Foundations of Allied Health
1/68
Earn XP
Description and Tags
Semester 1
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
69 Terms
Principles of Infectious Diseases - Transmission
infectious disease control and prevention relies on a thorough understanding on the following factors:
agent
host
disease
environment
Mode of Transmission
direct contact
indirect contact
respiratory droplets
airborne
vector bone
faecal oral
bloodborne
vertical
Stages of an Infectious Disease
Disease Progression:
incubation period - time from exposure to signs/symptoms of the disease
clinical illness - between first and last disease signs and symptoms
Transmission Progression:
latent (pre-infectious) period time between exposure and onset of infectiousness
infectious period - the time when an infected person can transmit an infectious agent to others
Terminology/Definitions
Sporadic diseases - occasionally/unpredictable i.e. dengue fever
Endemic - predictable/regular in a population - malaria
Epidemic - acute increase above the usual/escalation or in a new population - measles
Pandemic - epidemic over a large geographic region
Principles of Infectious Diseases
Host factors - age, sex, immune status, underlying medical facto
Pathogen Factors - virulence, transmissibility and adaptability of the infectious agent
Population Factors - population density, climate, sanitation
Social Factors - cultural factors, human behaviour, policy intervention
Disease Control measures - vaccination, treatment, isolation, contract tracing
Chain of Infection
Pathogen
Reservoir or Source
Exit Portal
Route of Transmission
Entry Portal
Susceptible Host
Aim = break the chain
Hierarchy of Controls
Elimination - physically remove the hazard
Substitution - replace the hazard
Engineering Controls
isolate people from the hazard
use physical barriers and other forms of hazard reduction for example, ventilation controls, patient separation.
Administrative Controls
change the way people work
effective and consistent implementation of policies and protocols
PPE
protect the worker
review PPE policies & guidelines
minimise opportunities for infection transmission
Standard Precautions
PPE refers to a variety of barriers, used alone or in combination, to protect mucous membranes, airways, skin and clothing from contact with infectious agents
PPE used as part of standard precautions include gowns, gloves, surgical masks, protective eyewear and face shields
Selection of PPE is based on the type of patient interaction known or infectious agents, and or likely modes of transmission
Complications of Bed Rest/Immobility
Decreased mood
Confusion
Blood clots
Postural hypotension
Osteoporosis
Death
Early Mobility
Improves functional outcomes
Reduces hospital length of stays
Reduces mortality
Day 0-1 surgery, injury
As early as medically stable and safety aspects have been addressed
What can you do to minimise the risk? Step 1
Involve the patient
Involve every patient regardless of their ability to move
Involve them by:
Explaining and/or demonstrating what the patient needs to do AND what the health professional will assist with - (good understanding of the important components of the activities)
Gaining consent as a confirmation that they understand the plan
Counting to 3!
Important Components of the Sit to Stand Test
Bottom forward in chair and ankles behind the knees (higher chair is easier to stand up from)
Hip flexion (shoulders move forward or nose over toes) Arms push in chair/chair rests
Knee extension and hip extension (shoulders move upwards)
What can you do to minimise the risk? Step 2
Assistance – Factors influencing patients movements
Vital measures
Level of pain
Cognition
Strength
Balance
Range of motion
Consciousness
Levels of Assistance
Independent - the ability to mobilise without assistance, monitoring or verbal cues (with or without a gait aid) E.g. patient can perform the task safely if you weren’t in the room
Prompting/Verbal Cues/Supervision - the ability to mobilise without the need for a staff member to stand by or provide physical assistance, but prompting may be required for specific reasons. Does not require person to touch patient in any way.
Stand by Assistance - staff members stand directly beside the patient ready to assist if necessary. The person can usually mobilise with no physical assistance, but performance may be unreliable or inconsistent
Assistant - patient requires physical assistance of one or more staff members
What can you do to minimise the risk? Step 3
Prior to moving the patient, the environment needs to be modified to suit the task
Bed height/chair height
Chair position
Create space to work
Apply bed breaks
What can you do to minimise the risk? Step 4
Select the correct type of equipment to assist the transfer
Check the weight capacity to ensure it is safe to handle patient's weight
Make sure selected equipment is in good working order
HoverMatt
Reduces friction: a thin layer of air is created between the two surfaces
Appropriate for patients who need high levels of care
Assists with flat transfers (e.g. bed mobility, reclining chair)
Hoist/Lifter
Appropriate for patients who need high level of assistance
Transfers from a laying or seated position and vice versa
Standard lifters are not bariatric compatible
Ceiling hoist – takes up no floor space making it a safer workplace
Floor hoist – easy to move
Powered Standing Lifter
Appropriate for patients who can assist a bit
Has knee and back support
Transfers from sitting to standing and back to a seated position
Non-powered Standing Aid
Appropriate for patients who can assist a bit more
Has knee support
Transfers from sitting to standing and back to seated position
Wheeled Chair
A qualified health professional following with a wheeled chair is appropriate for patients who:
Have reduced endurance and may require a rest
Are getting out of bed for the first time
Slide Board
Appropriate for patients who can assist a lot
Need to be able to push through the arms and have enough trunk control to maintain upright
Used for transfers from a seated position to a seated position
Both surfaces need to be close to each other
Best to transfer from a higher height to a lower height or height that is the same
Slide Sheets
Reduces friction: 2 surfaces of the slide sheet slide over each other
Appropriate for patients who can assist
Last option for dependant patients
Not designed to assist with lifting the weight of the patient
Walk belt/Transfer Belt
Appropriate for patients who can assist quite a lot
Use for STS (hip extension) and mobility (facilitate stability)
Not designed to assist with lifting the weight of the patient
FlexiMove
Appropriate for patients who can help quite a lot
Indications: used for bed mobility, both short and long handles enable more gripping options
Two different surface materials; soiling resistant and moisture repellent nylon or soft and comfortable polyester material
What can you do to prevent risks? Step 5
Wide base of support
Toes point in the direction of movement
Knees bent
Weight close to your centre of mass (COM)
Maintain a neutral spine
Brace abdominal muscles
Understanding of loads and forces
What can you do to prevent risks? Step 6
Type 1: No skin loss
Type 2: Partial Flap Loss
Type 3: Total Flap Loss
How can you prevent a skin tear?
Perform correct patient handling techniques
No jewellery, watches or long nails
Providing Hands on Assistance
Never support a patient by grabbing their arm
Support the patients COM
Stand on patients weaker side
Good understanding of the important components of activities
How do mobility aids improve stability?
Mobility aids increase base of support
This is most evident during the single-leg stance phase of gait
By expanding BOS, the mobility aids allows the patient to keep the COM within the BOS for a greater proportion for the gair cycle
How do mobility aids decrease LL weight bearing and support LL weakness?
Mobility aids redistribute the weight placed on an injured/weak leg by putting more
weight through the aid using the upper body. Therefore, the injured leg has none/less
weight placed on it and the weak leg has less body weight it needs to support.Always remember – the injured leg goes forward with the aid
Four-point stick/quad stick
PROS (compared to SPS)
Increased stability (bigger BOS)
Stands up by itself
CONS (compared to SPS)
Wider base can be a tripping hazard
Wider base might not fit on stairs
Heavier
Unable to transfer to uneven surfaces
Forearm/elbow/Canadian crutches
PROS (compared to axillary crutches)
Able to use hands more easily
No trunk/axillary irritation
Requires less energy expenditure
CONS (compared to axillary crutches)
Requires more balance and UL strength
More costly/not readily available in some hospitals
Mobility Aid Brakes
The brakes on most mobility aids work in a similar way to a bicycle.
The brakes use a simple cable braking system to apply pressure to the brake pads on the rear wheels
The brakes are only applied to the rear wheels which means the mobility aid can still move and the brakes only slow the device down
Self-Propelled Wheelchair
Indications:
• Poor endurance – can walk but not far
distances
• LL amputation/s with prosthetics
• Significant bilateral or unilateral LL
weakness (e.g., stroke, SCI)Maintaining LL weight bearing
restrictions with another aid is
impossible
• LL and UL injury where the UL injury has
weight bearing restrictions through the
humerus (upper arm bone)
• Bilateral LL weight bearing restrictions
• Bilateral LL amputations
Assistive Technology Definition
Are tools for enhancing the independent functioning of people who have physical limitations or disabilities
Replace or support an impaired function of the user but do not change the intrinsic functioning of the individual
Matching Person & Assistive Technology
Get to know the person
Set a baseline and establish a team approach
Considerations for setting a baseline"
Functional needs, capabilities and preferences
Prior exposure to and experiences with AT
Motivation and readiness to achieve goals
Expectations, mood and temperament
Lifestyle
Understand the Environment
Cultural
Impact on family culture
Impact on cultural practice
Physical
Access and physical space to accommodate and use AT
Possibility of modification
Legislative
Disability discrimination act
Legislation impacting on access to and use of AT
Attitudinal
Support from family and peers
Expectation of AT
Economic
Access to funds
Personal funds
Consider the Technology
Appearance
Cost
Comfort
Performance
Availability
Who are AHP?
Allied health professionals are health professionals who are not part of the medical, dental, or nursing professions
Require a minimum bachelor's degree
Professions are either regulated through AHPRA or they are self-regulated
Individuals professions use different terminology (registered practitioners vs accredited professionals) to reflect their regulation, but this doesn't mean there is a difference in quality and safety
Each profession has a National Board which is responsible for overseeing education standards, managing complaints against practitioners, verifying that practitioners have met the educational standards for practice and more
Professional Identity
Professional identity is defined as "the attitudes, values, knowledge, beliefs and skills shared with others within a professional group"
Behaviour: Code of Conduct
Professions operate under continual scrutiny and development and are self-regulated accountable, and guided by a code of ethical conduct in practice decisions and actions
Shared Code of Conduct:
Safe, effective and collaborative
Aboriginal and Torres strait islander health
Respect and culturally safe practice
Working with patients
5 Key Attributes of AHPs
The possession of coherent and disciplined sets of skills, knowledge, values and professional ethics relating to a specific health service discipline
The capacity to provide quality health care/health related care such as direct treatment, assessment, primary health care, community care, health promotion
a sense of professional, community and environmental responsibilities
The capacity to work collaboratively with other health care providers
The ability to reflect on and evaluate learning, and to learn independently in a self-directed manner
Roles and Scope of Practice
Roles and Responsibilities
Specific duties and obligations that healthcare professionals are expected to fulfil in their jobs
E.g. Job description
Scop of Practice
Specific activities and procedures that healthcare professionals are authorised to perform based on their education, training
e.g. information detailing scope of practice from AHPRA
Ethical Principles
Refers to rules provided by an external social system relating to a specific group that defines right and wrong behaviours
Example of ethics or codes of conduct in workplaces – they are governed by professional and legal guidelines
Disclosing confidential information or misleading a client are some examples of a breach of ethics
Must follow the ethical code regardless of your own feelings or preferences
4 Ethical Principles
Justice – fair and equitable treatment
Autonomy – ability to make informed decisions
Beneficence – doing good
Non-maleficence – do no harm
Traditional Healthcare Team
A group of healthcare providers working independently of each other in the care of the same patient
Interprofessional Collaborative Healthcare Team
When multiple health workers from different professional backgrounds work together with patients, families, carers, and communities to deliver the highest quality of care
Interprofessional Collaborative Practice - Benefits
For healthcare provider:
A broader understanding and enriched respect of other disciplines
Opportunities for cooperative research ventures
Development of a mindset to work cooperatively
Improved role satisfaction for practitioners
Improved service productivity an use of resources
Wider base of professional experience
For the Patient:
Improved problem solving
Improved patient efficacy in self-care behaviours
Reduced hospitalisation stays
Increased use of team members to meet clients varied needs
Wider range of services can be offered
Challenges of IPCP
For healthcare provider:
Hierarchies of disciplines and team members e.g. physician dominance
Tensions related to team participation/commitment
Different knowledge base
Role confusion and blurring
Frequent rotation of some disciplines especially in rural and remote areas
For the Patient:
Different technologies
Different language and terminology
Differing knowledge base
Role confusion and blurring
Effective Teamwork - Communication (Key Element)
Communication that is relevant to the client's medical history
Communication that is consistently authentic and demonstrates trust
Active listening to team members (including the patient/family)
Communication that ensures a common understanding of care decisions (don't use discipline specific abbreviations/language)
The development of trusting relationships with clients/families and other team members
Cultural empathy for all members of the care team
Effective Teamwork - Leadership in Healthcare Team
Any team member can take on the role of the leader
Effective leaders in team-based care value all team members' potential contributions in meeting the needs of the patients and communities
Effective leadership organises the team, articulates clear goals, make decisions through collective input of embers, empowers members to speak up and challenge when appropriate
Effective Teamwork - Share the load and success
Focus on patient outcomes
Problem solve together
Be mutually accountable for the results
Share responsibilities
SMART GOALS (S - SPECFIC)
Answers the question – who, what, where and any other details
Who – the patient's name should be included in the goal
What – what specifically does the patient want to achieve?
Should directly relate to one specific activity limitation or participation restriction
Functional tasks should include the following examples (as relevant): use of assistive technology/mobility aids
Where – is there a specific location of where the goal will be achieved?
SMART GOALS (M - Measurable)
Answers the question – How? The proof of how you know if the patient has achieved the goal
SMART GOALS (A - Attainable)
With hard work, is it possible to achieve the goal by the deadline?
Challenging goals, which might be difficult to achieve (yet still attainable), tend to result in higher levels of performance
SMART GOALS (R - Relevant)
Does the goal matter to the patient? Is the goal meaningful to the patient? Is the goal something that the patient wants to work towards? Why is achieving the goal important to the patient?
The likelihood of goal achievement is increased when the goal is relevant to the patient
The therapist establishes goals in partnership with the patient to ensure the goal is relevant to them. It is important the therapist assists the patient to understand the link between the goal and the management strategies
Only the patient can determine whether a goal is worth the effort. It is the patient that must expend energy if the goal is to be accomplished. Therefore, the core content of the goal must come from the patient and must be stated in terms the patient can understand.
SMART GOALS (T - Time Bound)
When will the patient reach their goal?
Without a time-frame, there is less urgency towards achieving the goal
It is best to specify by a date, rather than by a length of a time
The therapist needs to consider factors discussed in the attainable section when determining an appropriate time-frame
The Bio-Pyscho-Social Model of Disability
The international Classification of Function, disability and health, is based on an integrated biopsychosocial model of disability where:
Bio: physiological pathology
Psycho: thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution
Social: socio-economical, socio-environmental, and cultural factors such as work issues, family circumstances and benefits/economics
What is the ICF?
ICF stands for the International Classification of Functioning, Disability and Health
The ICF defines functioning and disability as multi-dimensional concepts relating to:
The body functions and structures of people
The activities people do and the life areas in which they participate
The factors in their environment which affect these experiences
Why the ICF?
Provide a scientific basis for understanding and studying health and health-related states, outcomes, determinants, and changes in health status and functioning;
Establish a common language for describing health and health-related states in order to improve communication between different users, such as health care workers, researchers, policy-makers and the public
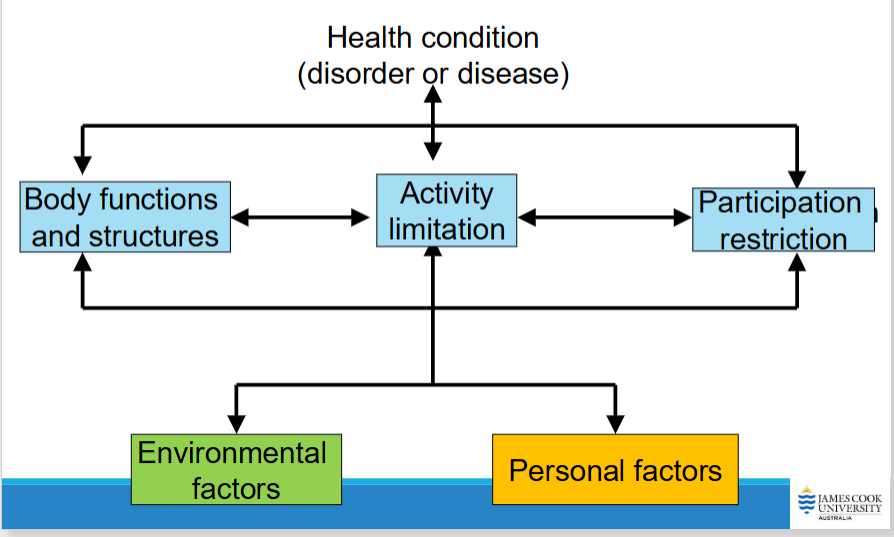
ICF Framework
ICF Terms
Health condition
Body functions (physiology) & structures (anatomy)
Impairment – primary 'damage' or 'loss'
Activity – ability to perform certain skills or tasks
Activity limitations
Participation – function level achievable; involvement in life and environment
Participation restrictions
Contextual factors – environmental and personal
Body Functions examples
Mental functions
Sensory functions and pain
Voice and speech functions
Functions of the digestive, metabolic and endocrine systems
Body Structure examples
Structure of nervous system
The eye, ear and related structures
Skin and related structures
Activities examples
Learning knowledge
Communication: speaking, writing
Self-care: showering, toileting
Participation Examples
Applying knowledge
Major life areas
Mobility in different environments
Interpersonal interactions and relationships
Environmental examples
Physical Factors:
Climate
Terrain
Building design (e.g. home workplace)
Products and technology (e.g. Bluetooth phone)
Natural environment and human-made changes to environment (e.g. roads, distance to health care)
Social Factors:
Support (emotional/physical)
Service, systems and policies
Attitudes of carers, family, community
Laws
Transportation services
Personal examples
Age
Ethnicity
Fitness
Lifestyle
Gender
Family
Access to Healthcare
'rural' community: dependent upon primary industry
'remote' location
People living in rural and remote areas often need to travel significant distances to access specific health services:
Travel and accommodation costs
Time off work/loss of income
Family disruption/care arrangements
Local services can vary according to staffing:
Recruitment/retention
Education
Educational levels can influence mode of information sharing
Diagram, drawings, pictures can all hep
More time needed in explanation
May need support personnel
Lack of educational opportunities can underpin biased views
Myth may need to be clarified
Access to internet facilities patient knowledge and expectations
Educational role in AHP services: patients need to be provided with adequate information to make an informed and collaborative decision about health management
Socio-economic factors
Treatment affordability
Public versus private systems
Equipment provision
Housing and environmental considerations
Community supports
Local council services
Government support systems
NDIS
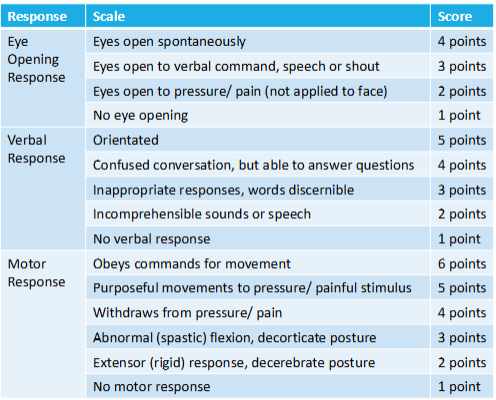
Glasgow Coma Scale
measurement of patient’s level of consciousness
completely unresponsive = 3 points
normal alertness = 15 points
minor brain injury = 13-14 points
moderate brain injury = 9-12 points
severe brain injury = 3-8 points