DSA20 - Chronic Diarrhea and Malabsorption
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
Passage of loose or watery stools, typically at least 3 times in a 24-hour period (for 14 days or less)
Define ACUTE Diarrhea
Passage of loose or watery stools, typically at least 3 times in a 24-hour period (for > 2 wks)
Define CHRONIC Diarrhea
Stool volume > 14L/day (may cause severe dehydration and death)
Define Severe Diarrhea
Systemic symptoms (fever) + Bloody diarrhea
Define Dysentery
Usually when luminal ion channels are disrupted -> ↑ion secretion or ↓ion absorption -> ↑ions in GI tract -> water follows the ions -> watery diarrhea; occurs with and without food
Define Secretory Diarrhea
Stimulates Cl- secretion --> Body response w/ Na+ and H2O
How is Cholera a "Secretory Diarrhea"?
↑Osmole (sugar, salt, meds, etc) in the bowel lumen -> draws too much water into the bowels -> watery diarrhea; IMPROVES WITH FASTING
Define Osmotic Diarrhea
Body can't digest lactose --> that sugar stays in bowel lumen ==> water drawn out ==> DIARRHEA
How does a Lactase Deficiency cause Osmotic Diarrhea?
Results from inadequate nutrient absorption; associated with steatorrhea (Fatty Stool); IMPROVES WITH FASTING
Define Malabsorptive Diarrhea
Unable to create enzymes for fat breakdown --> Can't absorb nutrients properly ==> Lost in LOTS of stool
How does Pancreatic Insufficiency cause Malabsorptive Diarrhea?
D/t inflammatory disease causing purulent, bloody diarrhea - CONTINUES during fasting
Define Exudative Diarrhea
GI tract becomes irritated/inflamed --> Stool filled with blood or inflammatory cells
How does Ulcerative Colitis/IBD cause Exudative Diarrhea?
Intraluminal Digestion - b/c won't allow protein, carbs and fats to be broken down into absorbable forms
In what phase of Nutrient Absorption do CF and Chronic Pancreatitis create a problem and why?
Terminal Digestion - b/c won't allow carb and peptide hydrolysis to occur in SI brush border
In what phase of Nutrient Absorption do Celiac Disease and Lactose Intolerance create a problem and why?
Transepithelial transport - b/c doesn't allow certain nutrients to be transported across and processed in SI epithelium (affects transport of cholesterol components)
In what phase of Nutrient Absorption does Abetalipoproteinemia create a problem and why?
Lymphatic Transport - causes obstruction for lipids that need to be transported by the lymphatic system
In what phase of Nutrient Absorption do Whipple Disease and Mycobacteria create a problem and why?
Malabsorption
Define Condition:
When nutrients can't be absorbed in the GI tract d/t disruption of at least one of the 4 phases of nutrient absorption
-Sx:
> Diarrhea
> Wt Loss
> Weakness
-PE:
Vitamin or Mineral Deficiencies
> Anemia, Mucositis (B6, B9 or B12)
> Bleeding (Vit K)
> Osteopenia, Tetany (Ca, Mg, Vit D)
> Neuropathy (Vit A or B12)
Stool Qualities
> Steatorrhea (fatty stool)
>> Acholic Stool
>> Voluminous stools
>> Stool floating in water (fat isn't soluble in water)
> Watery Stool (Carb)
> Edema (Protein)
-Dx:
Fat
> Sudan Stain (Qualitative fecal fat test)
>> Micro detect of fat on special stain
>> Castor/Mineral Oil suppositories may cause false positives
> Quantitative Fecal Fat Test (CONFIRMATORY)
>> Measures amt of fat in stool over 1-3 days
Carb
> D-xylose
>> Test carb absorption in SI - used to test integrity of SI mucosa (Small Bowel Disease vs Pancreatic Disease)
>> Fasting --> pt ingests
>> Monosaccharide that should be absorbed in SI w/o enzymes
>> Measured in serum/urine
>> Normal = Pancreatic Disease (D-xylose in blood/urine); Abnormal = Bowel malabsorption (D-xylose NOT in blood/urine)
Cystic Fibrosis (CF)
Define Condition:
Primary intraluminal digestion defect caused by mutation in CTFR gene (encodes ATP gated Cl- channel that secretes Cl- in lungs AND GI Tract)
-Path: Defective CFTR --> Less Cl- (and H2O) secretion --> Compensatory Na+ reabsorption via ENaC ==> H2O reabsorption --> Abnormally thick mucus secreted into GI tract and Pancreas
-Sx/PE: (usually in Infancy)
> Meconium Ileus
> FTT
> Pancreatic Insufficiency --> Steatorrhea + Chronic Diarrhea + Fat Vitamin Deficiency (Night Blindness = A, Coagulopathy = K)
-Dx:
> (+) Sweat Chloride Test
> Normal D-xylose (Small bowel mucosa integrity maintained)
Bile Acid Malabsorption (BAM)
Define Condition:
Inability to reabsorb bile acids in the distal ileum
-Hx:
> Ileal Resection
> Crohn's Disease of Ileum
-Path: Bile acids are passed into the colon -> bile acids draw in water and salt AND Excess/Overproduction of bile acid ==> chronic diarrhea
-Sx/PE:
> Chronic Diarrhea
-Dx:
> Normal D-xylose Test (Small bowel mucosa integrity maintained)
Small Intestinal Bacterial Overgrowth (SIBO)
Define Condition:
Abnormal bacterial overgrowth within the small intestine (normal small bowel has low bacterial colony count)
-Hx:
> Surgery causing food to get caught in a "loop"
> Motility Disorders
-Path:
> Bacterial overgrowth -> excessive breakdown of bile salts -> fat malabsorption -> diarrhea and fat-soluble vitamin (ADEK) deficiency
> Excess bacteria metabolizes Vit B12 to inactive analogues --> compete w/ normal Vit B12 for binding/absorption ==> Vit B12 Deficiency
-Sx/PE:
> Diarrhea
> Fat Soluble Vitamin Deficiency (ADEK)
>> Night Blindness = A
>> Osteopenia = D
>> Coagulopathy = K
> Peripheral Neuropathy/Anemia = B12
-Dx:
> (+) Lactulose (Carb) Breath Test (Less Invasive)
> Endoscopy --> Small bowel cultures (INVASIVE)
-Tx:
> Abx
> Parenteral supplement of vitamins/proteins
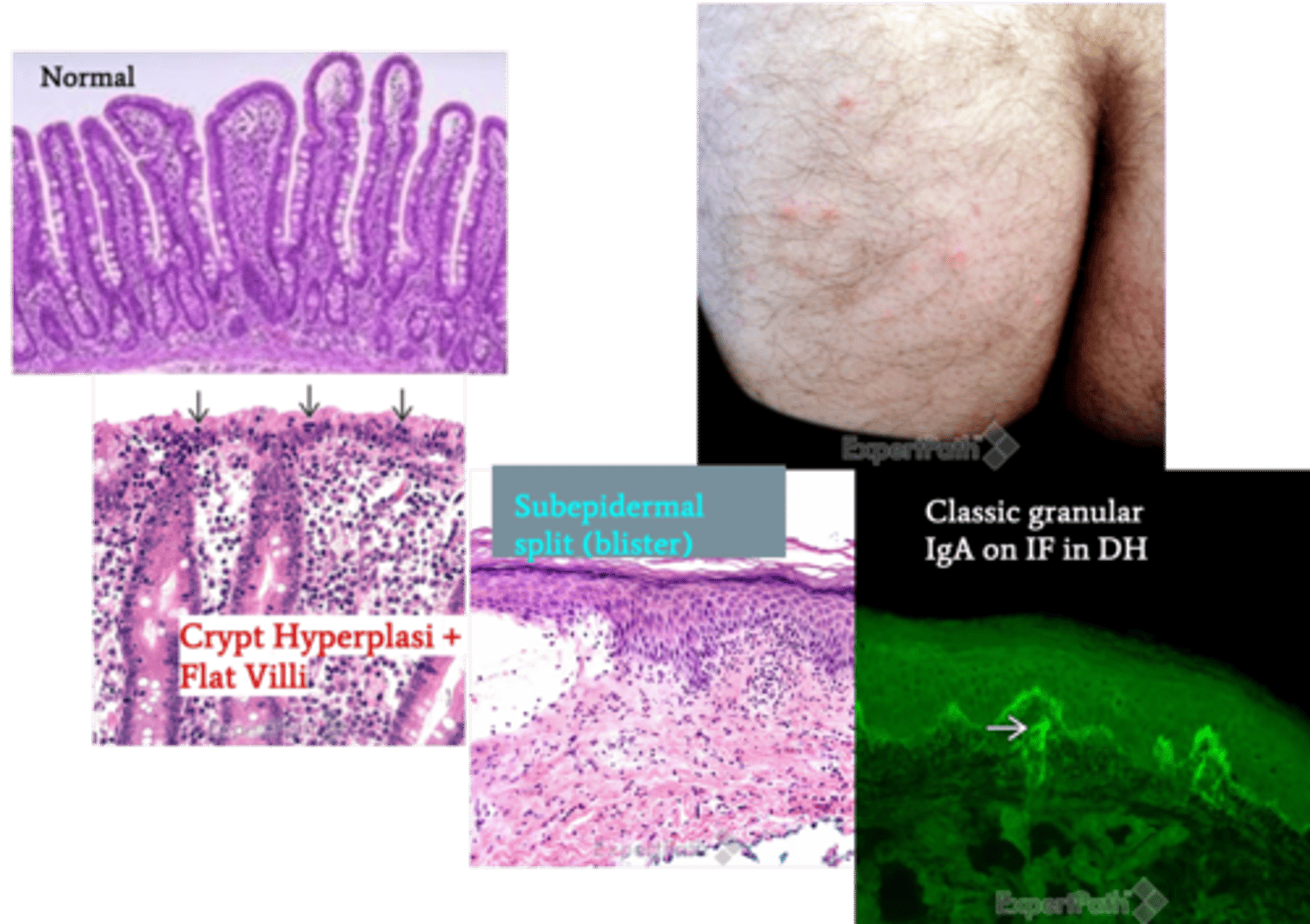
Celiac Disease (aka Gluten-Sensitive Enteropathy, Celiac Sprue)
Define Condition:
Terminal digestion defect d/t chronic Autoimmune disorder causing immune-mediated damage to small bowel villi from GLUTEN EXPOSURE
-Hx: A/w...
> HLA-DQ2
> HLA-DQ8
> Type I Diabetes
> Autoimmune Thyroiditis
> Sjogren Syndrome
-Path:
> Usually d/t protein Gliadin in Gluten
> Gliadin absorbed by enterocytes -> gliadin is deamidated by tTG -> deamidated gliadin is presented by APCs via MHC class II -> CD4+ T cells to produce an immune response causing local inflammation via Cytokines (INF-gamma that damage epithelial cells, IL-15 that stimulate CD8+ T cells that kill epithelial cells w/ NKG2D receptor & MHC-1) that stimulate Ab production from B cells -> destroys small bowel villi
> Usually affects Duodenum
-Sx/PE:
> Children = FTT
> Adults
>> Steatorrhea + Diarrhea (destruction of villi)
>> Flatulence
>> Bloating
>> Recurrent Canker Sores
>> Anemia d/t Iron Deficiency, Folate deficiency, or Vit B12 deficiency
>> Dermatitis herpetiformis (Inflammatory skin disease seen in 10% pts)
>>> Itchy blistering
>>> Herpes-like lesion
>>> D/t IgA deposition in dermal papillae
-Dx:
> Antibody Screening
>> Most Sensitive = IgA tTG Ab
>> Most Specific - IgA endomysial Ab
>> If IgA Deficient, use anti-tTG IgG Abs instead
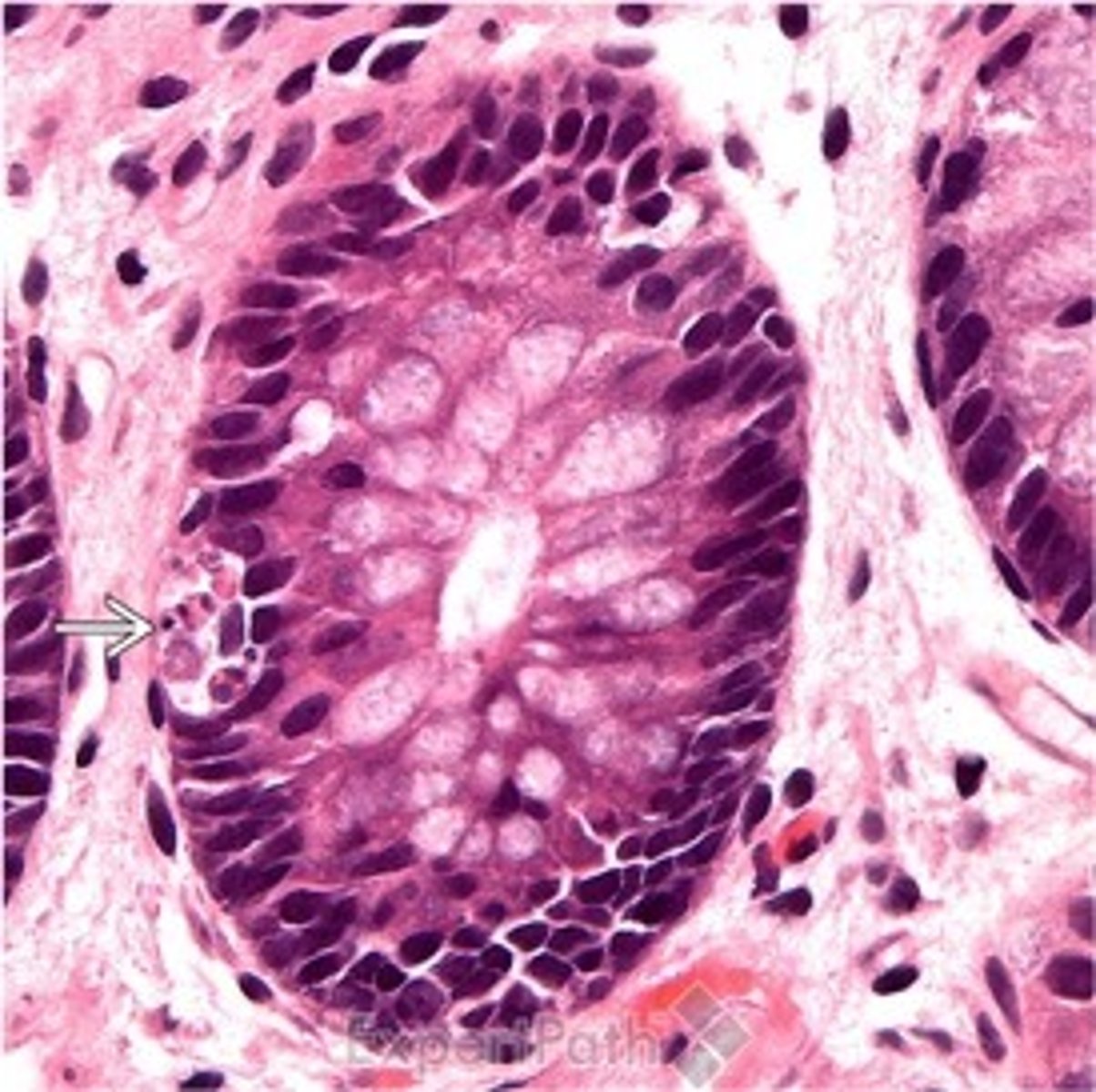
> Duodenal Biopsy (CONFIRMATORY/GOLD STANDARD)
>> Intestinal villous atrophy (blunting or flattening of villi)
>> More intraepithelial lymphocytes
>> Crypt hyperplasia (elongation of crypts)
> D-xylose ABNORMAL
-Tx: Gluten-Free Diet
-Prog:
> Risk of Enteropathy-Associated T-Cell Lymphoma (EATL)
> Risk of SI ACA
> Risk of Lymphocytic colitis & Lymphocytic gastritis
Environmental Enteric Dysfunction (EED) (aka Environmental Enteropathy)
Define Condition:
Acquired small intestine disorder among people living in conditions of poverty (defect in terminal digestion) --> enteric inflammation, villous blunting, decreased crypt-to-villus ratio
-Hx: A/w...
> Chronic malnutrition (stunted growth)
> Wasting
> Megaloblastic Anemia (Vit B12/B9 deficiency)
-Path: Enteric inflammation, villous blunting, decreased crypt-to-villus ratio ==> Less absorptive SA and impaired intestinal barrier function
-Sx/PE: Anemia d/t Iron Deficiency, Folate deficiency, or Vit B12 deficiency
-Tx: Abx
Lactose Deficiency (Intolerance)
Define Condition:
Terminal digestion defect d/t Disaccharidase deficiency
-Hx:
> Congenital = Rare autosomal recessive disorder
> Acquired = down-regulation of lactase gene expression
>> MC = Native Americans, African Americans, Asians
>> Late childhood
> Transient/Secondary = Follow Viral Gastroenteritis (Rotavirus or Norwalk virus) but pt recovers after 1-2 wks of illness
-Path: Deficiency of enzyme found in the brush border of enterocytes (tips of the villi) -> failure to break down lactose into glucose and galactose -> undigested lactose is osmotically active
-Sx/PE: (w/n 30 min to 2 hrs of consuming dairy)
> Osmotic Diarrhea & Flatulence/Bloating (Intestinal Bacteria)
> Abdominal Pain
> Nausea
-Dx:
> (+) Lactose Hydrogen Breath Test
>> Ingest lactose --> if undigested, bacteria ferment lactose ==> Release Hydrogen & Measure levels (elevated if intolerance)
> D-xylose = NORMAL
> Biopsy:
>> Acquired = Normal Villi on Biopsy
>> Transient = Virus --> sloughing of the tips of villi
Abetalipoproteinemia
Define Condition:
TRANSEPITHELIAL Transport defect d/t Autosomal recessive deficiency of apolipoprotein B-48 & B-100 (for synthesis and export of chylomicrons and VLDL, respectively)
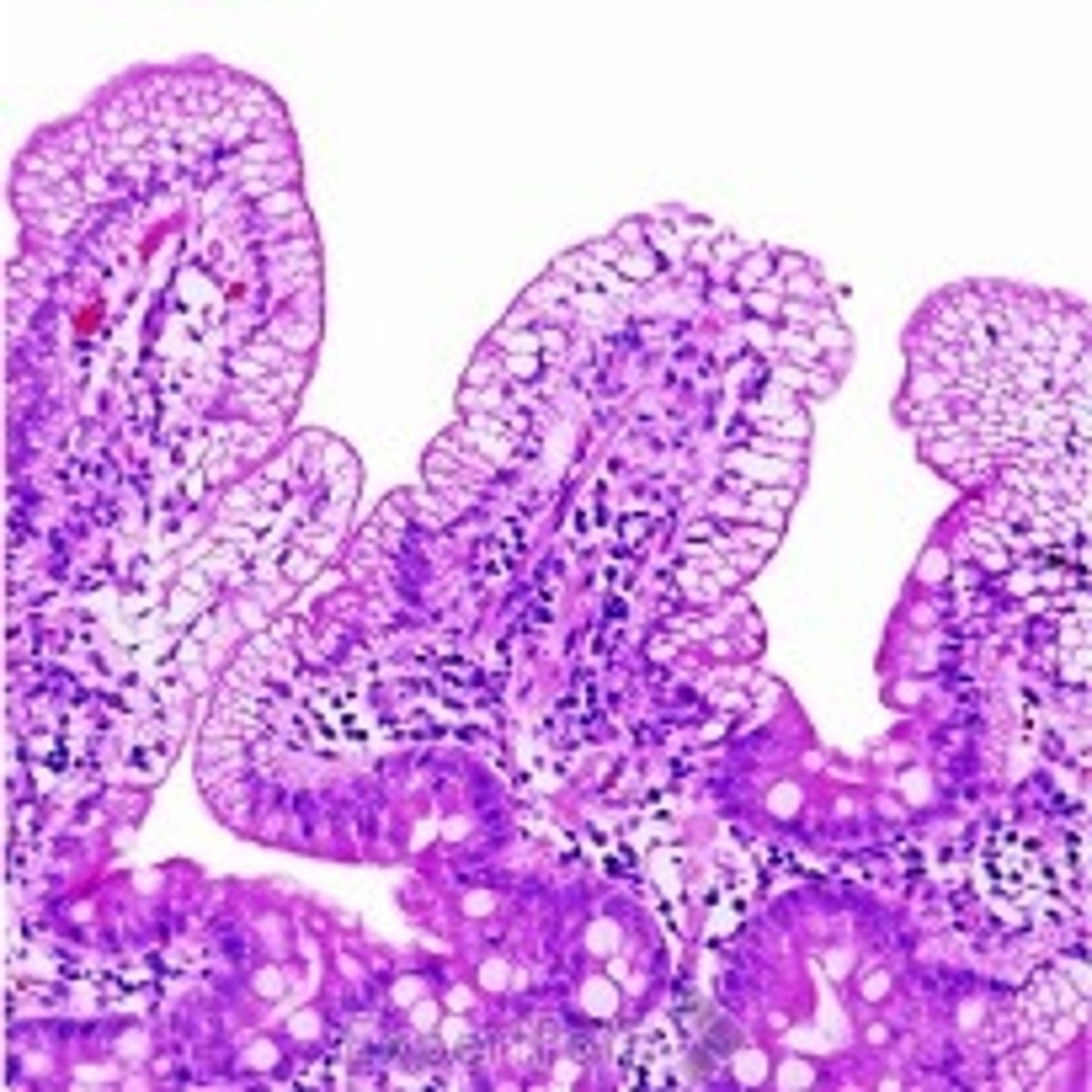
-Path: Mutation in the microsomal triglyceride transfer protein in the small intestine -> failure to properly export lipids into blood -> build-up of lipids in enterocytes which appear as lipid-filled vacuoles and fat malabsorption
-Sx/PE: (presents in Infancy)
> FTV
> Diarrhea
> Steatorrhea
> Fat Soluble Vitamin Deficiency (ADEK)
>> Night Blindness = A
>> Osteopenia = D
>> Coagulopathy = K
-Dx:
> Biopsy:
>> Vacuoles of fat in villia
> Blood Smear:
>> Acanthocytes (50% or more red blood cells) in peripheral blood d/t lipid plasma membrane defects
Carcinoid Syndrome
Define Condition:
Group of Sx occuring when tumor secretes certain chemical (serotonin) into bloodstream --> Transepithelial transport defect
-Path: Tumor secretes serotonin -> ↑ intestinal motility and excessive secretion of the GI tract
-Sx/PE:
> Chronic & Watery Diarrhea
-Prog: Fasting doesn't reduce diarrhea (increased motility and secretion are independent of intake)
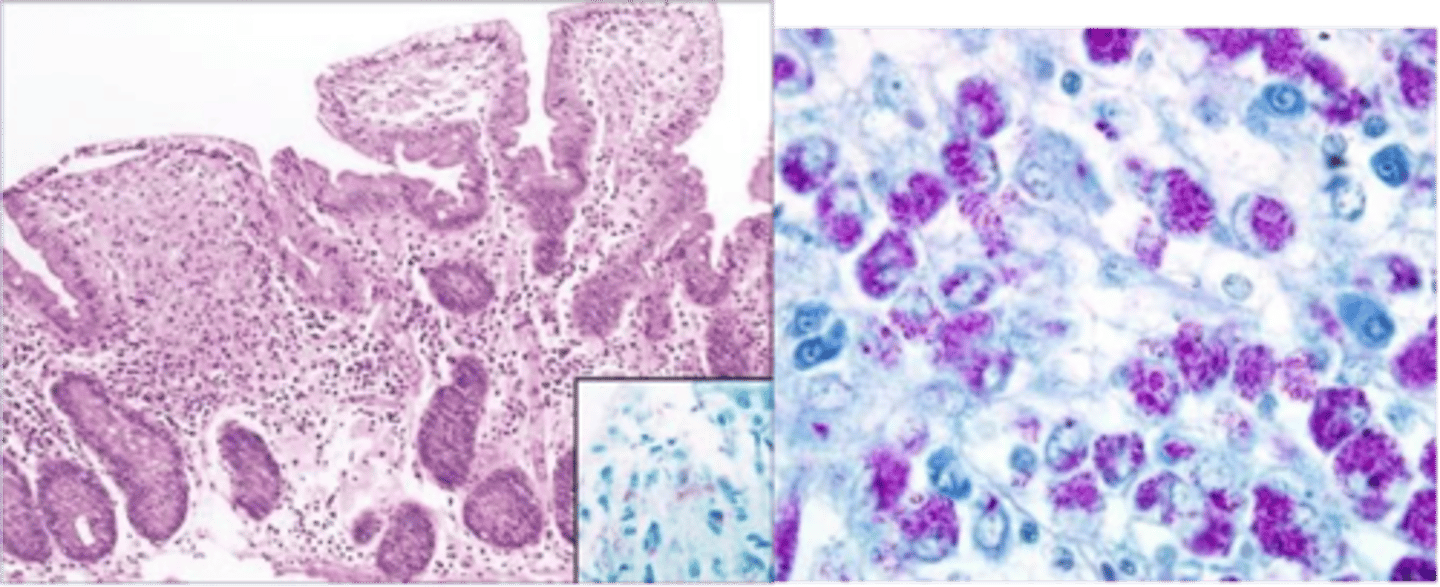
Whipple Disease
Define Condition:
Defect of lymphatic transport caused by Systemic infex d/t Tropheryma whipplei
-Hx:
> MC in Older Males (40-60 y/o) in Rural Areas
> NON-AIDS pt (AIDS = MAC)
-Path: Excess macrophages compressing lymph vessels in small bowel -> Bacteria damage the villi and cause malabsorption -> diarrhea and steatorrhea
-Sx/PE:
> Cardiac Isssues
> Arthralgias
> Neuro Sx
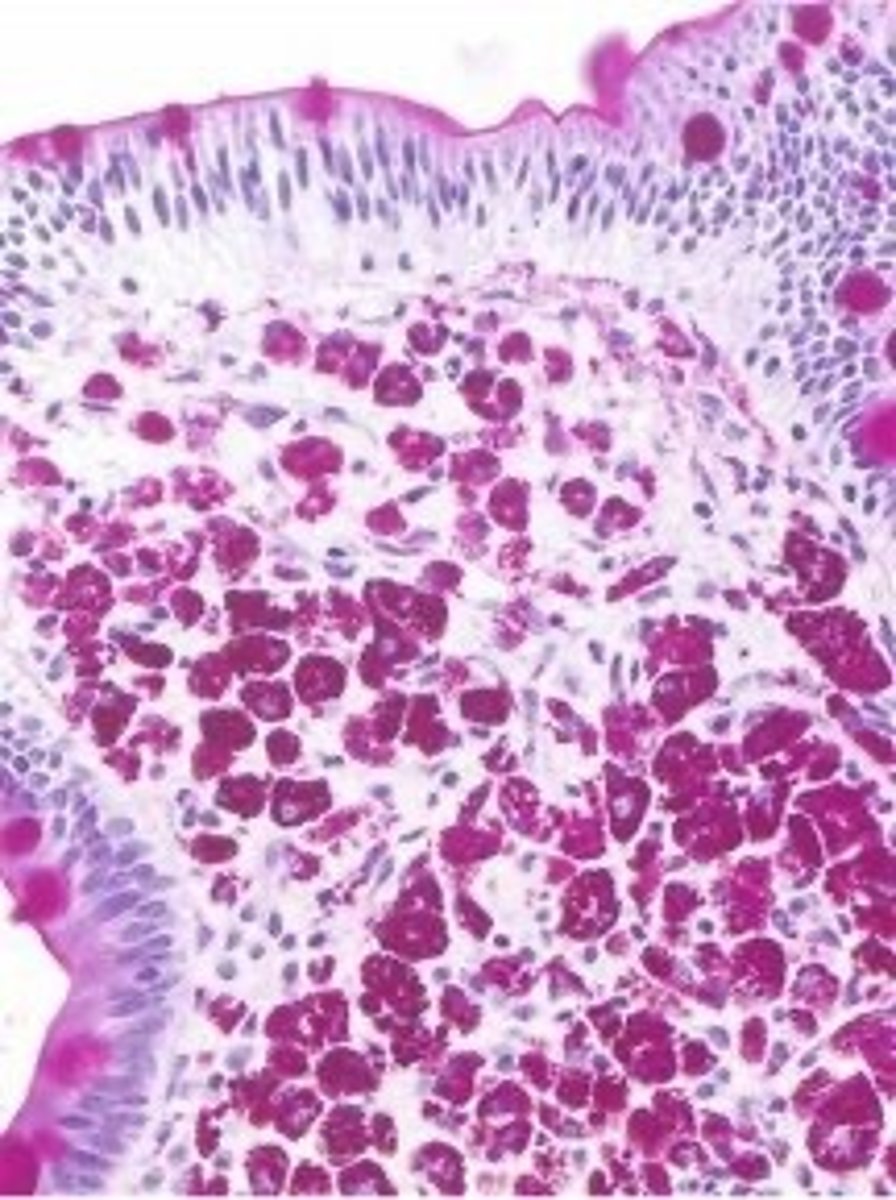
-Dx:
> Biopsy = PAS(+) Foamy (aka "STUFFED") Macrophages in intestinal lamina propria
Mycobacterium avium complex (MAC)
Define Condition:
Defect of lymphatic transport caused by Systemic infex d/t MAC (atypical mycobacterial infex/nonTB mycobacteria) made of M. avium and M. intracellulare
-Hx:
> Immunocompromised (HIV/AIDS)
-Path: MC Sites = Small Bowel & Large Bowel
-Sx/PE:
> Fever
> Diarrhea
> Malabsorption
> Loss of Appetitie
> Weight Loss
-Dx:
> Watery Diarrhea w/o fecal WBCs
> PAS (+) and diastase-resistant + (+) Ziehl Neelsen Acid Fast Stain
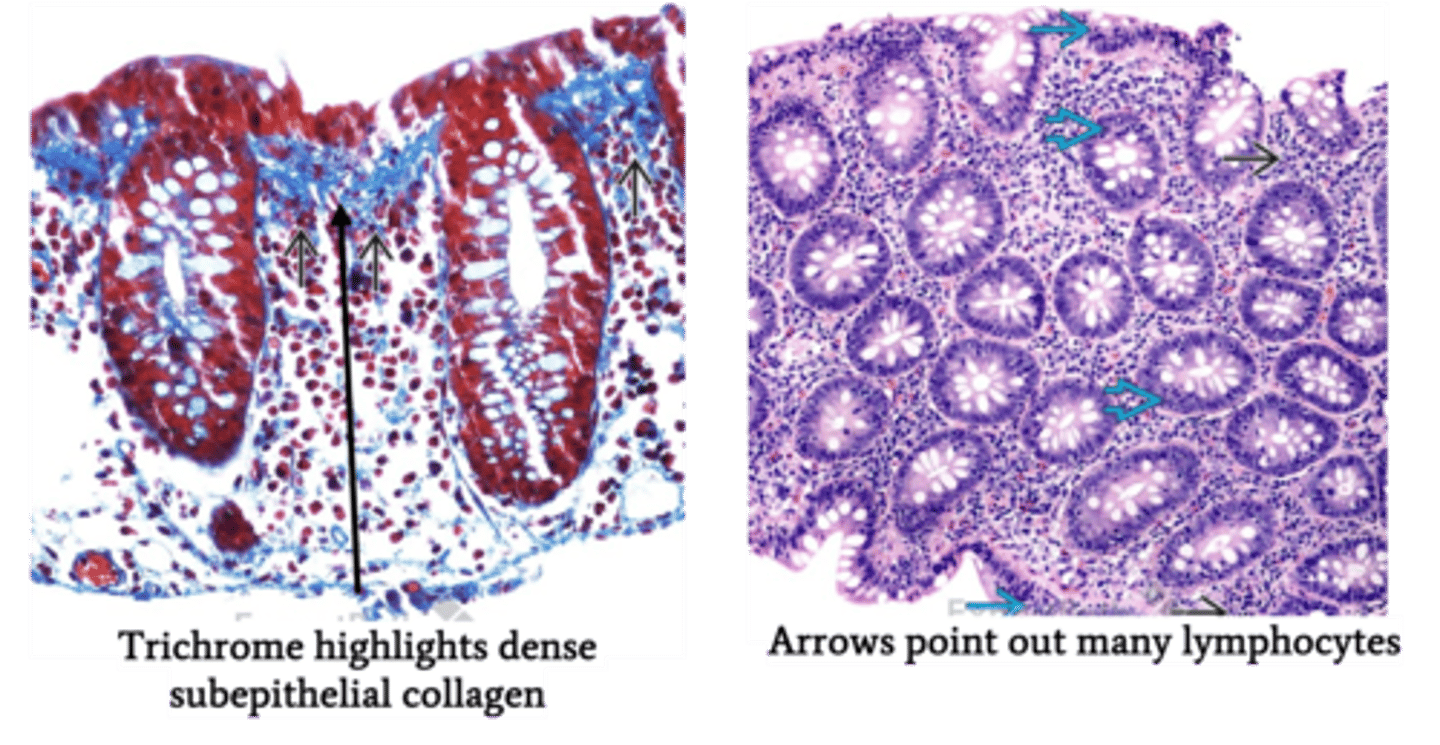
Microscopic Colitis
Define Condition:
Inflammatory disease of colon
-Hx: IDIOPATHIC
> Collagenous = Middle aged/Older Women
> Lymphocytic = A/w...
>> Celiac disease
>> Thyroiditis
>> Arthritis
>> Autoimmune Gastritis
-Sx/PE:
> Chronic Non-Blood Watery Diarrhea
> No Wt Loss
-Dx:
> Endoscopy = Normal Colonic Mucosa
Acute Graft vs Host Disease (GVHD)
Define Condition:
Immune-mediated disease due to cytokine induced damage by donor T-cells to recipient's epithelial cells after allogeneic hematopoietic stem cell transplantation
-Sx/PE: (w/n 100 days of allogenic HSC transplant) - involves upper & lower GI tract
> Watery diarrhea
> Abd Pain
> Nausea/Vomiting
> Anorexia
-Dx
> Biopsy (CONFIRM): Epithelial apoptosis