~Documentation for Geriatric Practice
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Importance of Documentation
***understand current documentation requirements and their impact on reimbursement
Identify the need for skilled therapy services
what we’re doing and why
Crucial for payment decisions and continuation of therapy services if needed
Communication with other professionals
Billing Codes: ICD-10 Codes
ICD-10 refers to the tenth edition of the International Classification of Diseases, which is a medical coding system chiefly designed by the World Health Organization (WHO) to catalog health conditions by categories of similar diseases under which more specific conditions are listed, thus mapping nuanced diseases to broader morbidities
ICD-10-CM diagnosis codes used in occupational therapy represent a client’s medical and treatment diagnoses; these codes are a uniform method of sharing information regarding a client’s condition and deficits with interdisciplinary team members, other providers, and payers
Accuracy with coding ICD-10-CM diagnoses is critical to ensuring the correct information is relayed to others involved in a client’s care
ICD-10 Codes
The US version of ICD-10, created by the Centers for Medicare & Medicaid Services (CMS) and the National Center for Health Statistics (NCHS), consists of two medical code sets—ICD-10-CM and ICD-10-PCS
ICD-10-CM (Clinical Modification) – ***Diagnosis Codes*** (used across all healthcare settings and hospitals)
The ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) is a system used by physicians and other healthcare providers to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States
According to WHO, physicians, coders, health information managers, nurses, and other healthcare professionals also use ICD-10-CM to assist them in the storage and retrieval of diagnostic information
ICD records are also used in the compilation of national mortality and morbidity statistics
ICD-10-PCS (Procedure Classification System) – (Codes used to bill for services in inpatient hospital settings only)
ICD-10-PCS stands for the International Classification of Diseases, Tenth Revision, Procedure Coding System; as indicated by its name, ICD-10-PCS is a procedural classification system of medical codes
It is used in hospital settings to report inpatient procedures
All health care providers who must comply with the Health Insurance Portability and Accountability Act (HIPAA) must use ICD-10 codes to report patient diagnoses
Medical Diagnosis vs. Treatment Diagnosis
Medical Diagnosis:
the medical condition that has led the client to be referred to skilled occupational therapy services; the ICD-10-CM medical diagnosis code represents the disease or medical condition that is causing the client’s symptoms
Often, there is a primary medical diagnosis, as well as comorbidities that might be influencing a client’s occupations
Treatment Diagnosis:
represents the functional limitations or performance deficits impacting the client’s ability to perform desired occupations, resulting from the disease or medical condition identified by the primary medical diagnosis code or comorbidities
OT and Treatment Diagnoses
Therapists should provide an ICD-10-CM treatment diagnosis to indicate the performance deficits for which the client will receive occupational therapy intervention
This diagnosis should be as specific and relevant to the conditions to be treated as possible; therapists must use their clinical judgment to select treatment diagnosis codes that correspond to the client’s condition and most closely reflect the condition for which they are providing intervention (should be as specifc as possible!)
In general, it is not within the occupational therapy scope of practice for OTs to identify a new medical diagnosis, which is usually provided by the physician; although practice acts tend to be broad and you may not see anything specific, the ability to assign a purely medical diagnosis (without physician input) to clients would need to be authorized for occupational therapists in their state practice acts
It’s important to be aware of any state licensure laws related to diagnosis coding
When selecting diagnosis codes, occupational therapists should choose the ICD-10-CM diagnostic codes that identify the greatest level of specificity possible; this means avoiding “unspecified” codes that indicate general conditions but lack clinical details such as site or laterality
e.g., MS: medical diagnosis- given by a physician;
e.g., pain in the right upper arm- treatment diagnosis- given by the OTs
should include laterality
ICD-10 Codes and Reimbursement
***understand current documentation requirements and their impact on reimbursement
When a claim is submitted to a payer, the first thing the payer sees are the ICD-10-CM diagnosis codes; accuracy with coding both the medical and treatment diagnoses can therefore affect whether the payer reimburses the claim
do not use cognitive codes if your patient’s main impairment is physical; this will not be covered/funded (even if they may be having cognitive impairments/need cognitive strategies too)
Both the medical and treatment diagnosis codes are used to support the medical necessity of the occupational therapy services being delivered
The codes tell the payer what is going on with the client and why the occupational therapy services billed on the claim were needed
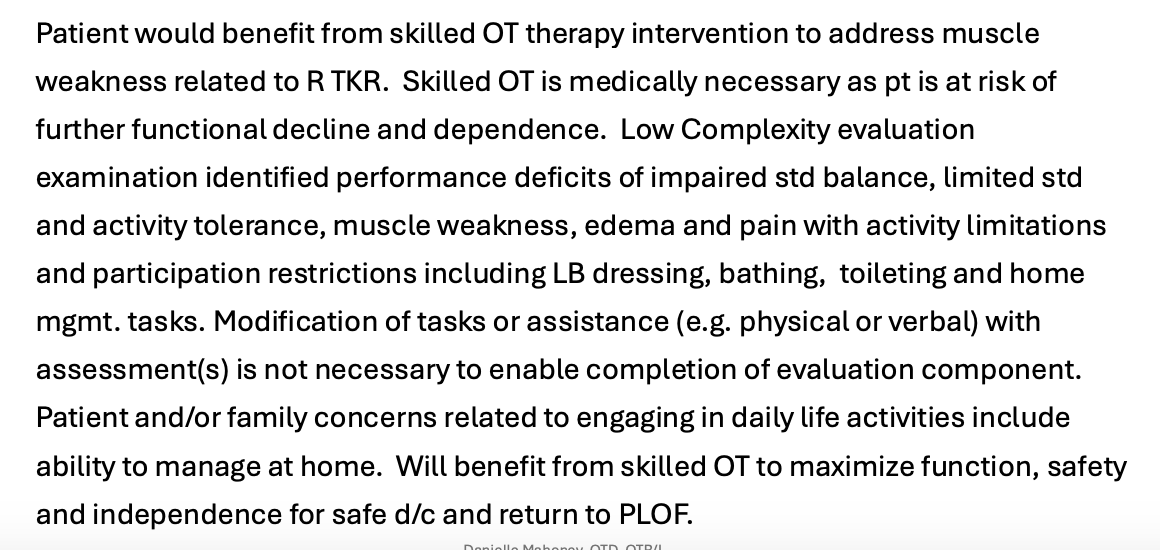
Billing Codes: ICD10 Codes Example
the diagnosis code lists are derived from ICD-10 diagnosis codes that CMS posts each year so that providers and suppliers utilize the applicable diagnosis codes when submitting medical claims to Medicare
don’t memorize; they will change in a year (most likely)!
ICD-10 Codes vs. CPT (Current Procedural Terminology) Codes
For a medical provider to receive reimbursement for medical services, ICD-10-CM codes must be submitted to the payer
While CPT codes depict the services provided to the patient, ICD-10-CM codes depict the patient’s diagnoses that justify the services rendered as medically necessary
ICD-10 provides a diagnosis code to describe the medical issues affecting the patient, while CPT codes indicate the treatment, surgery, or other procedures the patient received
CPT Codes for Occupational Therapy
CPT Codes are owned and copyrighted by the American Medical Association
CMS and Medicare adopted the use of CPT codes in 1983
New and revised CPT codes are published each year.
Current Procedural Terminology (CPT) Evaluation Codes for OT: ***3 Levels
***identify and distinguish between the 3 levels of evaluation complexity; need to know number of performance deficits impacted, expected time for evaluation and clinical decision making, number of co-morbidities, occupational history
On January 1, 2017, new codes for OT went into effect
97165: Occupational therapy evaluation, low complexity (straightforward)
97166: Occupational therapy evaluation, moderate complexity (involved)
97167: Occupational therapy evaluation, high complexity (very involved)
97168: Occupational therapy re-evaluation
Reflect a level of clinical decision-making during the evaluation process
***Low Complexity
“Identifies 1-3 performance deficits (relating to physical, cognitive, or psychosocial) that result in activity limitations and/or participation restrictions.”
Typically, evaluation is 30 minutes spent face-to-face
Typically, no comorbidities
***Moderate Complexity
“Identifies 3-5 performance deficits (relating to physical, cognitive, or psychosocial) that result in activity limitations and/or participation restrictions.”
Typically, evaluation is 45 minutes spent face-to-face
Expanded chart review
Co-morbidities
***High Complexity
“Identifies 5 or more performance deficits (relating to physical, cognitive, or psychosocial) that result in activity limitations and/or participation restrictions.”
Typically, evaluation is 60 minutes spent face-to-face
Extensive review of the history of physical, cognitive, or psychosocial
timing of evaluation is not set in stone- don’t let this be your determining/scoring factor (it’s more as a guide!)
score more so off the # of performance deficits + how expanded your chart review is
insurance would also much rather have you score down; it is much more likely to cover low complexity patients
rate as low complexity > (more often) than high complexity
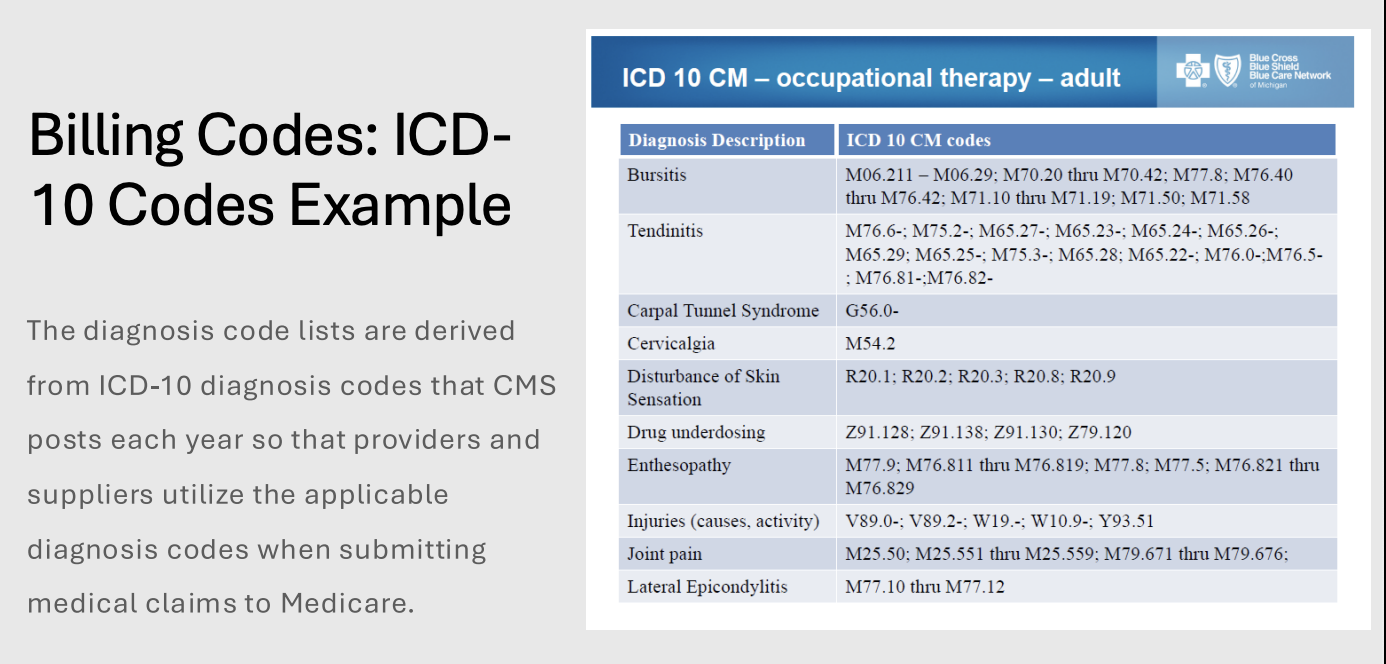
level example
moderate complexity
***7~ performance-related deficits BUT she’s 9 weeks out from stroke (she should have already been having therapy)
high-complexity patients need more immediate help
she lives at home
daughter is helping with routine care, but it doesn’t say she isn’t fully able to do her ADLs
always code down (even though it’s more likely that she’s really high complexity)
***(1) legally blind, (2) short-term memory deficits, decreased ability to complete tasks (3) vacuuming, (4) dusting, (5) doing laundry, (6) knee replacement, (7) trouble coping
Improving Medicare PostAcute Care Transformation (IMPACT) Act of 2014: Quality Reporting Program
CMS implemented new functional items and related outcome performance measures for post-acute care (PAC) settings
Intent of cross-setting quality reporting program is to facilitate quality measurement and quality improvement across PAC settings
GG items promote standardization across PAC settings to evaluate the effects of health care services on patients’ overall health and functional status over time

Value Over Volume in Documentation
***identify documentation strategies to facilitate value over volume for OT practice and point of service
Value is based on outcomes not volume (minutes)
i.e., are they becoming more functional? are they becoming more independent? are they able to go home?; NOT did you treat them for 60 minutes?
Impact:
If value or improved outcomes are not achieved, there may be no reimbursement for OT service
note should be concise: “__ is the functional outcome of this session” NOT “we did 10 reps of sit-to-stands, 3x”
Need to highlight the value of the scope of OT in documentation
Goal: provide the right care to clients, in the right amount, when they need it, to show documented outcomes in the following 6 areas:
Activities of Daily Living
Instrumental Activities of Daily Living
Behavioral & Psychosocial Skills
Falls Prevention
Vision
Functional Cognition
IMPACT Act: Requires 5 Sets of Quality Data
***identify documentation strategies to facilitate value over volume for OT practice and point of service
Physical and Cognitive Function and Changes in Function
Skin Integrity (onset and worsening of pressure ulcers)
Medication reconciliation (i.e., formal process in healthcare to ensure patients receive the correct medications, preventing errors during transitions of care)
Incidence of major falls
Discharge planning from one post-acute setting to another (including home setting):
Timely transfer of health information to the next care setting
Patient preference
IMPACT Act: Resource Use Quality Measures
***identify documentation strategies to facilitate value over volume for OT practice and point of service
Total Medicare spending per beneficiary
Whether the patient was discharged to the community
insurance wants people to go home
All-cause risk-adjusted preventable hospital readmission rates
huge issue if someone, e.g., falls
Functional Assessment in Post-Acute Care (PAC) Settings

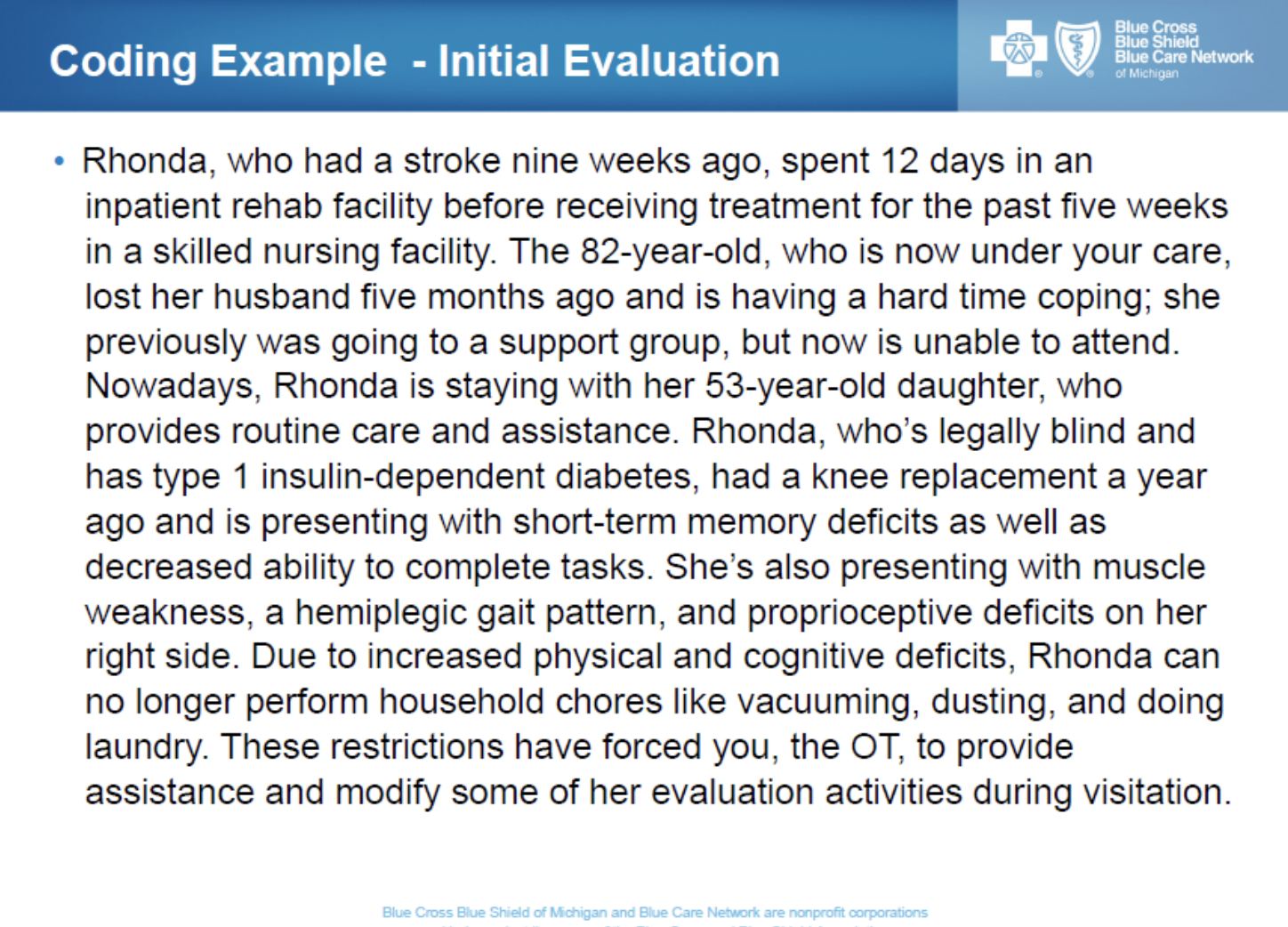
GG Coding
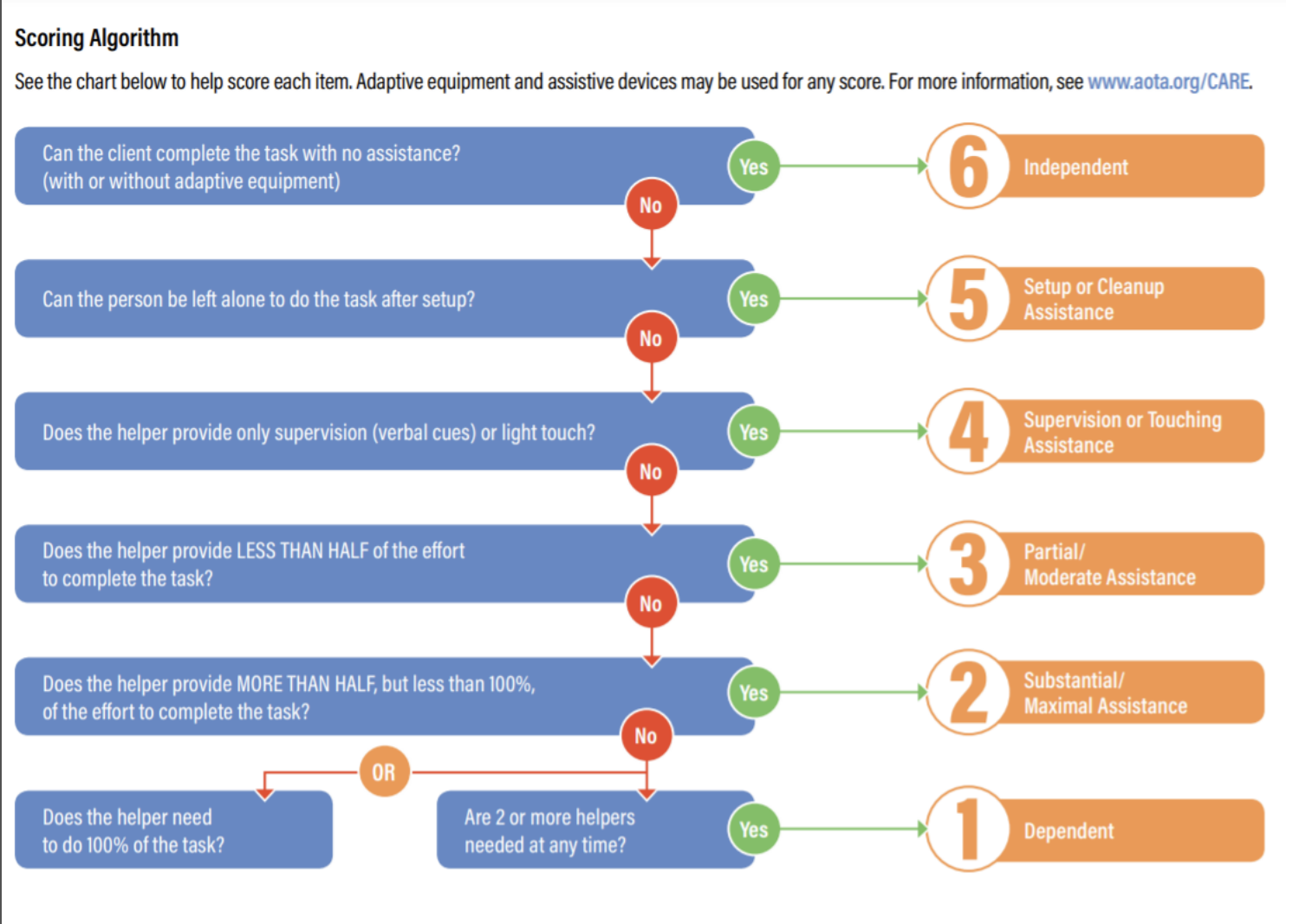
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
Section GG is a standardized assessment utilized by the Centers for Medicare and Medicaid Services (CMS) in post-acute care settings
The assessment measures a patient’s need for assistance with self-care and mobility while also documenting the patient’s prior level of function
Post-Acute Care settings consist of Long-Term Care Hospitals (LTCH), Inpatient Rehabilitation Facilities (IRF), Skilled Nursing Facilities (SNF), and Home Health (HH)
The IMPACT Act of 2014 required CMS to develop a set of standardized outcome measures in post-acute care; before Section GG’s implementation, CMS said that they were essentially comparing apples to oranges versus apples to apples (thus, preventing comparison or consistency)
CMS wanted a universal language to track how patients improve/decline as they move through the post-acute care continuum; this data helps CMS evaluate the services a patient receives and how it relates to functional improvements
GG Coding: Important for Goal Setting
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
***demonstrate the ability to formulate goals
score the person’s usual performance; guidelines for coding
using the 6-pt scale, code the patient’s or resident’s usual performance (not their best or worst performance) for each activity
if helper assistance is required because the patient’s or resident’s performance is unsafe or poor quality, score according to the amount and type of assistance provided
remember, activities may be completed with or without assistive devices, and patients or residents should perform activities as independently as possible, as long as they are safe
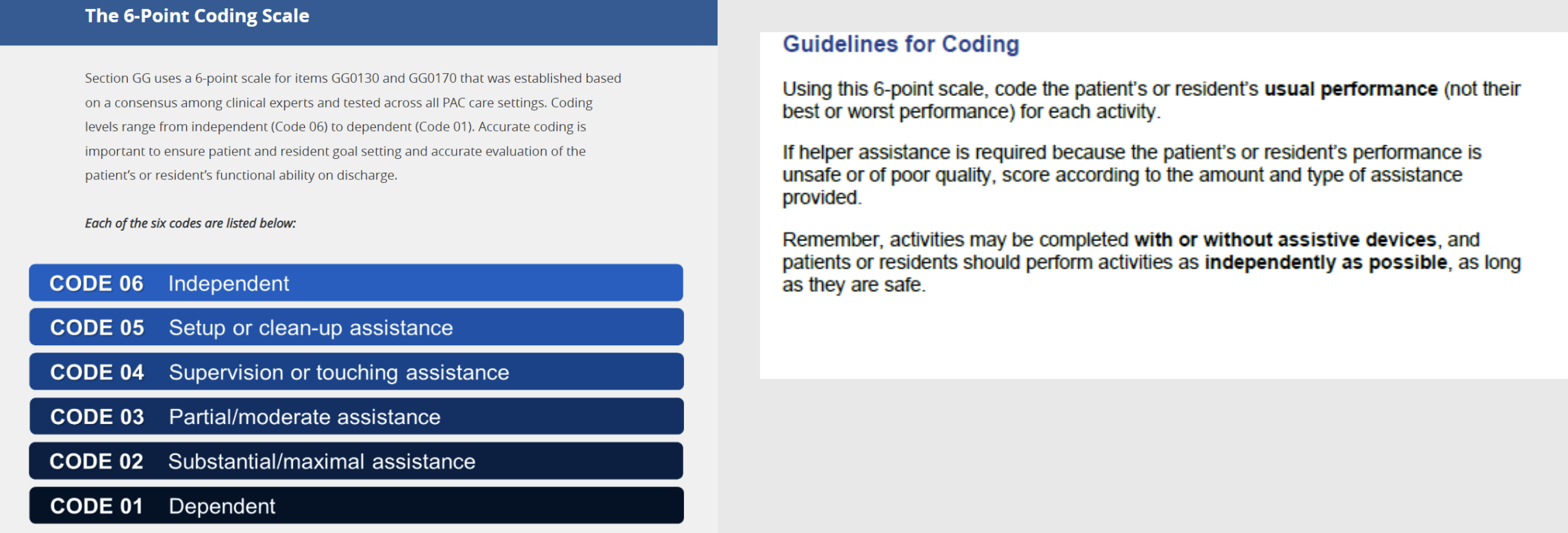
Section GG Scoring
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
6-Independent
Person completes the activity by themselves with no assistance from a helper
5-Setup or Cleanup Assistance
Helper SETS UP or CLEANS UP; person completes activity
Helper assists only before or following the activity (the helper can walk away and leave the person unsupervised to complete the task)
4-Supervision or Touching Assistance
Helper provides VERBAL CUES or TOUCHING/STEADYING and/or CONTACT GUARD ASSISTANCE as the person completes the activity
Assistance may be provided throughout the activity or intermittently
3-Partial/Moderate Assistance
Helper may lift, hold, or support the trunk or limbs but provides LESS THEN HALF of the effort
2-Substantial/Maximal Assistance
Helper may lifts or holds the trunk or limbs and provides MORE THAN HALF the effort
1-Dependent
Helper does ALL of the effort
Person does none of the effort to complete the activity
Or, the assistance of 2 or more helpers is required for the person to complete the activity
GG0100: Prior Functioning Everyday Activities
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
The assessment of a patient’s or resident’s prior functional status is key to realizing a patient’s or resident’s potential for improvement, stability, or decline
insurance only wants to restore someone to their prior level of function (don’t want to pay them to become any better than they need to be/exceed in outcomes)
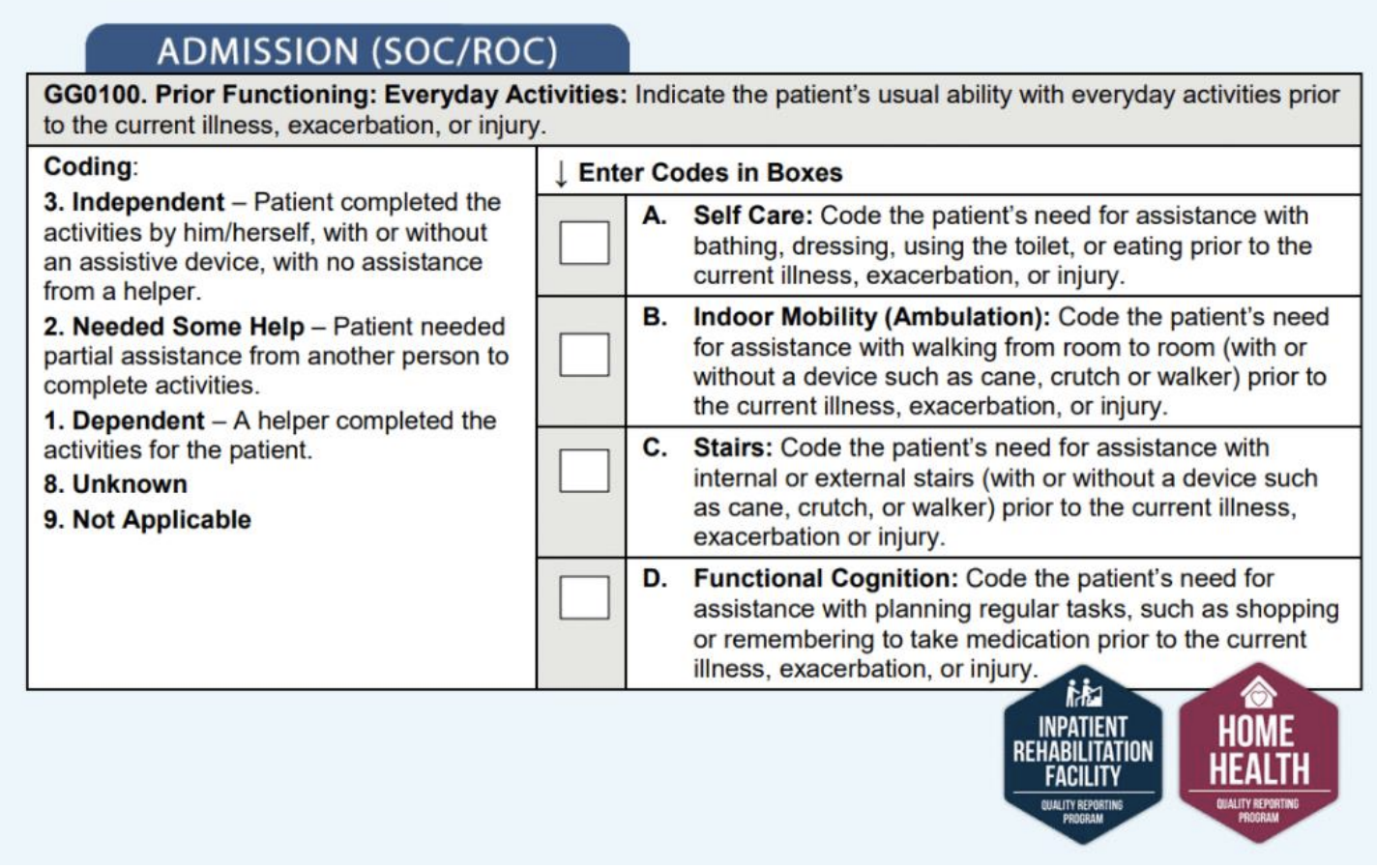
GG0110: Prior Device Use
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
This item collects data on a patient’s or resident’s usual ability with everyday activities prior to the current illness, exacerbation, or injury
e.g., be able to independently use a wheelchair (if that’s what they were doing before)

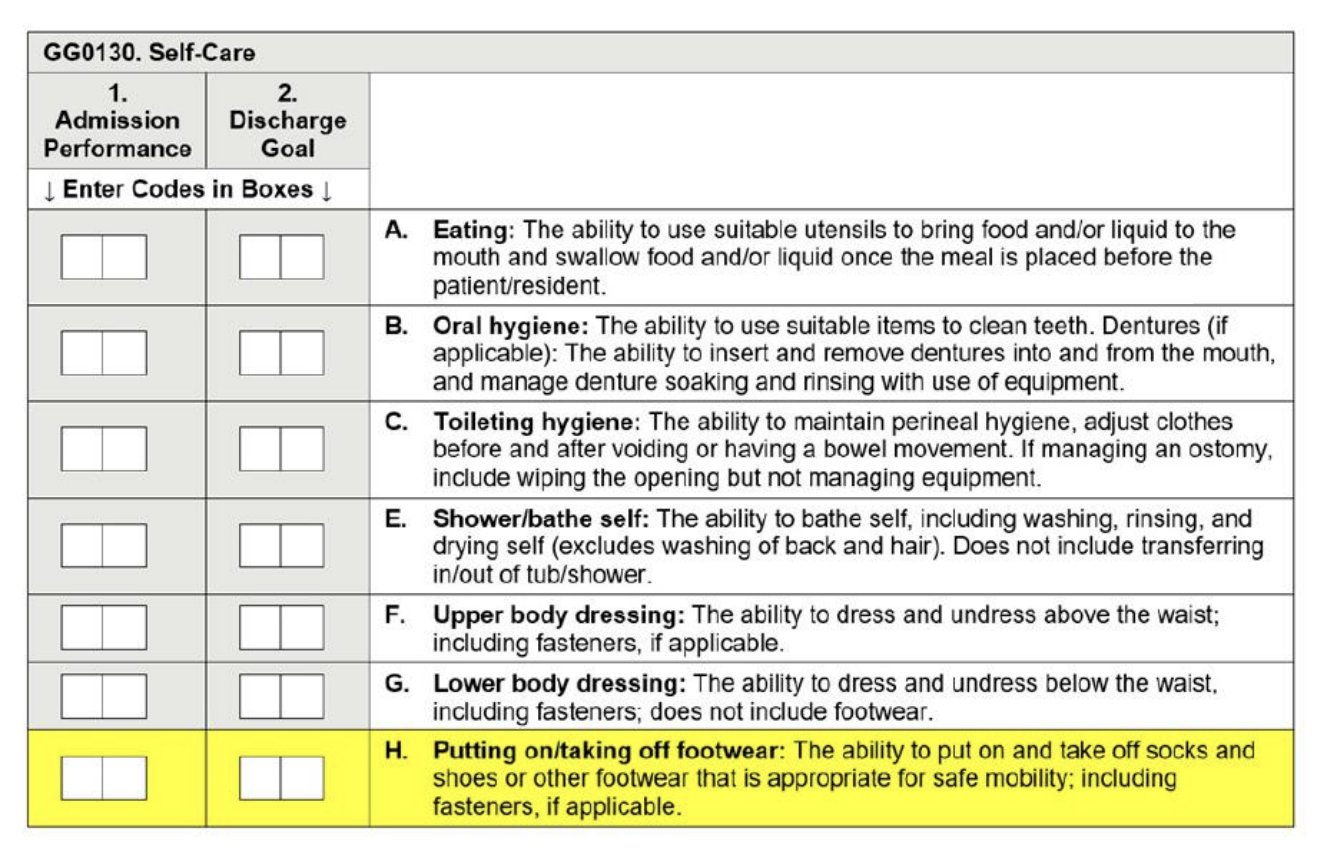
GG0130: Assessment and Coding
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
assess the patient’s or resident’s performance based on direct observation as well as reports from the patient or resident, clinicians, care staff, and/or family
GG Coding Tip
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
Use of an assistive device to complete the activity should not affect coding
e.g., use of a walker independently can still be coded as a 6
Activities should be performed as independently as possible, provided they are safe, for improved QOL and well-being
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
Code 05, Setup or clean-up assistance
had to be set up with a strap, but after that, doesn’t need any supervision
patient needed help opening a creamer from a nursing aide
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
Code 05, Setup or clean-up assistance
patient needed a walker to get up out of bed, but did it alone without any nursing assistant coming into the room
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
Code 06, Independent
use of tools doesn’t affect scoring
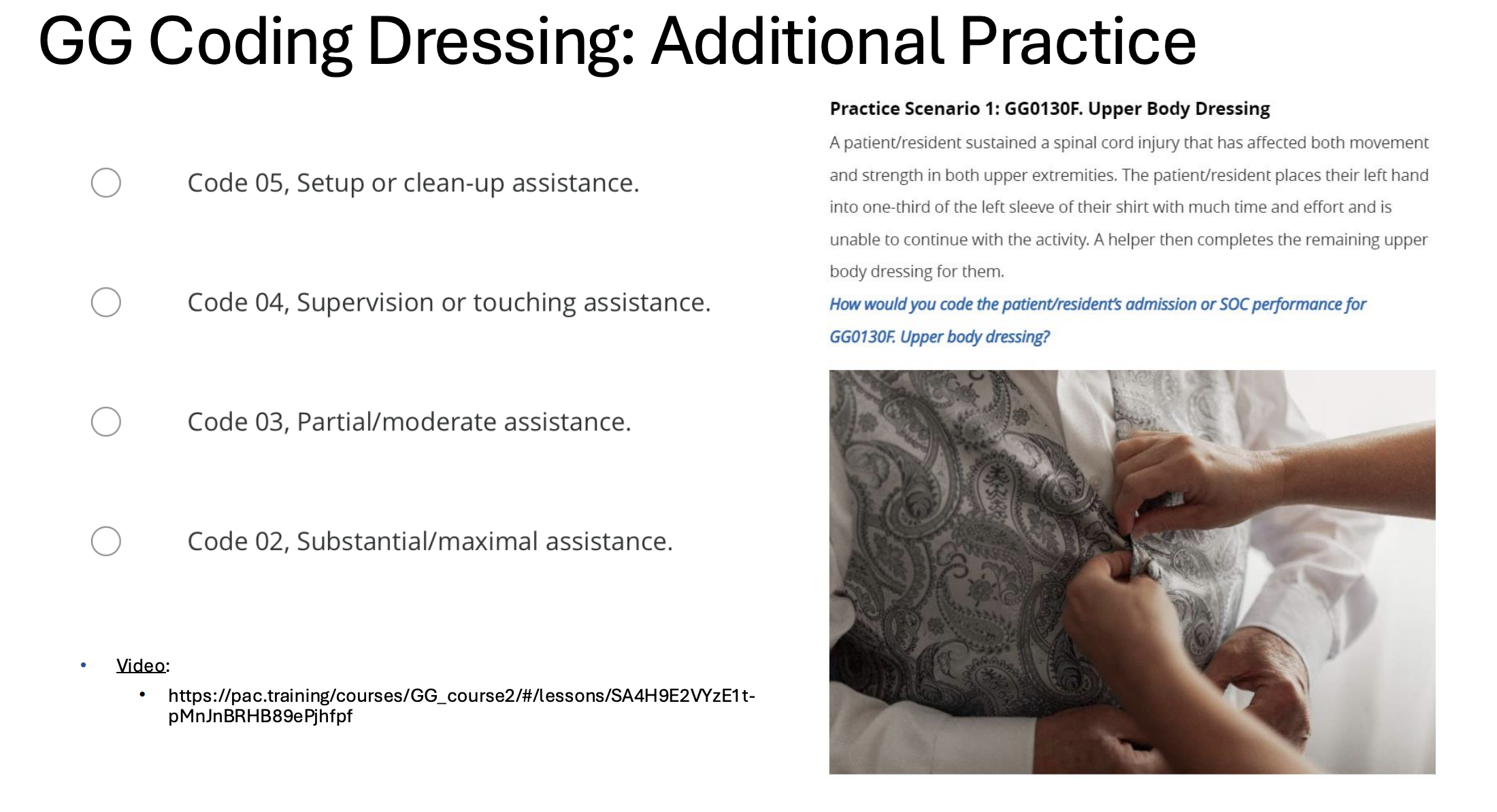
***be able to identify qualifier for and describe “GG Scores” (i.e., what does setup or cleanup assistance count as, what is partial/moderate assistance, what is dependent, etc.)
Code 02, Substantial/maximal assistance
able to get arm into the shirt independently (but with lots of effort), but the rest of the task of upper body dressing needed assistance (more than 50%, making it NOT partial/moderate assistance)
GG 0170 Mobility CARE Items

REIMBURSEMENT FOR OT SERVICES
***understand current documentation requirements and their impact on reimbursement
increased GG scores + increased independence
==> improved outcomes
==>==> reimbursement
Forms of Documentation
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
Initial Evaluation/Plan of Care
Daily Intervention/Treatment/Session (Contact Note)
Progress Note:
Written usually monthly, as determined by the facility
Summary of the intervention process and documents progress
Includes recommendations for continuation of services
Discharge Summary
to the home, subacute care, etc.
Objective Measures & Assessment Tools
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
Need to use objective assessment tools
for documenting change/progress
Measures for Varied Settings
Documentation of Standardized Assessments
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
Summary should include:
Test/screen that was administered (put the name of the assessment used)
Purpose/objective of the tool
State results (e.g., scored 17/30, indicating moderate cognitive impairment)
Indicate areas of strength & areas that posed a challenge
Recommendations
Occupational Therapy Initial Evaluation Report: SOAP Format
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
extremely common in mental health practices
a bit more standardized in acute settings (check-off digital system > handwriting note)
SOAP
S: Subjective- information provided by the client or caregiver
O: Objective- factual information, e.g., status of therapy goals, accuracy level, cueing level, etc.
A: Assessment- clinical impressions and interpretation of the subjective and objective information
P: Plan- what are the recommended next steps for the treatment and plan for the next session?

Plan of Care (initial evaluation)
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
Must include:
Diagnoses
Long-term treatment goals
Type and amount of treatment
Frequency (amount of time in a week that a person should get therapy)
Duration (how many weeks)
e.g., 2x/week (frequency) x 4 weeks (duration)
What does POC (Plan of Care) include?
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
Rehabilitation/Treatment Diagnosis
(MS weakness, Lack of coordination, Need for personal care assistance)
Identify specific interventions to be used to treat the patient’s needs (thinking CPT codes)
(i.e., therapeutic exercise, functional training, manual therapy techniques, adaptive devices/equipment needs, modalities)
Establish anticipated goals, expected outcomes, and any predicted level of improvement
Short-term goals (optional) or Long-term goals
Determine the intensity, frequency, and duration of care
Anticipated discharge plans
Medicare Documentation Requirements
***identify current Medicare requirements for documentation
Evaluation/Reevaluations
Plan of Care
Therapy Goals
Progress Notes/Reports
Treatment notes for each treatment day
Documentation Pitfalls
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable
Goals are not client-centered or measurable
Use of abbreviations that are not acceptable medical abbreviations
Intervention activities are not used as functional outcomes
e.g., “patient is able to throw a ball into a bucket” is NOT a functional outcome
Duplication of services
Need to demonstrate coordination of care
OT notes shouldn’t look identical to PT notes (e.g., both doing bed transfers); insurance will not pay for this!
No documentation of change
Goal Writing: COAST Method
***demonstrate the ability to formulate goals
***identify current Medicare requirements for documentation
C – Client will perform
O – Occupation
A – Assist Level
S – Specific Condition (ensures goal is measurable)
T – Timeline
Example of Short-term Goal:
Client will prepare a simple meal with contact guard assist in standing using a walker within 2 weeks
C: prepare a simple meal
O: prepare a simple meal
A: with contact guard assist
S: in standing using a walker
T: within 2 weeks
upgrade goal:
decrease assistance (independently)
be more specific with the description of a “simple meal”
< “hot meal”
downgrade goal:
increase assistance (min or mod)
increase timeline
in a seated position
Client will complete lower body dressing with minimal assistance using assistive devices within 1 week
C: will complete lower body dressing
O: lower body dressing
A: with minimal assistance
S: using assistive devices
T: within 1 week
Document Long-term Goals
***demonstrate the ability to formulate goals
***identify current Medicare requirements for documentation
To be included in Plan of Care
should match your short-term goal
STG: upper body dressing
STG: lower body dressing
STG: clothes acquisition
Examples:
LTG: Client will complete all dressing tasks independently by discharge
LTG: Client will perform yardwork independently while adhering to energy conservation strategies upon discharge
Daily Treatment Encounter Session Note
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
The daily note must contain:
Date of Service
Treatment rendered/ all services provided
How much time was spent on each service
e.g., 15 mins for therapeutic exercise
e.g., 10 mins for ADL training
Any changes made to treatment from the last visit
Any observations of the patient made during treatment
i.e., response to treatment, or changes noted during the session
example of how to start off
“Seen for 45 minutes OT session today … Tx included … or documented under each code …….”
Progress Note
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
***identify current Medicare requirements for documentation
An evaluation of the patient’s progress
Professional judgement about the medical necessity of continued care
Goal status
Any treatment modifications
De-emphasize treatment media
do not say the day-to-day exercise treatments
look at the big picture functional status/goals
SOAP format
D/C Summary
***identify key documents required in clinical practice for older adults
***understand current documentation requirements and their impact on reimbursement
The course of treatment
Discharge notification
Objective summary of patient status referencing the condition at the start of treatment
Equipment needs/status of their equipment (if you are recommending they purchase something)
Patient/Caregiver education & training
Recommendations/Follow-up
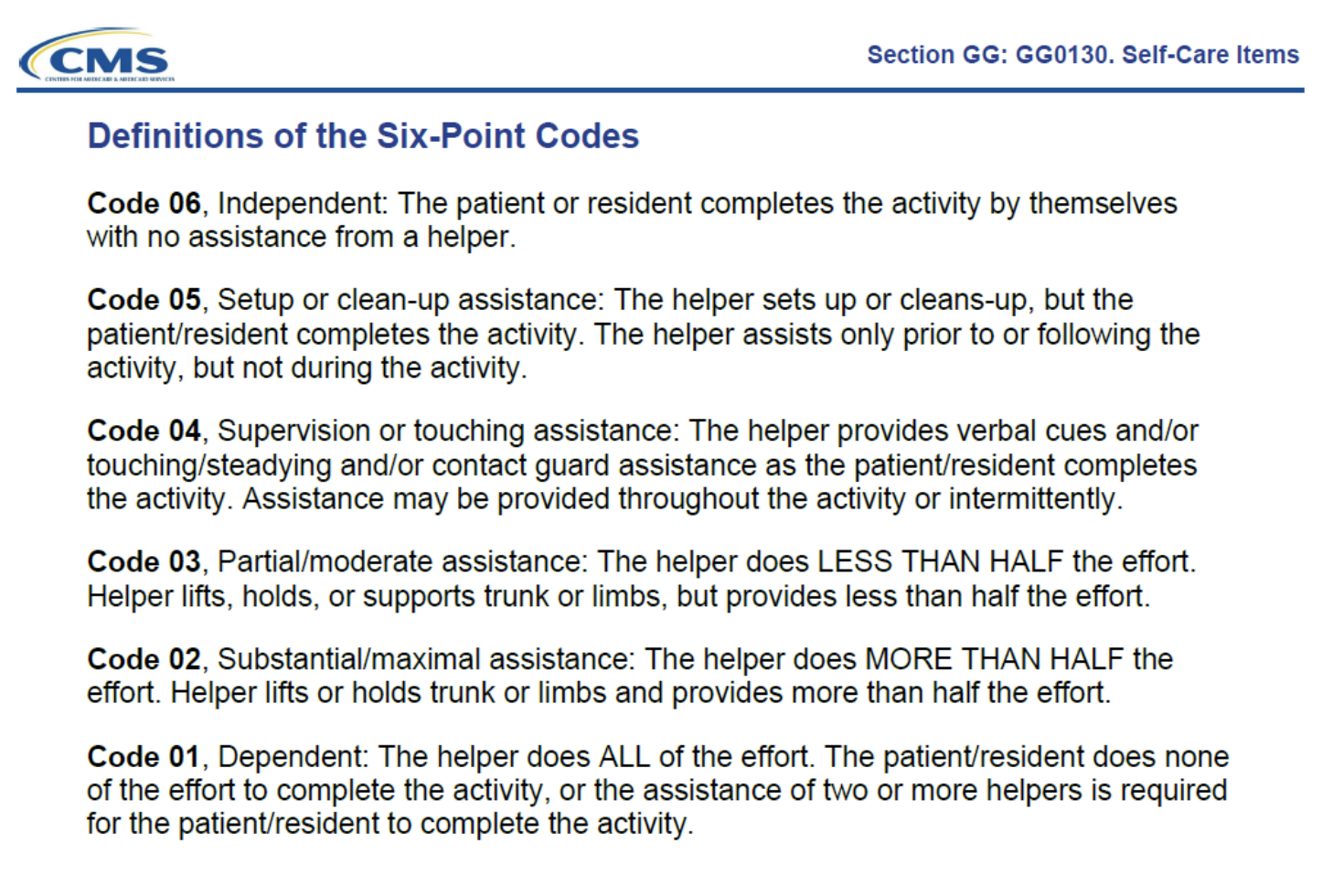
Progress Note Example of Medical Justification for Continued Skilled Services
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable
***identify current Medicare requirements for documentation
What is considered “NOT Reasonable and Necessary”
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable
Unskilled services
General exercises to promote fitness/ flexibility
e.g., don’t document “using the arm bike”- even if it is useful to do as a warmup before your actual intervention
Activities to provide diversion or general motivation
Services not included in the plan of care or provided by staff that are not properly supervised or qualified
Considerations
***understand current documentation requirements and their impact on reimbursement
Cognitive factors
Chronic vs. new injury/ illness
PLOF (prior level of function)
Assessing objective measurable gains for OT
Change in the level of assistance
Changes in types of functional activities
Modification of assistive devices
Noted decreased pain levels and changes in the ability to perform tasks because of decreased pain
Non-skilled Terminology – Terms to Avoid
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable
Ambulate
a very “PT term”
“functional transfer”, “functional mobility” is better for OTs
Discuss
Encourage
sounds like you had to push the person to do something
Help
Little Change
Maintain
Monitor
No changes
Observe
Watch
just watching? what are you really doing?
“cueing” better
Supervised
Skilled Terminology
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable
why do they need a skilled therapist?
Adapt
Assess
Analyze
Continues to progress because …
Continues to require …… because
Design
Fabricate
Facilitate
Instruct
Modify
Correction of techniques
Trained
Practice Writing Contact Note: SOAP Format
S: Patient has reported having increased LBP (low back pain)
O: Patient is able to perform all their UE therapy exercises; standing reaching activities; retrieve/return items from kitchen cabinets; cross midline using good safety techniques; do toilet transfer with supervision; hygiene tasks with minimal assistance; clothing management with minimal assistance; handwashing with cues
A: Missing; but could~ be that patient needs cues to achieve upright posture
P: Missing; should be “continue with OT sessions 1x/week to increase standing tolerance to increase engagement with functional tasks”
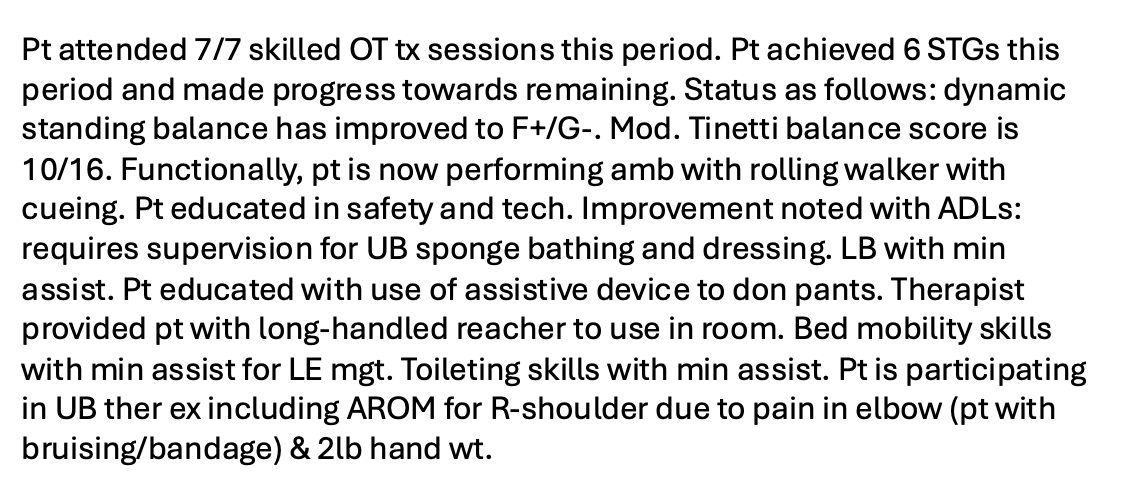
Progress Report: What Is Missing?
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable
not organized as a SOAP note- bad; make it more organized
does not have professional judgment for continued medical care
what improvements do you want them to make in therapy?
treatment modifications could be fine-tuned a bit
exclude part about 2lb hand weight; insurance doesn’t care and it’s not functional
Medical Justification Example
***be able to critique documentation samples to ensure medical justification, measurable, and reimbursable