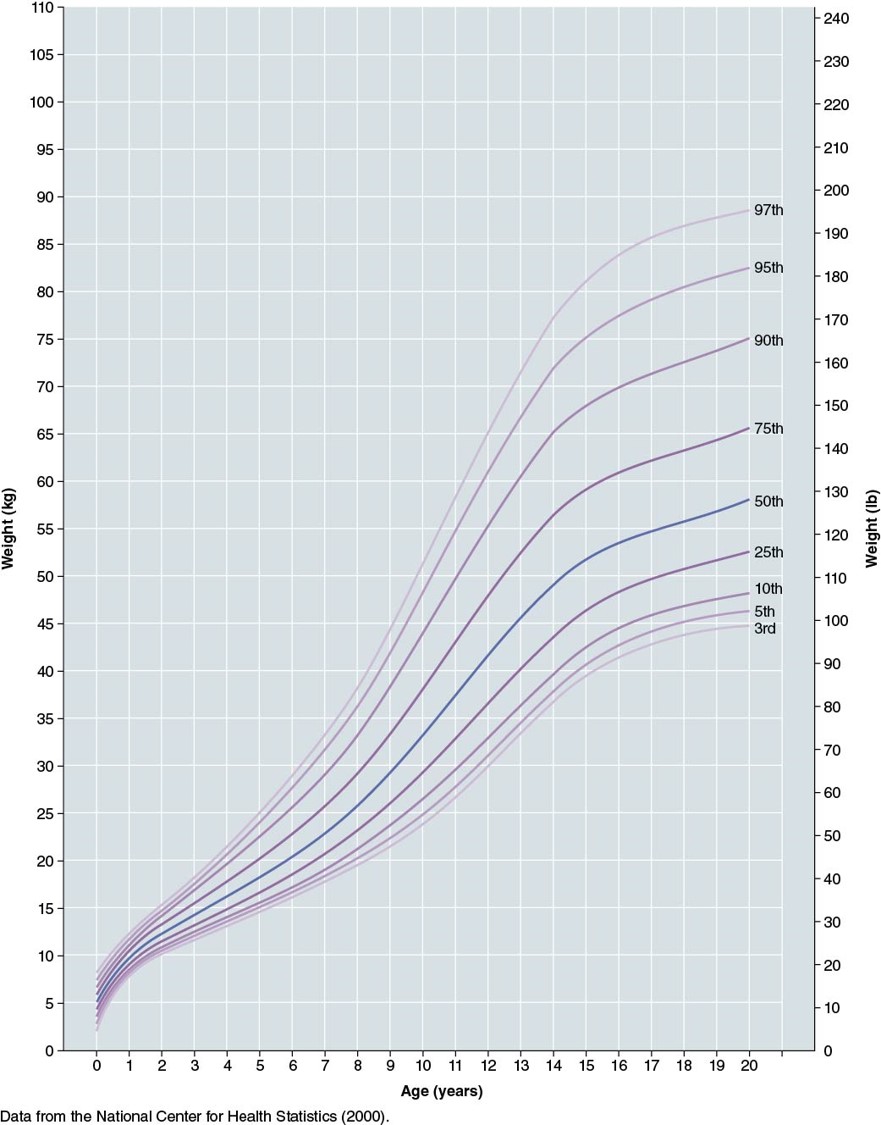
Weight
Sigmoid pattern
Susceptible to extrinsic factors (especially in early adulthood)
diet
exercise
disease
People:
grow up (height)
fill out (weight)
Peak weight velocity
follows peak height velocity; height velocity peaks occur before or at the same time as weight velocity peaks
by 2.5-5 months (boys)
by 3.5-10.5 months (girls)
Boys Weight (chart)
Girls Weight (chart)
Postnatal Growth: Extent vs. Rate
Distance curves = extent of growth
Velocity curves = rate of growth
Peaks on velocity curves show ages that growth rate changes
Postnatal Growth: Relative Growth
Body overall: sigmoid pattern
Specific parts/tissues/organs: differential growth rates
For example, the brain achieves more than 80% of its adult weight by age 4. So, even if 5-months old infants were neurologically ready to coordinate and control the walking pattern, it is unlikely they could balance their top-heavy bodies on such thin, short legs and small feet. This is a reminder that changing individual structural constraints related to body form and proportion could certainly interact with task and environment to produce different movements
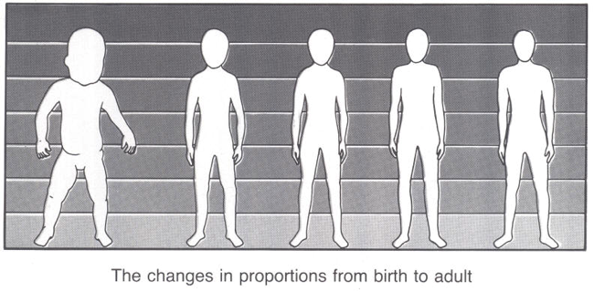
Postnatal Growth: Body Proportions
Changes from head-heavy, short-legged form at birth to adult proportions
Adolescent boys: increase shoulder breadth
Adolescent girls: increase shoulder and hip breadth
Physiological Maturation
Size and Maturation
Physiological maturation: the developmental process leading to a state of full function
increase in children/youth with age
rate varies
Can measure maturation:
Indirectly: compare anthropometric measurements
Directly: qualitative assessment of secondary sex characteristics, measure skeletal maturation
Secondary Sex Characteristics
appear as a function of maturation (based on hormone changes)
appear at younger age in early maturers
girls (as a group) mature sooner and at a faster rate than boys
Primary sex characteristics: appear at birth
How should we counsel parents of an early maturer and star athlete about the child’s future in athletics?
Maturation status is relevant as a structured constraint influencing movement.
It is tempting to infer movement performance potential from size and/or age, but maturation status is a powerful predictor of performance potential.
How concerned should we be if a young teen seems more awkward than he/she was in childhood?
Periods of motor incoordination, or “adolescence awkwardness,” may occur during the adolescent growth spurt. These are temporary and not associated with any underlying dysfunction. They may be associated with an increased risk of injury.
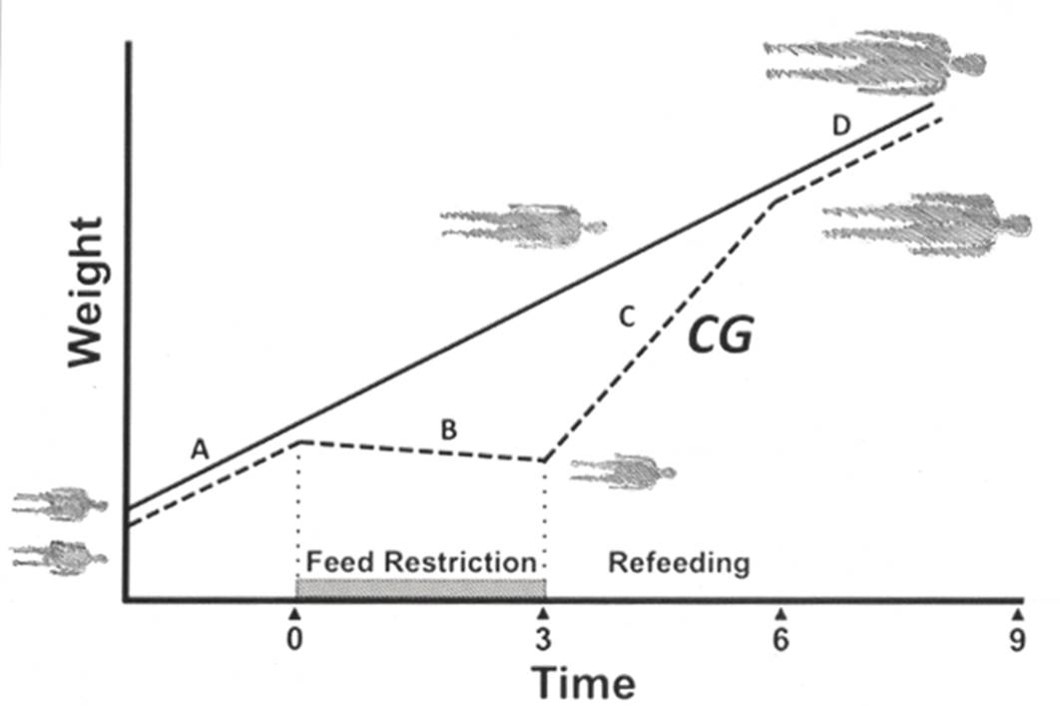
Postnatal Growth: Extrinsic Influences
especially sensitive during rapid growth periods
Genetics control the timing and rate of growth and maturation, but extrinsic factors (especially those influencing metabolism) can have a great effect.
For example, not having enough food for nourishment (severe malnutrition) can slow growth. Could also be due to severe disorder.
Catch-up growth (CG): period of rapid growth to recover some or all potential growth lost during period of negative extrinsic influence. Occurs once negative influence is removed.
Whether a child recovers some or all of the growth depends on the timing, duration, and severity of the negative environmental condition.
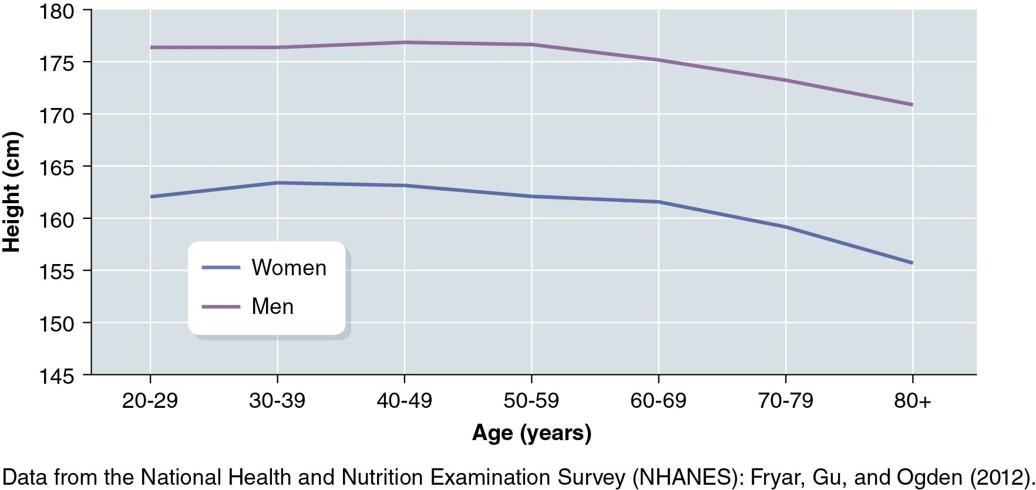
Adulthood and Aging: Height
Growth ends for humans in the late teens or early 20s
Stable in adulthood
May decrease in older age
compression of cartilage pads, mainly in the spine
osteoporosis: decreased bone density that can lead to decreased height due to compression fractures of the vertebrae (which can lead to kyphosis aka “dowager’s hump”) and increased pressure in the abdominal cavity
Adulthood and Aging: Weight
Increases starting in 20s
diet
hormones
exercise (sedentary)
decreased muscle mass
inactivity
appetite (unhealthy/lack of)
Active adults are not as likely to lose muscle mass