EKG CMA Review
0.0(0)
Card Sorting
1/103
Last updated 5:34 PM on 3/10/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
104 Terms
1
New cards
Circulation
superior & inferior venal cava→ right atrium → tricuspid valve → right ventricles → pulmonary valve → pulmonary arteries → lungs gas exchange →pulmonary veins → left atrium → bicuspid valve → left ventricles → aortic valve → aorta → arteries → arteroles → arteriol capillaries →gas exchange → venous capillaries → venules → veins → superior and inferior venal cava
2
New cards
Pathways for Conduction
SA node → AV node → Bundle of His → Bundle Branches → Purkinje fibers → interventricular septum → left bundle branch → right bundle branch → apex
3
New cards
SA node
Located in upper right portion of right atrium
initiates the heartbeat
pacemaker of the heart (60-100 bpm)
normal conduction begins in SA node
initiates the heartbeat
pacemaker of the heart (60-100 bpm)
normal conduction begins in SA node
4
New cards
AV node
located on the floor of the right atrium
causes delay in the electrical impulse, allowing for blood to travel to ventricles
Can act as pacemaker if SA node is not working (40-60
bpm)
causes delay in the electrical impulse, allowing for blood to travel to ventricles
Can act as pacemaker if SA node is not working (40-60
bpm)
5
New cards
Bundle of His (AV bundle)
Located next to the AV node
Transfers electrical impulses from the atria to the
ventricles via bundle branches
Transfers electrical impulses from the atria to the
ventricles via bundle branches
6
New cards
Bundle Branches
Split the electrical impulse down the right and left side
From interventricular septum, the impulse activates
myocardial tissue, causing contraction
Contractions occur in left-to-right pattern
From interventricular septum, the impulse activates
myocardial tissue, causing contraction
Contractions occur in left-to-right pattern
7
New cards
Purkinje Fibers
Electrical pathway for each cardiac cell
Impulse activates left and right ventricles simultaneously
Produce an electrical wave
Impulse activates left and right ventricles simultaneously
Produce an electrical wave
8
New cards
unique qualities of the heart
Automaticity- heart’s ability to generate an electrical impulse
Conductivity-ability of myocardial cells to receive and conduct electrical impulses
Contractivity- ability of the heart muscle to shorten in response to an electrical impulse
Excitability-ability of the heart to respond to an impulse or stimulus
Conductivity-ability of myocardial cells to receive and conduct electrical impulses
Contractivity- ability of the heart muscle to shorten in response to an electrical impulse
Excitability-ability of the heart to respond to an impulse or stimulus
9
New cards
Autonomic Nervous System
Speeds up or slows down the heart rate
\
Sympathetic branch can increase the heart rate (norepinephrine)
\
Parasympathetic branch can decrease the heart rate (vagus nerve)
\
Sympathetic branch can increase the heart rate (norepinephrine)
\
Parasympathetic branch can decrease the heart rate (vagus nerve)
10
New cards
Depolarization
State of stimulation, preceding contraction
Electrical activation of heart cells
Causes the heart to contract
Most important electrical event
Electrical activation of heart cells
Causes the heart to contract
Most important electrical event
11
New cards
Repolarization
State of cellular recovery, following contraction
Cell returns to a resting state
Heart relaxes, allowing for refilling of the chambers
Cell returns to a resting state
Heart relaxes, allowing for refilling of the chambers
12
New cards
EKG Waveform
Standardized graph paper used
Paper runs at a standard speed of 25mm/second
Normal amplitude is 10 mm or 1 mv
Paper runs at a standard speed of 25mm/second
Normal amplitude is 10 mm or 1 mv
13
New cards
P Wave
First positive deflection
Occurs when the atria depolarize
Small compared to other ECG waves
Occurs when the atria depolarize
Small compared to other ECG waves
14
New cards
Q Wave
Represents conduction of impulse down the interventricular septum
First negative deflection before the R wave
Not always visualized on the ECG
Less than 1/4 the height of the R wave
First negative deflection before the R wave
Not always visualized on the ECG
Less than 1/4 the height of the R wave
15
New cards
R Wave
First positive wave of the QRS complex
Represents conduction of electrical impulse to the left ventricle
Usually easiest to find
Represents conduction of electrical impulse to the left ventricle
Usually easiest to find
16
New cards
S wave
First negative deflection after the R wave
Represents conduction of electrical impulse through both ventricles
Represents conduction of electrical impulse through both ventricles
17
New cards
QRS complex
Represents complete ventricular depolarization
18
New cards
ST segment
Indicates end of ventricular depolarization and beginning of ventricular repolarization
Elevated ST segment indicates myocardial damage (ischemia-reduced oxygen to heart muscle) - STEMI
Elevated ST segment indicates myocardial damage (ischemia-reduced oxygen to heart muscle) - STEMI
19
New cards
T wave
Represents ventricular repolarization
20
New cards
U wave
Represents repolarization of Bundle of His and Purkinje fibers
Presence can indicate an electrolyte imbalance
Presence can indicate an electrolyte imbalance
21
New cards
PR interval
Measured from beginning of P wave to beginning of QRS complex
the time that the electrical impulse is initiated until the ventricles are stimulated by the impulse to start the contraction.
the time that the electrical impulse is initiated until the ventricles are stimulated by the impulse to start the contraction.
22
New cards
QT interval
Time required for ventricular depolarization and
repolarization to occur
repolarization to occur
23
New cards
R to R interval
Measurement of time from start of one QRS complex to start of next QRS complex
Used to calculate heart rate
Readily seen on ECG
Used to calculate heart rate
Readily seen on ECG
24
New cards
Electrocardiogram
machine that records and electrocardiogram
12 views (12-lead) of the heart at once
10 wires are attached to the body
12 views (12-lead) of the heart at once
10 wires are attached to the body
25
New cards
Telemetry
constant monitoring of the patient in a hospital setting
26
New cards
Stress Testing
Must have emergency equipment available during testing
Patient is attached to the EKG while exercising (bike or treadmill) to see how the heart handles the stress
Thallium can be used for patients that cannot exercise
CMA role – attach leads, monitor v/s
Patient is attached to the EKG while exercising (bike or treadmill) to see how the heart handles the stress
Thallium can be used for patients that cannot exercise
CMA role – attach leads, monitor v/s
27
New cards
Stress Testing pt edu
Wear comfortable walking shoes
Wear a separate shirt and pants – to access chest for leads
\
Take regular medications the day of stress test
Do not eat a large meal prior to the test
Wear a separate shirt and pants – to access chest for leads
\
Take regular medications the day of stress test
Do not eat a large meal prior to the test
28
New cards
Holter Monitor
Patient will wear monitor for 24 hours or more (as ordered by provider)
Holter records all EKG activity for that time period
Patient will press a button when symptomatic (syncope, pain, palpitations) and keep a diary of all activity
CMA role – attach leads, patient education
Holter records all EKG activity for that time period
Patient will press a button when symptomatic (syncope, pain, palpitations) and keep a diary of all activity
CMA role – attach leads, patient education
29
New cards
Holter Monitor pt edu
Do not remove or replace electrodes
Do not shower or get device wet
Avoid exposure to electrical forces such as metal detectors
Conduct normal activities while wearing
Return at designated time for removal
Do not shower or get device wet
Avoid exposure to electrical forces such as metal detectors
Conduct normal activities while wearing
Return at designated time for removal
30
New cards
Preparing the pt
Patient removes clothing from the waist up
Provide with drape, sheet, or hospital gown with \n opening in the front
Patient removes jewelry that may interfere
All electronic devices should be turned off and \n removed
Position patient comfortably on back and provide pillow for head and knees, if preferred
Work from patient’s left side if possible
Ensure privacy
Ensure that arms and legs are supported
Place patient in semi-Fowler’s position if SOB
Provide sheet or blanket to prevent chills
Make sure bed/exam table is not touching wall or \n electrical equipment
Ensure that patient is not touching metal
Make sure there is plenty of paper in machine
Provide with drape, sheet, or hospital gown with \n opening in the front
Patient removes jewelry that may interfere
All electronic devices should be turned off and \n removed
Position patient comfortably on back and provide pillow for head and knees, if preferred
Work from patient’s left side if possible
Ensure privacy
Ensure that arms and legs are supported
Place patient in semi-Fowler’s position if SOB
Provide sheet or blanket to prevent chills
Make sure bed/exam table is not touching wall or \n electrical equipment
Ensure that patient is not touching metal
Make sure there is plenty of paper in machine
31
New cards
Verification
Patient name/date of birth
Location/date/time of recording
Patient age/sex/race/cardiac medications
Height and weight
Reason for exam
Location/date/time of recording
Patient age/sex/race/cardiac medications
Height and weight
Reason for exam
32
New cards
Communication
Identify the patient
Check the patient name, identification number, and \n date of birth (two forms of identification)
Introduce yourself and explain what you are going to \n do
Answer all questions
If the patient refuses the ECG, determine the cause. \n Let them know that there is no “electricity”. It is like a \n photo.
Notify your provider if you cannot resolve the problem
Check the patient name, identification number, and \n date of birth (two forms of identification)
Introduce yourself and explain what you are going to \n do
Answer all questions
If the patient refuses the ECG, determine the cause. \n Let them know that there is no “electricity”. It is like a \n photo.
Notify your provider if you cannot resolve the problem
33
New cards
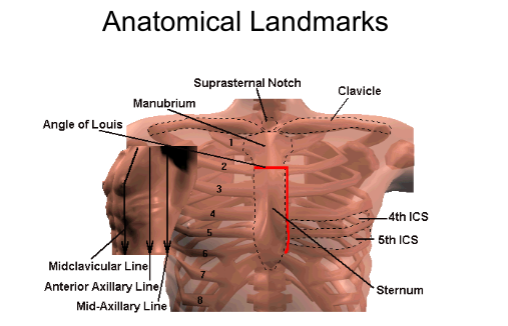
Anatomical Landmarks
Midclavicular Line- Usually starts in the center of clavicle and passes through nipple line
also there’s : Anterior axillary line, Mid-axillary line, ntercostal spaces (ICS), Suprasternal notch, Angle of Louis
also there’s : Anterior axillary line, Mid-axillary line, ntercostal spaces (ICS), Suprasternal notch, Angle of Louis
34
New cards
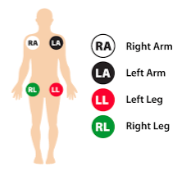
Limb Leads
Place on fleshy areas in same general vicinity (amputations, etc.)
Sky (white) over grass (green)
Smoke (black) over fire (red)
Sky (white) over grass (green)
Smoke (black) over fire (red)
35
New cards
Bipolar leads
Leads I, II, and III are bipolar – records impulses that travel from a negative to positive pole
36
New cards
Unipolar leads
AVL, AVR, and AVF – unipolar
37
New cards
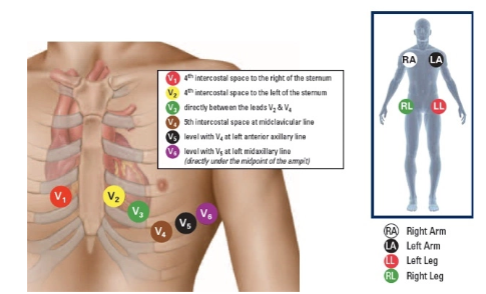
Precordial Leads
Precordial leads – located on the chest in \\n front of the heart
V1, V2, V3, V4, V5, V6
V1, V2, V3, V4, V5, V6
38
New cards
Where V1-V6 are placed
V1 - V2 - V4 - V3 - V5 - V6
39
New cards
Applying the Electrodes
Prep the skin with either an alcohol swab or electrolyte pad
Shave hair if necessary, or clip hair for continuous \n monitoring
*FOR FEMALES*
lift left breast and place electrodes in \n closest position possible. Do NOT place electrodes on \n top of breast tissue
Non-standard location of electrodes must be \n documented on recording
Shave hair if necessary, or clip hair for continuous \n monitoring
*FOR FEMALES*
lift left breast and place electrodes in \n closest position possible. Do NOT place electrodes on \n top of breast tissue
Non-standard location of electrodes must be \n documented on recording
40
New cards
Limb electrodes
Place on wrists or upper arms and inside of lower \n legs. Location of left and right leads must match.
*Alternate site*: shoulders (deltoid), upper legs, lower \n abdomen
*Alternate site*: shoulders (deltoid), upper legs, lower \n abdomen
41
New cards
Troubleshooting
P: Electrodes will not stick
S: Cleanse skin with alcohol pads and pat dry and/or clip or shave hair from the site only if necessary
S: Cleanse skin with alcohol pads and pat dry and/or clip or shave hair from the site only if necessary
42
New cards
Applying the leads
*Chest leads* = Electrode tabs point toward feet
*limb leads* = Arm electrode tabs point toward feet and Leg electrode tabs point toward hands
*limb leads* = Arm electrode tabs point toward feet and Leg electrode tabs point toward hands
43
New cards
Safety and Infection control
Follow universal precautions
Wash your hands
Wear gloves when exposure to blood or bodily fluids is \n likely
Make sure the procedure is performed on the correct \n patient
Raise bed rail if available
Pull out extension for legs and feet if using an exam \n table
Check grounding plug for security
Ensure that bed or table is not touching wall or electrical equipment
Ensure that patient is not touching bed rail, exam table frame or safety rail
Check insulation wires for cracks
Wash your hands
Wear gloves when exposure to blood or bodily fluids is \n likely
Make sure the procedure is performed on the correct \n patient
Raise bed rail if available
Pull out extension for legs and feet if using an exam \n table
Check grounding plug for security
Ensure that bed or table is not touching wall or electrical equipment
Ensure that patient is not touching bed rail, exam table frame or safety rail
Check insulation wires for cracks
44
New cards
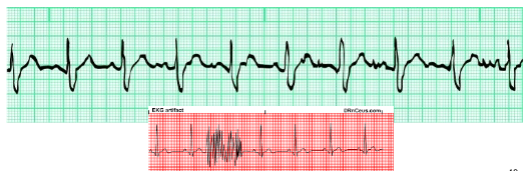
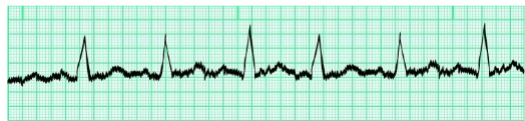
Artifacts (somatic tremor)
Large spikes caused by muscle movement
Causes: shivering, muscle tension, pain, fear, talking, \n chewing gum, disorders such as Parkinson’s disease.
Causes: shivering, muscle tension, pain, fear, talking, \n chewing gum, disorders such as Parkinson’s disease.
45
New cards
Artifacts (wandering baseline)
AKA baseline shift
Usually caused by improper electrode application. \n Can also be caused by poor skin prep, pulling on \n electrodes, old electrodes or clips, oil, lotion, dried out \n electrodes
Usually caused by improper electrode application. \n Can also be caused by poor skin prep, pulling on \n electrodes, old electrodes or clips, oil, lotion, dried out \n electrodes

46
New cards
Artifacts (AC interference)
Small, uniform spikes caused by electricity radiated \n from other machines
Common sources include improper grounding, lead \n wires crossed, corroded or dirty electrodes
Common sources include improper grounding, lead \n wires crossed, corroded or dirty electrodes
47
New cards
Other interrrupted baselines
Loose or unplugged lead
Switched wires
Broken wires
Switched wires
Broken wires
48
New cards
How to calculate the heart rate
ONLY method that can be used with an irregular rhythm
Multiply the number of complexes by 10
Do not count incomplete complexes
Multiply the number of complexes by 10
Do not count incomplete complexes
49
New cards
Reporting Results
Follow your facility’s policy
Make copy, if required
Fax tracing, if required
if ordered stat, immediately give tracing to your provider
Make copy, if required
Fax tracing, if required
if ordered stat, immediately give tracing to your provider
50
New cards
Equipment
Keep machine clean to prevent infection and present \n professional image
For disposable electrodes, clean alligator clips and \n check for paste/gel
Disinfect cables and reusable electrodes
Wash straps; replace cracked/broken straps
Wash reusable electrodes to prevent gel/paste buildup
Scour reusable electrodes once a week
Wipe patient cables and lead wires with damp cloth
Replace cracked or broken wires
Store neatly
For disposable electrodes, clean alligator clips and \n check for paste/gel
Disinfect cables and reusable electrodes
Wash straps; replace cracked/broken straps
Wash reusable electrodes to prevent gel/paste buildup
Scour reusable electrodes once a week
Wipe patient cables and lead wires with damp cloth
Replace cracked or broken wires
Store neatly
51
New cards
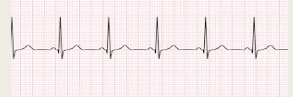
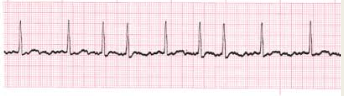
NSR (normal sinus rhythm)
All measurements are within normal limits
The rate is between 60 – 100 bpm
There is a P wave indicating that the rhythm started in the SA node (sinus)
The rate is between 60 – 100 bpm
There is a P wave indicating that the rhythm started in the SA node (sinus)
52
New cards
Arrhythimas
AKA dysrhythmia
A change from normal sinus rhythm
Can be rate, appearance, or conduction problems
A change from normal sinus rhythm
Can be rate, appearance, or conduction problems
53
New cards
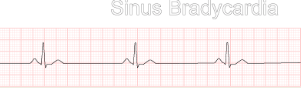
SInus Bradycardia
Sinus rhythm – normal P wave present, other measurements WNL
Rate
Rate
54
New cards
Sinus Tachycardia
Sinus rhythm – normal P wave and other measurements WNL
Rate > 100 bpm
Rate > 100 bpm

55
New cards
Sinus Dysrhythmia
Sinus rhythm – P wave present, other measurements WNL
Slight irregularity in rhythm – usually associated with breathing patterns
Slight irregularity in rhythm – usually associated with breathing patterns

56
New cards
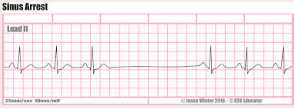
SInus Arrest
Normal Sinus Rhythm when complexes are present – consistent pattern
A break in the pattern is sinus arrest
The SA node fails to fire
Not significant unless lasts longer than 6 seconds
A break in the pattern is sinus arrest
The SA node fails to fire
Not significant unless lasts longer than 6 seconds
57
New cards
Atrial Flutter
Atria are contracting at a rapid rate –much faster than the ventricles are contracting
Sawtooth appearance of “F” waves (may look like P waves)
Consistent ratio (ex. 4 F waves to 1 QRS)
Regular rhythm - pulse
Sawtooth appearance of “F” waves (may look like P waves)
Consistent ratio (ex. 4 F waves to 1 QRS)
Regular rhythm - pulse
58
New cards
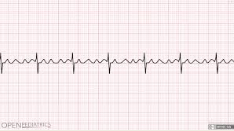
Atrial Fibrillation (A-fib)
No organized contraction of the atria
Quivering state
Blood clots can develop due to stagnation of blood
Irregular rhythm and pulse
Quivering state
Blood clots can develop due to stagnation of blood
Irregular rhythm and pulse
59
New cards
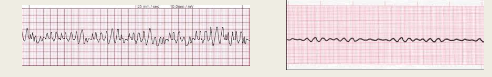
Ventricular Fibrillation
OMG rhythm! \n Immediate intervention needed – no pulse being generated – begin CPR
Patient will NOT be conscious
Ventricles are quivering – no wave forms on EKG \n Needs defibrillation (AED)
Patient will NOT be conscious
Ventricles are quivering – no wave forms on EKG \n Needs defibrillation (AED)
60
New cards
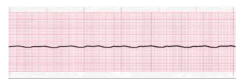
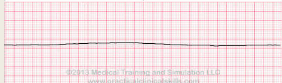
Asystole
OMG rhythm!
No heart electrical activity or pulse
Heart has stopped – Begin CPR
Patient will NOT be conscious. If talking, check your cables.
No heart electrical activity or pulse
Heart has stopped – Begin CPR
Patient will NOT be conscious. If talking, check your cables.
61
New cards
Junctional Dysrhythmia
Negative P-waves indicate a Junctional Rhythm
The impulse is generated in the AV node instead of the SA node.
Junctional rhythms may not have a P-wave at all
Rate is often between 40-60 bpm
The impulse is generated in the AV node instead of the SA node.
Junctional rhythms may not have a P-wave at all
Rate is often between 40-60 bpm

62
New cards
Premature Ventricular Contractions (PVC)
If the QRS is “wide and bizarre”, suspect a ventricular arrhythmia.
Occasional PVC’s are common and can be insignificant. Usually asymptomatic.
Can occur in pairs, be unifocal, multifocal, or occur in runs
Notify provider if PVC noted on EKG
Occasional PVC’s are common and can be insignificant. Usually asymptomatic.
Can occur in pairs, be unifocal, multifocal, or occur in runs
Notify provider if PVC noted on EKG
63
New cards
Anemia (blood diseases & treament)
an inadequate number of red blood cells
64
New cards
aplastic anemia
destruction of bone marrow
65
New cards
sickle cell anemia
chronic genetic anemia
66
New cards
Aneurysm
ballooning out of saclike on the wall of the artery
67
New cards
Arteriosclerosis
hardening of the walls of an artery
68
New cards
Atherosclerosis
Fatty plaques, cholesterol deposited on the walls of arteries
69
New cards
Atherectomy
a balloon is inserted in the vessel, a cutting tool used to clear plaque
70
New cards
CABG (Coronary artery bypass graft)
vein from the leg is implanted on the heart to bypass a blockage in the coronary artery
71
New cards
Congestive heart failure
Heart muscles cannot pump adequately to meet the needs of the body
Treatment: cardiac drugs and diuretics
Treatment: cardiac drugs and diuretics
72
New cards
Embolis
a foreign substance in the blood stream
73
New cards
Hemophilia
Inability to effectively form clots in the blood
74
New cards
High blood pressure
systolic pressure above 140-150
diastolic pressure above 90
diastolic pressure above 90
75
New cards
Angina
narrowing of the coronary arteries which causes ischemia
76
New cards
Nitroglycerin
treats angina
77
New cards
Myocardial infraction
heart attack
78
New cards
Phlebitis
inflammation of the vein, usually the leg
79
New cards
Varicose veins
dilated swollen veins that have lost elasticity
80
New cards
Productive cough (respiratory diseases & treatments)
wet cough
81
New cards
**Nonproductive cough**
dry hacking
Treatments for coughs: Antitussives, expectorants
Treatments for coughs: Antitussives, expectorants
82
New cards
**COPD**
**chronic obstructive pulmonary disease aka asthma**
83
New cards
**chronic bronchitis**
inflammation of the bronchi and bronchial tubes persisting over a long time
84
New cards
Emphysema
enlargement of the alveoli and progressive loss of lung function due to destruction of the alveoli
85
New cards
SRS (smoker’s respiratory syndrome
damage caused by smoking that causes chronic symptoms like coughing, wheezing, hoarseness, difficult breathing, and infections
86
New cards
Epistaxis
Nosebleed
87
New cards
Influenza (flu)
highly contagious viral disease
88
New cards
Laryngitis
inflammation of larynx and vocal cord
89
New cards
lung cancer
mainly due to smoking
90
New cards
Pleurisy
inflammation of the pleura
91
New cards
Pneumonia
inflammation/infection of the lung with fluid in the alveoli
92
New cards
Rhinitis
inflammation of the nasal mucous membrane
93
New cards
Sinusitis
inflammation of the mucous membrane of the sinuses
94
New cards
Upper respiratory infection (URI)
aka common cold
inflammation of the mucous membranes of the respiratory tract
inflammation of the mucous membranes of the respiratory tract
95
New cards
Pertussis
whooping cough
96
New cards
Atelectasis
partial or complete collapse of the lung due to the alveoli becoming deflated or filled with fluid
97
New cards
Bronchitis
inflammation of the lining of the bronchial tubes
98
New cards
Legionnaires’ disease
severe form of pneumonia by a bacteria called legionella
99
New cards
Pulmonary edema
excess fluid in the lungs
100
New cards
Pulmonary embolism
A blockage in one of the pulmonary arteries in the lungs