Athletic Training: Knee Injuries
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
16 Terms
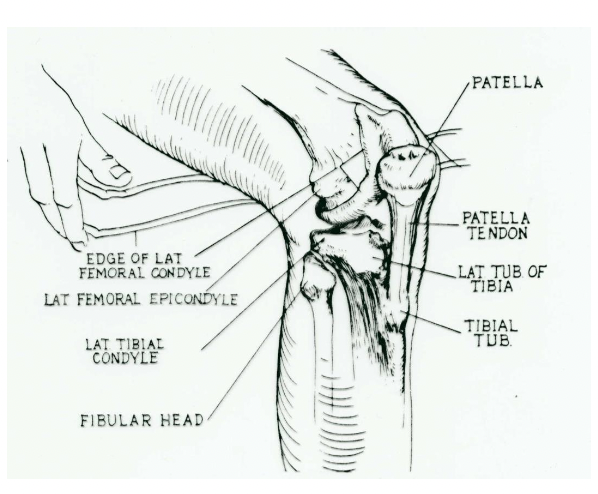
Explain some basic aspects of knee anatomy
Femoral condyles & epicondyles: medial & lateral
Patella: Femoral sulcus, patellar tendon
Tibial plateau w condyles
Tibial tubercle, fibula
Joints:
Tibio-femoral
patello-femoral
proximal tibio-fibular
Ligaments:
Extra-articular: MCL/LCL
Intra-articular: ACL/PCL
Menisci: medial & lateral
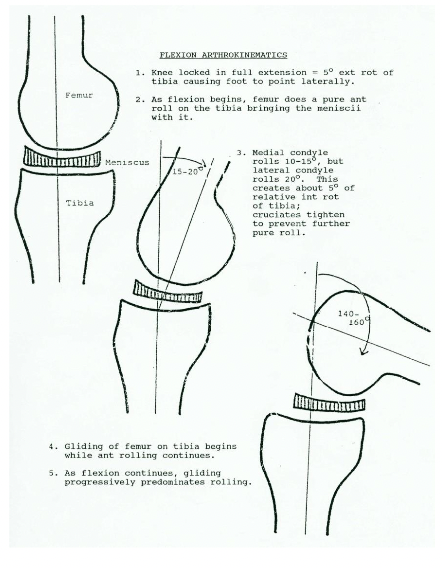
Explain knee motion: Arthrokinematics
Hinge joint
Flexion & extension (physiologic - voluntary control)
Femoral condyles roll on tibial plateaus
Accessory movement (involuntary)
Tibial plateau spins & glides/slides on femoral condyles
Explain how the Q-angle is used as a screening technique
Computed as the difference btwn:
A line drawn from the cener of the patella to the ASIS
Compared with: a line drawn from the center of the patella through the tibial tubercle
Normal = 15-20 degrees
> 20: genu valgum (knock knees)
< 15: genu varum (bow legs)
Excessive Q-angle is thought to be a risk factor for knee injury
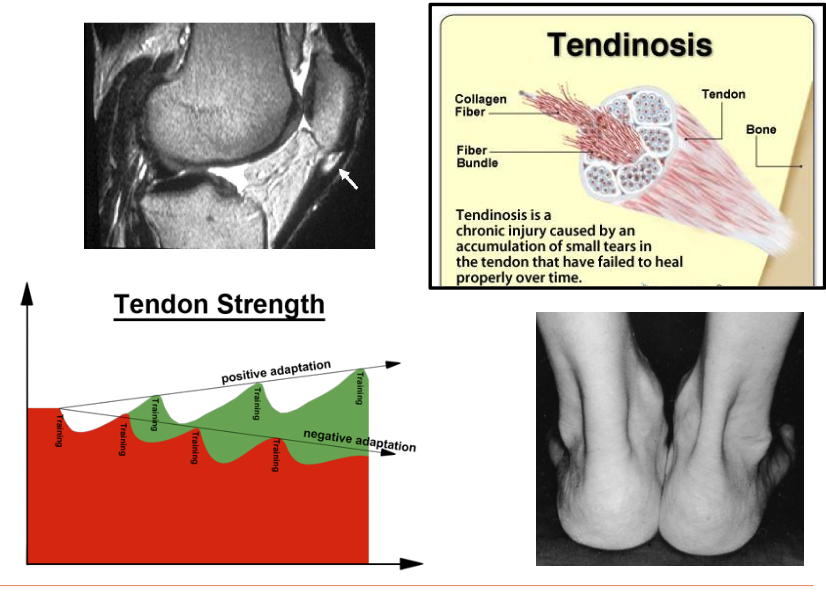
Explain Patellar Tendon-related injuries that cause anterior knee pain
Not tendon “itis”, -osis (degenerative changes) or -opathy (symptomatic)
MOI: jumping/landing activity: eccentric loading
S/S: point tender over tendon, proximal, mid-substance, distal, quadriceps weakness, pain upon loading quads
Risk factors: Limited dorsiflexion, muscle weakness (gluteals), tightness of quads, hamstrings and calves
4 stages based on duration of symptoms
1: pain after activity, w/o functional limitation
2: pain during & after activity, w/o functional limitation
3: prolonged pain during & after activity, w functional limitations
4: complete tendon tear, requires surgical repair
Possible Degenerative changes
Chronic attenuation
Loss of tensile stregth
Mucoid (pockets of fluid, gel like
Thickens: Fatty infilitratioon, calcification
Management: Strengthen quadriceps (eccentric loading), Cho-pat strapping
Explain this condition: Osgood-Schlatter's Disease
Traction apophysitis
Adolescent condition
Outgrow of bone from tibial tuberosity
Avulsion fracture, separation of TT
Growth disorder: asymmetric, bone > muscle
Explain this condition: Chondromalacia Patellae
Degenerative softening or wearing away of the articular cartilage underneath patella
Compression & shear forces
Irritation and exposure of free nerve endings
MOI: excessive Q-angle, abnormal tracking of patella
S/S: pain during patellar motion (quad activity)
Explain this injury: Patella Dislocation/Subluxation
Risk factors: excessive q-angle (lateral pull), quad weakness, joint laxity (loose ligaments)
MOI: direct blow to the knee, quick start or cutting motion when running
Tear of the medial retinaculum or medial patello-femoral ligament (MPFL)
S/S: pain and abnormal movement about patella, patella may be out of place or spontaneous reduction, extreme pain along medial aspect of patella, athlete may report that the knee "gave out"
Management: PRICE, immobilize leg, refer for x-ray and reduction
May become chronic on acute w recurrent episodes

What are the benefits of Patellar Bracing
#1 benefit is to prevent abnormal tracking of patella
Secondary beefits: prevent lateral displacement, control patellar tracking during activity, maintain normal sliding motion

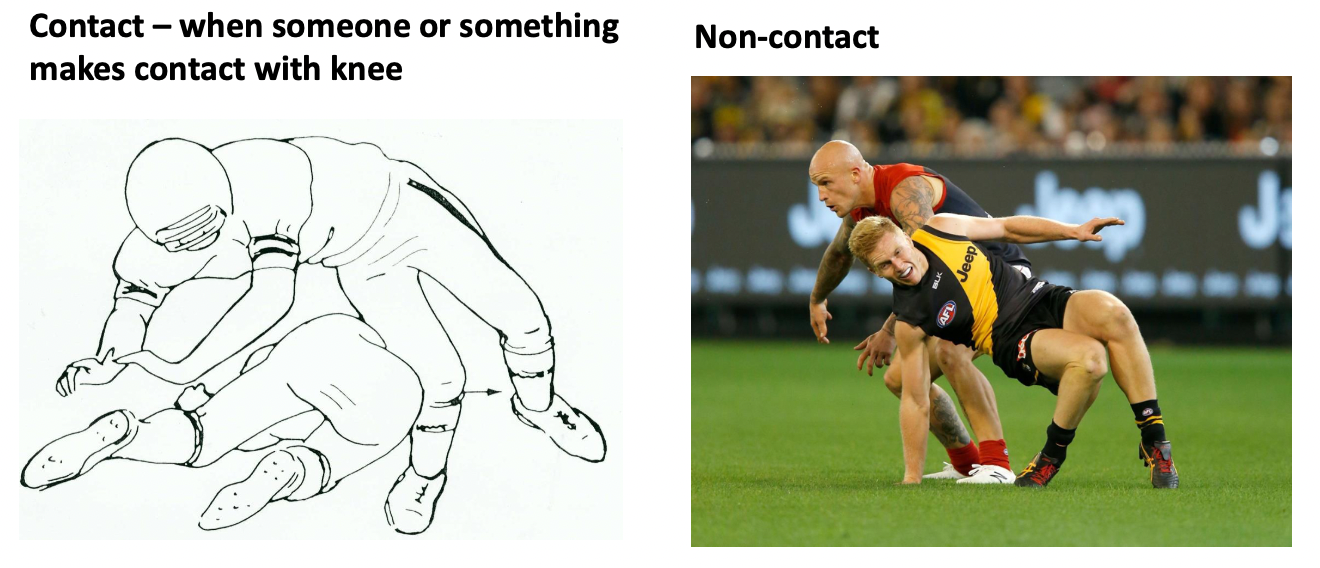
Explain this Injury: MCL tear
MOI: valgus loading of the knee in extension, contact vs non-contact knee mechanism
MCL is primary restraint to valgus loading (ACL is secondary)
Most frequent injured knee ligament
S/S: point tender and pain over MCL upon palpation or hyperextension, swelling of medial knee, athlete states knee feels "stiff", felt and/or heard a snap or pop
Immediate and short-term care: PRICE, place athlete on crutches, treat conservateively
Special test: Valgus stress teast; open up medial compartment of knee, bilateral comparison
Explain this injury: ACL tear
contact vs non-contact mechanisms
ACL is watchdog of knee → major static stabilizer
MOI: valgus loading w tibial rotation; and or/ anterior tibial displacement (driven forward), or hyperextension
Prevalence:
25%: damage is isolated to ACL
60%: meniscal damage (medial and/or lateral)
30%: articular cartilage damage
30%: damage to collateral ligaments, joint capsule, or a combination of injuries
S/S: heard/felt pop, rapid hemarthrosis: swelling in joint (golden period), stiff, warm and extremely painful
Hemarthrosis: joint inflammation followed by muscle guarding (protective spasm)
Golden peiod: 15-30 min window
Surgical reconstruction for athletes: restores stability
Conservative management: Not very effective → chronic ACL deficiency: knee gives out or buckles during tibial rotation
Special Test: Lachman Test, knee @ 30 degrees flexion, grasp femur and tibia, displace tibia anteriorly, bilateral comparison, amount of movement?
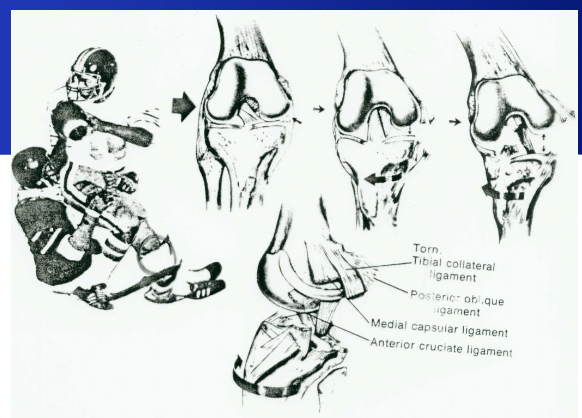
Explain what is the unhappy or terrible triad
3 structures damaged
MCL rupture: Valgus loading tibia rotates outward
Meniscus (lateral) tear: Compression of postero-lateral tibio-femoral compartment → valgus collapse, femoral plateau contusion
ACL rupture: tibial rotaion and anterior displacement on femur
Explain the different theories for the gender or sex bias for ACL tears
Anatomic: excessive Q-angle
Hormonal: menstrual cycle release of relaxin, progesterone decrease tensile strength of CT
Neuromuscular: slower muscle activation patterns (diminished dynamic stability)
Genetic predisposition (collagen gene malfunction): waker collagen → decreased tensile strength
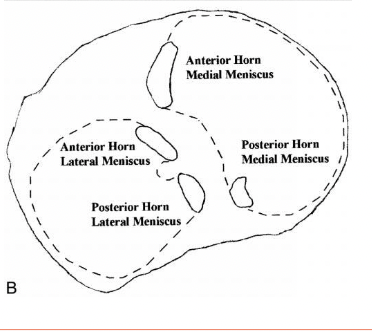
Explain the functional anatomy of the meniscus
Structure: semilunar wedges
Fibrocartilage
Circumferential fibers (outside run longitudinally)
Radial fibers (inside to outside)
Blood vessels penetrate the outer third
Functions:
Load bearing → absord and distribute loads (contact forces) over the articular surface
stability to joint by increasing fit and resisting AP displacements
Proprioception (sense position awareness and motion)
Anatomy:
Medial: C-shaped
Lateral discoid (more mobile)
Stability:
Anterior: transverse ligaments
Coronary (menisco-tibial ligaments
MCL and capsular attachments
Horn attachments: root ofr spine
Posterior-menisco femoral ligaments
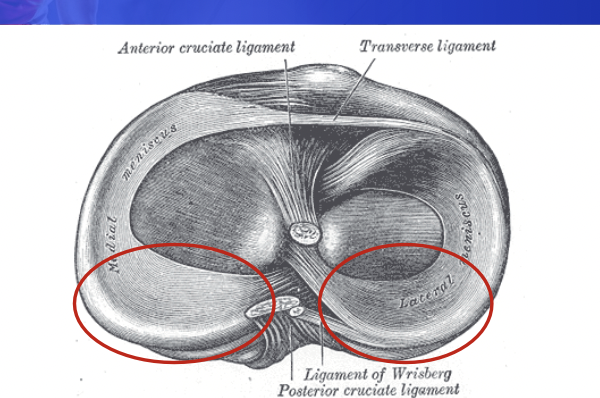
Explain this injury: Meniscal tears
Meidal meniscus is less mobile and more often torn in ACL deficient knee
Location of most tears: posterior horn of meniscus (red circles)
MOI: tears occur when knee is flexed and rotated
Forces:
Compression: condyles on plateau
Shear: AP displacement
Tensile: stretch out
Tears include radial or oblique, longitudinal or cleavage plane (internal)
Avulsion from root (spine)
Healing & repair:
Outer 1/3 may repair itself w surgery
Hypovascular: no repair (degenerates)
Meniscetomy: removes loose fragments, trimmed
Repair: sutured
S/S: joint line tenderness: posterior horn region, slow effusion (delayed swelling) hypovascular, limited ROM, popping, clicking or locking sensation, narrowing of joint space: reduces funciton
Special Tests: Appley's Compression, McMurray's
Explain this injury: PCL
PCL is larger and stronger than ACL
Does not provide rotary stability for knee because it is more vertically aligned
Prevents posterior displacement of tibia
MOI: knee flexed, tibia driven posteriorly (dashboard injury), or hyperextension, isolated or combined w damage to postero-lateral corner, joint capsule and arcuate complex
Special Tests: posterior drawer, displacement of tibia posteriorly, external rotation recurvatum (hyperextension
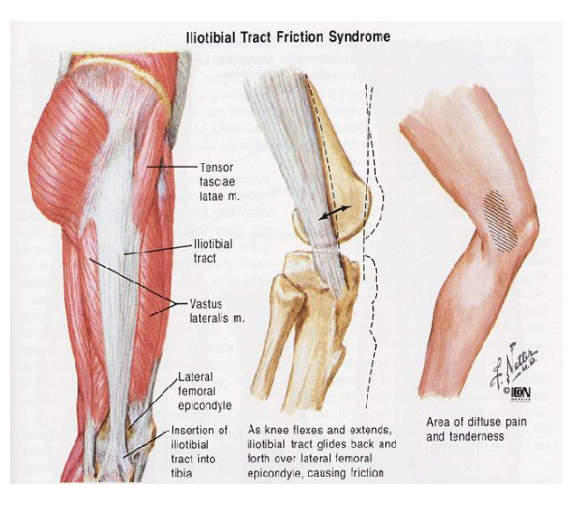
Explain this injury: Ilio-Tibial band friction syndrome (ITBFS)
Ilio-tibial band: thick band of CT (fascia)
Gerdy's tubercle: attachment point on lateral tibia
MOI: Overuse (compression & shear forces)
Lateral epicondyle of femur
Friction @ 20-30 degrees
S/S: lateral knee pain w running, point tender, swelling
Risk factors: Excessive Q-angle, tightness, excessive running
Pathophysiology: friction irritates ITB, lateral synovial recess (bursae), bursitis: inflammation