Chronic Kidney Disease Discussion
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
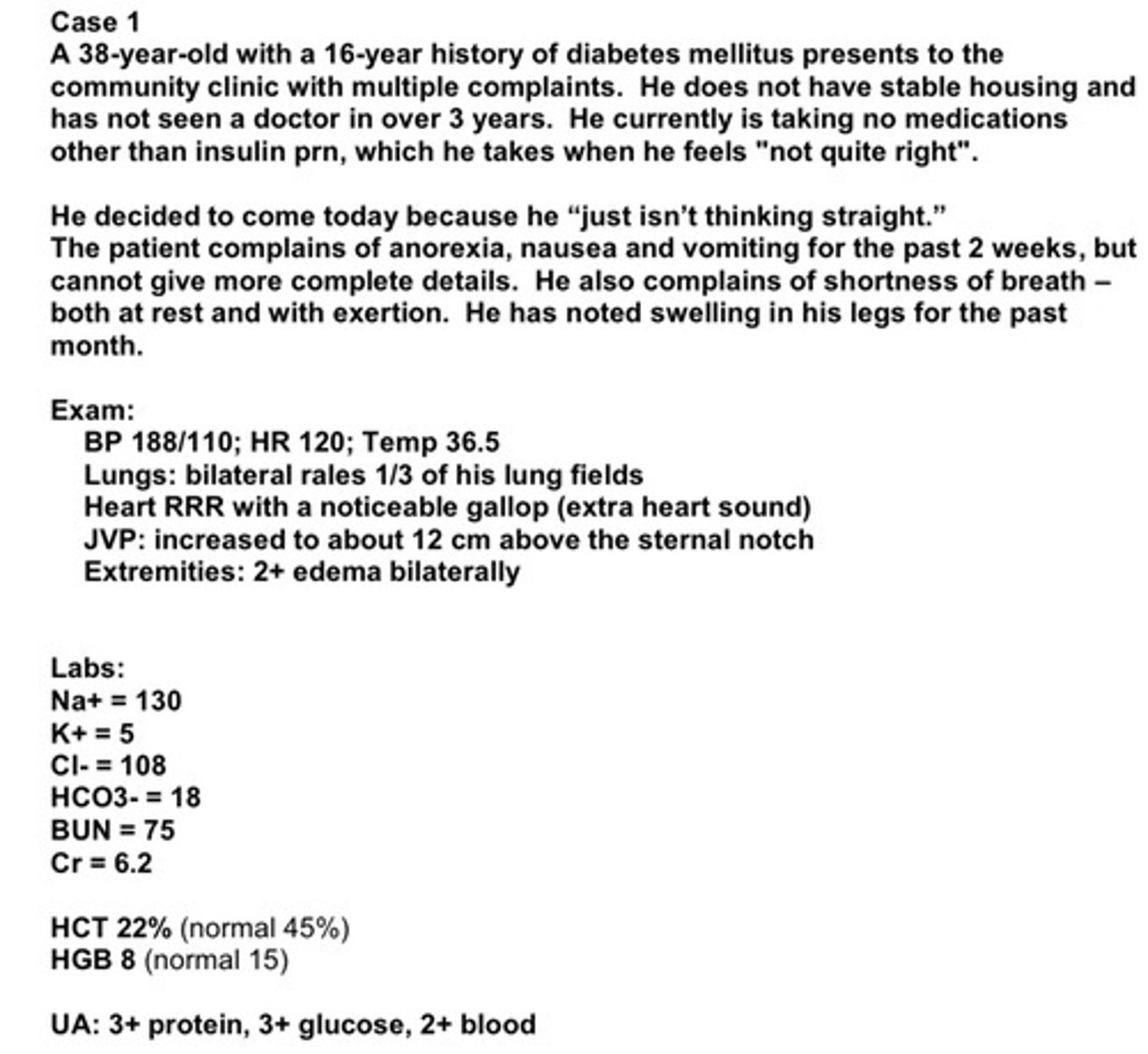
use this case for the following questions
what do you notice about the pt's labs
labs are abnormal!
1) he has hyponatremia (total body water excess), hyperkalemia, metabolic acidosis (low bicarb), high BUN, and very high creatinine (defines extremely poor renal function
2) very anemic (low RBC count)
3) pt is spilling protein, glucose, and blood in his urine, suggesting both kidney disease as well as uncontrolled diabetes
what do you notice about the pt's PE
1) BP is very elevated to an acutely dangerous level (pt is at risk for stroke, esp if this is a new elevation)
2) tachycardic, which may be explained by anemia
3) edema suggests that he has too much total body sodium, which we presume is primarily bc he has poor renal function
what might be some further studies and interventions we would consider and why?
1) blood glucose: pt needs his blood sugar controlled asap as chronically uncontolled blood sugar can spin out of control, wreaking havoc on multiple organ systems and homeostasis, which he may be approaching. pt also likely needs insulin which will bring down blood sugar as well as high potassium
2) 24 hour urine collection to determine level of proteinuria and GFR; depending on his status, pt may get dialysis instead since his creatinine is 6.2
3) diuresis for water overload and edema; if pt's kidneys cannot perform to diurese, we would manage volume status with dialysis
4) bicarbonate supplmentation to correct pH/metabolic acidosis
5) renal ultrasound as an investigation into the ultimate cause of situation (look for clues, determine if acute or chronic)
what might we consider to treat the pt's anemia but how might this worsen the pt's condition
blood transfusion might be considered for his anemia, but could worsen his fluid overload if he cannot diurese the extra fluid bc of his kidney status; epo (erythropoietin) could be given, but it takes weeks to work. pts anemia probably reflects his poor kidney function
what are some ways to differentiate AKI from CKD
1) urine volume: sudden oliguria is assoc with AKI; people with CKD often have normal urinary output. end stage renal disease may have decreased urine output, but even people on dialysis still urinate (although urine is not effectively managing toxins and electrolytes
2) renal ultrasound: size of kidneys is normal in AKI; kidneys are often small in CKD
3) anemia is very common in CKD, but unlikely in AKI
4) access to previous records to compare serum creatinine levels is useful esp bc people with CKD can have acute exacerbations
CKD is not reversible, and it progresses towards kidney failure/end stage renal disease (ESRD). what are the terms used to describe this progression (the stages)
stage 1: normal or high GFR (>90)
stage 2: mild CKD (GFR = 60-89)
stage 3A: moderate CKD (GFR = 45-59)
stage 3B: moderate CKD (GFR = 30-44)
stage 4: severe CKD (GFR = 15-29)
stage 5: end stage CKD (GFR <15)
besides knowing criteria for stage 5 and that there are 5 stages, also note that if your pt has stage 3 or higher, their meds will need to be adjusted for GFR
you may have heard the terms "renal insufficiency", "azotemia", and "uremia" to describe CKD. what does "renal insufficiency" mean
mild renal dz; the GFR is diminishing, but the pt is able to maintain electrolyte/acid-base homeostasis somewhat and is relatively asymptomatic. there may be evidence of other loss of kidney function, such as loss of epo production or decrease in renal hydroxylation of vit D. this ineffective vitD leads to reduced calcium absorption in the intestines. utlimately, this ineffective vitD leads to increased parathyroid hormone (PTH) which causes bone changes called "renal osteodystrophy" and hyperparathyroidism
you may have heard the terms "renal insufficiency", "azotemia", and "uremia" to describe CKD. what does "azotemia" mean
worsening renal function; nitrogen in the form of BUN is building up in the blood because so few working nephrons remain. ammonia builds up, which has liver and brain implications. these pts are at risk for thrombosis and ecchymosis. pts are often symptomatic with fatigue, anorexia, headaches. the inability to get rid of BUN is assoc with a metabolic acidosis and pts may hyperventilate to compensate. electrolyte balance is not maintained well
you may have heard the terms "renal insufficiency", "azotemia", and "uremia" to describe CKD. what does "uremia" mean
severe renal dysfunction (essentially, urine in the blood). the kidneys are unable to filter the nitrogenous wastes which are toxic. pts are very symptomatic with unclear thinking, depression, nausea, vomiting, pruritis. the kidneys are unable to maintain electrolyte and acid-base homeostasis. they are at risk for spontaneous stomach and intestinal hemorrhage due to the abnormal interaction between kidneys and liver, where the clotting factors are produced. kidneys do not stimulate RBC production; kidneys have failed and is fatal if not managed
identify the pt's complications associated with CKD (8)
1) volume overload
2) anemia
3) hypertension
4) metabolic acidosis
5) neurologic
6) GI
7) bone
8) skin
explain the likely pathogenesis of this complication: volume overload
may be partly due to CKD (decreased GFR), but could also be secondary to nephrotic syndrome (likely secondary to diabetic kidney disease). in nephrotic syndrome, the pts lose their albumin in the urine, and they develop edema with the loss of the main source of capillary oncotic pressure
explain the likely pathogenesis of this complication: anemia
pt's anemia is likely from decreased epo production. however, his anemia may be multifactorial and may also come from blood loss thru stool (since uremia is assoc with poor clotting) and from poor nutrition
explain the likely pathogenesis of this complication: hypertension
likely is secondary to renal failure although there is an increased incidence of essential htn in pts with diabetes
explain the likely pathogenesis of this complication: metabolic acidosis
although we do not have an ABG, we expect he has a metabolic acidosis bc he is unable to effectively reabsorb his bicarbonate (HCO3- = 18)
explain the likely pathogenesis of this complication: neurologic
malaise, difficulty concentrating, not thinking clearly is secondary to electrolyte abnormalities and inability to excrete toxins and uric acid
explain the likely pathogenesis of this complication: GI
loss of appetite, nausea, vomiting is common with severe CKD
explain the likely pathogenesis of this complication: bone
osteopenia from decreased Ca+ absorption (from inactive vitD) and elevated PTH levels (a hormone that stimulates bone resorption)
explain the likely pathogenesis of this complication: skin
pruritis is often seen with high BUN. pt reports skin dryness as well
what potential interventions could be employed to slow the progression of CKD (6)
the most common causes of CKD in the USA are diabetes mellitus and hypertension. controlling these diseases have a big impact on renal function:
1) lifestyle measures: weight loss, low protein diet, low sodium diet
2) BP control
3) RAAS blockade: damage to kidneys increases RAAS which causes more damage. RAAS blockade decreases proteinuria and reduces mediators of renal injury. recall that ang-II can lead to hyperfiltration at the glomerulus, which can be challenging to the nephron, so ang-II blockade can protect the nephron. pts with CKD are often on ACEIs or ARBs
4) glycemic control: this will optimize whatever renal function remains (glucose is toxic both to glomeruli membranes as well as to blood vessels)
5) lipid control: this will optimize perfusion to kidneys
6) SGLT2 inhibitors: prevent reabsorption of glucose in PCT