3. Ocular glycosaminoglycans, lipid storage disorders, eicosanoids
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
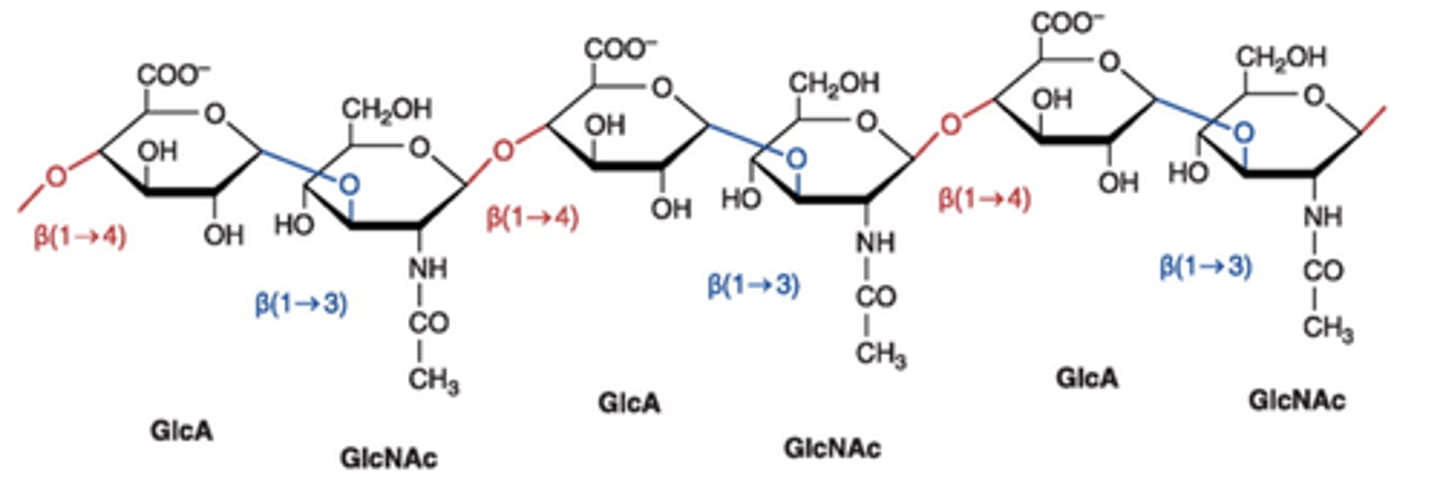
Glycosaminoglycans (GAGs)
-one of the components of connective, extracellular tissue in the eye (other is collagen)
-formerly called mucopolysaccharides
-polymers that consist of repeating two sugar units of a sugar and an amino sugar
What contributes to the negative charges on glycosaminoglycans?
-the presence of negative charges on the carboxylate and sulfate groups
-sulfation may take place in several positions – each adds another negative charge
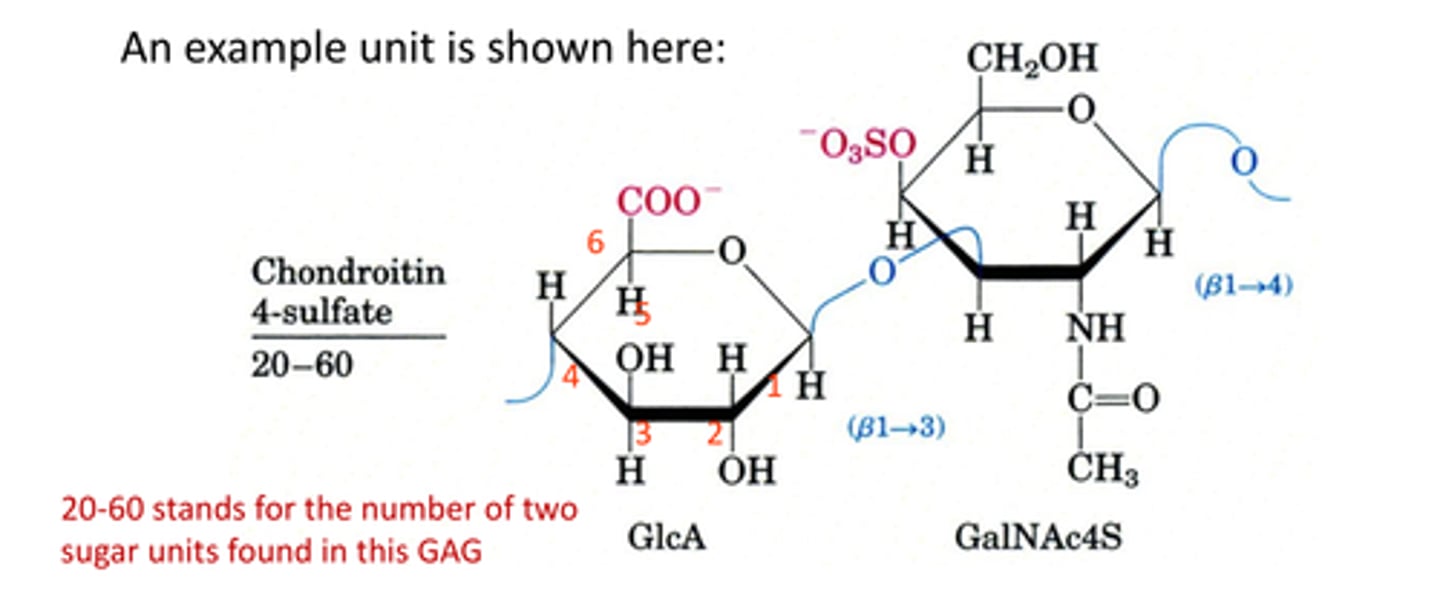
4 basic GAG units in the eye
-Hyaluronic acid (hyaluronate)
-keratan sulfate
-dermatan sulfate (similar to chondrointin sulfate)
-chondrointin sulfate
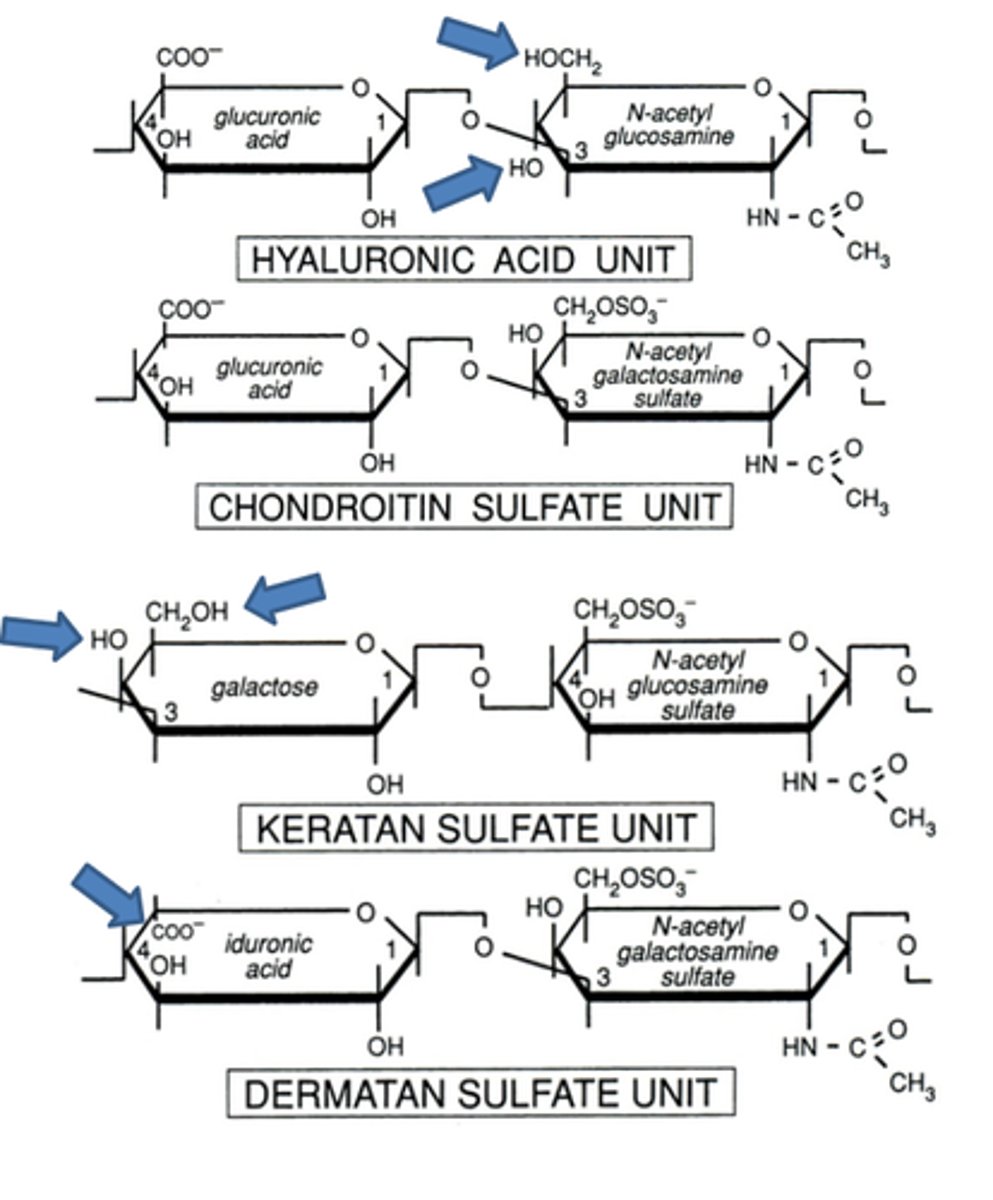
There are small structural differences between the 4 basic GAGs in the eye.
Does this impact the corneal component?
No, BUT these structural changes do account for different levels of accumulation of negative charges.
How do corneal GAGs compare to other GAGs in the eye (Specifically hyaluronate in the vitreous)?
-corneal GAGs have relatively short lengths
(~120 glycan units) whereas hyaluronate is composed of ~50,000 glycan units per molecule.
It can, therefore, be contained in a much larger volume.
The point is that these molecules (in very twisted and curved forms) absorb tremendous volumes of water and help the gel to have viscoelastic properties.
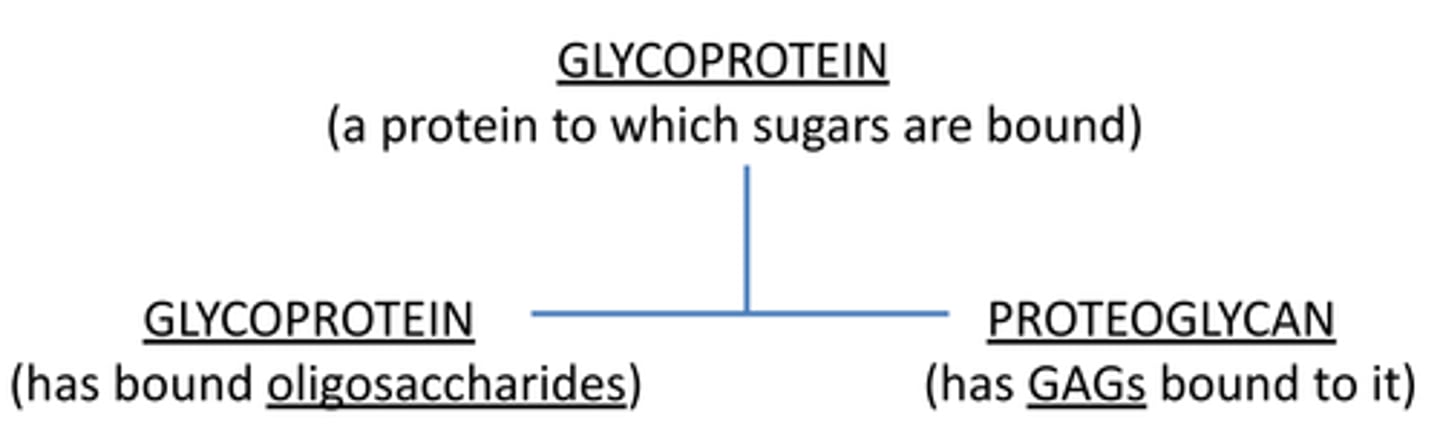
What is a glycoprotein?
protein + sugar
BUT, when referring to a glycoprotein specifically we specify the sugar as an oligosaccharide.
Protein + sugar (oligosaccharide)
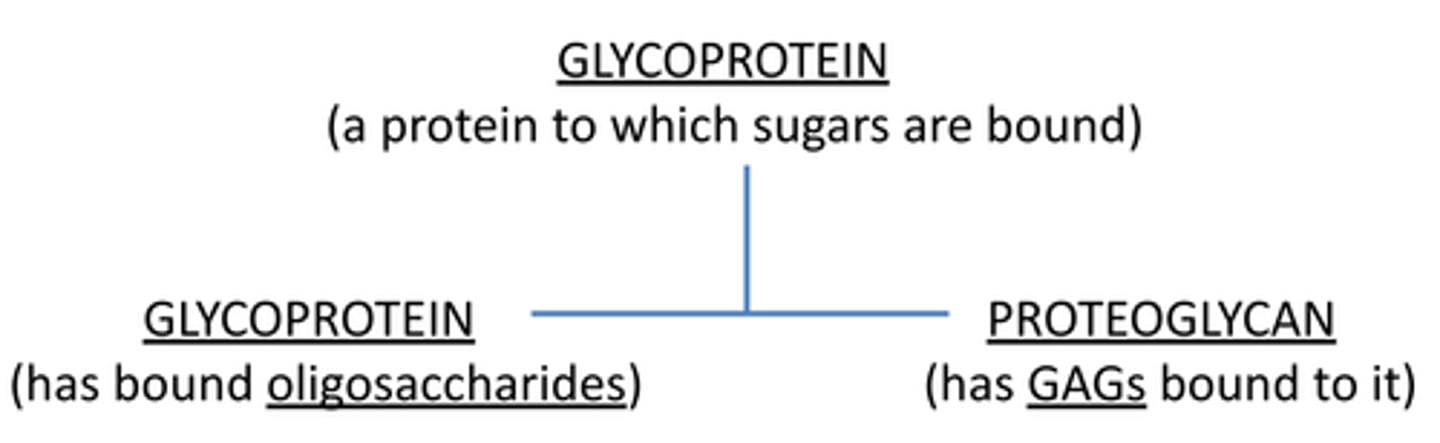
What is a proteoglycan?
-technically a glycoprotein BUT it is a:
protein + sugar (GAGs) & can have oligosaccharides
-can be holoprotein (conjugate of protein & GAGs)
-or an apoprotein - protein component (less GAGs)
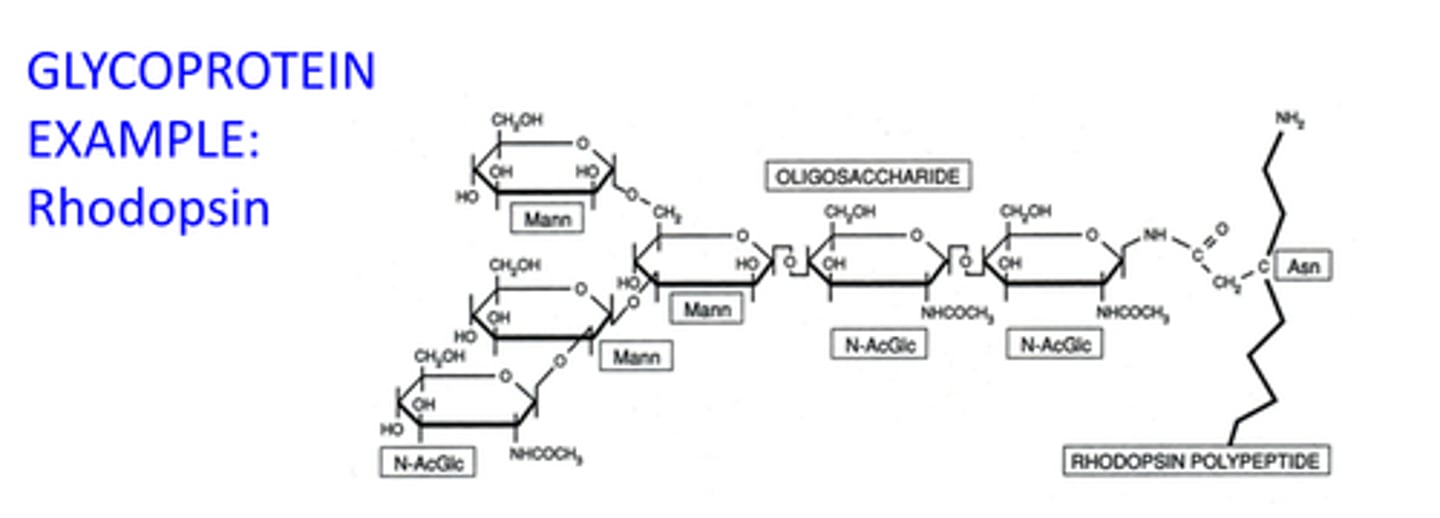
What is an example of a glycoprotein?
Rhodopsin
-2 sites of N-glycosylation w/asparagines 2,15 on rhodopsin, entire strings of sugars added to these sites in steps
-sugar is important for entering the membrane and being in proper arrangement
What are the 2 proteoglycans in the human cornea?
what are their functions?
decorin and lumican
-these also happen to be glycoproteins (have linking oligosaccharides & at the ends)
-These molecules act as molecular spacers between type I collagen fibers and also exhibit some viscoelasticity.
Lumican proteoglycan is composed of what GAG
keratan sulfate
Decorin proteoglycan is composed of what GAGs
-chondroitin sulfate
-dermatan sulfate
-keratan sulfate
-bind to different positions at different amino acids
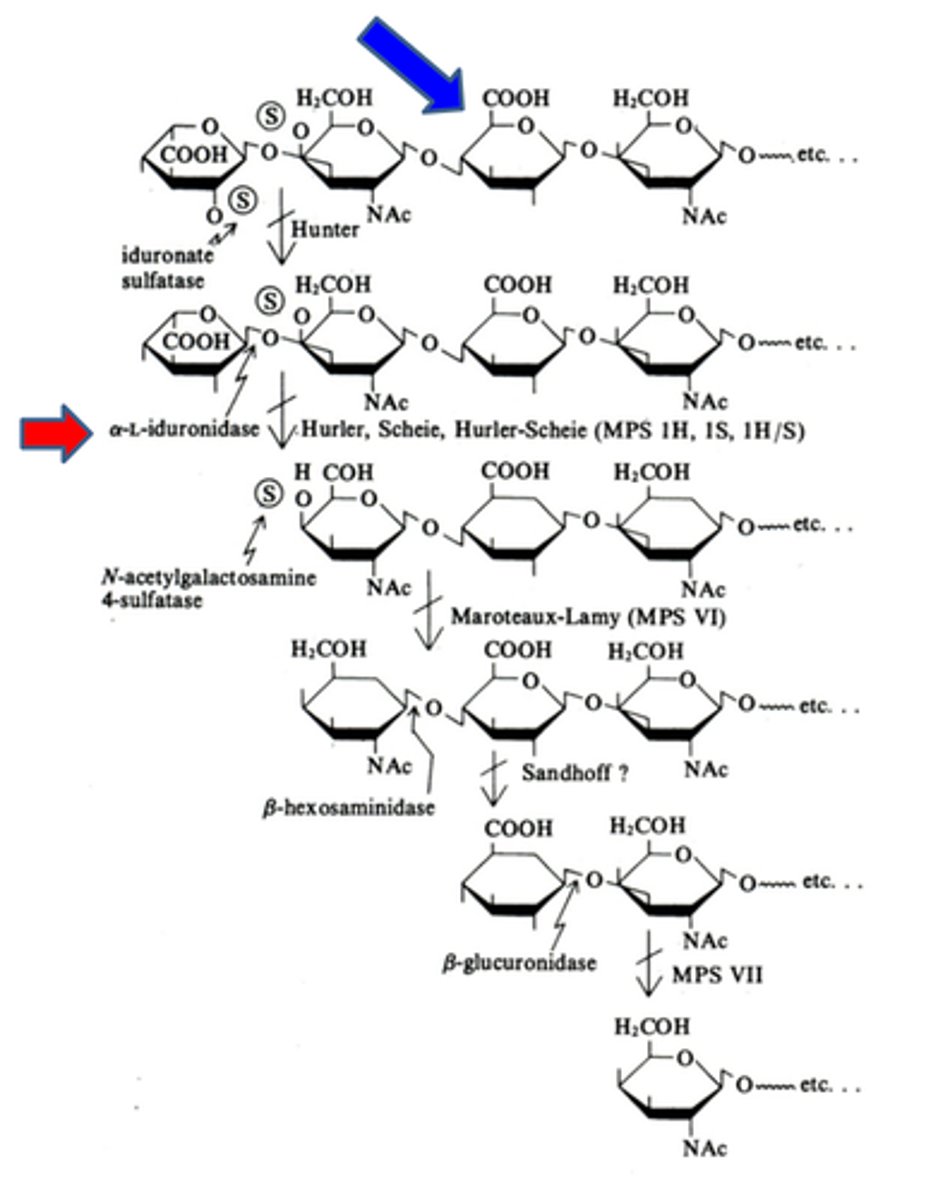
What happens to old or damaged glycosaminoglycans?
-transported to lysosomes w/ low pH and a host of about 30 degradative enzymes that will convert them to simpler molecules that can be reused.
mucopolysaccharidoses
-what is this caused by?
-rare genetic disease usually involving defects in degradative enzymes that are needed to break down GAGs
-can be missing, non-functional, or have signaling defects in which they can't enter into lysosomes
ex: Galactosemia in which any of the 3 proteins are missing
What happens in mucopolysaccharidoses when GAGs can only be partially broken down?
-partly degraded GAGs accumulate in the lysosomes, engorge the cells and then spill out into nearby tissues.
-devastating to limbs and joints as well as brain tissues.
Metabolic storage diseases
-recessive congenital disease
-mental retardation
-can involve only partial degradation of GAGs, lipids, and polysaccharides.
-(complete inability to break down is embryonically lethal)
Hurler Syndrome (MPS IH) & Scheie's Syndrome (MPS IS) cause:
-caused by a α-L-iduronidase deficiency (red arrow)
-this is needed to break down dermatan sulfate and heparan sulfate
-onset in infancy
How Hurler Syndrome affects the eyes
-In the eyes, the cornea becomes cloudy and the optic nerve degenerates; glaucoma may occur.
-There is an accumulation of dermatan sulfate and heparan sulfate (2:1) in the tissues including the eyes, blood and urine
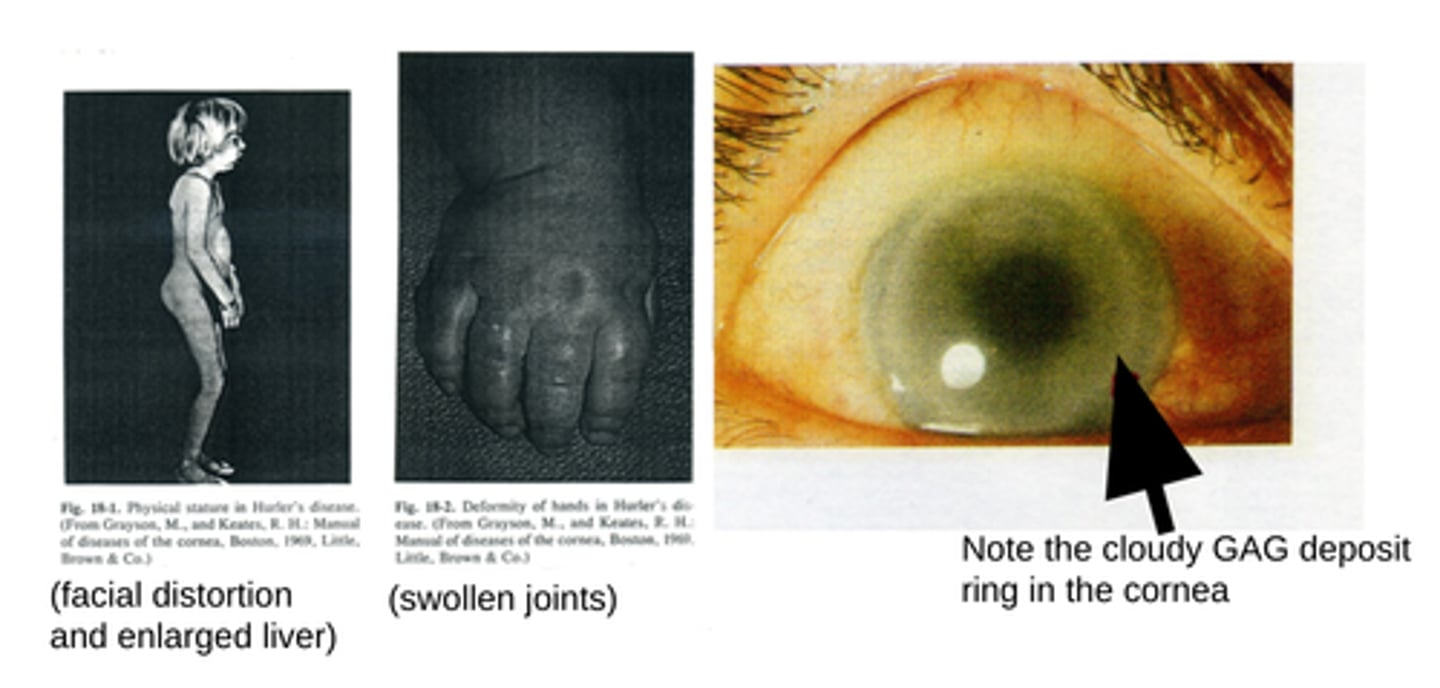
Hurler Syndrome symptoms (besides the eye)
-linear arrest in growth at ~1 year of age
-psychomotor retardation
-GAGs pile up in the joints and internal organs, causing a distorted facial appearance, deformed and stiff joints with an enlarged liver and spleen
-Usually fatal within a few years, due to congestive heart failure and respiratory pulmonary infections.
What is the least common lysosomal storage disease?
Hurler syndrome 30 cases/year in the U. S.
Hurler/Sheie disease 30 cases/year in the U. S.
Sheie's disease 10 cases/year in the U. S.
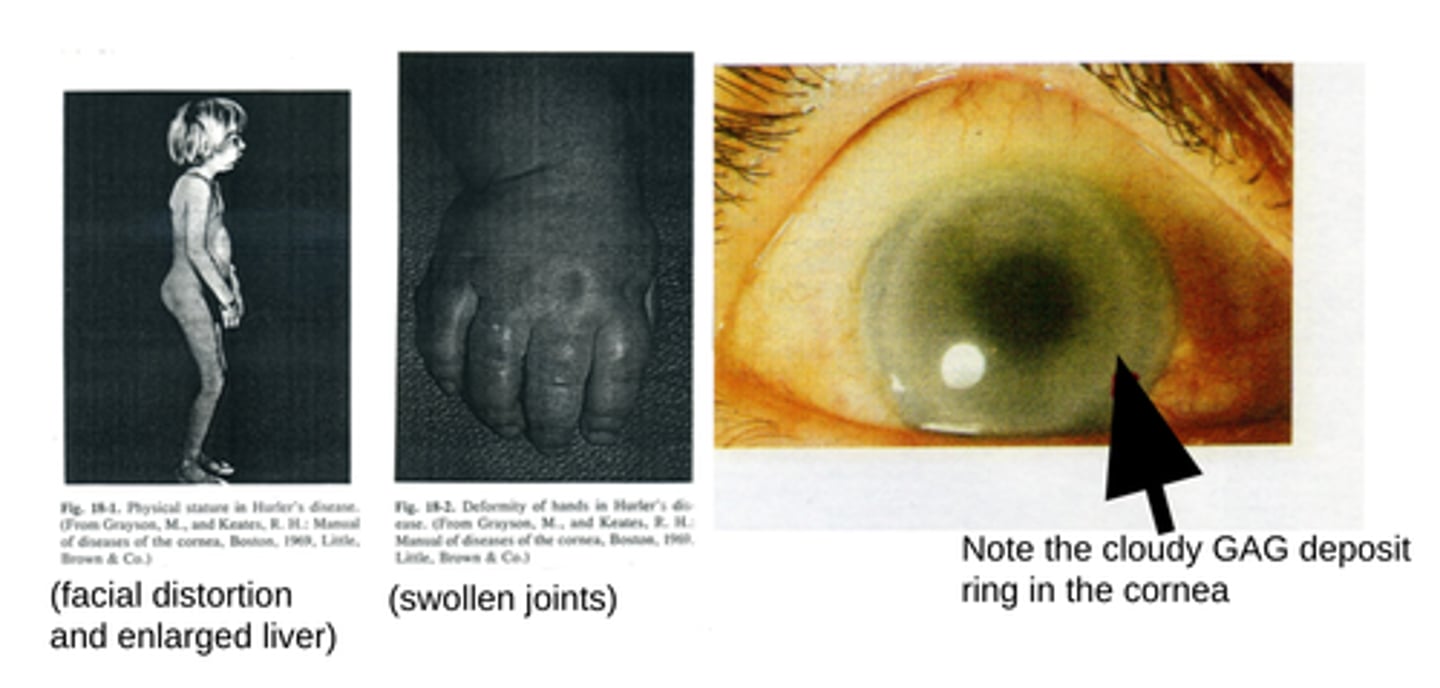
Accumulation of GAGs in a histiocyte of the brain of a Hurler’s patient.
histiocyte is a type of phagocyte derived from bone marrow that invades other tissues.
-Note the engorgement of GAGs in the vacuoles of the cell (colored red).
Assay for Hurler's Syndrome
1. An artificial substrate replaces dermatan sulfate (or other GAG) with a fluorogen bound to iduronic acid.
2. When the enzyme lyses the substrate, the product: 4-methylumbelliferone fluoresces at 446 nm (excitation at 365 nm) in proportion to the activity of the enzyme.
Treatment of mucopolysaccharidoses
-Bone marrow/umbilical cord blood transplantation
-The earlier this is done the better to avoid irreversible brain damage.
-New bone marrow makes the missing enzyme and can be successful, but is risky with a high rate of morbidity and mortality
Treatment of mucopolysaccharidoses
-Enzyme replacement therapy
-This has limited success and often will not correct neural damage
-has been useful in reducing non-neurological symptoms and pain.
-It’s long term outcome is not known.
Treatment of mucopolysaccharidoses
-Gene replacement therapy
-Viral gene transfer has been successful in animal studies, but not yet approved for human treatment.
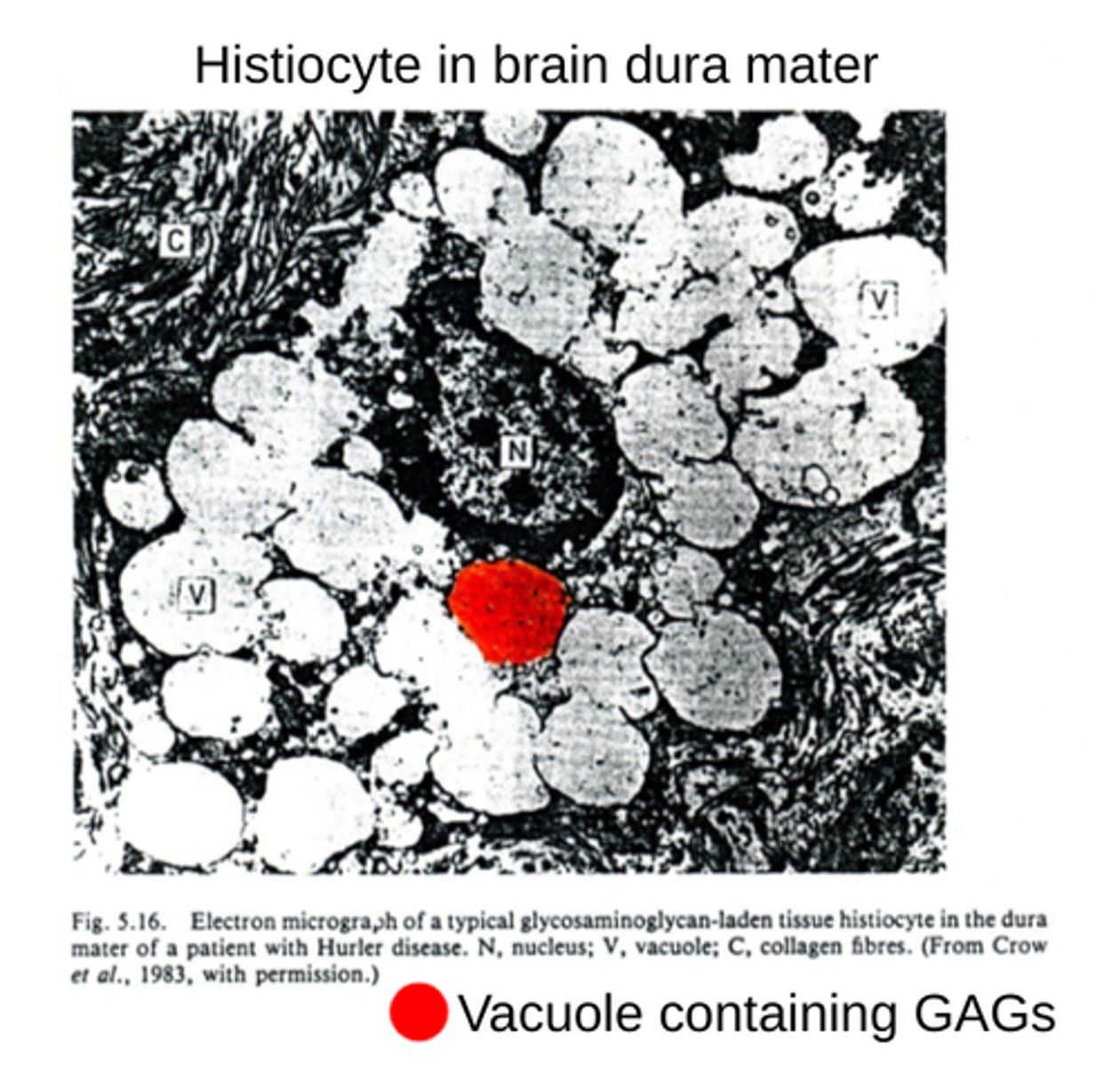
Cherry Red spot
-occurs notably in storage diseases involving lipids
-whiteish area is from retinal neurons, filled with accumulation of gangliosides
-The red area is the blood circulation of the choroid in the fovea which is normal.
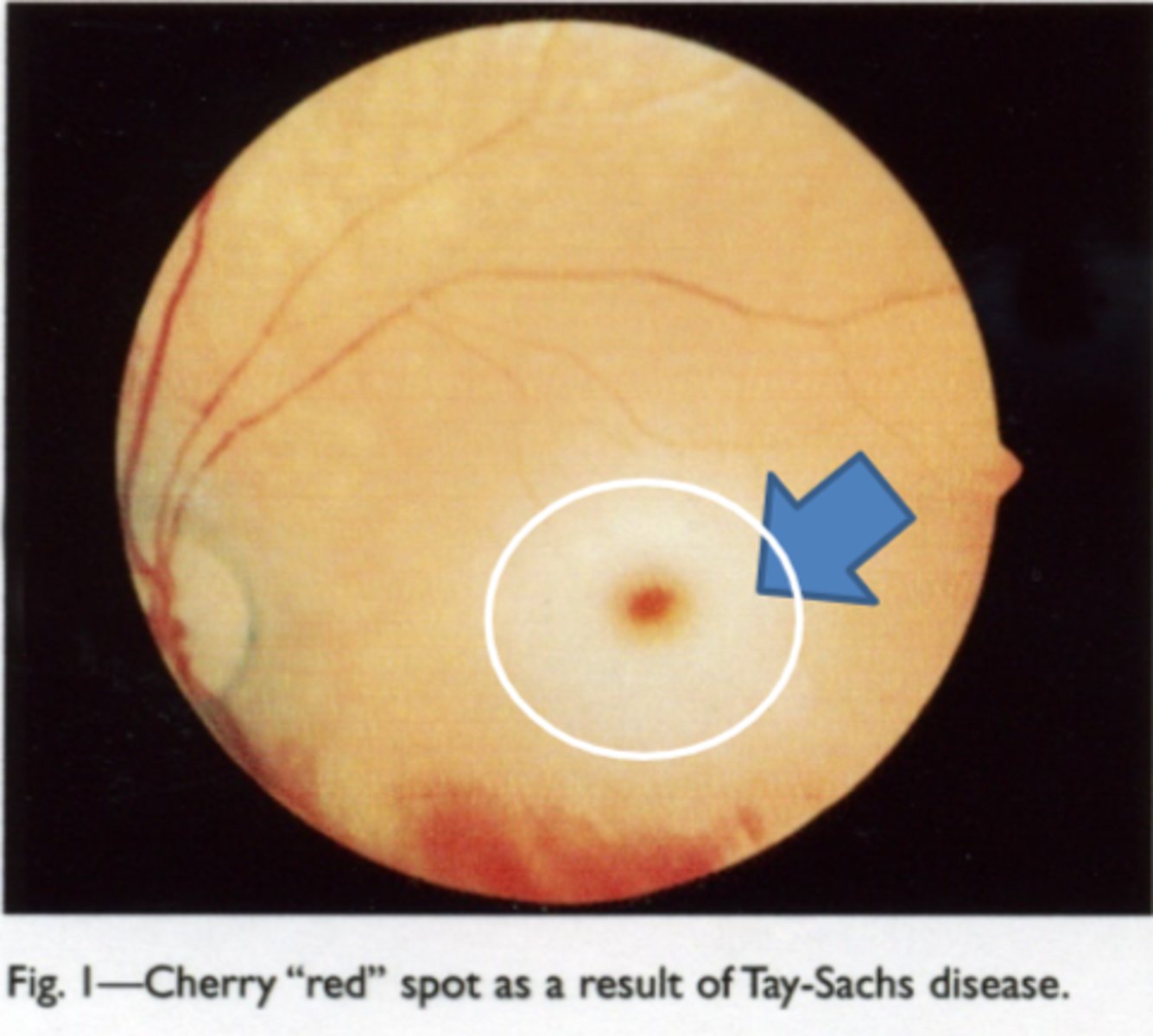
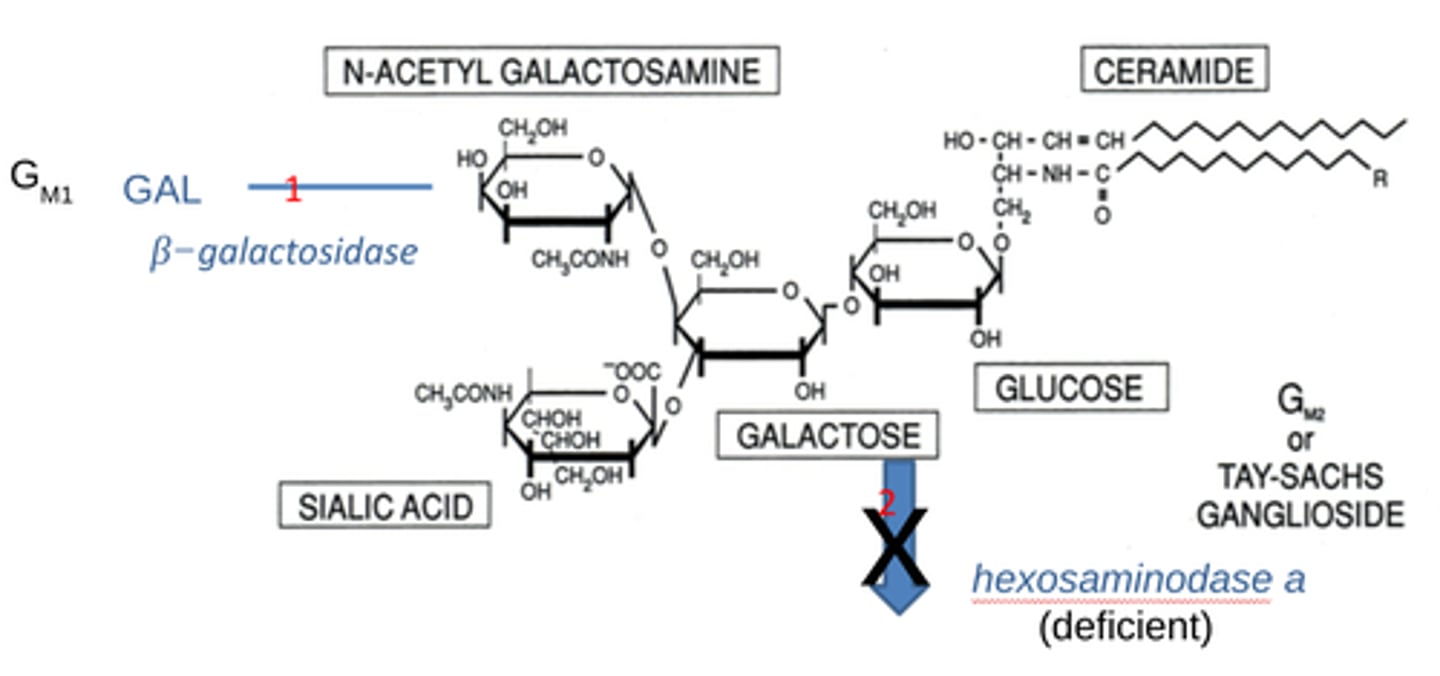
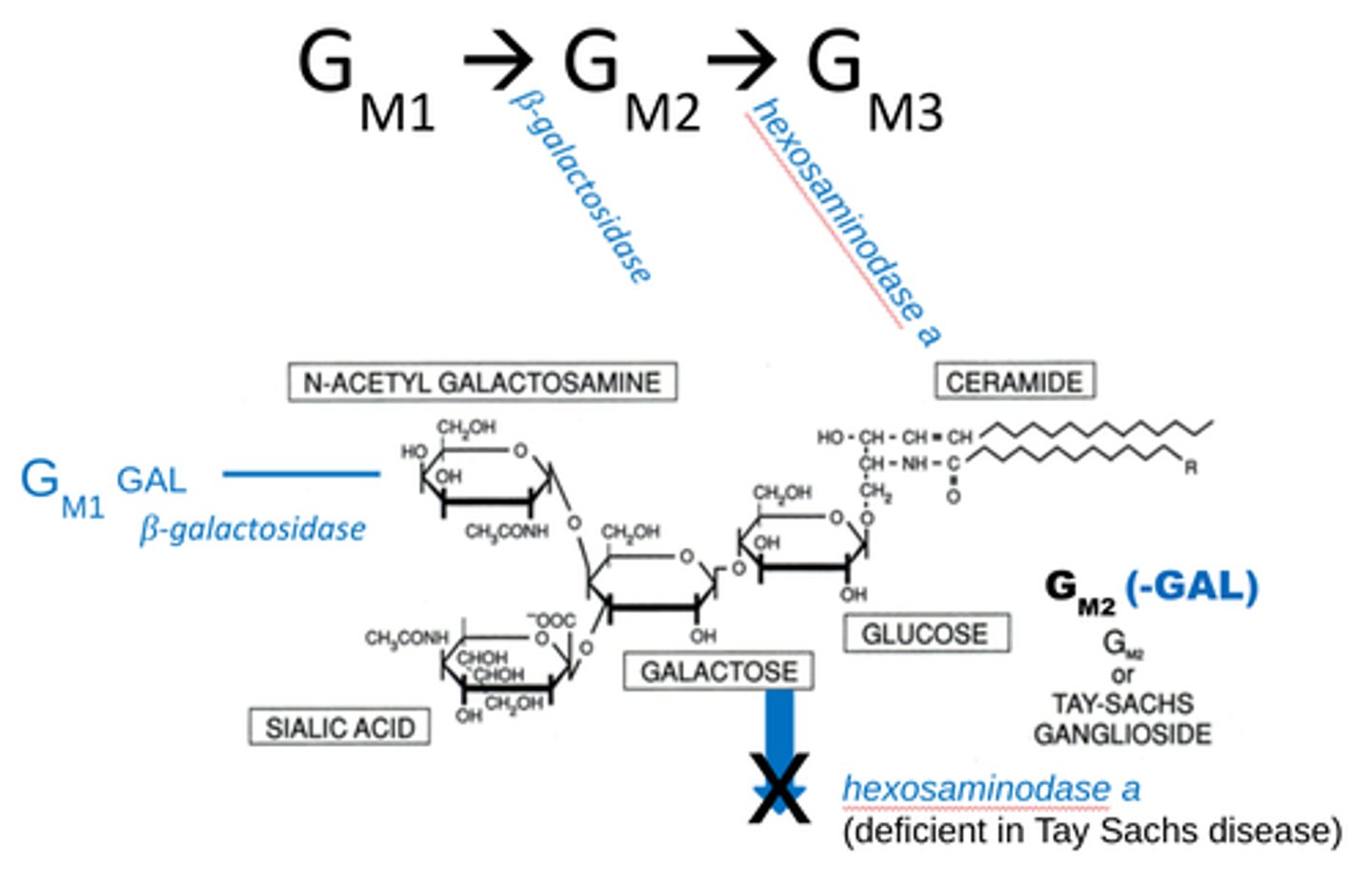
Tay-Sach's Disease
-caused by hexoaminodase a (HEXA gene) deficiency
-A sphingolipidosis in which GM2 ganglioside accumulates in neural tissue and destroys neural cells in both the brain and neural retina.
What ethnic demographics are primarily impacted by Tay-Sach's Disease
-It occurs in Ashkenazi Jews, Cajuns and French Canadians.
Is there are cure for Tay-Sach's disease?
-There is no cure or treatment.
-Brain cells start dying by about 6 mos. and survival is usually not beyond 5 yrs.
Tay-Sach's Disease Biochemical mechanism
1. β−galactosidase removes galactose from GM1-GAL ganglioside to make GM2
2. hexoaminodase a removes terminal N-acetyl hexosamines from GM2 to make GM3, BUT, those w/ Tay-Sach's lack this
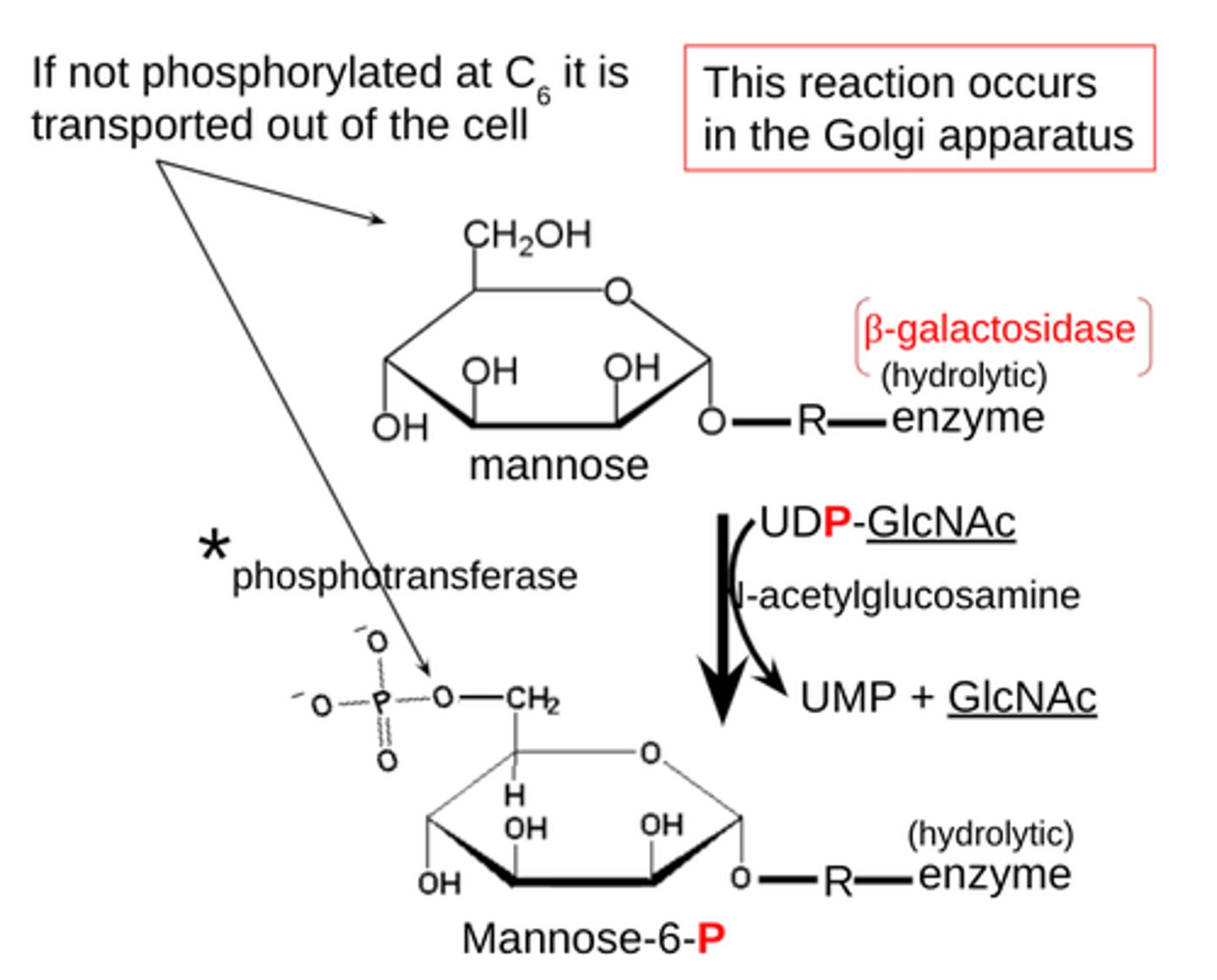
(Inclusion)-CELL DISEASE
I-cell disease
-mucolipidosis
-N-acetylglucosamine 1-phosphotransferase is genetically defective and is needed to add a phosphate group to a mannose sugar at C6 on the β-galactosidase as a signal to move it to lysosomes.
-occurs in the golgi apparatus
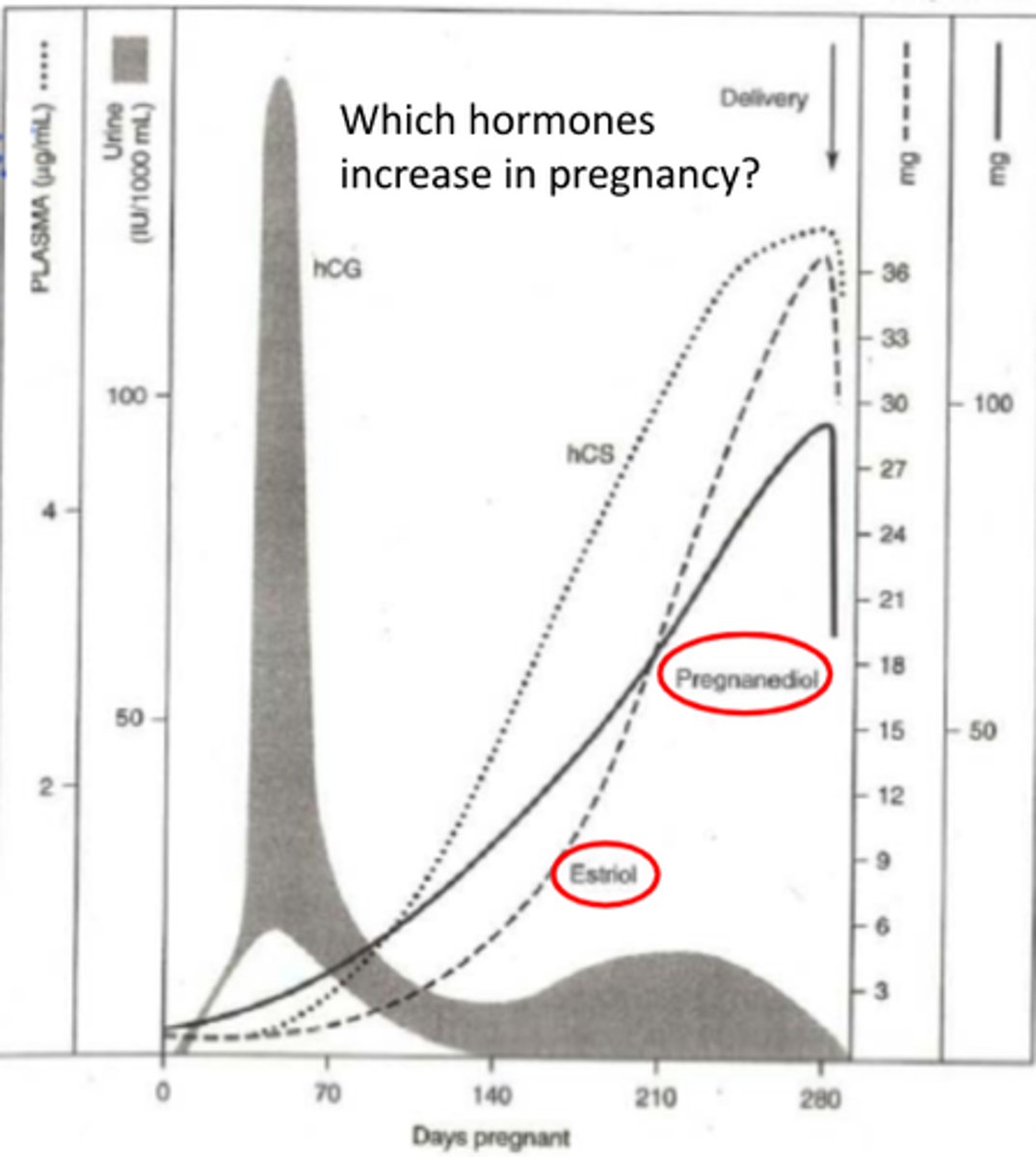
Thyroid hormone complications in pregnancy
-pregnant women often complain of dry eyes
-caused by fluctuations of estrogen & androgen (decrease production of tears)
-can also have thickening of cornea due to fluid retention (can cause blurry vision)
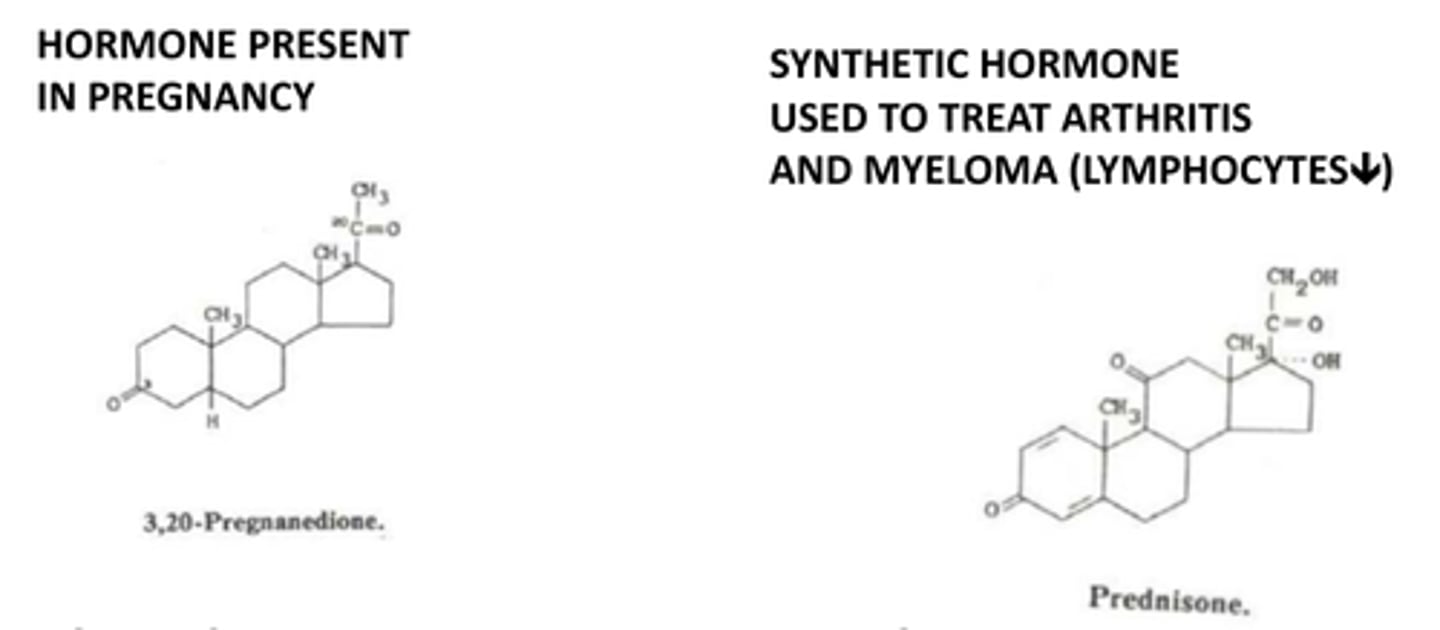
Estriol
type of estrogen produced by the ovaries
-increased during pregnancy
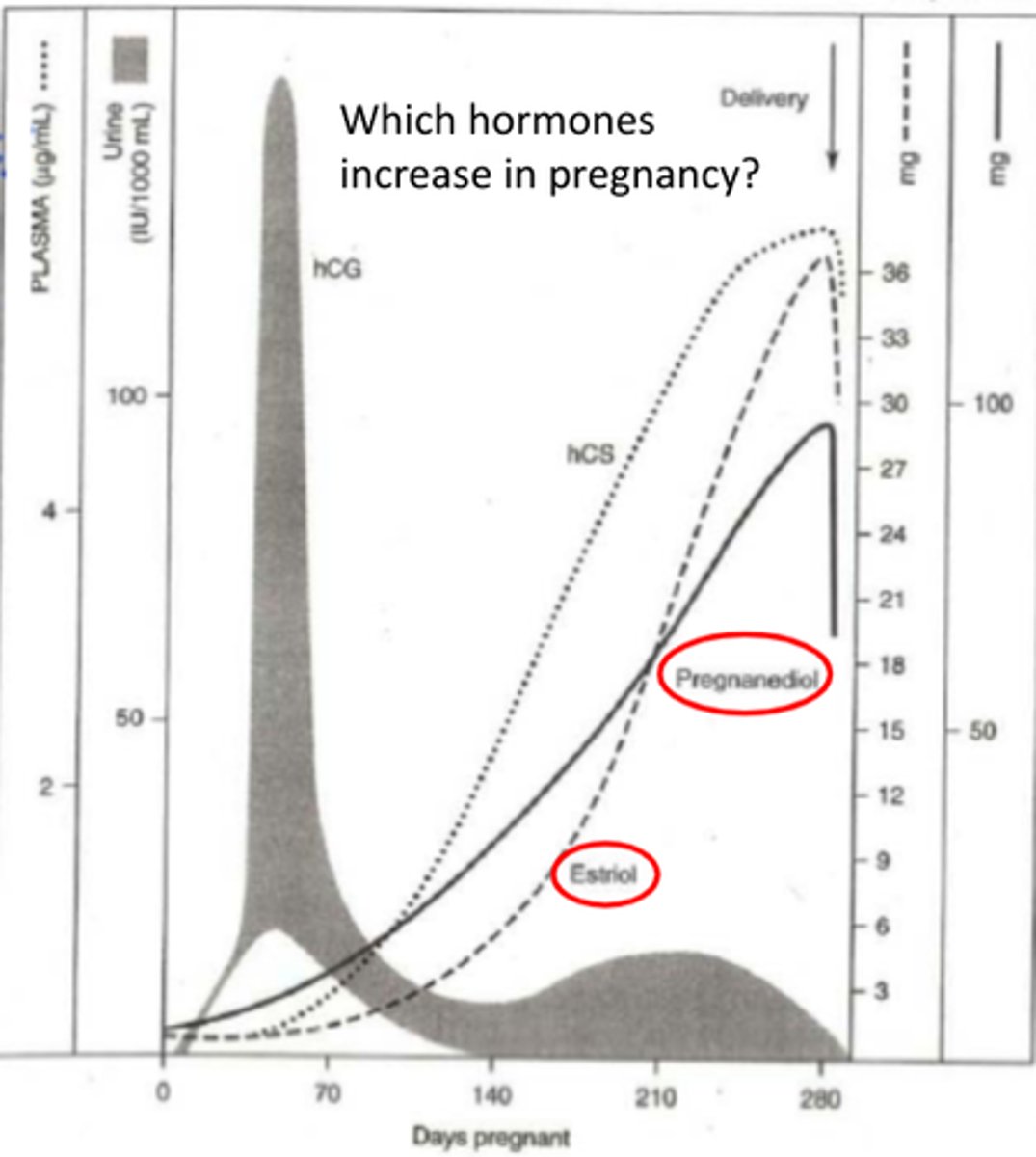
Pregnanediol
an inactive byproduct of progesterone
-increases during pregnancy
-Progesterone is an endogenous steroid hormone involved in the menstrual cycle, pregnancy, and embryogenesis.
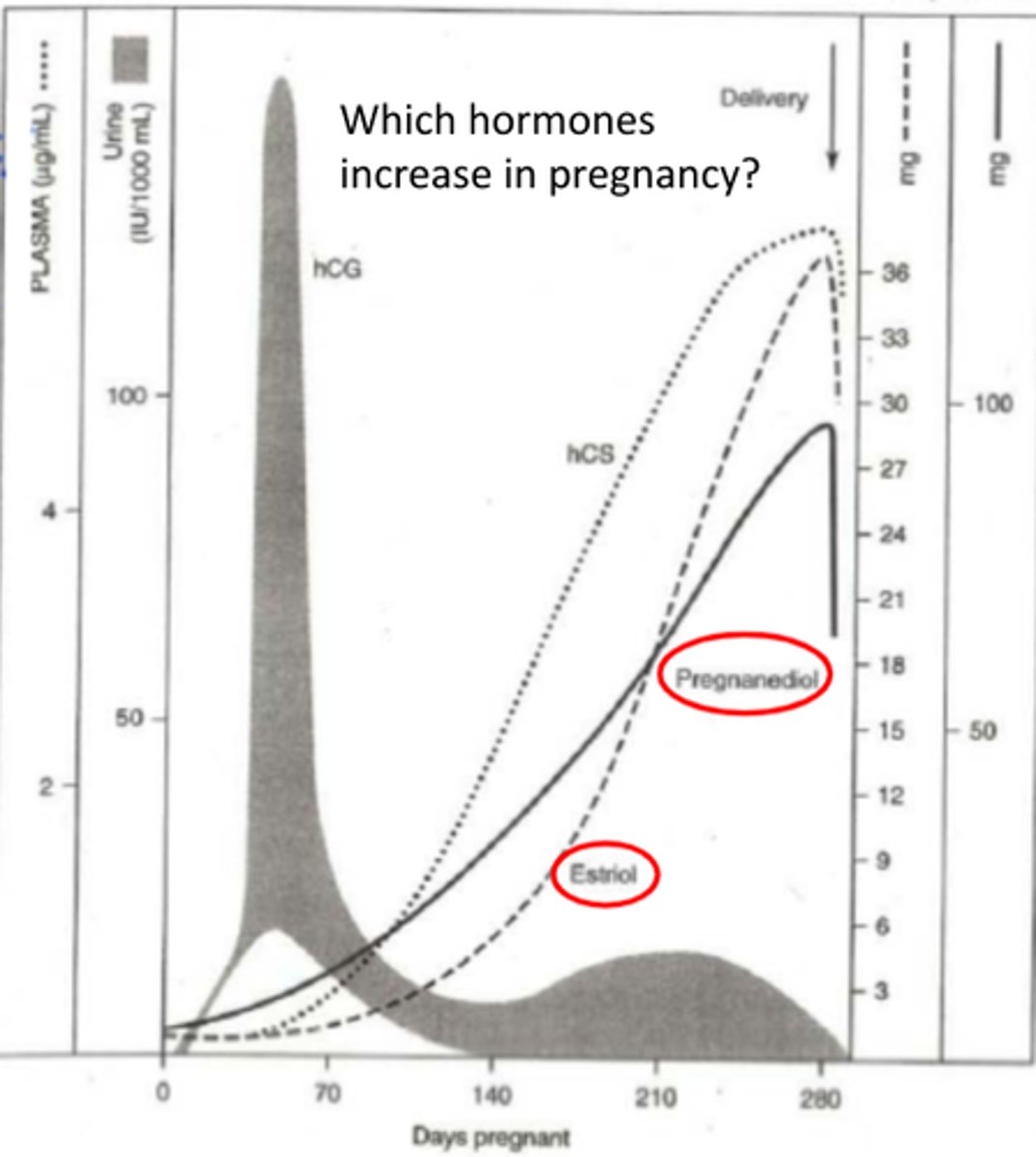
What is HCG?
-functions to maintain the corpeus luteum in the early stages of pregnancy
-promotes progesterone release.
-also called human placental lactogen, supports fetal nutrition.
structure of Eicosanoids
-local hormone made by oxidation of twenty-carbon Essential fatty acids, (EFAs)
-have at least 3 dbl bonds
-from either omega-3 (ω-3) or omega-6 (ω-6) EFAs (pro-inflammatory)
Functions of Eicosanoids (eicosa is Greek for 20)
-signaling molecules in CNS
-effects on cardiovascular disease, triglycerides, blood pressure, and arthritis.
-Inflammatory
-Anti-inflammatory
-Induction of labor
-Smooth muscle contraction
-Asthma relief
*affects ocular tissues
How do non-steroidal anti-inflammatory drugs (NSAIDs) like asprin work?
act by down regulating Eicosanoids synthesis
-remember omega-6 (ω-6) EFAs derived Eicosanoids are pro-inflammatory
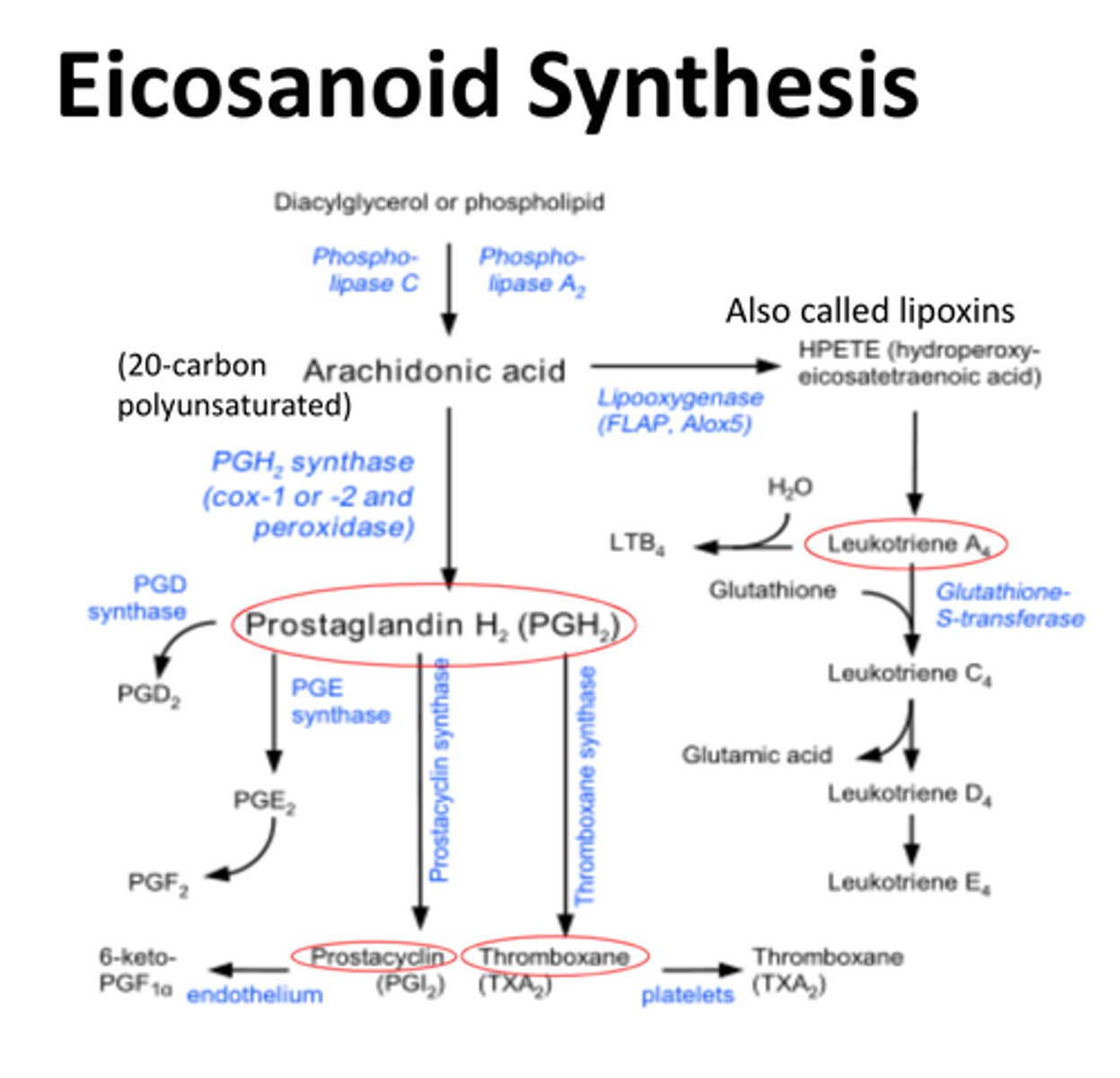
4 families of Eicosanoids
-Prostaglandins
-Prostacyclins
-Thromboxanes
-Leukotrienes
-For each, there are two or three separate
series, derived either from an ω-3 or ω-6 EFA.
-These series' different activities largely explain the health effects of ω-3 and ω-6 fats
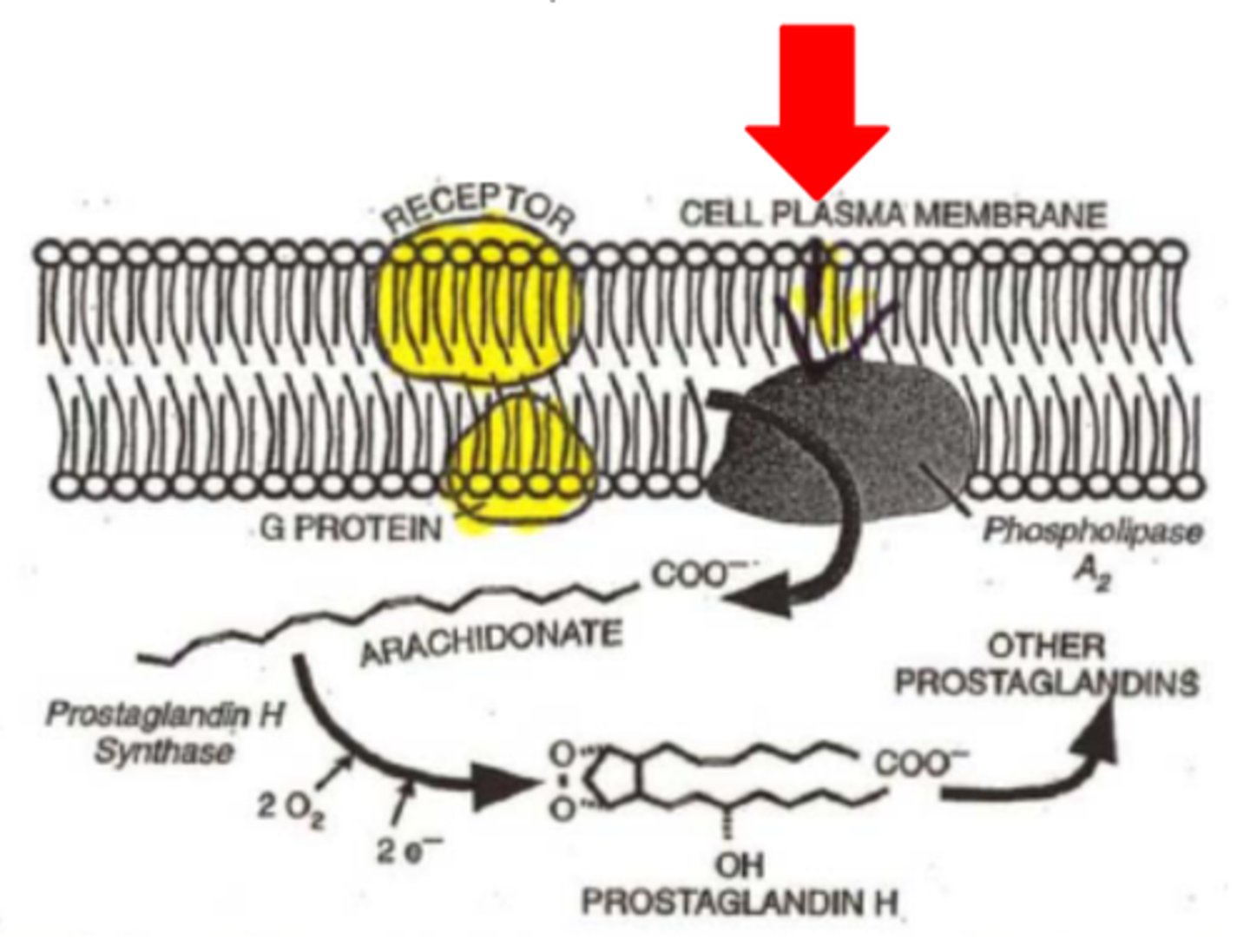
synthesis of Eicosanoids depends on 4 enzymes:
1. Phospholipase A2 (in plasma membrane)
2. Prostaglandin H synthase (membrane associated)
-Cycloocygenase (COX)
-peroxidase
(Separate Pathway)
3. 12- Lipoxygenase
4. 5- Lipoxygenase
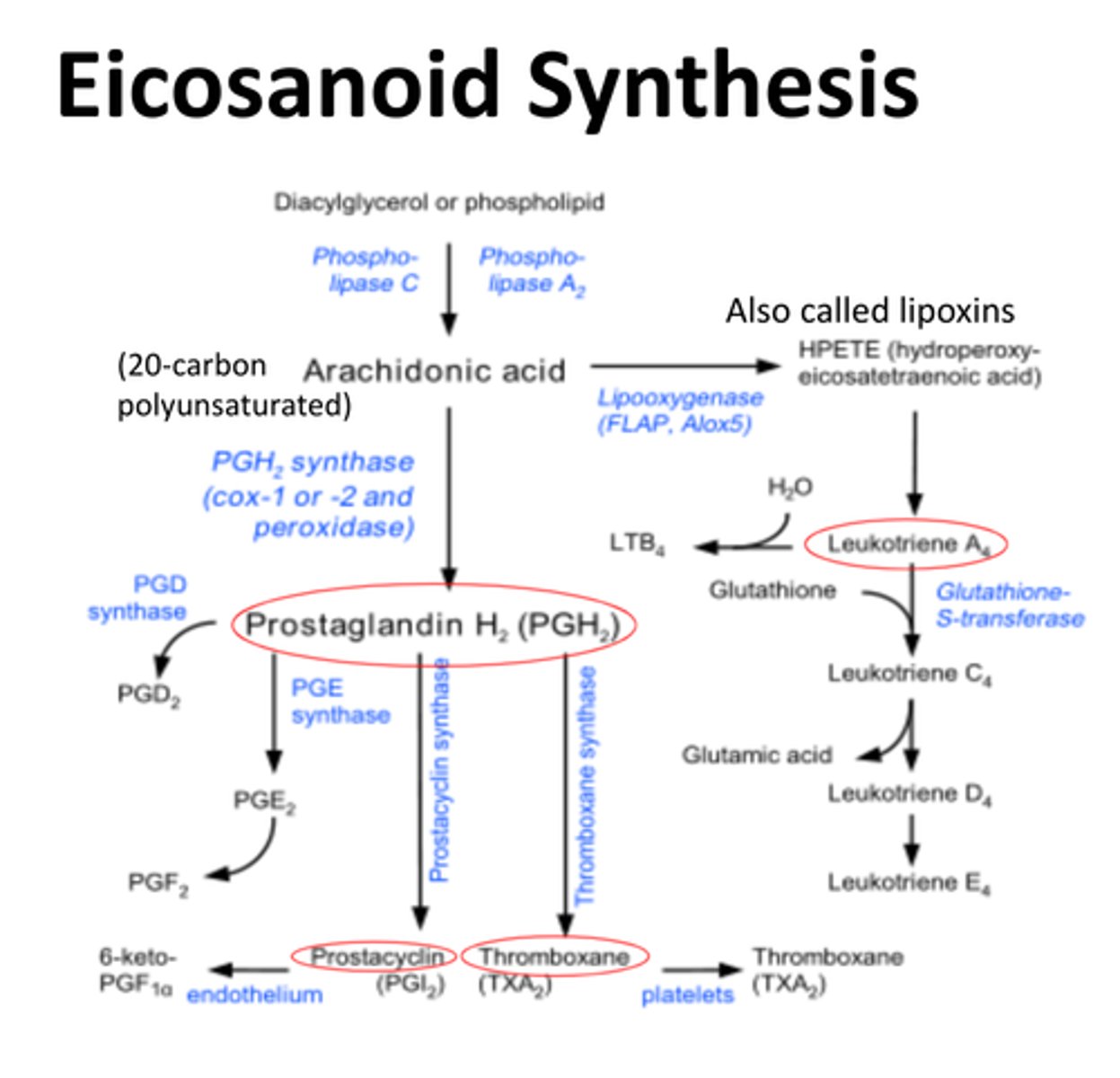
Pathway for synthesis of Prostacylin
1. diacylglycerol or phospholipid converted to Arachidonic acid by Phospholipase A2
3. Arachidonic acid converted to prostaglandin H2 (PGH2) by Prostaglandin H synthase (COX or peroxidase)
4. prostaglandin H2 converted to Prostacylin by prostacylin synthase
5. goes to endothelium
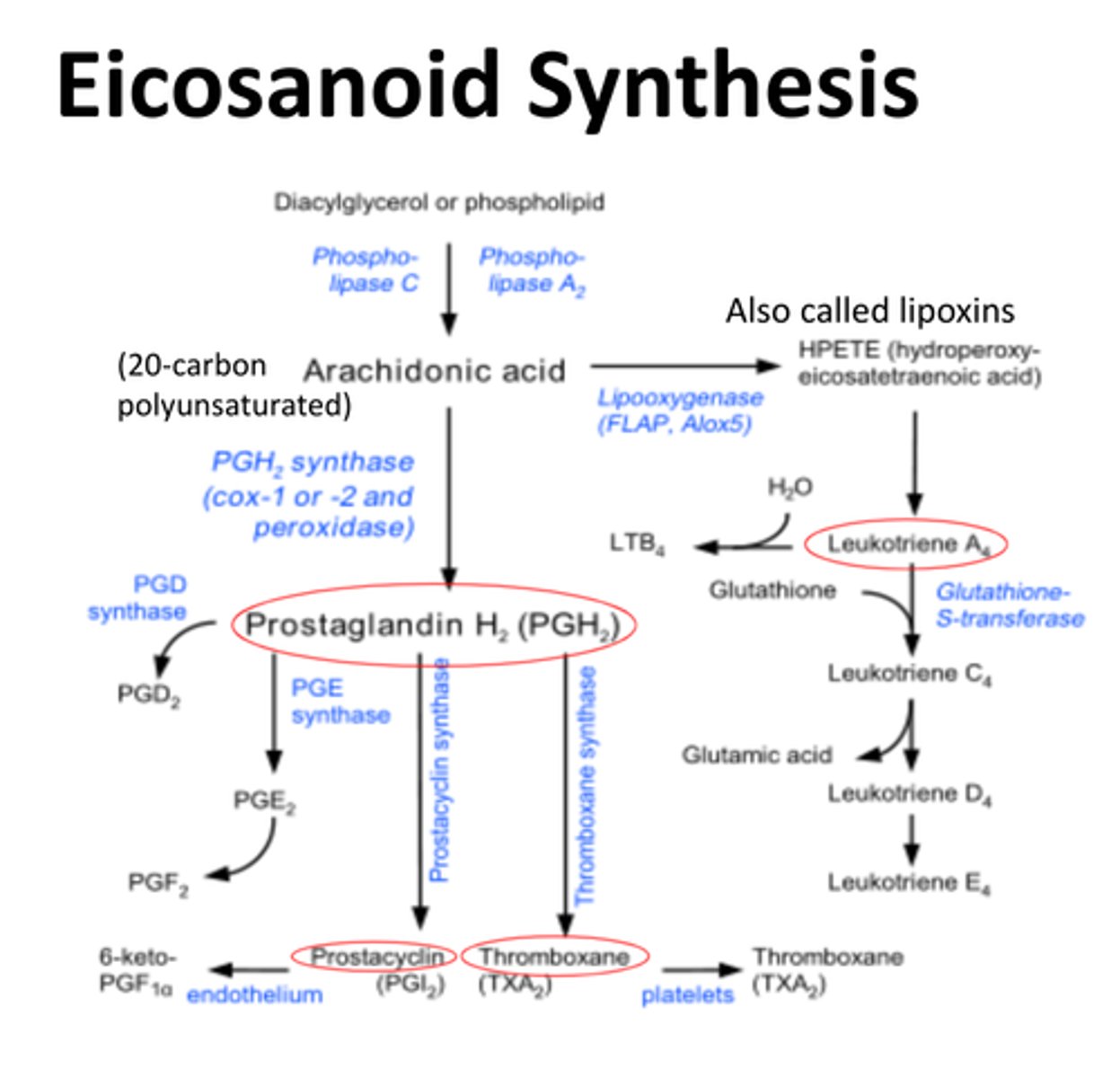
Pathway for synthesis of Thromboxanes
1. diacylglycerol or phospholipid converted to Arachidonic acid by Phospholipase A2
3. Arachidonic acid converted to prostaglandin H2 (PGH2) by Prostaglandin H synthase (COX or peroxidase)
4. prostaglandin H2 converted to thromboxane by thromboxane synthase
5. goes to platelets
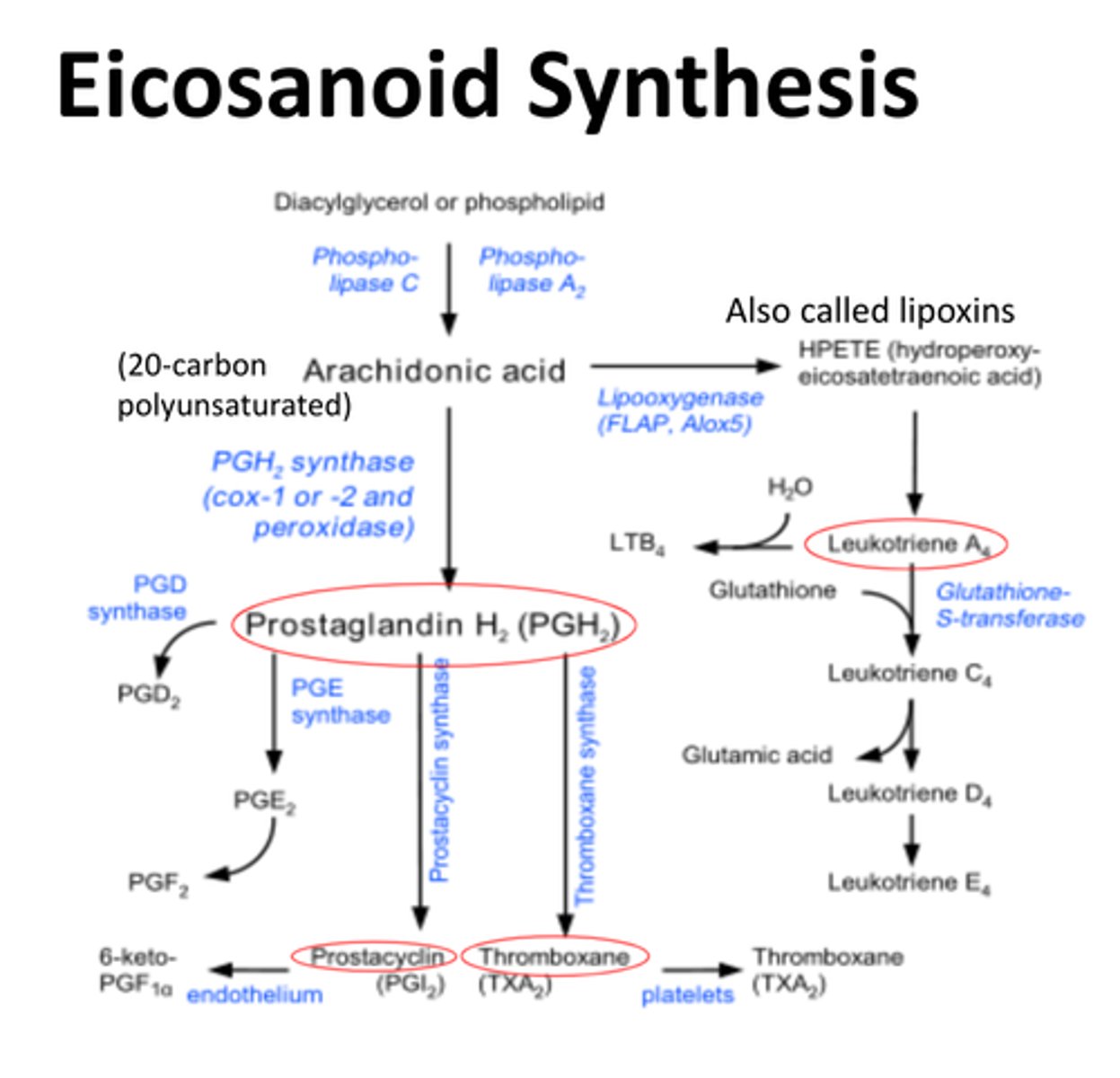
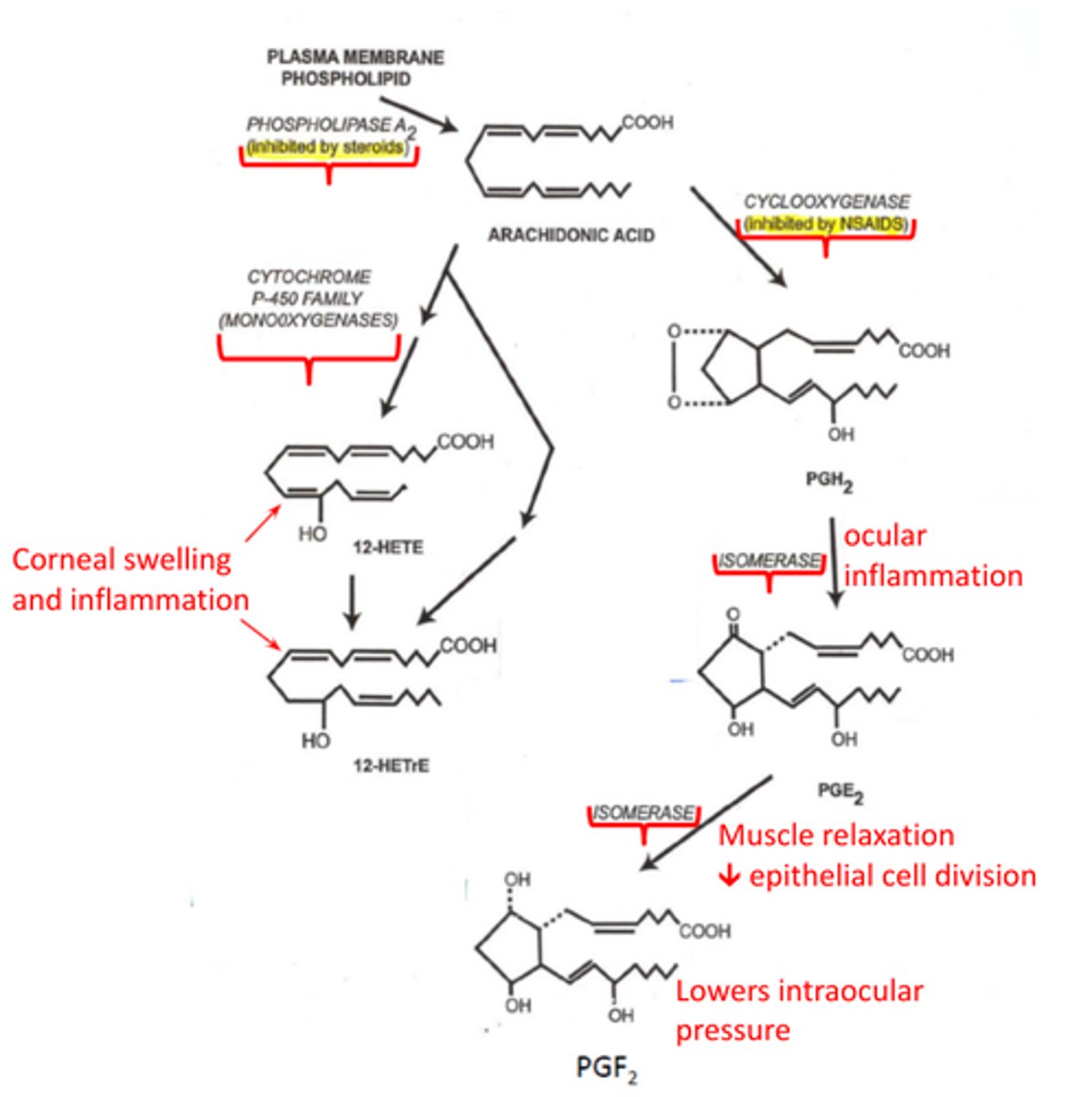
Pathway for synthesis of prostaglandins PGE2 & PGF2
1. diacylglycerol or phospholipid converted to Arachidonic acid by Phospholipase A2
3. Arachidonic acid converted to prostaglandin H2 (PGH2) by Prostaglandin H synthase (COX)
3. ocular inflammation happens, isomerase converts PGH2 to PGE2 (causes muscle relaxation & decrease in epithelial cell division)
4. isomerase then converts PGE2 to PGF2 (lowers IOP)
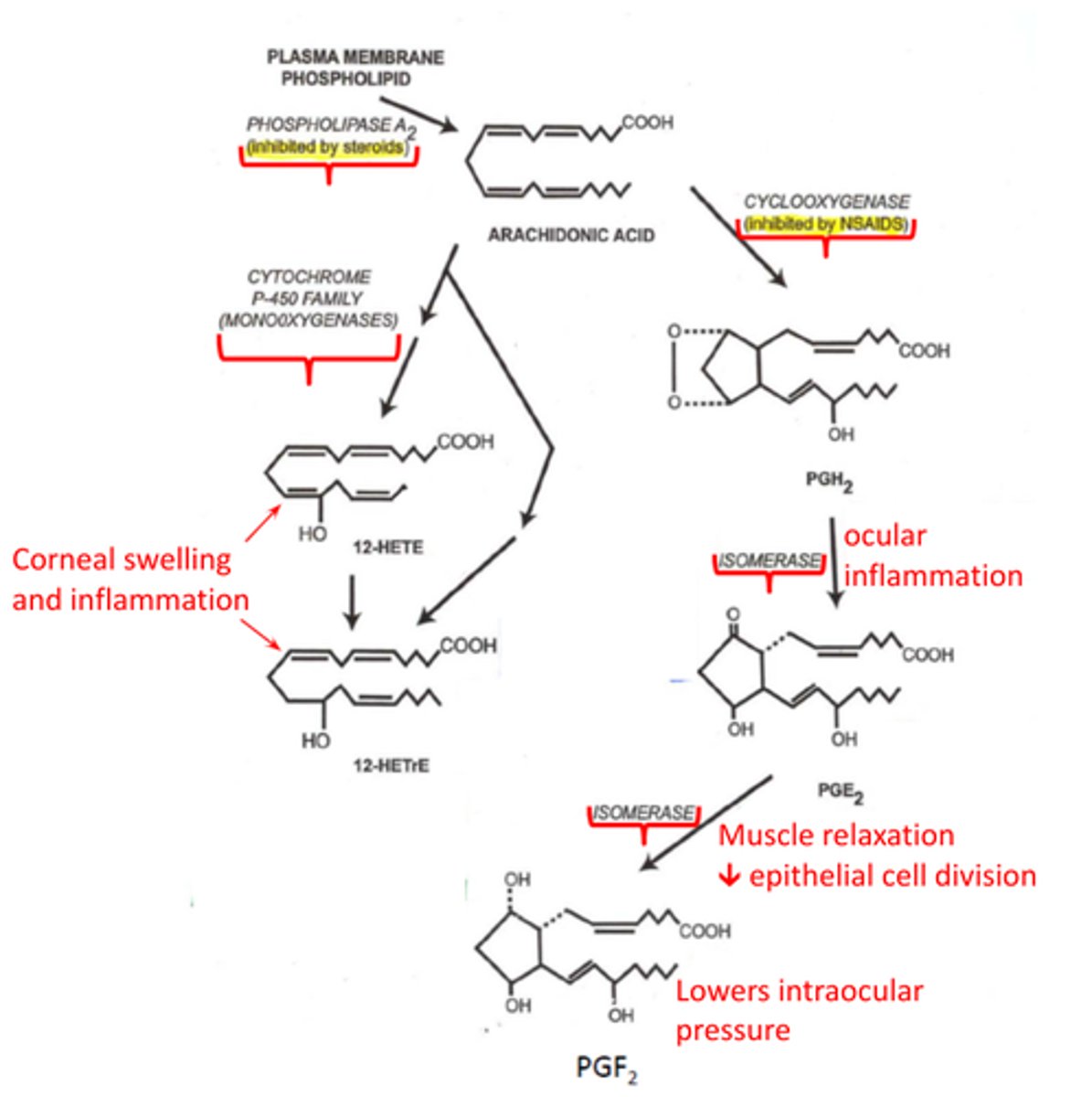
How does PGE2 affect the eye
causes muscle relaxation & decrease in epithelial cell division
How does PGF2 affect the eye
lowers IOP
Pathway for synthesis of Leukotrienes
1. diacylglycerol or phospholipid converted to Arachidonic acid by Phospholipase A2
2. Arachidonic acid is converted to lipoxins hydroperoxyeicosatetraenoic acid (HPETE) by lipoxygenase
3. HPETE converted to leukotriene A2
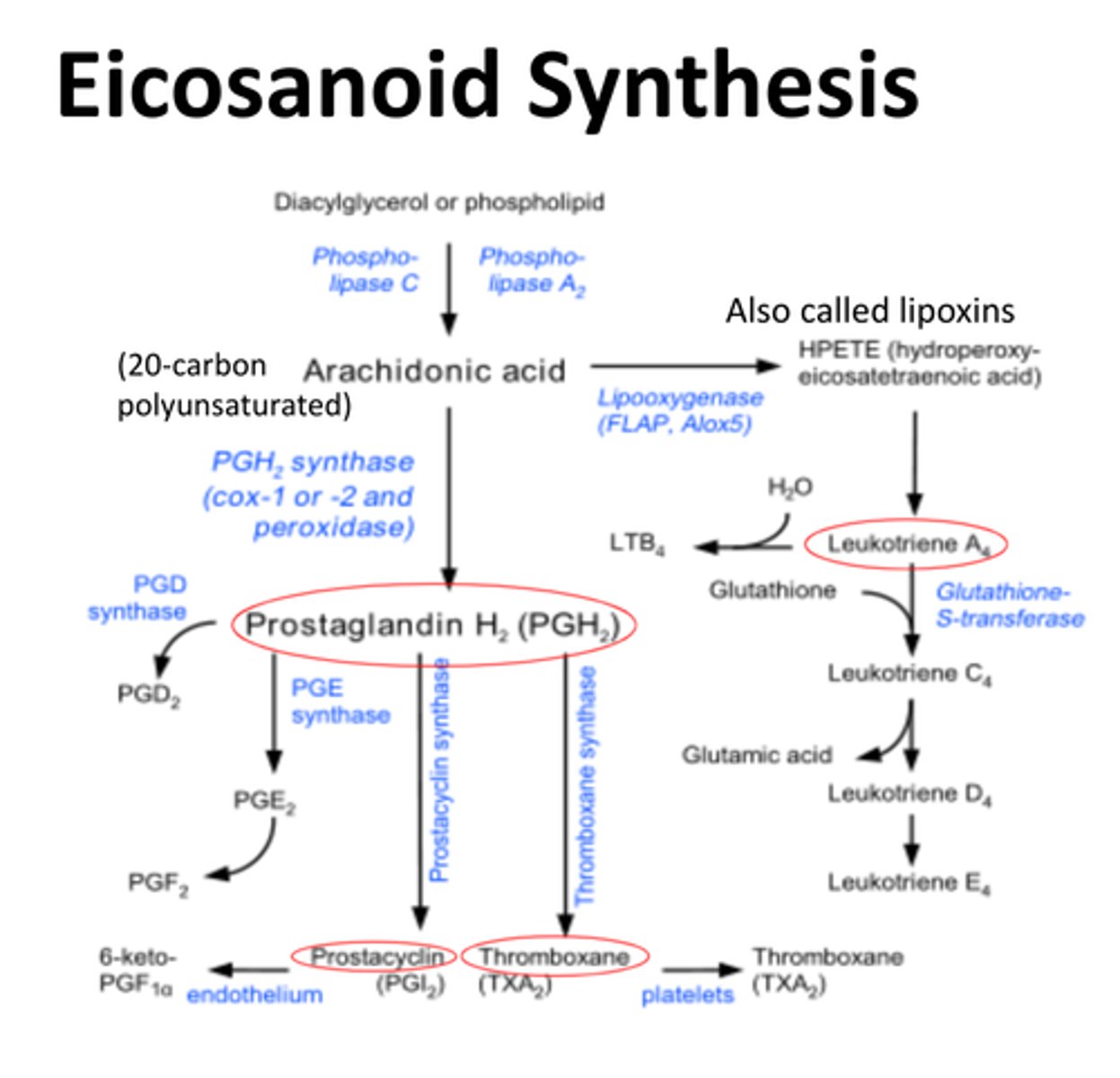
What enzyme in Eicosanoid synthesis is inhibited by steroids?
Phospholipase A2
-completely blocks Eicosanoid synthesis by preventing Diacylglycerol or phospholipid conversion to arachidonic acid
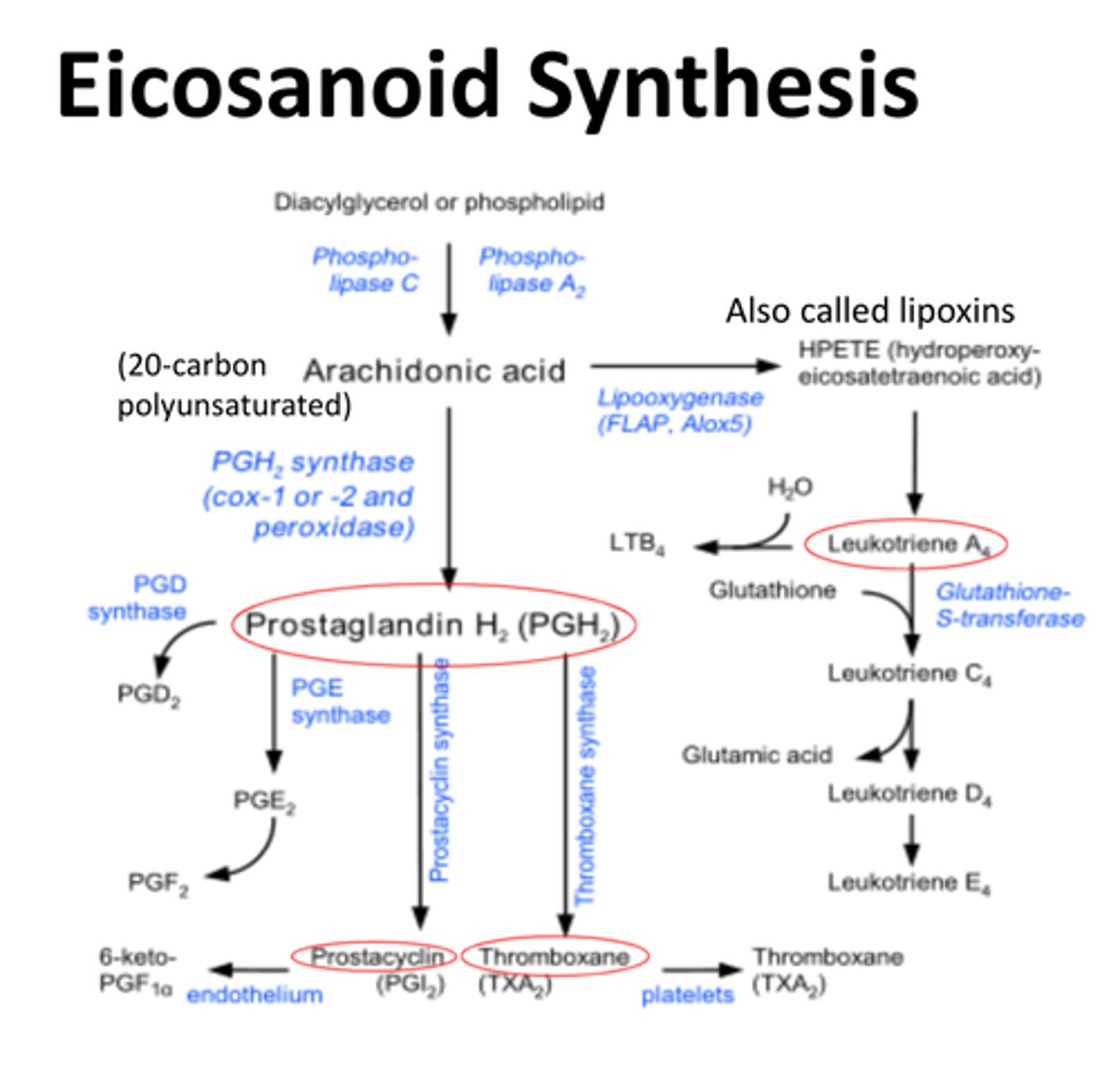
What enzyme in Eicosanoid synthesis is inhibited by NSAIDs and asprin?
Prostaglandin H synthase
-prevents conversion of arachidonic acid to Prostaglandin H2 (PGH2)
12 (R)-HETE
-inhibits Na+/K+ ATPase in the corneal endothelium
-mediates corneal swelling & inflammation
1. diacylglycerol or phospholipid converted to Arachidonic acid by Phospholipase A2
2. Arachidonic acid is converted to either
HETE = hydroxyeicosatetraenoic acid
HETrE = hydroxyeicosatrienoic acid
by cytochrome P-450 family monooxygenases
What activates Phospholipase A2?
-optional
-receptor protein/G protein
-mechanical pressure/injury