Containment - lecture 3 - control of infectious disease
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
30 Terms
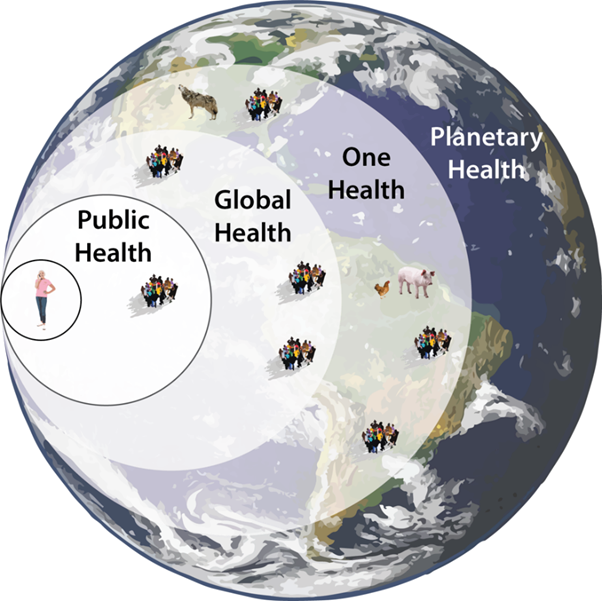
one health
human, animal and environmental
infection
when a microorganism is present in a host in placed where it is not normally found (replicating)
infectious disease
when the microorganism causes symptoms
different things that cause disease
bacteria
cholera, TB, e. coli
viruses
HIV, HPV, hepatitis
protozoa
malaria, giardia
multicellular
helminths, fungi, algae
external organisms
fleas
nonliving
prions (mad cow disease)
direct versus indirect transmission
Direct: skin skin, blood, across placenta, sneeze cough, breast milk
Indirect: food, water, vector borne
subclinical
don’t have symptoms (yet)
don’t see them as they don’t get sick but carry the disease
index case
the first case identified in the population
primary case
case that brings infection into a population
reproductive rate
how many people one person can infect
explain this type of epidemic curve
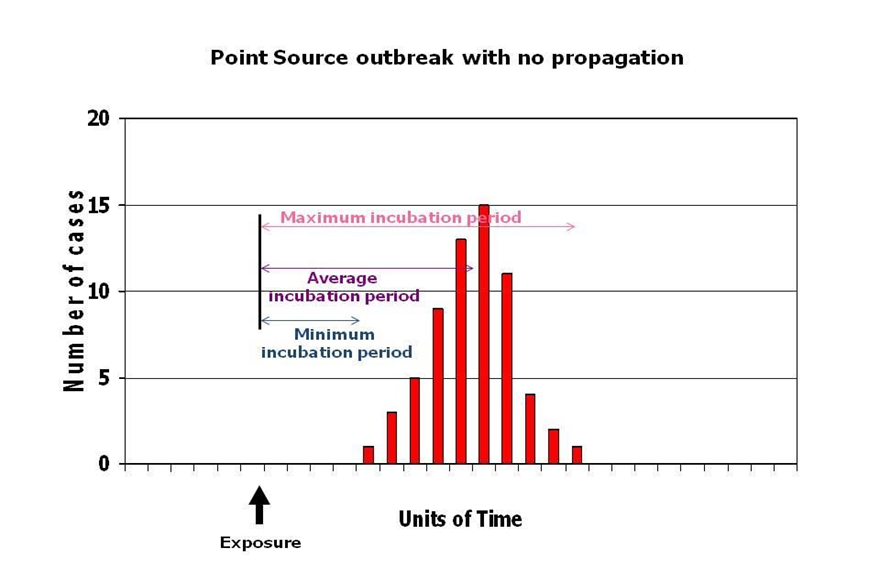
All cases are exposed to the same source at about the same time (a single exposure event).
The number of cases rises rapidly, peaks, and then falls gradually — forming a sharp, single peak.
Transmission: No person-to-person spread
Example: Food poisoning from a contaminated meal at a wedding — everyone exposed at once.
explain this type of epidemic curve
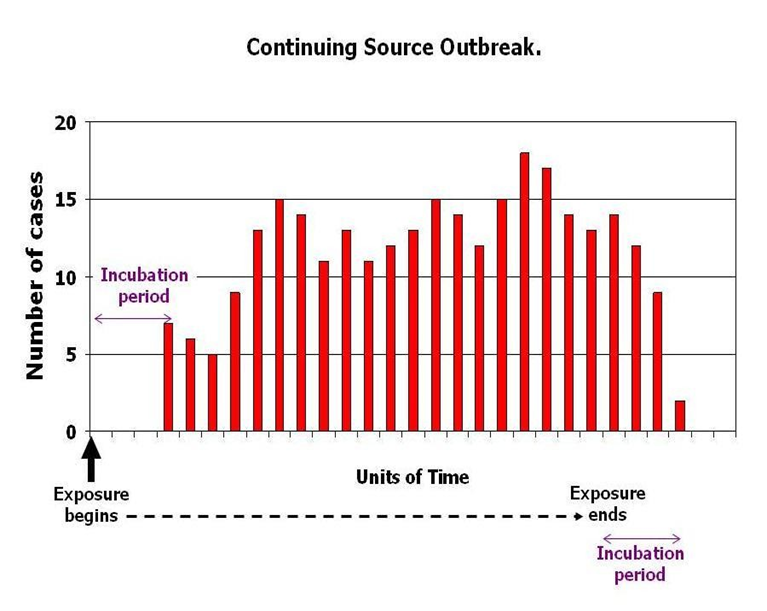
Exposure to the source occurs over a prolonged period (days, weeks, or longer).
As long as exposure continues, new cases appear.
The curve shows a plateau or broad peak rather than a sharp one
Transmission: Still from the source — not person-to-person
Example: Typhoid fever from a continuously contaminated water source.
explain this type of epidemic curve
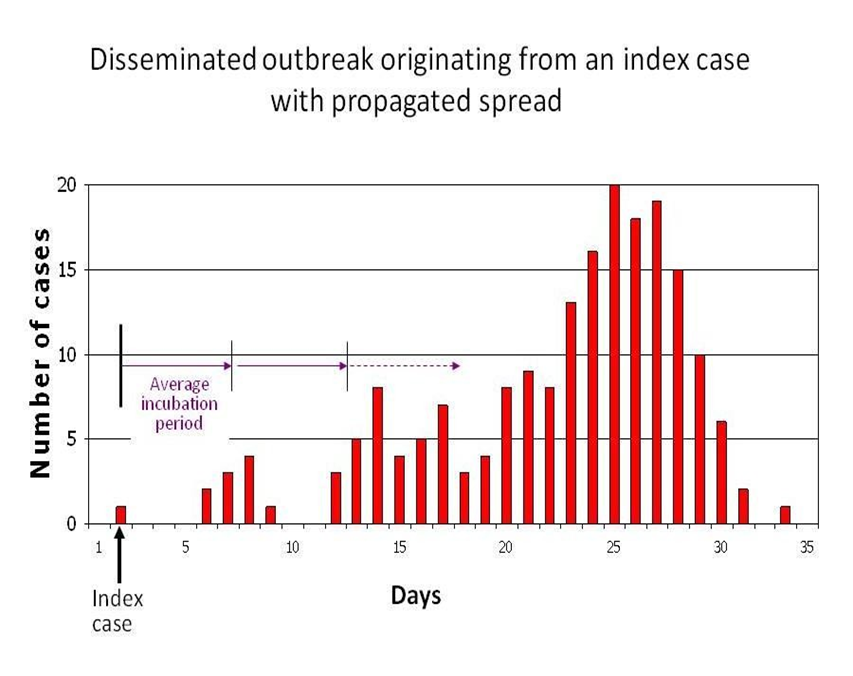
propagated outbreak
Caused by person-to-person transmission (propagation).
The curve shows successive waves, each separated roughly by one incubation period.
The first case is the index case, and secondary, tertiary waves follow.
Transmission: Person-to-person spread
Example: Measles, influenza, or COVID-19 spreading within a community.
epidemiological triangle
public health model that explains disease transmission by examining the relationship between three key components
the agent
the host
environment
adequate chain of transmission
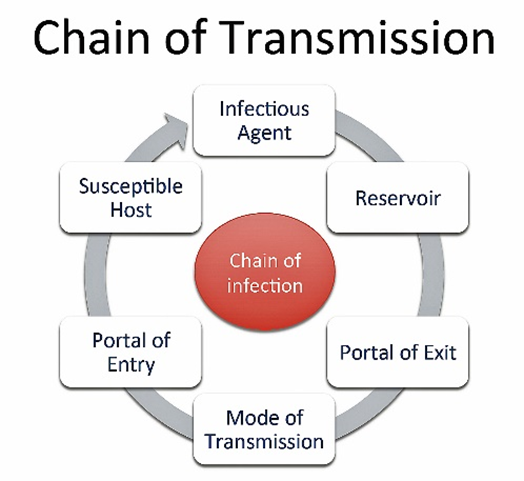
reservoir of disease very important
Types of host – humans are intermediate host of malaria!
limiting infectious disease, control, elimination, eradication
control → reduction of disease incidence, prevalence, mortality and morbidity
elimination → reduction to zero of the incidence of infections caused by a specific agent
eradication → permanent reduction of the incidence of infections worldwide
what does disease control aim to do
reduce incidence of disease
reduce duration of disease → and thus risk of transmission
reduce effects of infection
reduce financial burden
control strategies (jenkins)
problem definition
proposal development and assessment of success of implementation economic assessment
societal relevance
policy development
professional and public acceptance
political decision
public health surveillance definition and goal
definition → the systemic collection, analysis and interpretation of health data on an ongoing basis and its timely distribution to those who need to know and subsequent use of the data
goal → to prevent or control the diseases within a population by knowing and timely action.
passive surveillance
using existing routine structures to inform about infectious diseases (Stronger health system= more coverage with passive surveillance)
it is based on the data being readily available and the health care providor providing this data.
advantages and disadvantages of passive surveillance
advantage;
inexpensive
covers many diseases
allows for international comparisons
disadvantage
depended on many actors
limited access to health facilities
under-recognition of diseases (non specific symptoms)
active surveillance
based on periodic field visits to identify new cases
more expensive, difficult to develop but accurate reporting and local outbreaks are identified
advantages and disadvantages of active surveillance
advantages
reporting is more accurate
local outbreaks are generally identified
limitations
more difficult to develop for routine work
more expensive to maintain
potentially invasive of privacy
dutch public health act
contains list of notifiable diseases
contains measures (MHS/GGD) may take to control infectious disease
mayor is responsible for control actions → force measures upon patients
A1&2 → isolation of patient, examination, observation quarantine of contacts
A1 → potential pandemic threat
A2 → immediate reporting after suspected case
small pox, poliomyelitis, SARS, MERS, viral hemorrhagic fever (EBOLA)
B1 → all measures except quarantine of contacts
B2 → only exclusion from workplace
C → only advice no measures enforcable on patient
levels of prevention
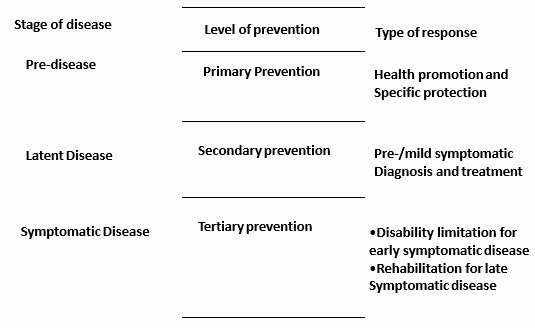
primary prevention
action taken prior to the onset of disease, which removes the possibility that the disease will ever occur.
health promotion (talking) and specific protection (eg immunization)
health promotion → the process of enabling people to increase control over the determinants of health and thereby improve their health
medical primary prevention
vaccination of risk groups
use of prophylactic medicines
MDA
expanded programme on immunization (EPI)
routine vaccinations. “cold chain problem” issues in low/middle income countries – temperature of fridges as vaccines need to be cold
MDA
issues with releasing into nature, resistance – have to be very careful
difference isolation and quarantine
isolation → seperation and restricted movement of ill people with contagious diseases. primarily on individual level
quarantine → restriction for well people, still in use for highly contagious infectious diseases (EBOLA)
secondary prevention
preventative screening
rapid tests to identify things quicker and treat quicker = prevent transmission
tertiary prevention
prevention of increasing disability and death
ART to prevent transmission of hiv