Transplantation Immunology
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
14 Terms
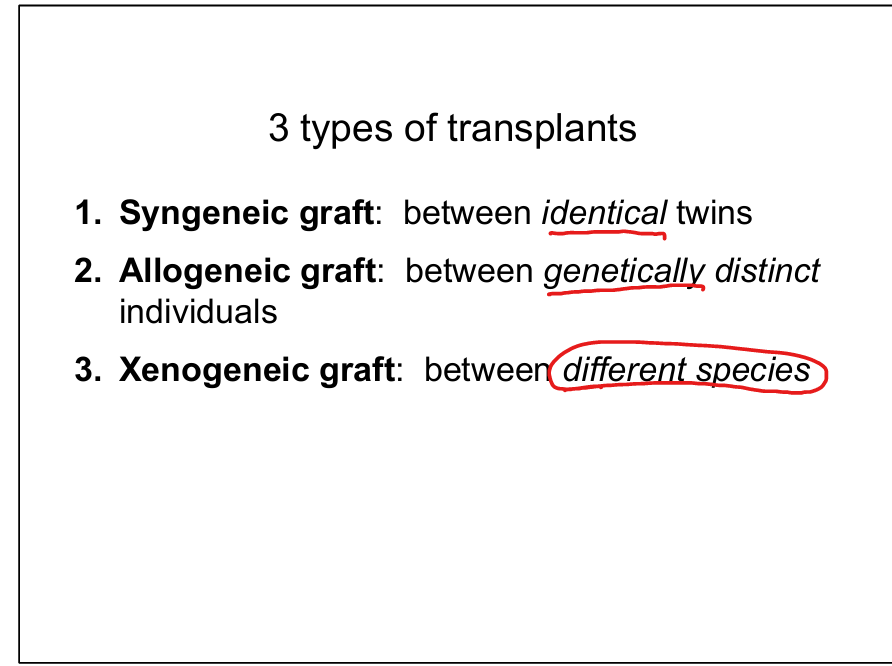
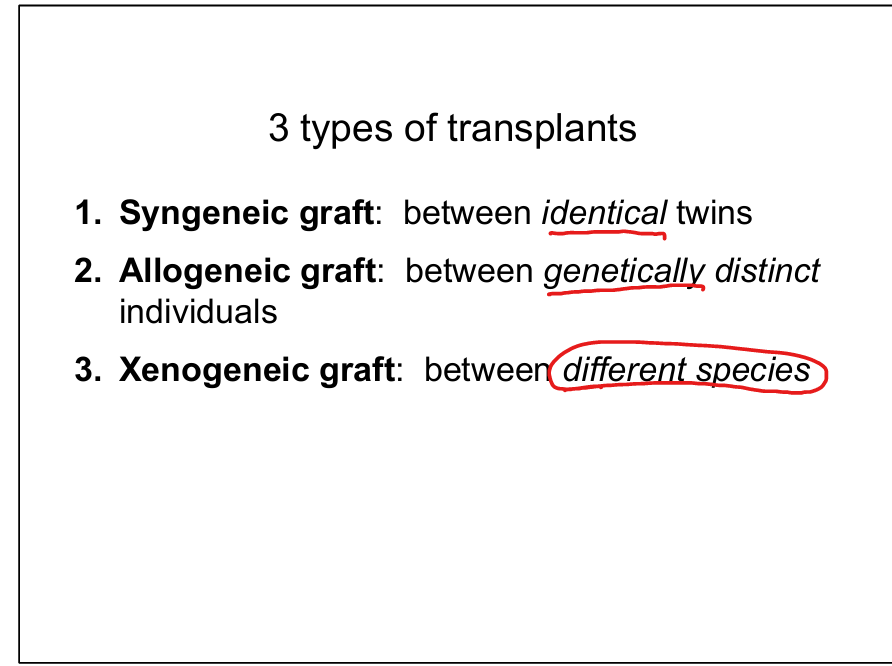
Define the three types of transplants.
Syngeneic graft: between identical twins; Allogeneic graft: between genetically distinct individuals; Xenogeneic graft: between different species.
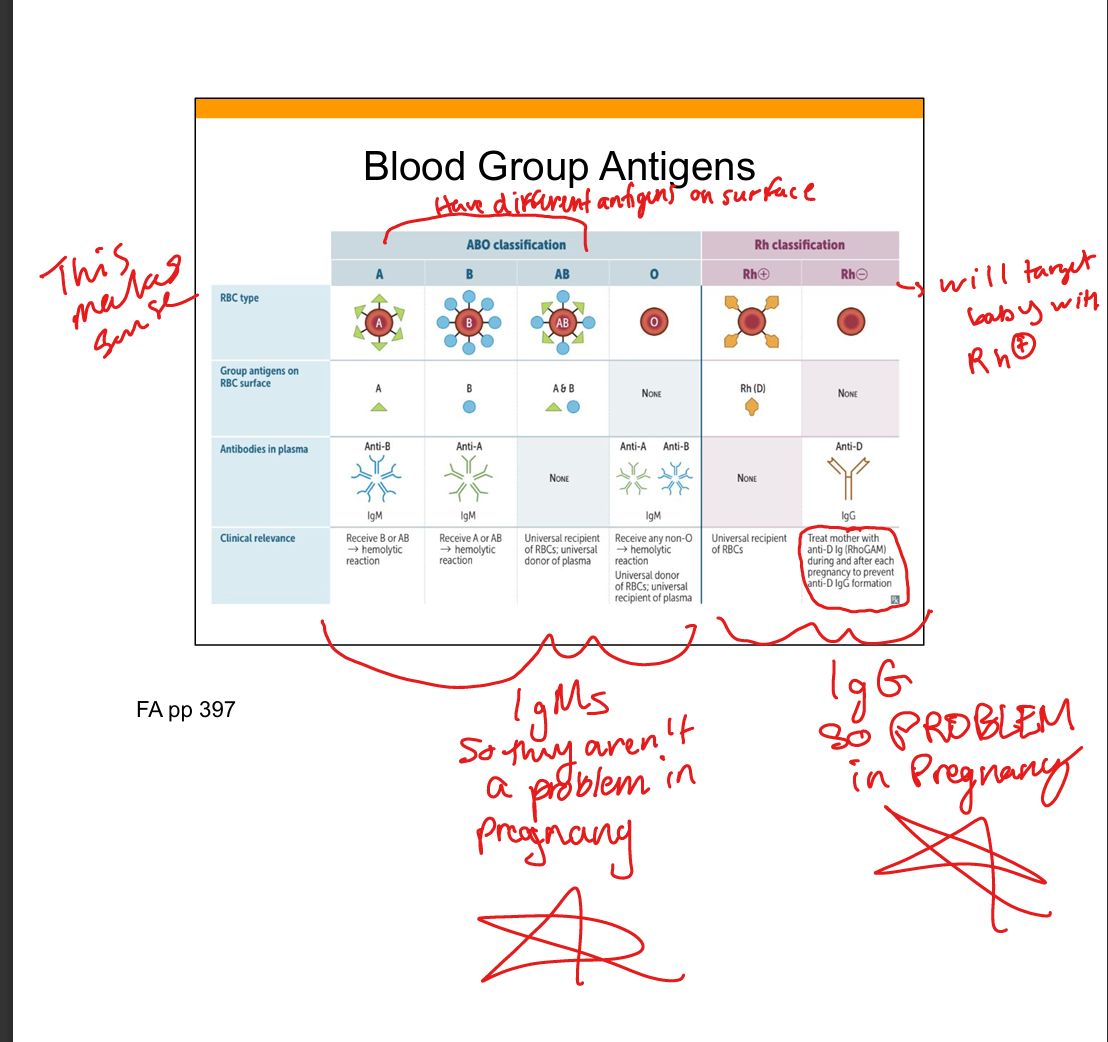
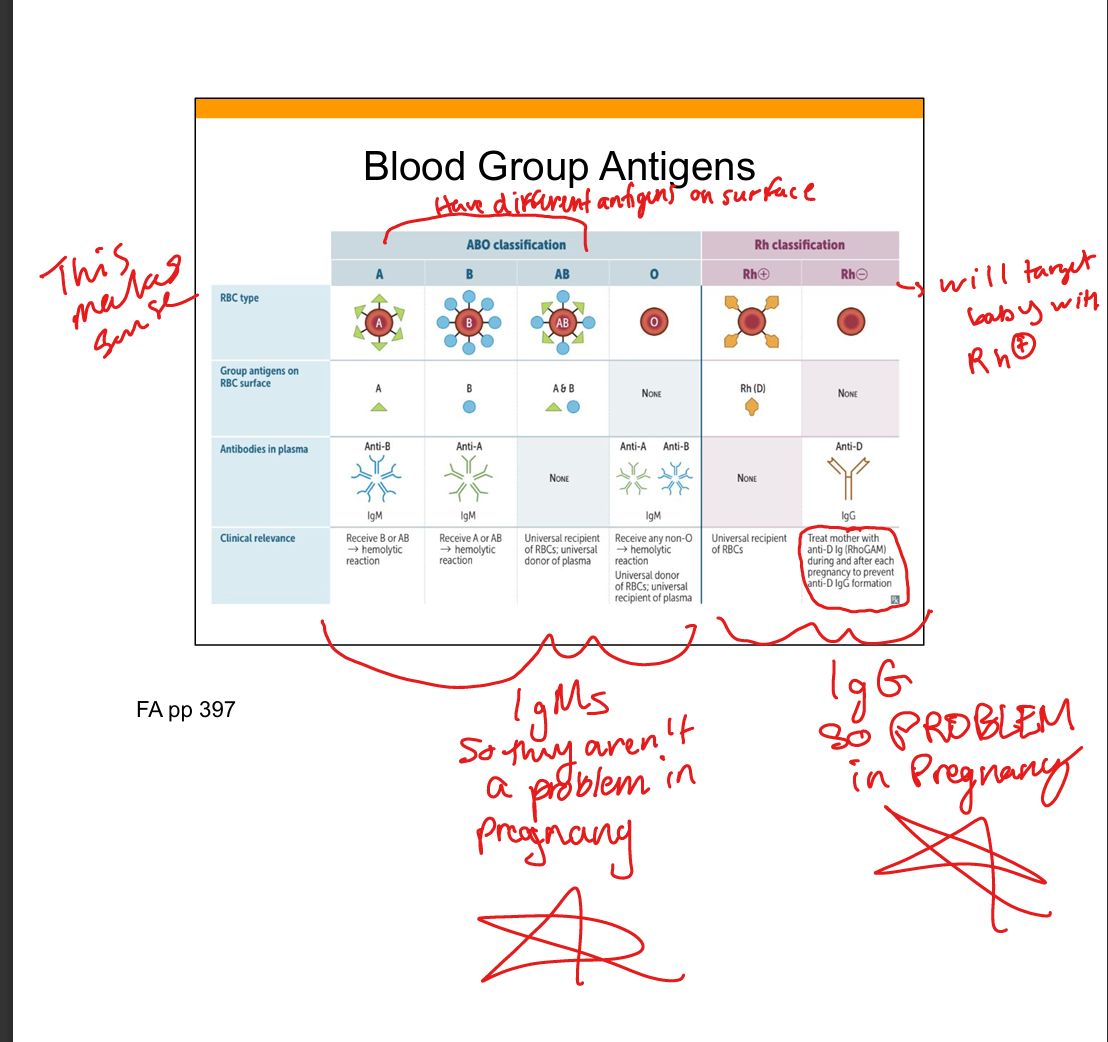
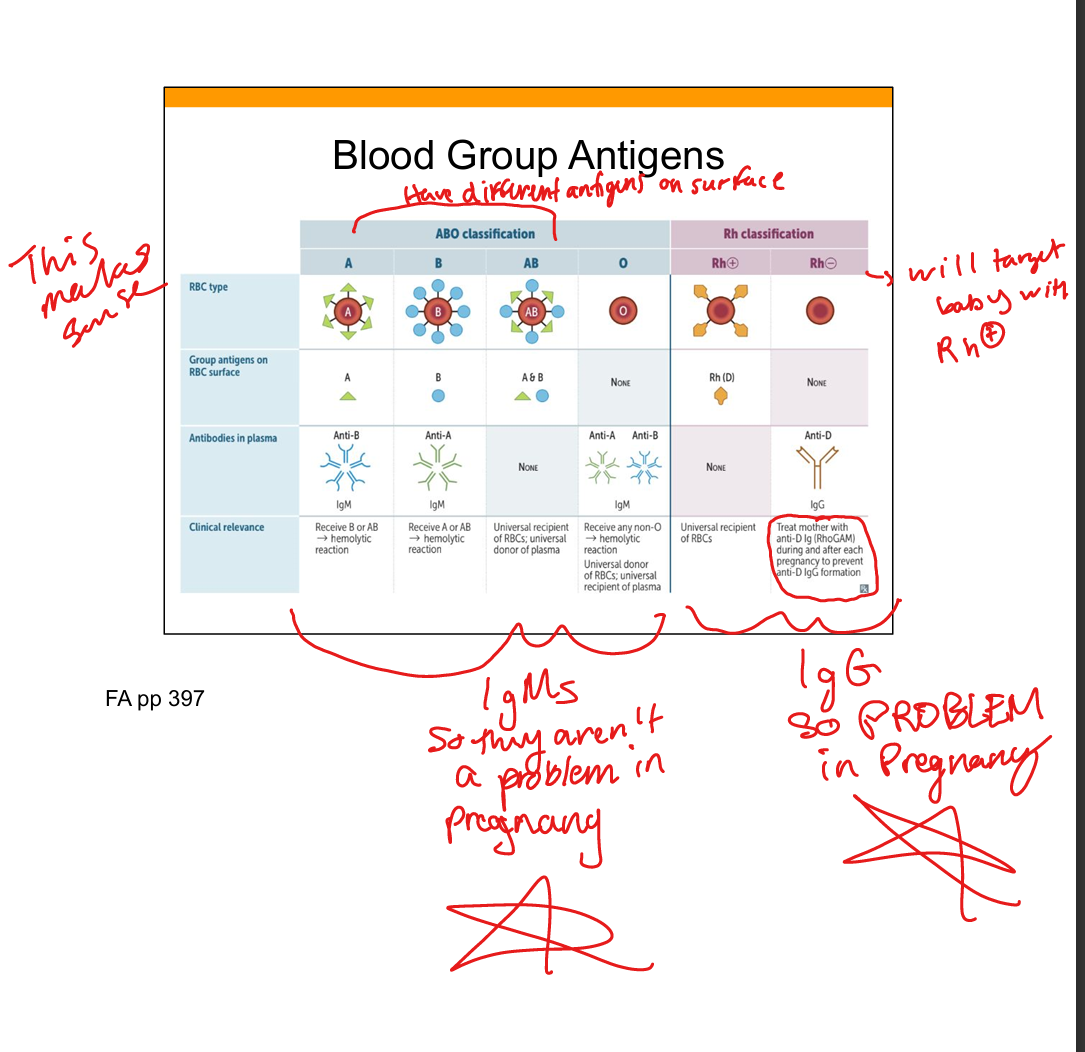
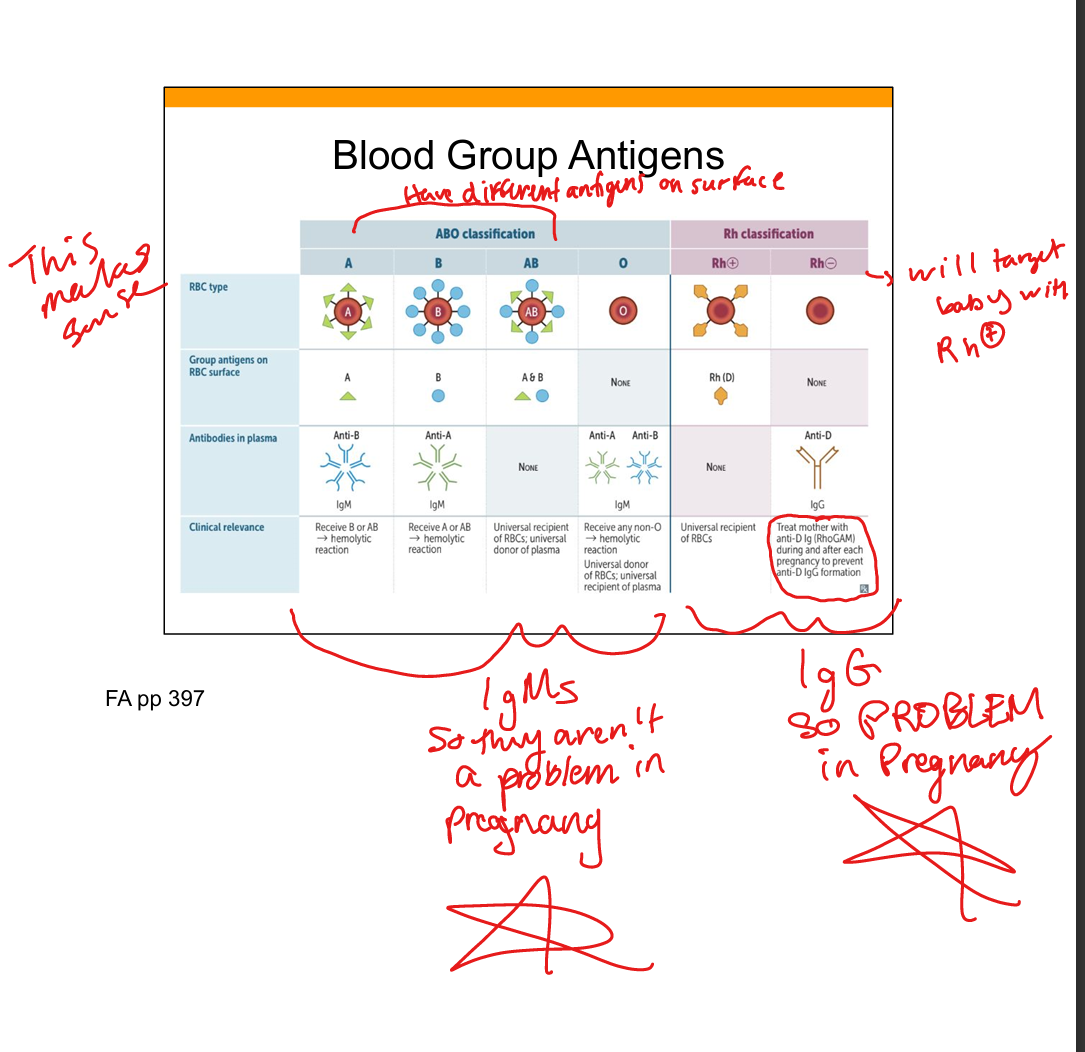
Describe the role of ABO antigens in blood transfusion.
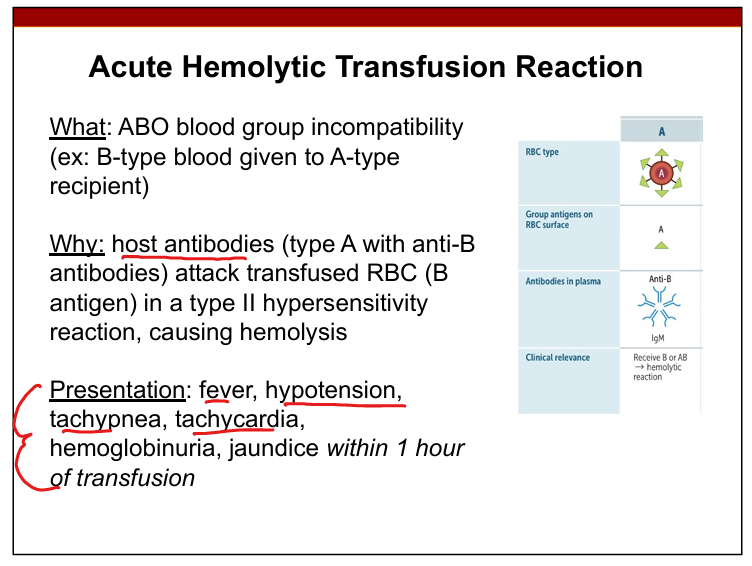
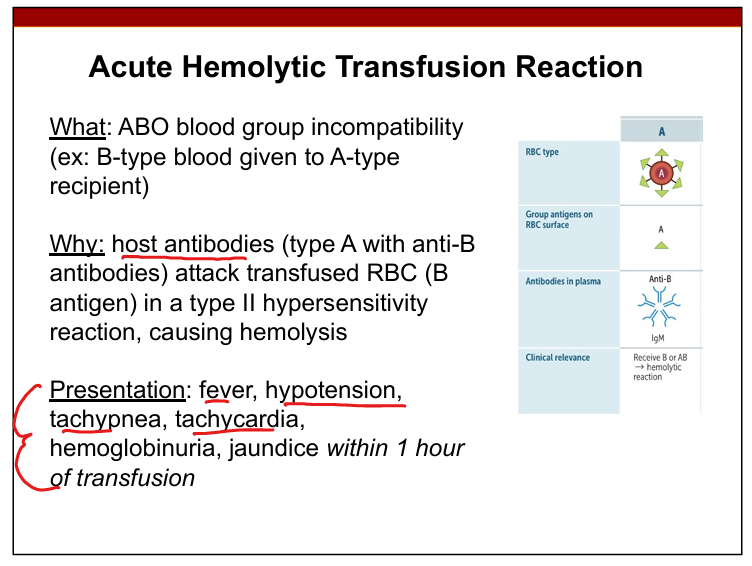
ABO antigens are carbohydrate antigens on RBCs; mismatched transfusion leads to IgM‑mediated type II hypersensitivity causing acute hemolysis.
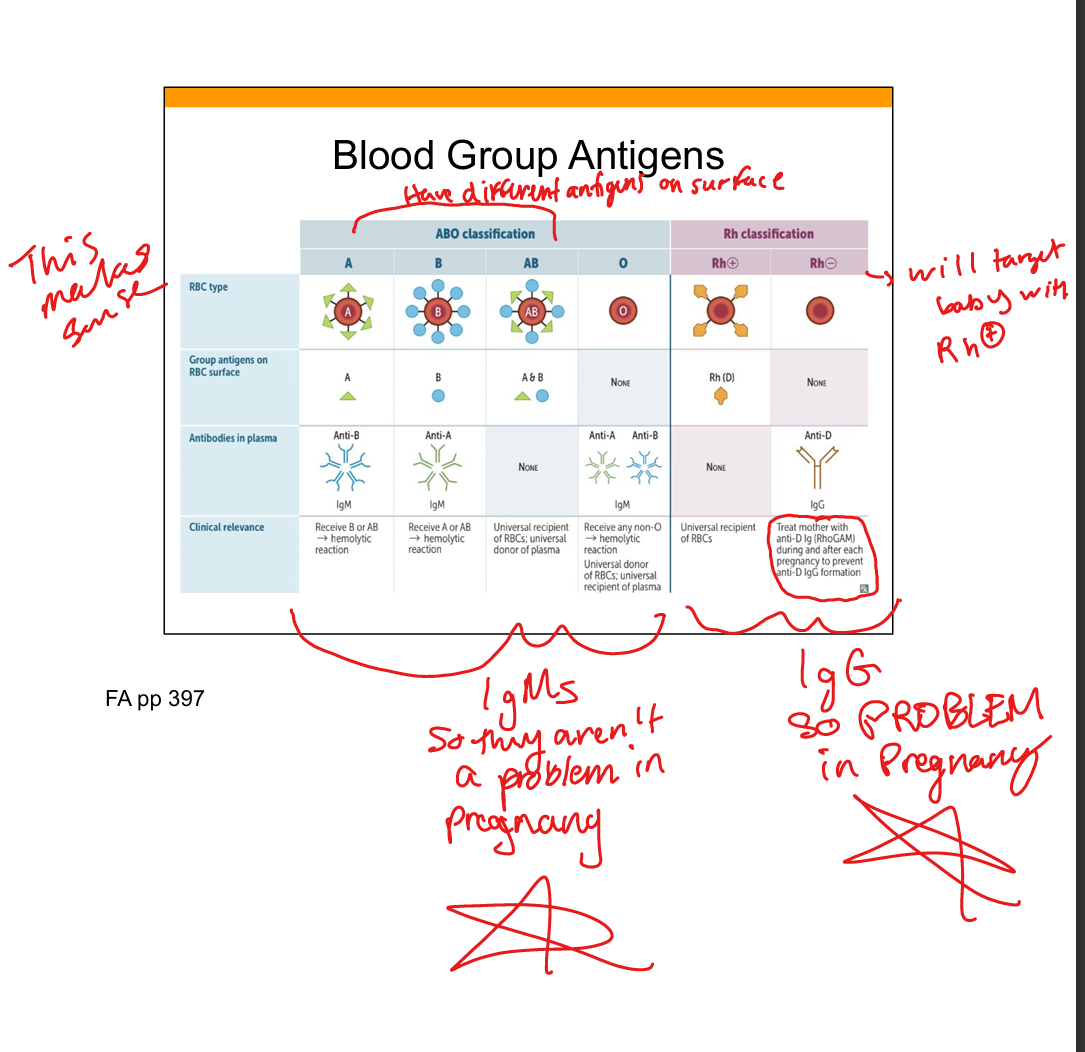
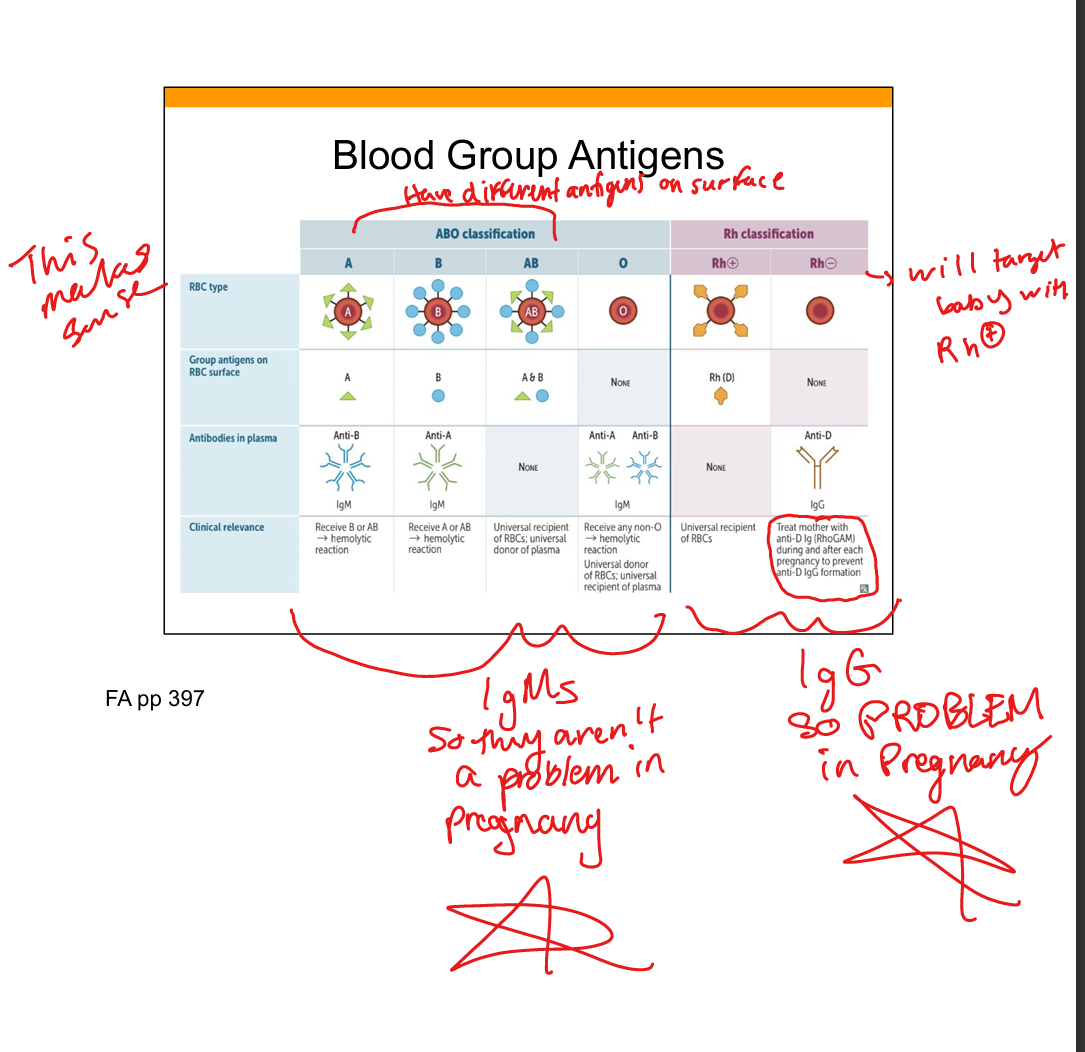
Describe the role of RhD antigens in transfusion reactions.
RhD is a protein antigen; anti‑D antibodies are IgG and can cross the placenta, causing hemolytic disease of the newborn; prevented with RhoGAM.
What causes an acute hemolytic transfusion reaction?
Recipient IgM antibodies bind donor RBC ABO antigens → complement activation → intravascular hemolysis within 1 hour.
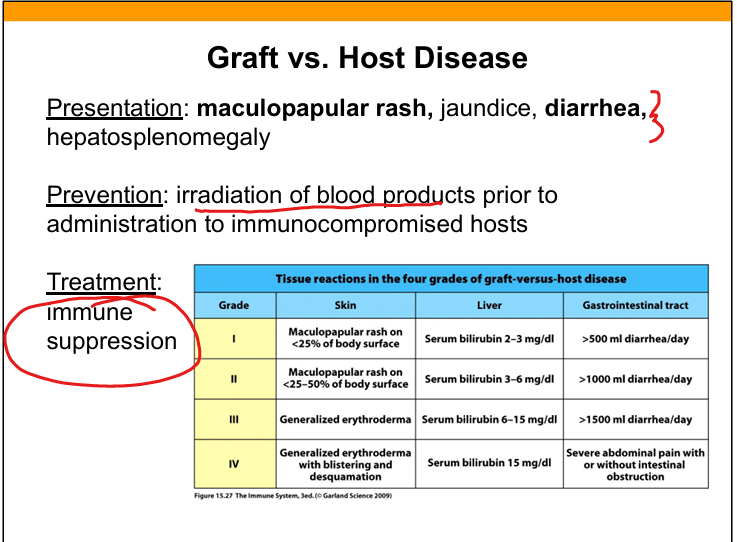
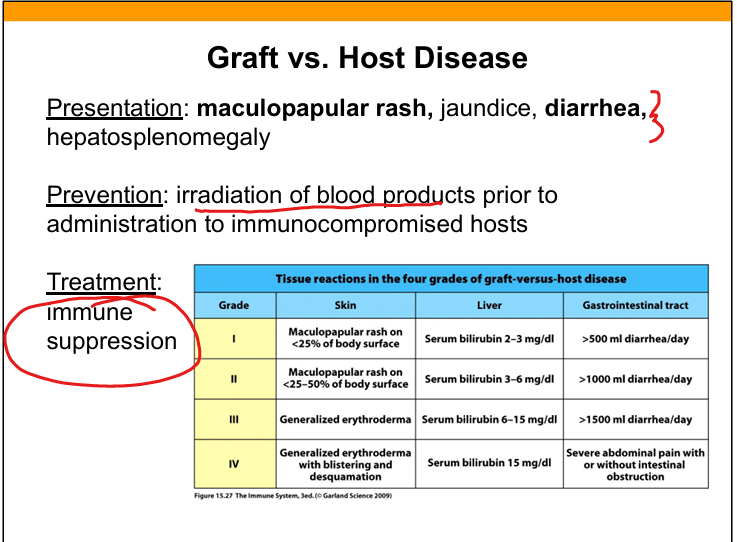
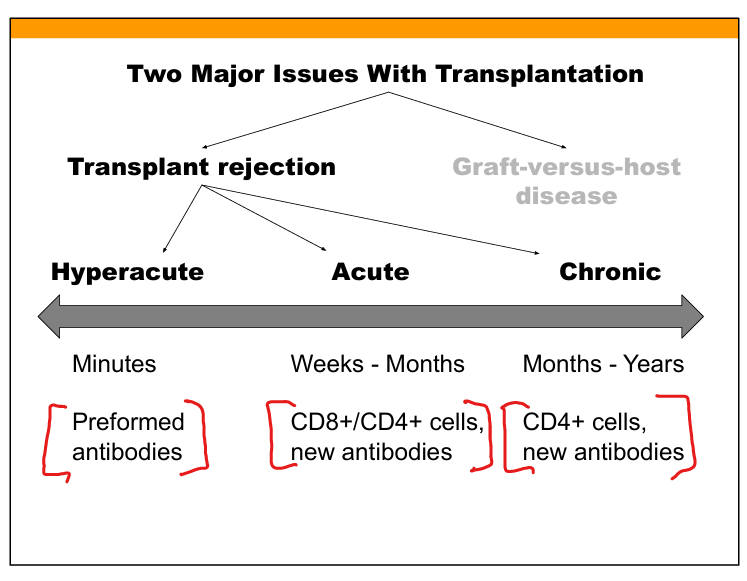
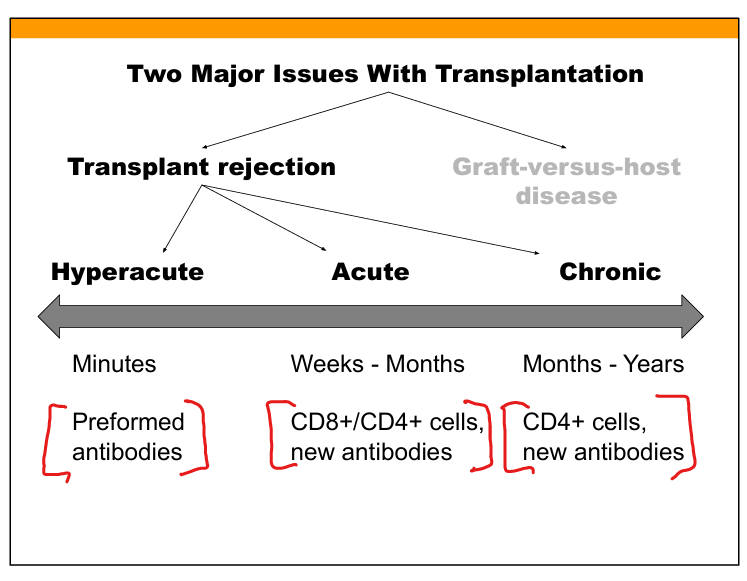
Differentiate graft-versus-host disease (GVHD) from transplant rejection.
GVHD: donor T cells attack host tissues (skin, liver, GI). Transplant rejection: host immune system attacks donor graft.
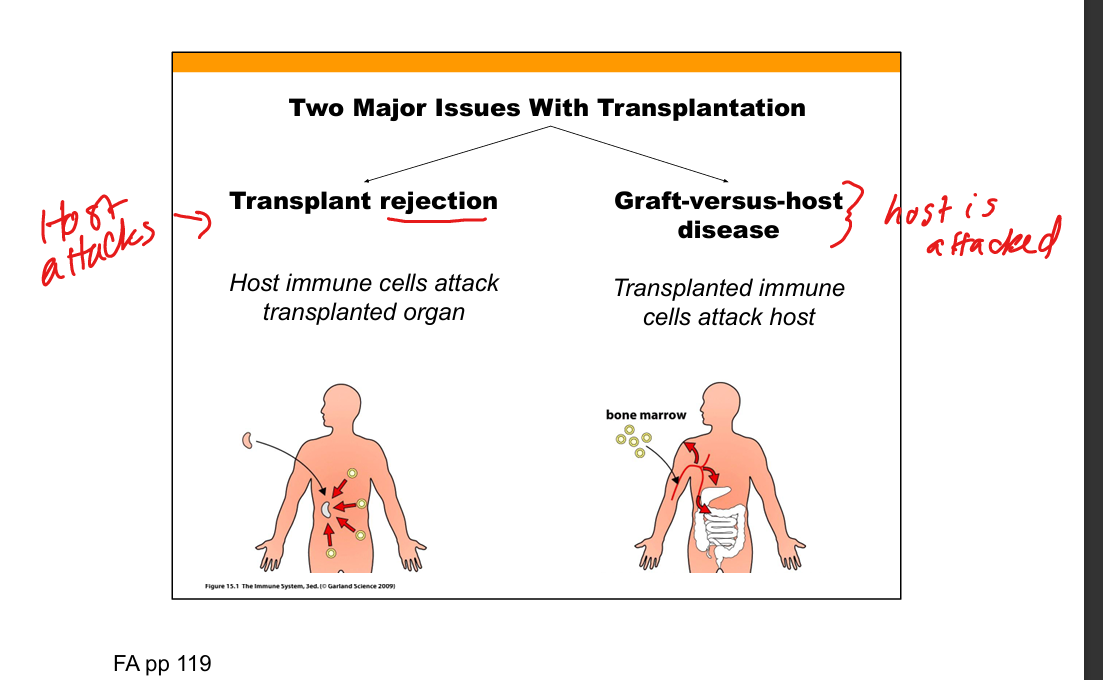
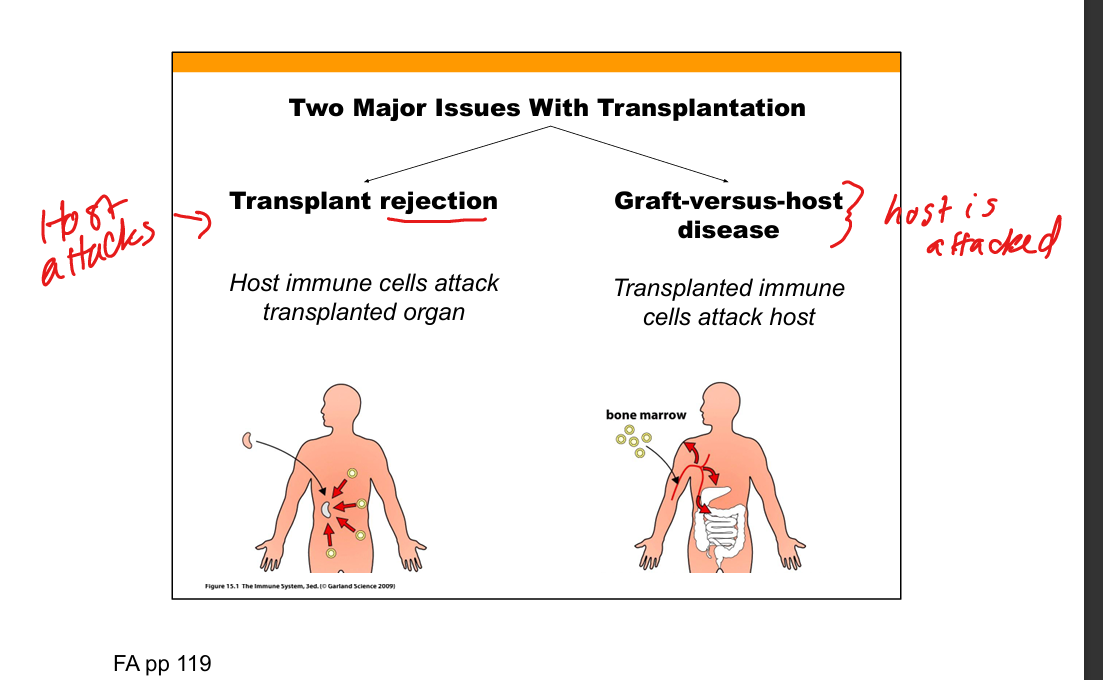
What is graft-versus-host disease?
Donor T cells recognize host cells as foreign → type IV hypersensitivity → rash, jaundice, diarrhea, hepatosplenomegaly.
What is transplant rejection?
Host T cells and antibodies recognize donor alloantigens (HLA/minor antigens) → graft damage.
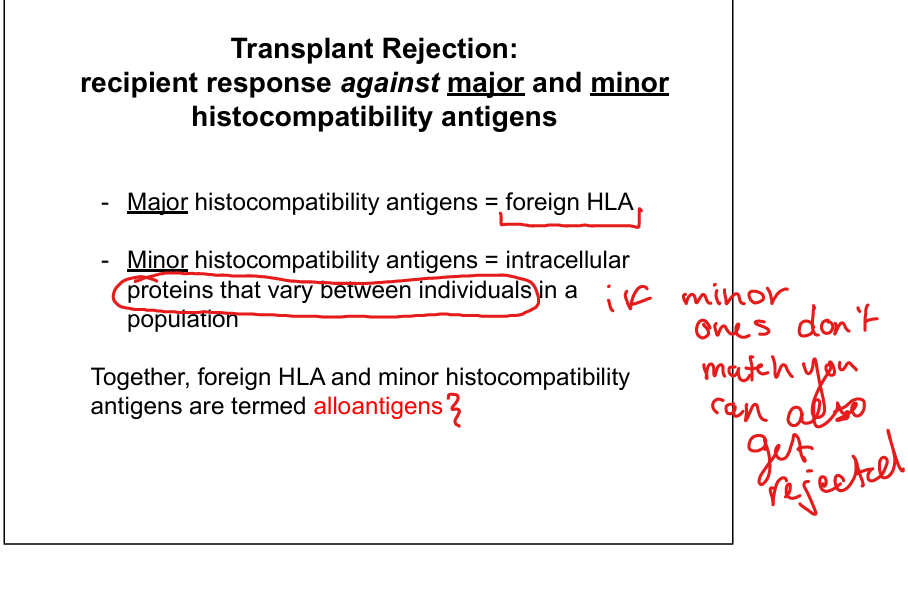
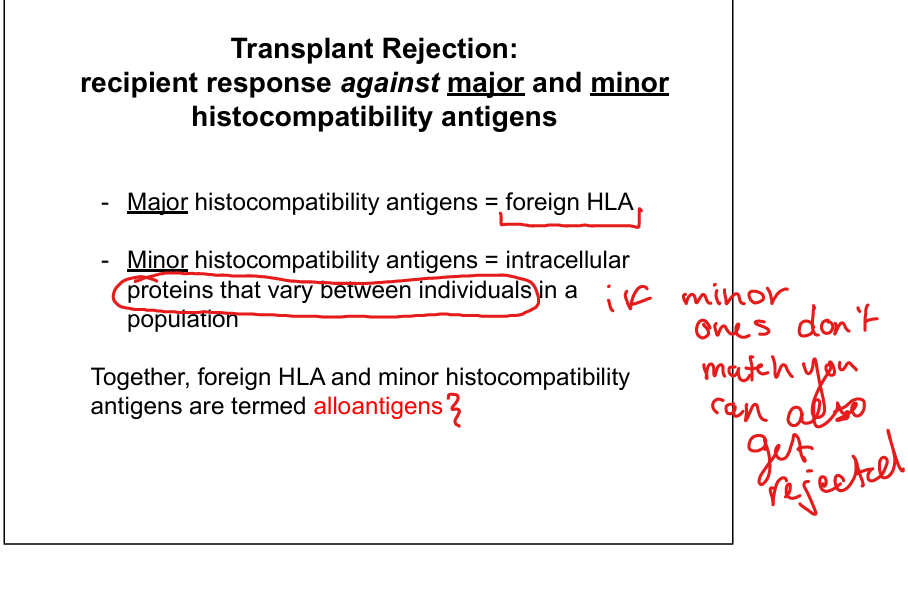
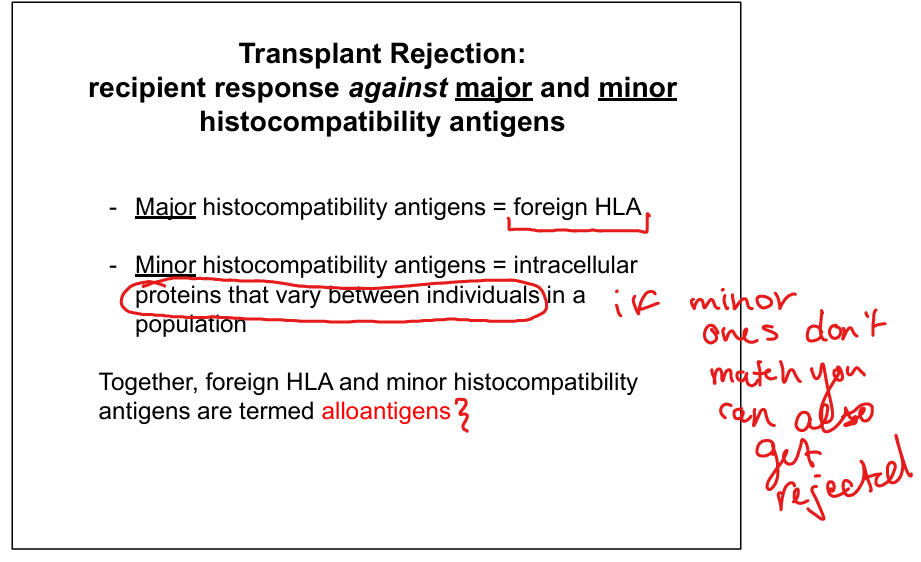
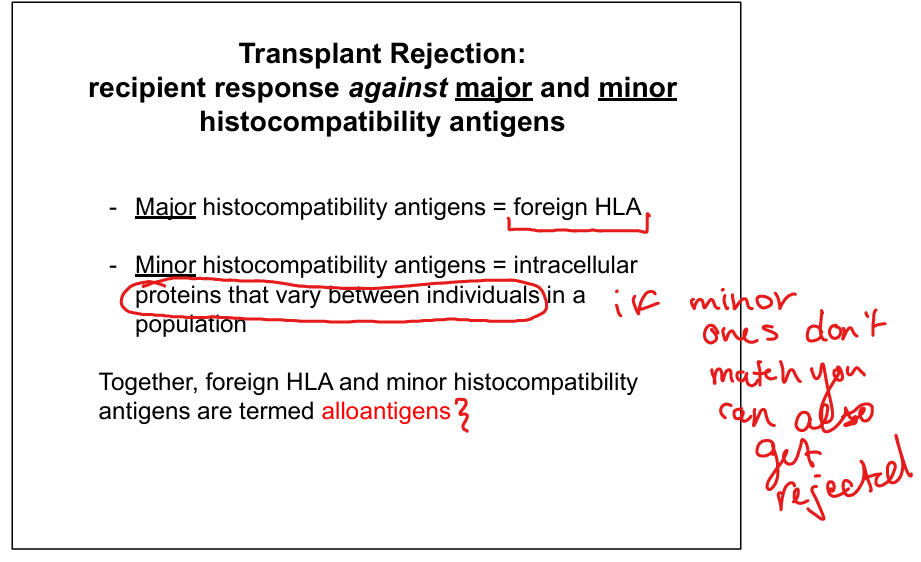
Identify the role of histocompatibility antigens in transplant rejection.
Major histocompatibility antigens = HLA mismatch; Minor histocompatibility antigens = polymorphic intracellular proteins; both trigger alloimmune responses.
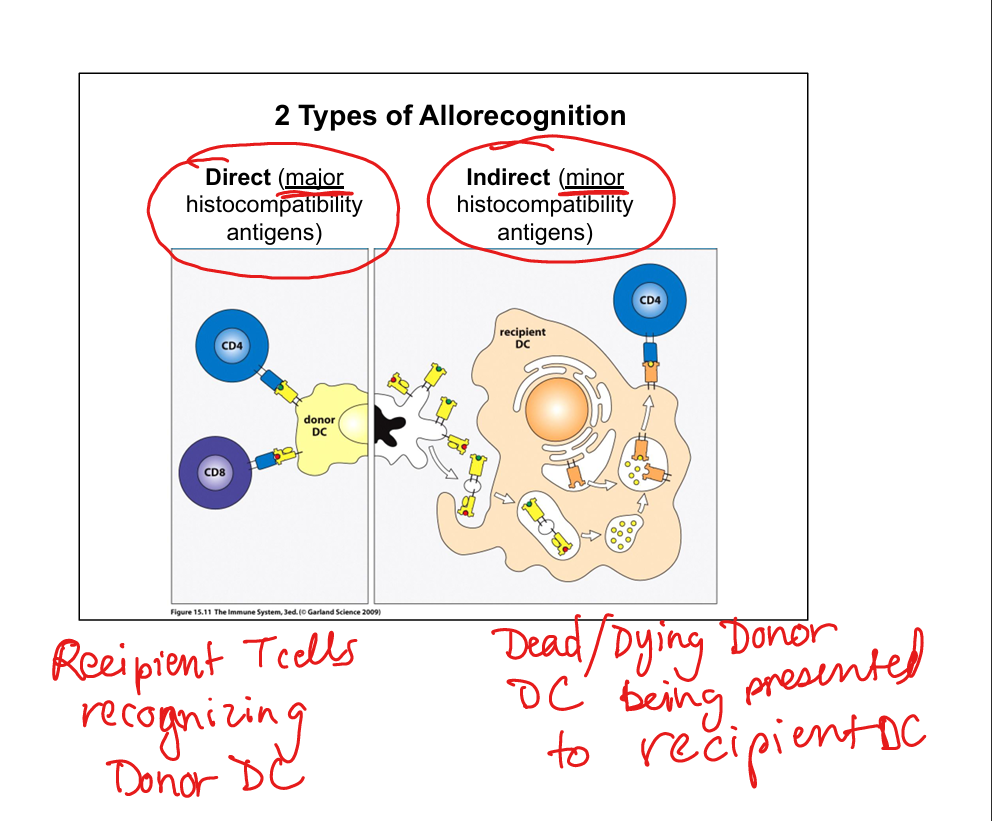
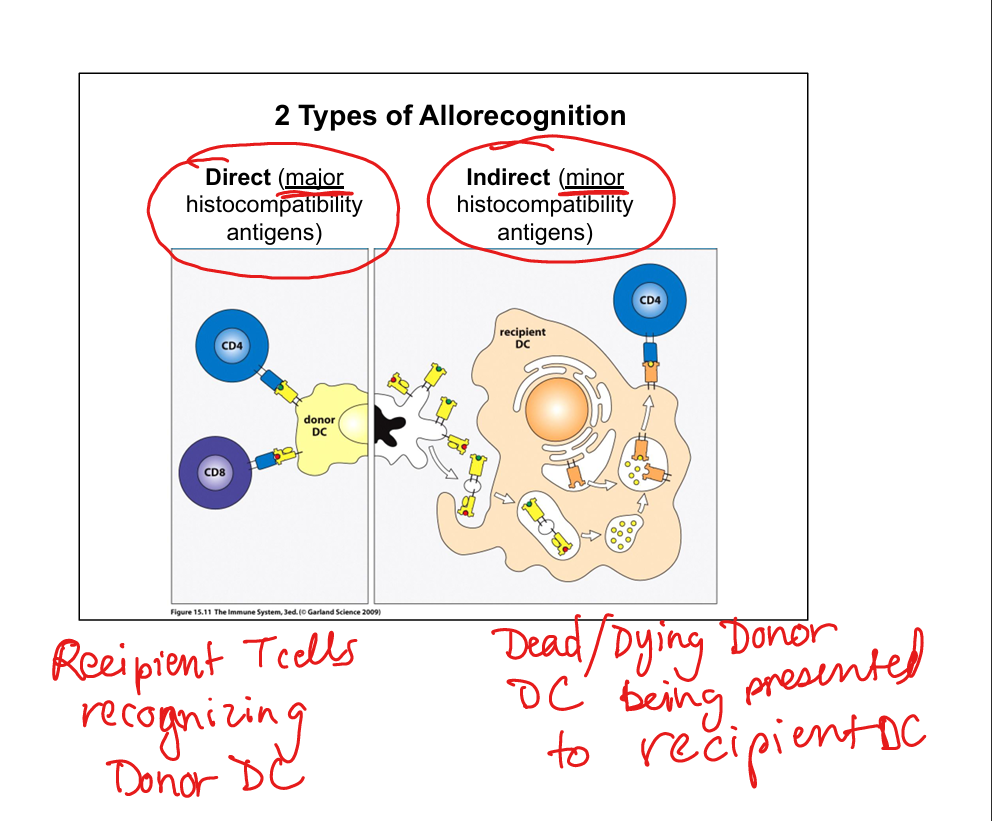
What are alloantigens?
Foreign HLA + minor histocompatibility antigens that stimulate host immune rejection.
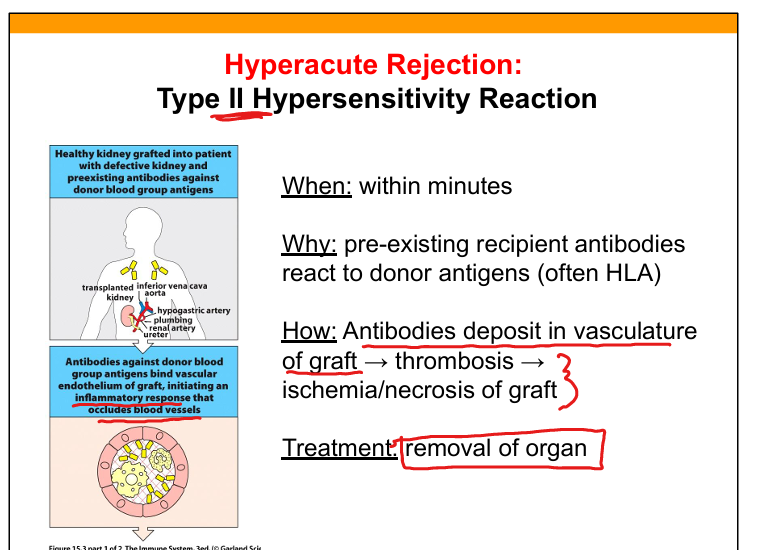
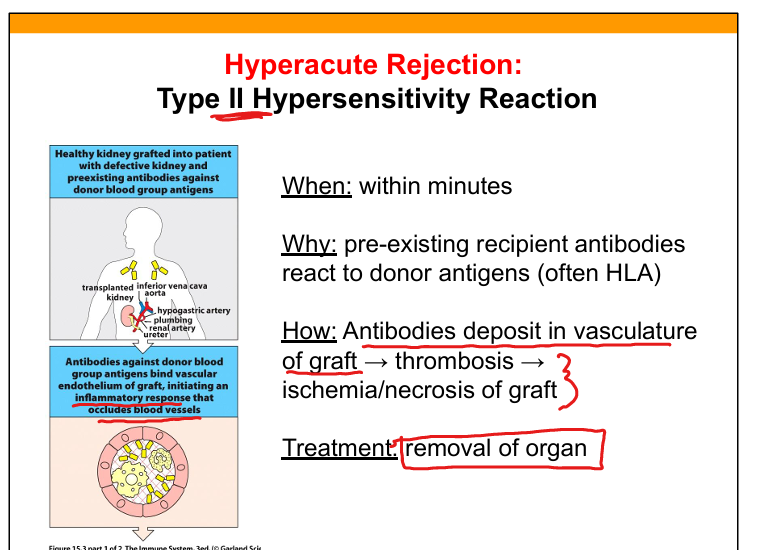
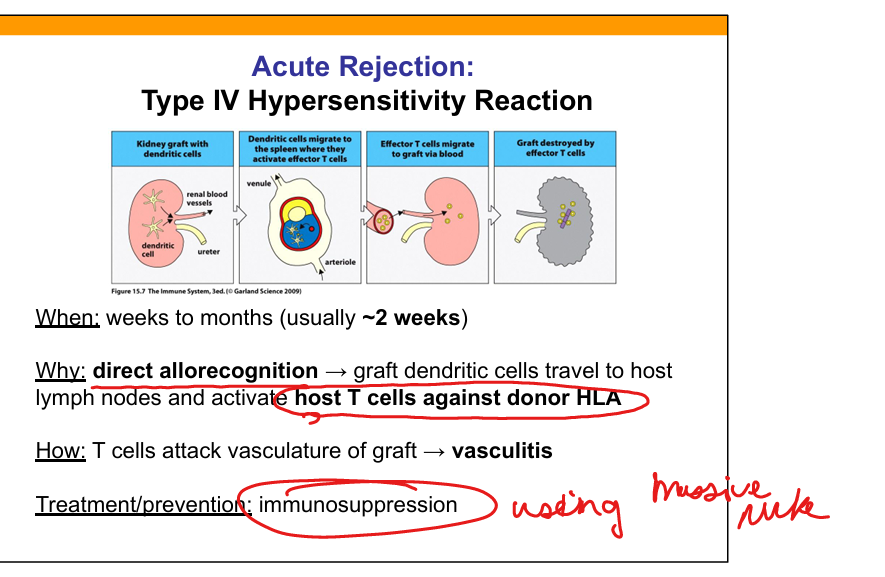
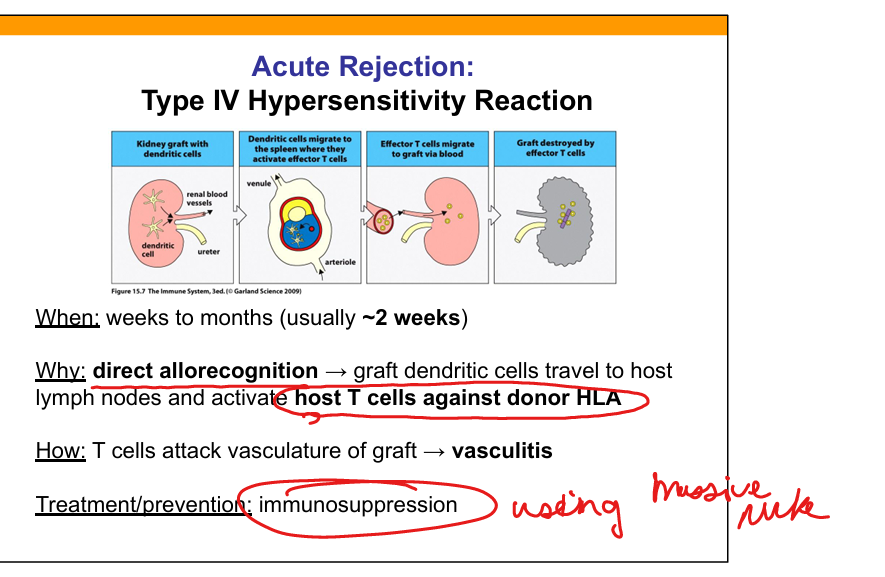
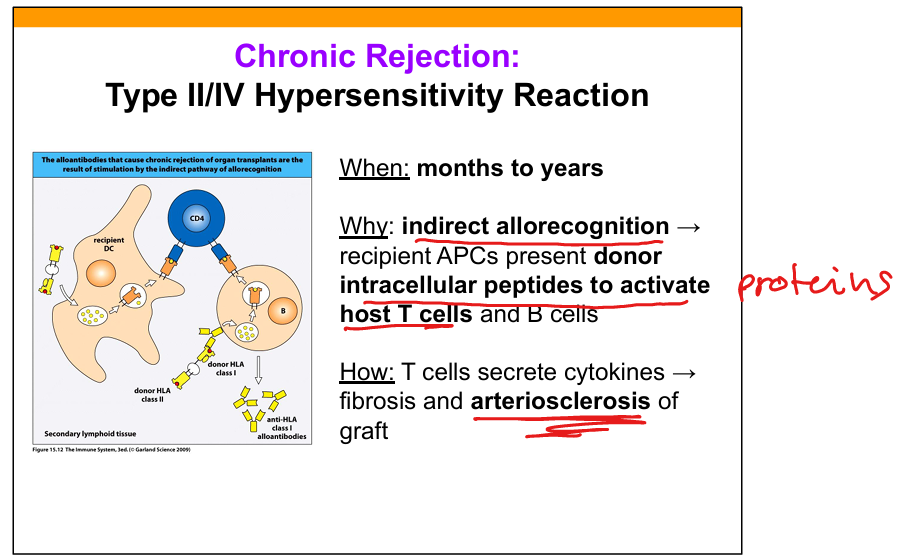
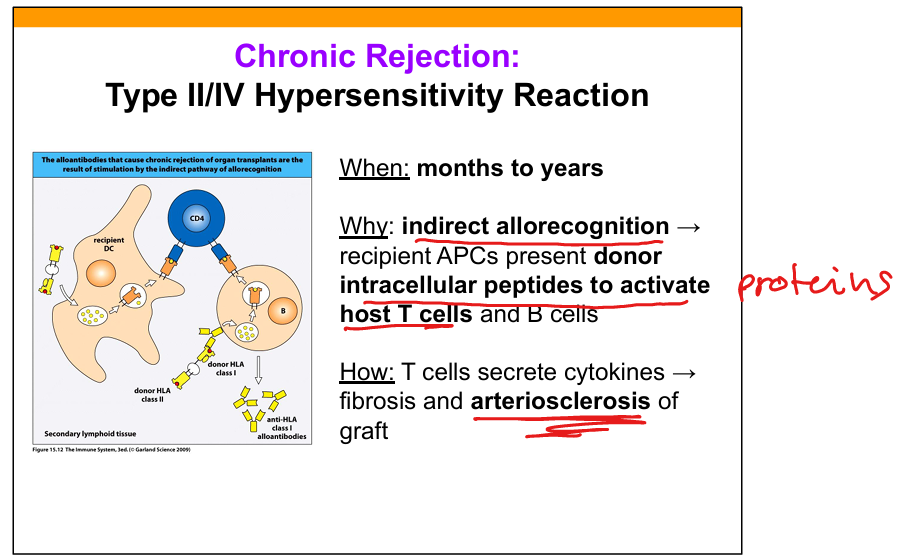
Compare hyperacute, acute, and chronic rejection.
Hyperacute: minutes; preformed antibodies; thrombosis/necrosis. Acute: weeks–months; host T cells attack donor HLA; vasculitis. Chronic: months–years; indirect allorecognition → fibrosis and arteriosclerosis.
Hyperacute rejection mechanism.
Preformed recipient IgG antibodies (anti‑HLA or anti‑ABO) bind graft endothelium → complement → thrombosis → ischemia.
Acute rejection mechanism.
Host CD8+ and CD4+ T cells recognize donor HLA via direct allorecognition → vasculitis; may also involve new antibodies.
Chronic rejection mechanism.
Indirect allorecognition → host APCs present donor peptides → CD4+ T cells and antibodies cause fibrosis and arteriosclerosis.
Why does Rh incompatibility cause disease but ABO incompatibility usually does not?
Anti‑D is IgG (crosses placenta); anti‑A/anti‑B are IgM (do not cross placenta).