Psychopathology & Mental Health Exam #2
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
116 Terms
Traumatic Stress
An event that involves actual or threatened death, serious injury, or sexual violence to self, or witnessing others experience trauma, learning that loved ones have been traumatized, or repeatedly being exposed to details of trauma
Posttraumatic Stress Disorder (PTSD)
A psychological disorder characterized by recurring symptoms of numbing, re-experiencing, and hyperarousal following exposure to a traumatic stressor
Acute Stress Disorder (ASD)
Defined as a reaction occurring within four weeks of a traumatic stressor. It is characterized by dissociative symptoms, re-experiencing, avoidance, and marked anxiety and arousal.
Contrats with PTSD, which either lasts longer or has a delayed onset.
Symptoms of ASD and PTSD
(1) Intrusive Reexperiencing
(2) Avoidance
(3) Increased Arousal or Reactivity
(4) Negative Mood or Thoughts
(5) Dissociative Symptoms
Symptoms of ASD & PTSD: Re-experiencing
Intrusive, repeated, distressing memories of a trauma or reliving a trauma in horrifying dreams
Psychological/physiological distress at exposure to cues that symbolize or resemble events
Symptoms of ASD & PTSD: Exaggerated Startle Response
A symptom in which people have excessive fear in reaction to the unexpected
Symptoms of ASD & PTSD: Dissociative State
A rare case of re-experiencing where the people feel and acts as if the trauma actually were recurring in the moment
Symptoms of ASD & PTSD: Derealization
A symptom in which people have a marked sense of unreality that may continue for days or longer
Symptoms of ASD & PTSD: Dissociative Amnesia
A symptom in which people are unable to remember aspects of a trauma event
Symptoms of ASD & PTSD: Flashbacks
Sudden, repeated, and intrusive memories during which the trauma is replayed in images or thoughts; often at full emotional intensity
Symptoms of ASD & PTSD: Depersonalization
A symptom in which people feel cut off from themselves or their environment; they might feel like a robot, or as if they were sleepwalking
DSM-5 Criteria for PTSD
A. Exposure to trauma stressor
B. Experiencing symptoms from the following 4 categories of symptoms (1 or 2 from each category for a total of 6 symptoms)
i. Instruvie symptoms
ii. Persistent avoidance of stimuli associated with trauma
iii. Negative alteration in thoughts and mood associated w/ trauma
iv. Marked changes in arousal/reactivity
C. Duration of disturbance is more than a 1 month
D. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
E. The disturbance is not attributable to the physiological effects of a substance or another medical condition
DSM-5 Criteria for ASD
A. Exposure to trauma stressor
B. The presence of 9 or more symptoms from the following five categories
i. Intrusive Symptoms
ii. Negative mood
iii. Dissociation Symptoms
iv. Avoidance Symptoms
v. Arousal Symptoms
C. Duration of disturbance is 3 days to 1 month after trauma exposure. Symptoms typically begin immediately after the trauma, but persistence for at least 3 days to up to a month is needed to meet disorder criteria.
D. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
E. The disturbance is not attributable to the physiological effects of a substance or another medical condition
Prolonged Exposure Therapy
A cognitive-behavioral treatment for PTSD that involves repeatedly exposing individuals to stimuli that remind them of their past trauma in order to alter their fear networks.
Image Rehearsal Therapy
An effective form of treatment for recurring nightmares that is based on talking and in which a counselor asks a person to imagine their nightmare and then come up with a strategy to make it less scary
Eye Movement Desensitization and Reprocessing (EMDR)
A technique that involves rapid back-and-forth eye movements used to reduce anxiety.
Antidepressant Medication for PTSD
Psychiatrists may prescribe antidepressants (like SSRIs) for PTSD treatment.
The effectiveness of SSRIs is likely at least partially due to the high comorbidity between PTSD and depression.
Only 30% of PTSD patients can fully recovery from PTSD symptoms.
Dissociative Disorder
A category of psychological disorders characterized by persistent maladaptive disruptions in the integration of memory, consciousness, or identity
Hypnosis
An altered state of consciousness during which hypnotized subjects are particularly susceptible to suggestions.
There is considerable debate as to whether hypnosis is a unique state of consciousness or merely a form of relaxation.
Explicit Memory
Conscious recollection, memory of facts and experiences
Implicit Memory
Unconscious and evident only because past experiences can change behavior
Implicit Association Test
Tests that reveal implicit memories by comparing response times to different cues
Dissociative Identity Disorder (DID)
A dissociative disorder when two or more personalities within a single individual.
Demonstrates that the mind can function on multiple levels of consciousness
At least two personalities repeatedly take control over the person's behavior and some personalities have limited or no memory of the other.
Dissociative Amnesia Disorder
A type of dissociative disorder characterized by the sudden inability to recall extensive and important personal information
The onset often is sudden and may occur in response to trauma or extreme stress.
Depersonalization/Derealization Disorder
A dissociative disorder is characterized by feelings of being detached from oneself or. the world around you.
Iatrogenesis
The creation of a disorder by an attempt to treat it.
Merskey (1992) argues that DID is a social role, that highly hypnotizable people are likely to suffer from iatrogenic effects.
Anxiety
A general/diffuse emotional reaction, and is out of proportion to threats from the environment.
Anxious Apprehension
An unpleasant combination of thoughts and feelings often associated with an anxiety disorder that includes...
(1) High levels of diffuse negative emotion
(2) A sense of uncontrollability
(3) A shift in attention to a primary self-focus or state of self-preoccupation.
Worrying
A cognitive activity that is associated with anxiety, defined as a relatively uncontrollable sequence of negative, emotional thoughts that are concerned with possible future threats or danger.
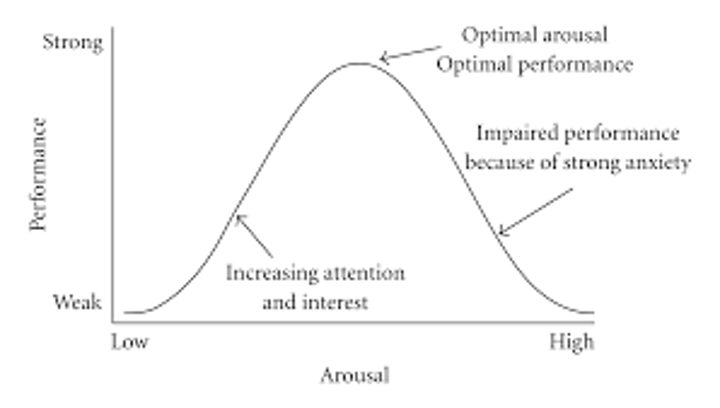
Yerkes-Dodson Law
There is an optimal level of arousal/anxiety for the best performance of any task
Low levels of anxiety can cause fatigue and unproductiveness but when anxiety exceed optimal levels can be harmful and impair performance
Panic Attack
sudden, overwhelming experience of terror, fear, or intense discomfort that reaches a peak within minutes and during which time four (or more) symptoms occur
Panic Attack Symptoms
(1) Palpitations, pounding heart, or accelerated heart rate
(2) Sweating
(3) Trembling or shaking
(4) Sensations of shortness of breath or smothering
(5) Feelings of choking
(6) Chest pain or discomfort
(7) Nausea or abdominal distress
(8) Feeling dizzy, unsteady, light-headed, or faint
(9) Chills or heat sensations
(10) Paresthesias (numbness or tingling sensations)
(11) Derealization (feelings of unreality) or depersonalization (being detached from oneself)
(12) Fear of losing control or "going crazy"
(13) Fear of dying
Situationally-Bound Panic Attack
Panic attack is associated with a certain stimuli/situation
Situationally-Predisposed Panic Attack
A person is more likely to have a panic attack where they've had one before, but having one is not inevitable
Unexpected Panic Attack
A person is likely to have a panic attack in unlikely places/times
Panic Disorder
An anxiety disorder marked by recurrent, unexpected panic attacks followed by at least one month of one or both of the following...
(1) Persistent concern or worry about how additional attacks or their consequences
(2) Significant behavioral change related to the attacks
DSM-5 Criteria for Panic Disorder
The disturbance cannot be attributed to the physiological effects of a substance
The disturbance is not better explained by another mental disorder.
At least one of the attacks has to be followed by 1 month (or more) of one or both of the following
- Persistent consent or worry about additional panic attacks
- A significant maladaptive change in behavior related to the attacks
Catastrophic Misinterpretation
Panic attacks are triggered by bodily sensation, thoughts, or images
This leads to more physical sensation, increasing negative emotions
More aware of what is going on and it is then interpretation as something catastrophic
Panic Disorder Treatment: Situational Exposures
Confronting places or situations that the person avoid due to fear of having a panic attack
Panic Disorder Treatment: Interoceptive Exposures
Confronting bodily sensations that an individual associated with panic attacks
Certain symptoms can initiate "catastrophic misinterpretation" and this form of treatment will try to trigger these symptoms to show that these stimuli will not always lead to the dreadful outcome.
Panic Disorder Treatment: Breathing Retraining
Using the diaphragm (not the chest) to take slow, deep breaths
Panic Disorder Treatment: Cognitive Reconstructing
Evaluating evidence for and against maladaptive beliefs.
Focuses on addressing the real odds and de-catastrophizing
Agoraphobia
fear or avoidance of situations, such as crowds or wide open places, where one has a fear of experiencing panic attacks and not being able to escape
DSM-5 Criteria for Agoraphobia
Symptoms need to occur for at least 6 months
Situations are avoided or endured with marked distress or require companion
Specific Phobia
Persistent and excessive or unreasonable fear related to a specific object/situation
DSM-5 Criteria for Specific Phobias
Exposure almost always provokes fear and/or anxiety
Recognizes fear is excessive and avoidance/anxiety interferes with routines or functioning or there is distress about having it
Symptoms persist for more than 6 months
Etiology of Specific Phobias
Evolutionary Adaptation: Certain things are dangerous so having a phobia (which causes you to avoid it) is evoluntariory beneficial
Negative Information: You are exposed to information about something, and that causes you to develop to a phobia of something
Classical Conditioning: Something is often paired with something negative, so you learn to fear it.
Exposure Therapy
Treatment for specific phobias.
Clients will undergo a form of relaxation, then, using a hierarchy of feared objects, they will slowly address different situations that evoke fear
Imainal: Imagining the feared situation
In Vivo: Physically being in the feared situation
Generalized Anxiety Disorder (GAD)
Persistent and uncontrollable worry, future orientated negative thoughts
People with GAD tend to experience more negative thoughts, their worries tend to be more unrealistic, and their worries tend to feel more uncontrollable
DSM-5 Criteria for GAD
A. Excessive anxiety and worry that occurs more days than not for at least 6 months about many events/ activities
B. Hard to control worry
C. Associated with 3+ symptoms
i. Restlessness/ feeling keyed up
ii. Being easily fatigued
iii. Difficulty concentrating/mind goes blank
iv. Irritability
v. Muscle tension
vi. Sleep disturbance
D. Anxiety, worry, physical symptoms cause clinically significant distress or impairment in social, occupation or other important areas of functioning
E. Not due to direct physiological or substance or medical conditions
GAD: Cognitive Vulnerability
Positive beliefs about worry
Chronic over-arousal
Intolerance of uncertainty
Focus on threat-related stimuli that may indicate future negative events
Progressive Muscle Relaxation
Part of exposure therapy and a treatment of GAD
(1) Taught to detect early signs of muscle tension
(2) Employ relaxation deepening techniques
(3) Learn to alleviate the physiological components of anxiety by interrupting the learned association between overarousal and worry
(4) Practice relaxation in the session and it at home with tapes of the session
Social Anxiety Disorder (SAD)
Characterized by the fear of being negatively evaluated by others in one or more social or performance situations
DSM-5 Criteria for SAD
A. Marked and persistent fear of one or more social situations where the person is exposed to possible scrutiny
B. Almost always provokes anxiety
C. Anxiety is unreasonable or excessive
D. People will wither avoid or suffer through anxiety
E. Fear, anxiety, or avoidance is persistent for at least 6 months
F. Causes distress or impairment
G. Not due to substance or medical condition
H. Not better explained by symptoms of another mental disorder
SAD: Cognitive Bias
Attentional Bias: People with SAD will focus on more negative cues in the environment
Maladaptive and often untrue
- Fear of positive evaluation
- Emotional dysregulation
- Internal Negative Dialogue
SAD Treatment
Cognitive reconstructing
Exposure therapy to feared social situation
Obsessive-Compulsive Disorder: Obsessions
Recurrent and persistent thought, urges or images that are experienced as intrusive and unwanted and cause anxiety and distress
Individual attempts to ignore or suppress or neutralize them with some other thought or action
Obsessive-Compulsive Disorder: Compulsions
Repetitive behavior or mental acts person feels compelled to perform in response to an obsession or according to rules applied rigidly
Behaviors or mental acts are designed to prevent or reduce anxiety or prevent some dreaded event from happening. However, the behavior is not connected in realistic way or is clearly excessive.
DSM-5 Criteria for OCD
A. Individual must exhibit either obsessions or compulsions
B. Time consuming or caused marked distress or impairments
C. Symptoms not due to substances or medications
D. Symptoms not better explained by another mental disorder.
OCD Treatment: Exposure and Response Prevention Therapy
Form of cognitive-behavioral therapy that exposures clients to their fears but prevents them from performing their compulsions.
Teached clients that they don't need compulsions ot be okay or for the things they fear to not happen
Information gathering about symptoms is essential to enable the client to be monitored effectively
The following must be identified:
- Triggers
- Obsessional intrusions
- Feared consequences
- Compulsive rituals
- Avoidance
OCD: Common Beliefs and Misinterpretations
Responsibility Exaggeration: overestimate how much accountability they have to protect others from harm
Importance of Thoughts: Belief that your obsessions reveal something about yourself
Thought-Action Fusion: People equate actions to thoughts as the same thing. The emotional reaction and mental experiences as if the action is performed.
Need to Control Thoughts: Hold the belief that they should not be thinking things at all, must have complete control over thoughts.
Major Depressive Episode
Characterized by a depressed mood with symptoms that persistent almost everyday for at least 2 weeks
Major Depressive Episode Symptoms
- Depressed mood
- Anhedonia: Loss of interest or pleasure
- Weight or appetite change
- Sleep disturbance
- Psychomotor agitation or retardation
- Fatigue
- Worthlessness or excessive guilt
- Inability to concentrate
- Thoughts of death, suicidal ideation or attempt
Persistent Depressive Episode
Characterized by a depressed mood on more days than not over a period of at least two week
Persistent Depressive Episode Symptoms
- Poor appetite or overeating
- Insomnia or hypersomnia
- Low energy or fatigue
- Low self esteem
- Poor concentration or difficulty making decisions
- Feeling of hopelessness
Major Depressive Disorder (MDD)
Mood disorder characterized by at least 1 major depressive episode that lasts at least 2 weeks
No manic or hypomanic episodes
DSM-5 Criteria for MDD
A. Five (or more) of MDD symptoms that have to include either depressed mood and loss of interest/pleasure
B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
C. The episode is not attributable to the physiological effects of a substance or another medical condition.
D. The occurrence of major depressive episode is not better explained by another mental disorder
E. There has never been a manic episode or a hypomanic episode.
Persistent Depressive Disorder (Dysthymia)
Mood disorder characterized by depressive symptoms that persistent for at least 2 years
No manic or hypomanic episodes
Symptoms cause clinically significant distress or impairment in occupational, social, or other important areas of functioning
Premenstrual Dysphoric Disorder (PMDD)
Defined in terms of various mood-related symptoms that occur repeatedly during the pre-menstrual phase of the cycle, and are diminished at the onset or shortly after menses
PMDD Symptoms
Mood Symptoms:
- Mood lability
- Irritability
- Dysphoria
- Anxiety
Cognitive Symptoms:
- Difficulty concentrating
- Feeling of being overwhelmed or out of control
Somatic Symptoms
- Lethargy
- Changes in appetite
- Sleep problems
- Join or muscle pain
- Sensation of bloating
DSM-5 Criteria for PMDD
A person must exhibit at least five symptoms and at least one of those symptoms must involve a disturbance in mood
These symptoms must have been present for most of a person's menstrual cycles in the past year
Symptoms must be associated with clinically significant distress or interference with social or occupational functioning
Manic Episodes
Periods of mania, or unusually elevated mood and extreme restlessness
Should cause impairment or hospitalization for psychotic features (delusional beliefs)
These symptoms cannot be due to the effects of a substance or general medical condition
Manic Episode Symptoms
- Elevated mood, expensive, or irritable mood
- Inflated self-esteem or grandiosity
- Decreased need for sleep
- More talkative than usual or pressure to keep talking
- Racing thoughts
- Distractibility (very high levels)
- Increase in goal-directed activity or psychomotor agitation
- Excessive involvement in pleasurable activities that have high potential for painful consequences
DSM-5 for Manic Episode
A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, last at least 1 week and present most of the day, nearly every day.
B. During the period of mood disturbance and increased energy or activity three symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior.
C. The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or other, or there are psychotic features.
D. The episode is not attributable to the physiological effects of oa substance or to another medical condition.
Hypomanic Episodes
Have symptoms same as manic episode but is shorter (at least 4 days) and the symptoms are less severe
Must be noticeable to others but does not cause impairment
NO psychotic symptoms, like delusions.
Bipolar I Disorder
A type of bipolar disorder marked by full manic and major depressive episodes
At least one manic episode. Depressive episodes are not required but could happen.
Bipolar II Disorder
A type of bipolar disorder marked by mildly manic (hypomanic) episodes and major depressive episodes
At least one hypomanic episodes and one major depressive episode
Cylcothymic Disorder (Cyclothymia)
Characterized by periods of depression and hypomania over two years
Two period with no more than 2 months without them
No history of major depressive episodes or manic episodes
Specifier of Mood Disorder: Melancholia
Used to describe a particularly severe type of depression.
Subtype of depression that is caused by different factors than those response for other forms of depression.
Melancholic features may indicate that the person is likely to have a good response to biological forms of treatment.
DSM-5 Criteria for Melancholia
A depressed patient must either
(1) Lose the feeling of pleasure associated with all activities
(2) Lose the capacity to feel better
The person must also exhibit at least three of the following
(1) The depressed mood feels distinctly different from depression a person would feel after the loss of a loved one
(2) The depression is most often worst in the morning
(3) The person awakens early, at least two hours before usual
(4) Marked psychomotor retardation or agitation
(5) Significant loss of appetite or weight loss
(6) Excessive or inappropriate guilt
Specifier of Mood Disorder: Psychotic Features
The presence of hallucination or delusions during depressive or manic episodes.
The psychotic features can be either consistent or inconsistent with a patient's mood
Specifier of Mood Disorder: Postpartum Onset
Applies to women who become depressed or manic followinf pregnancy.
This episode begins within four weeks after childbirth and must meet full diagnostic criteria for a depression.
Specifier of Mood Disorder: Rapid Cycling
A person experiences at least four episodes of major depression, mania, or hypomania within a 12 month period
Specifier of Mood Disorder: Seasonal Affective Disorder
A mood disorder that follows a seasonal pattern, there is a regular relationship between the onset of a person's episodes and the particular times of the year
This pattern must be continuous for at least two years with no other episode outside this seasonal pattern
Course & Outcome of Major Depressive Disorder
Average age of onset is in the 20s
Episodes often last much longer than two weeks
Frequently a chronic and recurrent condition
5-10% of people who have MDD go on to have a manic episode
MDD has high comorbidity with anxiety disorders like social phobia, PTSD, and GAD, as well as substance abuse
Course & Outcome of Dysthymia
Often begins in teenage years
The 10-year recovery rate was found to be 74%, however among ⅓ of them relapsed in 3 years.
Course & Outcome of Bipolar I
Average age of onset: 18-28
Long term course: recurrent
Manic episodes tend to be shorter. 60% of manic episodes happen immediately after a depressive episode.
Rapid cycling
More frequent and severe episodes compared to MDD
Course & Outcome of Bipolar II
Average age of onset: Mid 20s
Usually begins with a depressive episode
Time between episodes decreases over life
More frequent and less intense episodes
Depression Etiology
Environmental Factors
- Stressful life events
- Interpersonal factors
Biological Factors
- HPA axis
- Genetic vulnerability
- Brain function
- Neurochemical s
Psychological Factors
- Information processing bias
- Cognitive dissertations
- Ruminations
- Personality
Bipolar Etiology
Environmental Factors
- Stressful life events
- Interpersonal factors
- Schedule disruption
Biological Factors
- Genetic vulnerability
- Brain function
Psychological Factors
- Cognitive distortions
- Grandiose thinking
Social Rhythms Stability Theory
People with bipolar I have a sensitivity to things that disrupt their daily rhythm. This situation can increase the symptoms of people with bipolar I.
Cognitive Vulnerability
Depressed people often exhibit certain biases, errors, and distortions in the interpretation of events
Cognitive Vulnerabilities: Hopelessness
Refers to the person's negative expectations about future events and the associated belief that these events cannot be controlled
Cognitive Vulnerabilities: Depressogenic Attributional Style
A cognitive style that includes people who tend to explain negative events in terms of internal, stable, global factors.
Cognitive Vulnerabilities: Ruminative Style
A cognitive style that includes people who respond feelings of depression by turning their attention inward, contemplating the causes and implications of their sadness
Cognitive Vulnerabilities: Distracting Style
A cognitive style that includes people who divert themselves from their unpleasant mood
Thought Inhibition
"Inhibiting" in the processing of ideas which is subjectively perceived as foreign and unwanted
Can contribute to the maintenance of depressive episodes by preventing executive controls from shifting away from distressing thoughts.
Coyne (1976) Method
Undergrad psychology students participated in a study on the "acquaintance process".
They had to interact on the phone for 20 minutes with some from one of three groups: someone with depression, someone with a mental health disorder other than depression, and someone with no mental health disorder.
Afterwards, participants completed a questionnaire about their experience.
Coyne (1976) Result
Participants were significantly more depressed, anxious, and hostile following interaction with depressed patients than any other group
Participants were more rejecting of the depressed patients compared to any other groups
More likely to reject opportunities for future interaction if their own mood was depressed following the conversation.
Cognitive Therapy
Based on the assumption that depression will be relieved if maladaptive schemas are changed.
Cognitive therapists focus on helping their patients replace self-defeating thoughts with more rational self-statements