[OB FINAL] 1/5 (Exam 1 Content)
1/536
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
537 Terms
5 P’s of Labor Explained in 5 Minutes
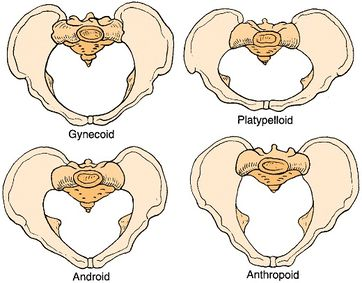
Gynecoid: Pumpkin shape (best prognosis)
Anthropoid: Human-face shape (decent prognosis)
Android: Alien-face shape (poor prognosis, leads to C/S)
Platypelloid: Flat shape (poor prognosis, leads to C/S)
“We love to give birth to PUMPKINS (BABIES) and ANTHROS/HUMANS, not ANDROIDS/ALIENS and PLATYPUSES”
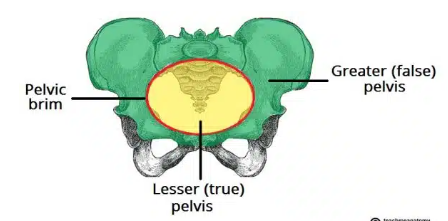
Passageway (aka highway)
Presentation: Body part reaching inlet first
Lie: Spinal axis relationship
Attitude: Flexion (Angry!) vs Extension (Excited!)
Position: Pelvis spine axis relationship (LOA, LOP, etc)
Station: How far down birth canal and which part
Passenger (fetus and placenta)
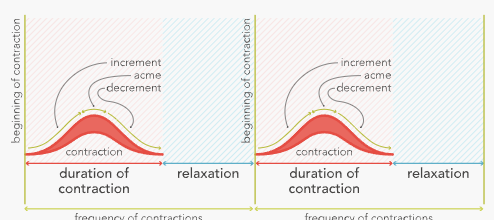
Powers (UCs: Duration, Frequency, Intensity)
Position (Maternal adjustments)
Psyche (Maternal Emotions)

Performing Leopold’s Maneuvers
1st: Check for baby’s head/butt
Form triangle, face mom’s face, feel fundus
Head = Firm, hard, moves independently
Buttocks = Squishy, moves with body
2nd: Check for baby’s back
Press lateral side of abdomen
Back = Flat, long, firm, smooth
Extremities = Small, bent
Side where fetal heart monitor placed (most accurate)
3rd: Check if baby part (e.g., head) is in pelvic outlet (engaged)
Form L, place near symphysis pubis, try lifting baby’s part up (e.g., head)
Cannot lift baby head = engaged
Can lift baby head = not engaged
4th: Check for baby’s position (cephalic prominence)
Face mom’s feet, palpate upward lateral sides of abdomen
Expected: Brow (cephalic prominence) on opposite side of back
Not always used d/t ultrasounds on most units
https://www.youtube.com/embed/5K-ERuVrvj4?si=EaxldjGDVvR9gadf
Delineate the procedure for performing Leopold’s maneuvers and the information obtained.
1st Leopold Maneuver
Checks for baby’s head/butt
Form triangle, face mom’s face, feel fundus
Head = Firm, hard, moves independently
Buttocks = Squishy, moves with body
Determines shape, size, consistency & mobility of presenting part
2nd Leopold Maneuver
Checks for baby’s back
Press lateral side of abdomen
Back = Flat, long, firm, smooth
Extremities = Small, bent
Side where fetal heart monitor placed (most accurate)
Determines fetal back & side.
3rd Leopold Maneuver
Checks if baby part (e.g., head) is in pelvic outlet (engaged)
Form L, place near symphysis pubis, try lifting baby’s part up (e.g., head)
Cannot lift baby head = engaged
Can lift baby head = not engaged
Determines what fetal part is lying above the pelvic inlet
4th Leopold Maneuver
Checks for baby’s position (cephalic prominence)
Face mom’s feet, palpate upward lateral sides of abdomen
Expected: Brow (cephalic prominence) on opposite side of back aka flexion
Determines fetal attitude (extension vs flexion)
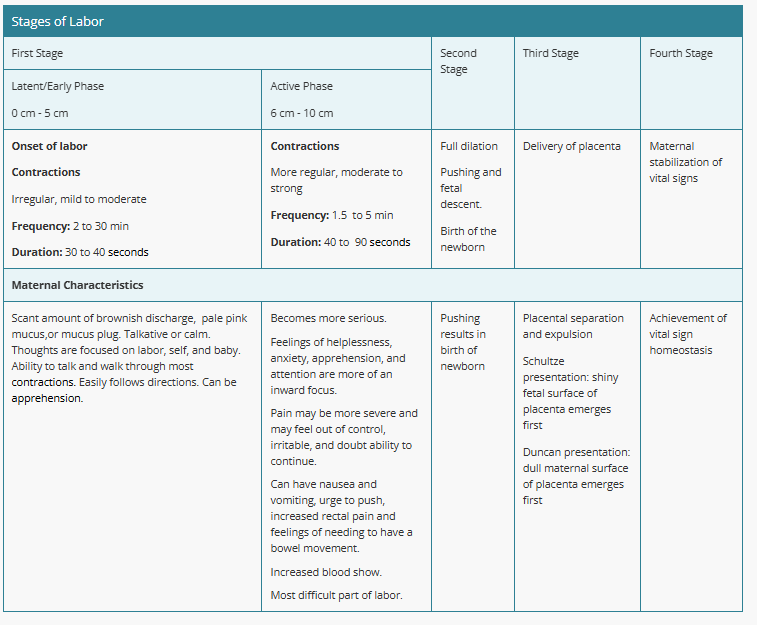
Stages of Labor (Image)
First Stage
Phases:
Latent/Early Phase (0-5 cm):
Contractions: Irregular, mild to moderate
Frequency: 2-30 minutes apart
Duration: 30-40 seconds
Maternal Characteristics:
Scant brownish or pink discharge, mucus plug
Talkative or calm, focused on labor and baby
Able to walk through contractions, follows directions
May feel apprehension
Active Phase (6-10 cm):
Contractions: More regular, moderate to strong
Frequency: 1.5-5 minutes apart
Duration: 40-90 seconds
Maternal Characteristics:
More intense emotions (anxiety, helplessness)
Pain feels severe, may feel out of control
Nausea, vomiting, rectal pressure, urge to push
Increased blood flow
Considered the most difficult part of labor
Second Stage
Key Features:
Full dilation (10 cm)
Pushing and fetal descent
Results in the birth of the baby
Maternal Characteristics:
Active pushing
Feelings of exhaustion and determination
Third Stage
Key Features:
Delivery of the placenta
Placental separation:
Schultze Presentation: Shiny fetal surface of the placenta comes out first
Duncan Presentation: Dull maternal side of the placenta emerges first
Fourth Stage
Key Features:
Maternal stabilization of vital signs
Goal: Achievement of homeostasis
Compare and contrast the physiologic and psychologic changes occurring in each of the stages of labor.
Chapter 11/14 Hiighlights
QPCC
An intrapartum nurse should assess maternal and fetal well-being during labor, including determination of labor, the progress of labor, and psychosocial and cultural factors that affect labor.
Promote baby-friendly activities between the family and the newborn, which facilitates the release of endogenous maternal oxytocin. Examples of such activities include introducing the parents to the newborn and facilitating the attachment process by promoting skin-to-skin contact immediately following the birth. Allow private time and encourage breastfeeding.
QS
Immediately following the rupture of membranes, a nurse should assess the FHR for abrupt decelerations, which are indicative of fetal distress to rule out umbilical cord prolapse.
Group B streptococcus: Culture is obtained if results are not available from screening at 36 0/7-37 6/7 weeks for screening patients.. If positive, an intravenous prophylactic antibiotic is prescribed
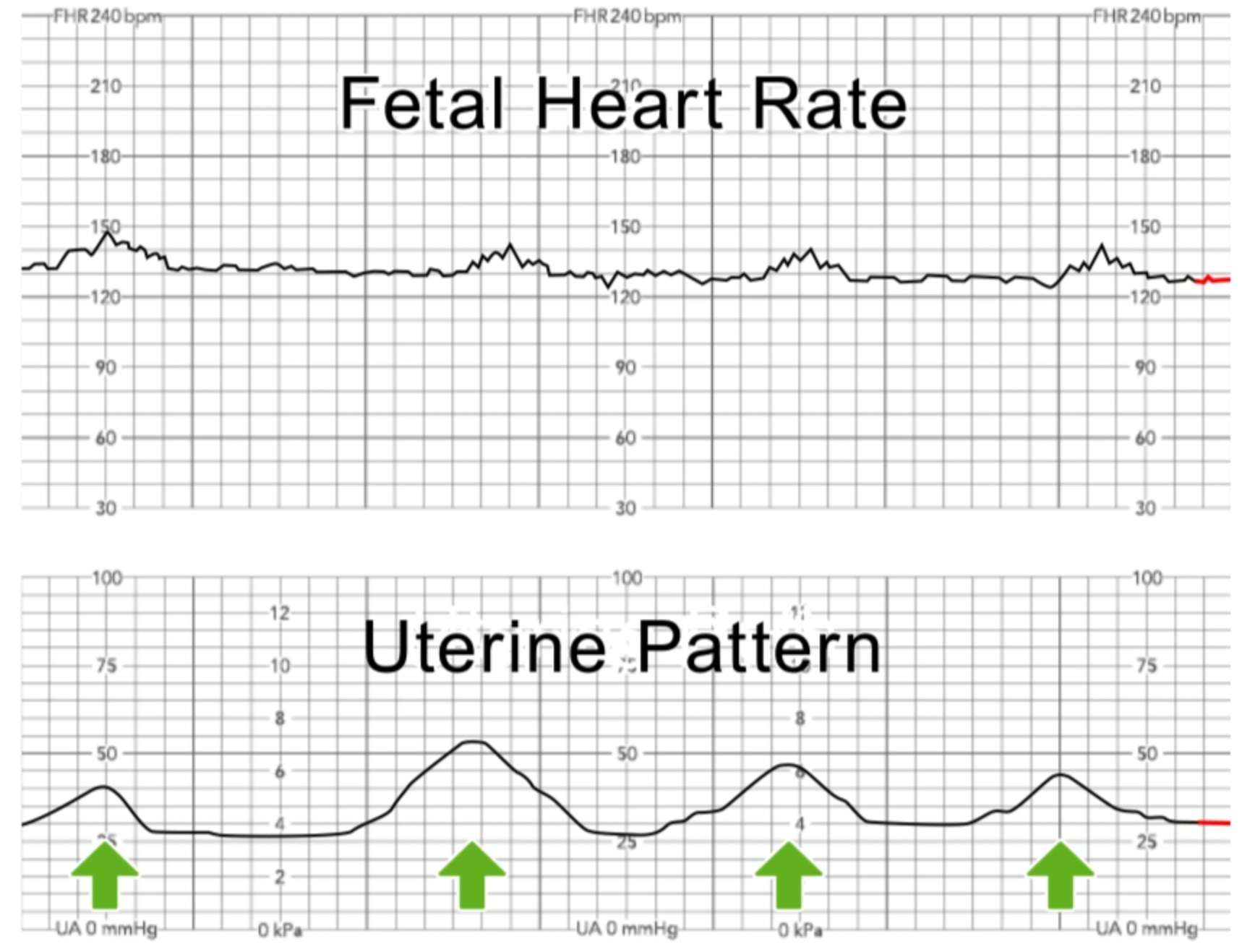
Resting tone of uterine contractions: Tone of the uterine muscle in between contractions. A prolonged contraction duration (greater than 90 seconds) or too frequent contractions (more than five in a 10-min period) without sufficient time for uterine relaxation (less than 30 seconds) in between can reduce blood flow to the placenta. This can result in fetal hypoxia and decreased FHR.
When there is suspected rupture of membranes, first assess the FHR to ensure there is no nonreassuring fetal status caused from possible umbilical cord prolapse, which can occur with the gush of amniotic fluid.
During Stage 4, massage the uterine fundus and/or administer oxytocics to maintain uterine tone and to prevent hemorrhage
First Stage of Labor (1 of 4)
Latent/Early Phase (0-5 cm):
Contractions: Irregular, mild to moderate
Frequency: 2-30 minutes apart
Duration: 30-40 seconds
Maternal Characteristics:
Scant brownish or pink discharge, mucus plug
Talkative or calm, focused on labor and baby
Able to walk through contractions, follows directions
May feel apprehension
Active Phase (6-10 cm):
Contractions: More regular, moderate to strong
Frequency: 1.5-5 minutes apart
Duration: 40-90 seconds
Maternal Characteristics:
More intense emotions (anxiety, helplessness)
Pain feels severe, may feel out of control
Nausea, vomiting, rectal pressure, urge to push
Increased blood flow
Considered the most difficult part of labor
Two phases
Latent/Early Phase Main Characteristics (1st Stage)
0-5 cm dilation
UC Q2-30, 30-40 secs
Talkative or calm
Able to walk and follow directions
Educate breathing techniques
Assess cervical dilation, pain, maternal/fetal condition
IV pain medication usually administered
Active Phase Main Characteristics (1.5 Stage)
6-10 cm dilation
UC Q1.5-5, 40-90 secs (strong)
Intense emotions (anxious/scared)
PAIN, N/V, Pressure, Urge to Push
Second Stage of Labor (2 of 4)
Key Features:
Begins with full dilation (10 cm)
Pushing and fetal descent
Ends with the birth of baby
Maternal Characteristics:
Active pushing
Feelings of exhaustion and determination
Ensure sterile room, equipment, supplies
Prepare radiant heat warmer and neonatal emergency equipment
Continue assessing fetal/maternal VS and condition
Support mother’s bearing down efforts
Third Stage of Labor (3 of 4)
Key Features:
Begins with birth of baby
Ends with the delivery of placenta
Placental separation:
Schultze Presentation: Shiny fetal surface of the placenta comes out first
Duncan Presentation: Dull maternal side of the placenta emerges first
Oxytocic medications available AFTER expelling placenta
Prevents Postpartum Hemorrhage (PPH)
Uterus must contract and narrow open blood vessels where placenta was attached
Ensures Complete Placental Expulsion
Uterus can contract strongly and expel any remaining placental fragments
Prevents Trapping the Placenta (aka retained placenta)
Promotes Uterine Recovery (prevents atony)
Why are oxytocic (uterine contraction) medications given AFTER stage 3 (placental delivery)?
Prevents Postpartum Hemorrhage (PPH)
Uterus must contract and narrow open blood vessels where placenta was attached
Ensures Complete Placental Expulsion
Uterus can contract strongly and expel any remaining placental fragments
Prevents Trapping the Placenta (aka retained placenta)
Promotes Uterine Recovery (prevents atony)
Fourth Stage of Labor (4 of 4)
Key Features:
Maternal stabilization of vital signs
Goal: Achievement of homeostasis
Factors Affecting the Delivery
Fetus
Size
Position
Presentation
Mother
Adequate pelvis size
Contractions
Pushing effort
Other
Maternal anesthesia
Premonitory
(adjective) something gives a warning or feeling that something unpleasant is going to happen
Premonitory signs refers to physiologic changes BEFORE/PRECEDING labor (e.g., back pain, weight loss, contractions, lightening, etc)
Physiologic changes preceding labor (premonitory signs)
1. Low Backache (constant, dull)
Caused by pelvic muscle relaxation.
2. Weight Loss (0.5 to 1.5 kg (1 to 3.5 lbs))
Hormonal changes lead to fluid shifts and loss of water
3. Lightening (Baby Drops)
The fetal head descends into the pelvis (usually about 14 days before labor in first-time pregnancies).
Symptoms: Easier breathing, but increased pressure on the bladder, causing frequent urination.
Note: More noticeable in first pregnancies (primigravida).
4. Irregular Uterine Contractions (Braxton Hicks)
These "practice" contractions gradually become stronger, more frequent, and regular.
5. Increased Vaginal Discharge/Bloody Show
Expulsion of the cervical mucus plug.
Appearance of brownish or blood-tinged mucus, signaling the start of cervical dilation and effacement.
6. Energy Burst ("Nesting Instinct")
A sudden surge of energy, often leading to preparing the home for the baby.
7. Gastrointestinal Changes (n/v, indigestion)
8. Cervical Ripening
The cervix softens (ripens), begins to open (dilate), and becomes thinner (effaces) in preparation for labor.
9. Rupture of Membranes (Water Breaks)
The amniotic sac may rupture spontaneously, either initiating or occurring during labor.
Labor typically starts within 24 hours after the rupture.
If membranes remain ruptured for more than 24 hours, the risk of infection increases.
Nursing Alert: Immediately check Fetal Heart Rate (FHR) to monitor for signs of umbilical cord prolapse or fetal distress.
Utilize the premonitory and physiological signs of labor to differentiate between true and false labor.
Rupture of Membranes / ROM (Water Breaks)
When the amniotic sac (keeping the baby afloat) ruptures (can occur before or during labor)
Typically starts within 24 hours of labor
Infection risk increases if any longer
Initiates natural hormone secretion (oxytocin) to facilitate contractions
Some mothers want to avoid medications during this time for a more natural birth
Assess fetal heart rate (FHR) for fetal distress IMMEDIATELY
If too low, cord could be occluded
Assess cervix for umbilical cord prolapse
Medical Emergency: If cord felt, keep hand inside to create space for the cord
Record time, color, and odor of fluid.
Perform Nitrazine or Ferning tests to confirm.
What happens when ROM happens?
Hormones secrete to facilitate contractions
Oxytocin
Some mothers want to avoid medications during this time for a more natural birth
What immediate actions must be done when the water breaks (Post-ROM)?
Assess fetal heart rate (FHR) for fetal distress
AND 5 minutes later
If too low, cord could be affected
Record time, color, and odor of fluid.
Assess cervix for umbilical cord prolapse but limit vaginal examinations
Medical Emergency: If cord felt, keep hand inside to create space for the cord
Assess temperature Q1-2 HR / per policy
Perform Nitrazine (pH) or Ferning (microscope slide) tests to confirm.
Notify HCP if meconium present
Cervical Ripening
Cervix softens, preparing or beginning to open (dilate) and thin (efface) in preparation for labor
Lightening
Premonitory Sign
When the “baby drops”
The fetal head descends into the pelvis (usually about 14 days before labor in first-time pregnancies).
Symptoms: Easier breathing, but increased pressure on the bladder, causing frequent urination.
More noticeable in first pregnancies (primigravida)
Braxton Hicks
Premonitory Sign
“Irregular, practice contractions”
Become more stronger, regular, frequent
Decreases with hydration and walking
Braxton Hicks vs True Contractions (No Table)
Decreases with hydration and walking
Irregular frequency, duration, intensity
No bloody show
DOES NOT decrease with hydration or walking
Regular frequency, duration, intensity
Stronger when walking
LEADS TO CERVICAL DILATION/EFFACEMENT
Cervical mucus plug
Thick, gelatinous substance that fills and seals the cervical canal during pregnancy
Expelled as a Premonitory Sign aka “Bloody Show”
What sign may indicate the start of cervical dilation/effacement
Appearance of brownish or blood-tinged mucus
Indicates expulsion of the cervical mucus plug.
Premonitory Sign
Nesting Instinct
Premonitory Sign
aka Energy Burst
A sudden surge of energy, often leading to preparing the home for the baby.
Preterm
20-36-6/7 weeks gestation
Term
=>37 weeks gestation
Abortion
<20 weeks gestation
Fetal/Abrupt Decelerations
Short-term but clear decreases of the fetal heart rate (FHR) identified during fetal heart monitoring.
Hydramnios
Condition where there is an excessive amount of amniotic fluid surrounding the developing fetus in the uterus
>25 cm surrounds
Oligohydramnios
Condition where there is too little an amount of amniotic fluid surrounding the developing fetus in the uterus
<5 cm surrounds
FIVE P’s: Passenger (Fetus and Placental Navigation)
Key Factors:
Presentation: The part of the fetus entering the pelvic inlet first.
Examples: Back of the head (occiput), shoulder, breech (sacrum/feet), or face.
Lie: Relationship of the maternal spine to the fetal spine.
Transverse: Fetal spine is horizontal (requires a C-section).
Parallel/Longitudinal: Fetal spine aligns with maternal spine (cephalic or breech presentation).
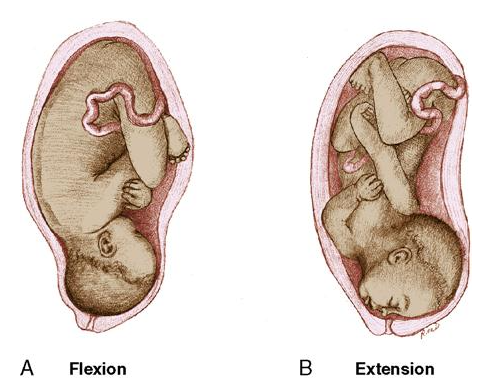
Attitude: Relationship of fetal body parts to each other.
Flexion: Chin tucked, extremities flexed toward body (ideal for delivery).
Extension: Chin extended away, less favorable.
Fetopelvic (Fetal) Position: The position of the presenting part in relation to the mother’s pelvis.
Three Letters:
First letter: Right (R) or Left (L) side of the maternal pelvis.
Second letter: Presenting part (Occiput [O], Sacrum [S], Mentum [M], or Scapula [Sc]).
Third letter: Position (Anterior [A], Posterior [P], or Transverse [T]).
Station: Measurement of fetal descent into the pelvis.
0 station: Fetal head is at the level of the ischial spines.
Negative station: Above the spines.
Positive station: Below the spines.
Molding Helps the Fetus Exit
Differentiate between fetal lie, fetal presentation, fetal positions, & fetal attitude.
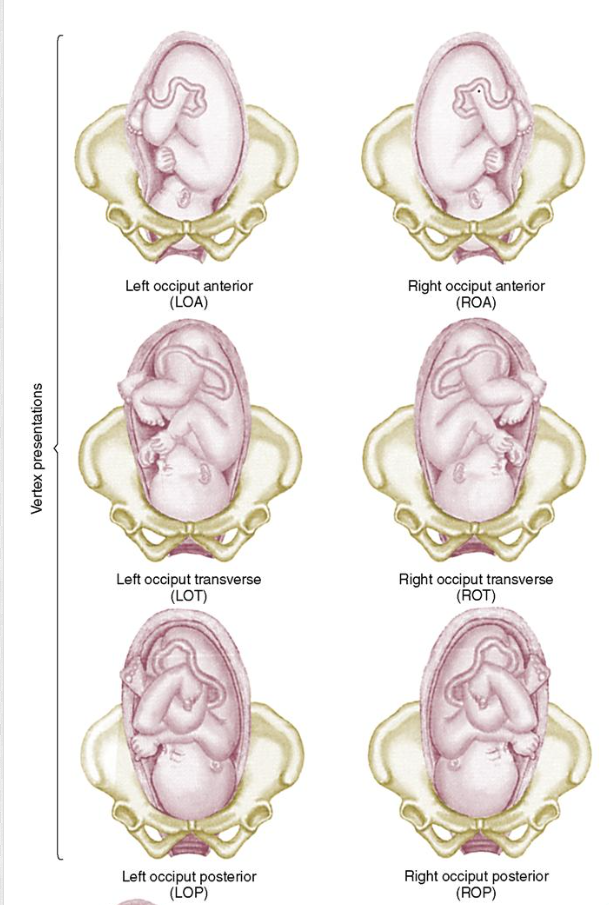
Passenger: Fetal Presentations/Positions
Vertex / Cephalic
LOA / ROA
Occiput facing left/right quadrant and anterior (symphysis pubis): ideal (can tuck chin)
LOT / ROT
Occiput facing left/right quadrant and anterior (symphysis pubis) / posterior (sacrum)
LOP / ROP
Occiput facing left/right quadrant and posterior (sacrum): not ideal (applies pressure to sacrum, cannot tuck chin)
97% of all term births
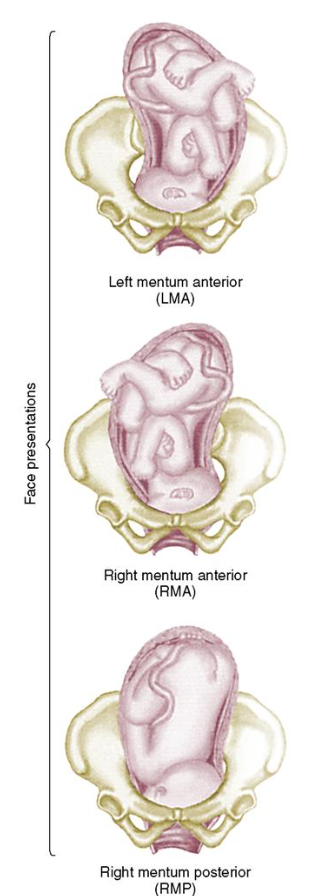
Face
LMA / RMA
Mentum facing left/right quadrant and anterior (symphysis pubis)
LMP/RMP
Mentum facing left/right quadrant and posterior (sacrum)
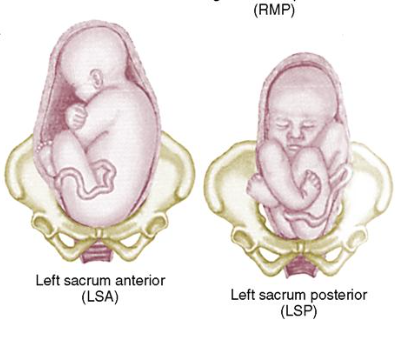
Breech
LSA/RSA
Sacrum facing left/right quadrant and anterior (symphysis pubis)
LSP/RSP
Sacrum facing left/right quadrant and posterior (sacrum)
Subdivided: Complete (butt first, legs crossed), Frank (butt first, body doubled), Footling (foot/feet first)
Transverse
Acromion first
Charted using the three-letter notation:
First Letter: Maternal side (R = Right, L = Left).
Second Letter: Presenting part (O = Occiput, S = Sacrum, A= Acromion, M = mental/face, B= Brow).
Third Letter: Orientation (A = Anterior, P = Posterior, T = Transverse).
"WHICH PART OF THE FETUS REACHES THE PELVIC INLET (HOLE) FIRST?”
Anterior Positions (ROA & LOA)
Facilitate smoother labor progression as the fetal head is aligned with the pelvic outlet.
Posterior Positions (ROP & LOP)
May require additional interventions, such as manual rotation or assisted delivery (e.g., forceps or vacuum).
Applies pressure to sacrum (posterior quadrant)
Baby cannot properly tuck chin
Passenger: Fetal Vertex Presentations (Image)
LOA / ROA
Occiput facing left/right quadrant and anterior (symphysis pubis): ideal
LOT / ROT
Occiput facing left/right quadrant and anterior (symphysis pubis) / posterior (sacrum)
LOP / ROP
Occiput facing left/right quadrant and posterior (sacrum): not ideal
Passenger: Fetal Face Presentations (Image)
LMA / RMA
Mentum facing left/right quadrant and anterior (symphysis pubis)
LMP/RMP
Mentum facing left/right quadrant and posterior (sacrum)
Passenger: Fetal Breech Presentations (Image)
LSA/RSA
Sacrum facing left/right quadrant and anterior (symphysis pubis)
LSP/RSP
Sacrum facing left/right quadrant and posterior (sacrum)
Passenger: Attitude (Image)
Relationship of fetal body parts to each other.
Flexion: Chin tucked, extremities flexed toward its trunk/body (ideal for delivery).
Extension: Chin extended away, less favorable.
“HOW TIGHT IS THE FETUS?”
Passenger: Lie
Relationship of the maternal longitudinal axis/spine to the fetal spine.
Transverse: Fetal spine is horizontal (requires a C-section).
Parallel/Longitudinal: Fetal spine aligns with maternal spine (cephalic or breech presentation).
“WHICH AXIS IS THE FETUS RELATIVE TO MOTHER’S SPINE?”
Passenger: Station
Relationship of presenting part vs maternal pelvic ischial spines
Measurement of fetal descent into the pelvis.
0 station: Fetal head is at the level of the ischial spines.
Negative station “-”: Above the spines.
-1 to -5 (at the inlet)
Positive station “+”: Below the spines.
+1 to +4 (at the outlet or crowning)
DO NOT AROM if NEGATIVE
Risks cord prolapse/tangling
“HOW DEEP IS THE FETUS?”
Five P’s (Factors That Affect/Define Labor & Delivery Process)
Passenger (Fetus + Placenta)
5 subtypes
Presentation, lie, attitude, fetopelvic positions, station
Passageway (Birth Canal)
4 Subtypes
Gynecoid: Favorable for vaginal delivery.
Android, Anthropoid, Platypelloid: Less favorable
Powers (Contractions)
2 Subtypes
Primary - involuntary
Secondary - Voluntary
Position (of mother)
Psychological response (Emotions of mother)
Mentum
face
Occiput
back of head
Cephalic lie
Upside down fetus (expected finding)
Breech lie
Right-side up fetus (unexpected finding)
Mecnoium
First poop
SROM
Spontaneous Rupture of Membranes
AROM (Artificial Rupture of Membranes)
Purpose
Helps stimulate labor
If no ROM after full dilation
If internal monitoring necessary
Procedure is called called amniotomy
DO NOT PERFORM UNLESS BABY IS ENGAGED (NOT A MINUS/NEGATIVE STATION)
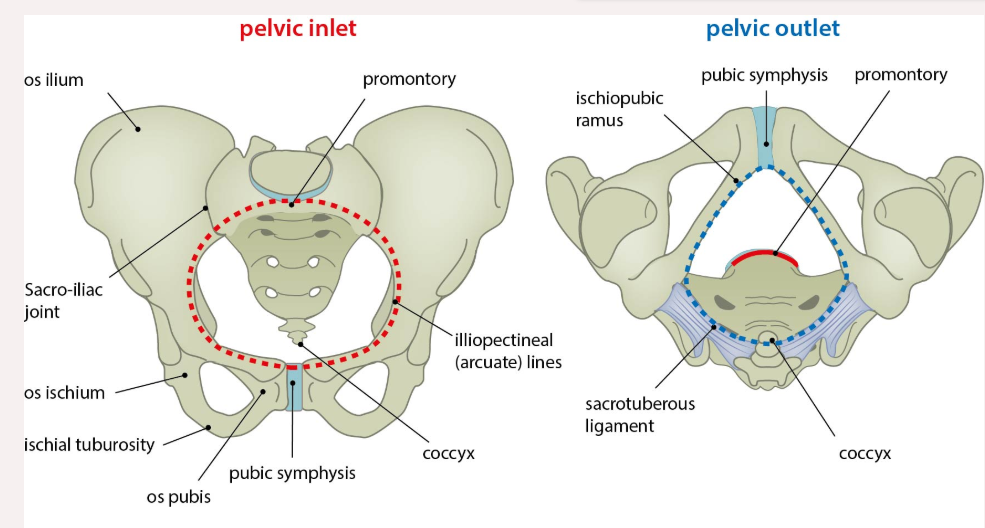
FIVE P’s: Passageway (Birth Canal)
Components: Bony pelvis, cervix, pelvic floor, vagina, and vaginal opening.
Key Points:
Size and shape of the bony pelvis are crucial.
Gynecoid: Favorable for vaginal delivery.
Android, Anthropoid, Platypelloid: Less favorable
Cervix must dilate (open 10cm) and efface (thin) for the fetus to descend.
The fetus must pass through this bony canal during the vaginal birth process. It is divided into 3 sections:
The inlet (top portion)
The pelvis cavity (hole)
The outlet (bottom portion)

FIVE P’s: Powers (Contractions)
Primary:
Uterine contractions cause:
Effacement (thinning of the cervix).
Dilation (widening of the cervix).
Secondary: Voluntary bearing down and pushing by the mother.

FIVE P’s: Position (Maternal)
Benefits:
Reduces fatigue and improves comfort.
Promotes fetal descent using gravity.
Positions include upright, kneeling, and squatting.
Encourage frequent position changes during labor
Upright uses gravity
Hands/knees relieves back pressure
Ball helps rotate baby
No supine – compression of vessels
FIVE P’s: Psychological Response (Maternal)
Impact: Maternal stress, tension, and anxiety can:
Slow labor progress.
Increase pain perception.
Affect uterine contractions negatively.
Provide emotional support to reduce fear and promote relaxation.
Orient To The Room, Call Her By Name, Encourage Verbalization, Listen Attentively, Answer All Questions- Re-answer Prn, Explain Procedures, Give Choices When Possible, Keep Informed Of Progress, Encourage Relaxation Techniques, Encourage Support Person To Participate, Provide Reassurance And Praise, Remain Calm And In Control During Emergencies, Explain That No Two Labors Are Alike, Don’t Make Promises, If Lips Are Tingling Or Lightheaded (Hyperventilating) Give Paper Bag Or Have Patient Breath Into Cupped Hands
Fetal Heart Rate w/ Uterine Pattern (Image)
Preprocedure Nursing Actions
Leopold Maneuvers:
Abdominal palpation to determine:
Fetal presenting part (e.g., head, breech).
Lie (longitudinal or transverse).
Attitude (flexion or extension).
Descent in the pelvis.
Helps locate the best area to listen to fetal heart tones (FHT).
External Electronic Monitoring (Tocotransducer):
A device placed on the maternal abdomen to measure:
Uterine contraction patterns.
Key Points:
Easy to apply.
Must be repositioned if the mother moves.
External Fetal Monitoring (EFM):
A transducer placed on the abdomen to monitor fetal heart rate (FHR) during labor and birth.
Tracks patterns to assess fetal well-being.
Updates about the labor and delivery process.
Opportunity for the client to ask questions or clarify procedures.
Provides reassurance and preparation for the next steps.
Preprocedure Labs
Group B Streptococcus (GBS):
A culture taken if not already done at 36-37 weeks of gestation.
Positive Result: Requires IV prophylactic antibiotics to prevent transmission to the baby.
Urinalysis (Clean-catch sample):
Assesses for:
Dehydration: Measured via specific gravity.
Ketones: Signs of poor nutrition or uncontrolled glucose.
Proteinuria: Indicates gestational hypertension or preeclampsia.
Glucosuria: Suggests gestational diabetes.
Urinary Tract Infection (UTI): Identified via bacterial count.
Includes universal drug screening for maternal safety.
Blood Tests:
CBC: Checks for anemia, infection, and clotting abnormalities.
ABO Typing and Rh Factor: Ensures compatibility to prevent hemolytic disease in the newborn.
No Prenatal Care: All necessary bloodwork is drawn if prenatal testing was missed.
Updates about the labor and delivery process.
Opportunity for the client to ask questions or clarify procedures.
Provides reassurance and preparation for the next steps.
Leopold Maneuvers
Abdominal palpation to determine:
Fetal presenting part (e.g., head, breech).
Lie (longitudinal or transverse).
Attitude (flexion or extension).
Descent in the pelvis.
Helps locate the best area to listen to fetal heart tones (FHT).
Do before labor
External Electronic Monitoring (Tocotransducer) / TOCO
A device placed on the maternal abdomen to measure:
Uterine contraction patterns
Easy to apply.
Must be repositioned if the mother moves.
Do before labor
External Fetal Monitoring (EFM)
A transducer placed on the abdomen to monitor fetal heart rate (FHR) during labor and birth.
Tracks patterns to assess fetal well-being.
Do before labor.
Pelvic inlet
The “hole” above the pelvic cavity
Marks the boundary between the greater pelvis and lesser pelvis.
Its size is defined by its edge, the pelvic brim.
Determines the size and shape of birth canal
Borders
Posterior – sacral promontory (the superior portion of the sacrum) and sacral wings (ala).
Lateral – arcuate line on the inner surface of the ilium, and the pectineal line on the superior pubic ramus.
Anterior – pubic symphysis.
Intraprocedure Nursing Actions
1. Assess Maternal Vital Signs
Check temperature every 2 hours if membranes are ruptured
2. Assess Fetal Heart Rate (FHR)
Tools:
External Fetal Monitor (EFM): Applied to the abdomen.
Spiral Electrode: Applied to the fetal scalp (requires ruptured membranes and cervical dilation).
3. Assess Uterine Contraction Characteristics
Method: Palpation of the uterine fundus or use of external/internal monitors.
Key Terms:
Frequency: Time from the start of one contraction to the start of the next.
Duration: Time from the beginning to the end of one contraction.
Intensity: Strength of contraction at its peak:
Mild (feels like pressing the tip of the nose).
Moderate (feels like pressing the chin).
Strong (feels like pressing the forehead).
Resting Tone: Uterine muscle tone between contractions (important for fetal oxygenation).
Prolonged contraction duration or frequent contractions (>5 in 10 minutes) can lead to fetal hypoxia and abnormal FHR patterns.
4. Intrauterine Pressure Catheter (IUPC)
A sterile catheter is inserted to measure the pressure of uterine contractions.
Requirements: Ruptured membranes and sufficient cervical dilation.
Use: Provides more precise contraction data.
5. Vaginal Examination
Performed digitally by a qualified nurse or provider to assess:
Cervical Dilation and Effacement:
Dilation: Opening of the cervix (measured in cm).
Effacement: Thinning and shortening of the cervix (measured in percentage).
Fetal Descent: Station (distance of fetal presenting part in relation to ischial spines).
Fetal Position and Presentation: Part of the fetus leading through the pelvis.
Membrane Status: Intact or ruptured.
How many contractions within a short time risks fetal hypoxia and abnormal FHR patterns?
MORE THAN 5 in 10 MINUTES
“>5 UC Q10min” (Tachysystole)
Measures Fetal Heart Rate
External Fetal Monitor (EFM): Applied to the abdomen.
Spiral Electrode: Applied to the fetal scalp (requires ruptured membranes and cervical dilation).
Intrauterine pressure catheter (IUPC)
A sterile catheter inserted to measure the pressure of uterine contractions.
Requirements: Ruptured membranes and sufficient cervical dilation.
Use: Provides more precise contraction data.
Measures Uterine Contractions
Tocotransducer (external)
Intrauterine pressure catheter (more precise)
Spiral Electrode
Another way to check fetal heart rate
Applied to the fetal scalp (requires ruptured membranes and cervical dilation) during labor
Intraprocedure Examination (Vaginal)
Performed digitally by a qualified nurse or provider to assess:
Cervical Dilation and Effacement:
Dilation: Opening of the cervix (measured in cm).
Effacement: Thinning and shortening of the cervix (measured in percentage).
Fetal Descent: Station (distance of fetal presenting part in relation to ischial spines).
Fetal Position and Presentation: Part of the fetus leading through the pelvis.
Membrane Status: Intact or ruptured.
Uterine Contraction Characteristics
Frequency: Time from the start of one contraction to the start of the next.
Duration: Time from the beginning to the end of one contraction.
Intensity: Strength of contraction at its peak:
Mild (feels like pressing the tip of the nose).
Moderate (feels like pressing the chin).
Strong (feels like pressing the forehead).
Resting Tone: Uterine muscle tone between contractions (important for fetal oxygenation).
Prolonged contraction duration or frequent contractions (>5 in 10 minutes) can lead to fetal hypoxia and abnormal FHR patterns.
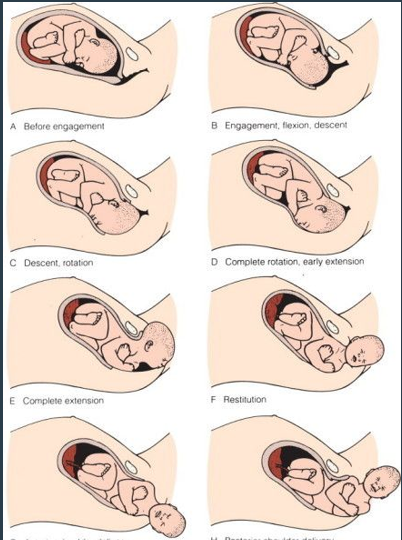
CARDINAL MOVEMENTS: Mechanisms of Labor (Vertex Presentation)
Engagement:
Fetal head passes through the pelvic inlet at station 0 (ischial spines level)
Descent:
Movement of the fetus down the birth canal (measured as negative or positive station).
Flexion:
Fetal head flexes (chin to chest) to fit through the pelvis.
Internal Rotation:
Fetal occiput rotates to a lateral position as it moves through the pelvis.
Extension:
Fetal head emerges under the pubic symphysis and extends to deliver.
External Rotation (Restitution):
After the head is born, it rotates back to align with the shoulders.
Birth by Expulsion:
After rotation, the baby is delivered completely as the shoulders and trunk pass through the birth canal.
EVERY DAY FAT INFANTS EAT EXTRA BREASTMILK
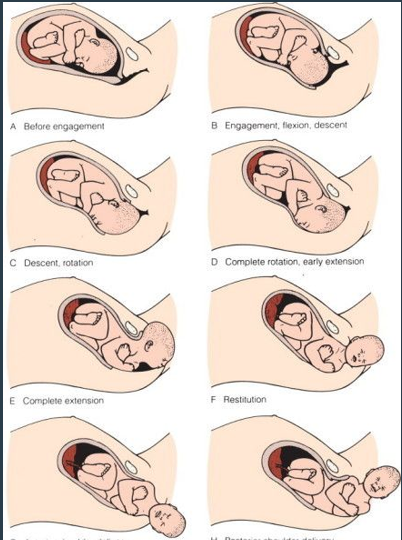
EVERY DAY FAT INFANTS EAT EXTRA BREASTMILK (CARDINAL MOVEMENTS)
Mechanisms of Labor (Vertex Presentation)
Engage (head reaches station 0)
Descent
Flexion (chin tuck to fit)
Internal Rotation (occiput rotates toward lateral)
Extension (chin untuck past pubic symphysis)
External Rotation aka Restitution (head pops out, then re-aligns w/ trunk)
Birth by Expulsion (shoulders and trunk pass)
Restitution
To restore or return to
References 6th of 7 Mechanisms of Labor (External Rotation to realign w/ shoulders
Postprocedure Nursing Actions & Education
Maternal Vital Signs
BP/Pulse: Q15 × 8 (first 2 hours)
Temp: Q4H x 2 (first 8 hours), then Q8H
Fundus:
Assess firmness and position to prevent uterine atony (soft uterus).
Q15 × 4 (first hour), then follow protocol
Massage PRN to maintain firmness
Administer oxytocics (e.g., ptocin) as prescribed to prevent hemorrhage
Lochia:
Monitor type, color, and amount of vaginal discharge.
Q15 × 4 (first hour), then follow protocol
Perineum:
Check for swelling, lacerations, or signs of infection.
Provide comfort measures (e.g., ice packs, analgesia)
Urinary Output:
Ensure the bladder is not distended, as this can interfere with uterine contractions.
Encourage voiding
Maternal/Newborn Bonding:
Encourage activities such as skin-to-skin contact and breastfeeding.
Educate to notify if:
Increased vaginal bleeding.
Passage of large blood clots.
Signs of infection (fever, unusual discharge, or foul odor).
True vs. False (e.g., Braxton Hicks) Contractions (Table)
Leads to cervical dilation and effacement, with stronger, regular contractions that persist.
“Bloody show” (vaginal bleeding) evident
Stronger when walking
No cervical changes, and contractions are irregular, painless, and stop with comfort measures.
Contractions felt in low back
Decreases with hydration and walking
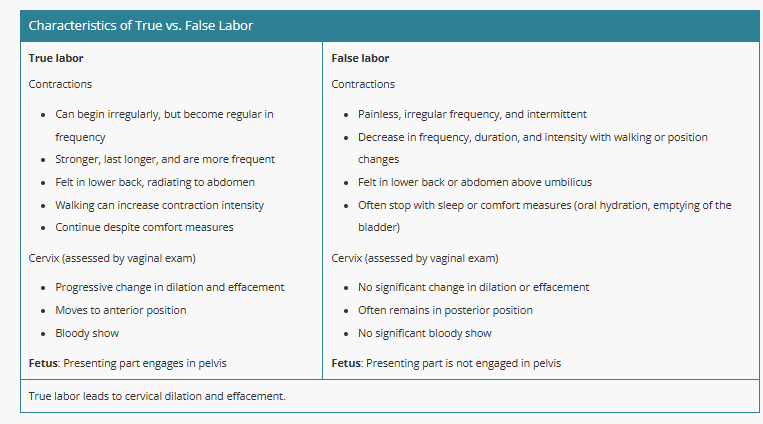
True Labor
Contractions:
Begin irregularly but become regular in frequency.
Stronger, last longer, and occur more frequently over time.
Felt in the lower back and radiate to the abdomen.
Walking increases contraction intensity.
Do not stop with comfort measures (e.g., rest, hydration).
Cervix (Assessed by Vaginal Exam):
Progressive changes in dilation (opening) and effacement (thinning).
Moves to an anterior position (closer to the front).
Presence of a bloody show.
Fetus:
Presenting part engages in the pelvis (descends into position for delivery).
False Labor
Contractions:
Painless, irregular, and intermittent.
Decrease in frequency, duration, and intensity with walking or position changes.
Felt in the lower back or abdomen above the umbilicus.
Often stop with sleep or comfort measures (e.g., hydration, emptying the bladder).
Cervix (Assessed by Vaginal Exam):
No significant change in dilation or effacement.
Cervix often remains in a posterior position (closer to the back).
No significant bloody show.
Fetus:
Presenting part is not engaged in the pelvis.
NSVD
Normal spontaneous vaginal delivery
VBAC
Vaginal birth of a C/S (c-section)
BOW
Bag of water
EFM
Electronic fetal monitoring
FHT/FHR
Fetal heart tone or fetal heart rate
PRIMIP
Woman delivering a baby for the first time
Nagel’s Rule
LMP Date: -3 Months +7 days (Knuckles: Months w/ 31 days)
6/11 = 3/18
4/18 = 1/25
3/11: 12/18
5/25: 3/4
6/30: 4/7
EDD/EDC
Estimated date of confinement or delivery
LMP
Last Menstrual Period
PPROM
Preterm Premature Rupture of Membrane
Before UCs start (high risk of infection, cord compression, cord prolapse)
Before 37 weeks gestation
PROM
Premature Rupture of Membrane
Before UCs start (high risk of infection, cord compression, cord prolapse)
Multip
Woman delivered a baby before
GRAN Multip
Woman delivered 5+ babies before
What is the definitive sign of true labor (not false labor)?
Cervix thins and dilates
GTPAL (Pregnancy Assessment)
Gravidity (number of pregnancies)
Present pregnancy
Miscarriages/abortion
Twin/triplets count as one
Term births (delivered >37 weeks)
Alive or stillborn
Twins/triplets count as one
Pre-term births (delivered 20-36-6/7 weeks)
Alive or stillborn
Twins/triplets count as one
Abortions/Miscarriages (delivered <20 weeks)
Counts toward gravidity
Twins/triplets count as one
Living children
Twin/triplets count individually
Always count the current pregnancy
NULLGRAVIDA
Never been pregnant
How do you help rotate an OP baby?
Maternal positions
Have the mother perform upright positions/exercises
Opens her pelvis
Aids effacement
Helps perception of pain
NEVER SUPINE (compresses the vessels)
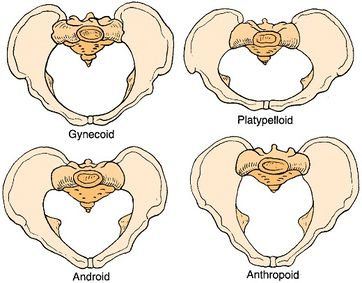
Which passageways are ideal and not ideal for vagina delivery?
Gynecoid: Favorable for vaginal delivery.
Android, Anthropoid, Platypelloid: Less favorable
Nursing Responsibilities (Assessment)
Assess Labor Status (Pre-Admission):
Take admission history
Review the birth plan.
Obtain laboratory reports for any abnormalities.
Monitor baseline FHTs and UC patterns for 20–30 minutes.
Check maternal vital signs for distress or complications.
Assess amniotic membranes state (e.g., ruptured or intact).
Orientation:
Orient the client and their partner to the unit upon admission.
Continuous Maternal and Fetal Monitoring (Admission):
Perform continuous assessments of both the mother and fetus throughout labor and immediately after birth.
Avoid vaginal examinations if:
There is vaginal bleeding.
Placenta previa or abruptio placentae is suspected (these conditions should only be handled by the provider).
Key Indicators of Labor Progress
Cervical Dilation:
Most reliable indicator of labor progress (measured in cm).
Factors Affecting Labor Progress:
Size of the fetal head.
Fetal presentation (e.g., head-first or breech).
Fetal lie (alignment of the fetus with the maternal spine).
Fetal attitude (flexion or extension).
Fetal position in the pelvis.
Contraction Characteristics:
Frequency, duration, and strength of contractions are critical for:
Fetal descent (lightening)
Cervical dilation.
Explain the needed information during the admission process to labor and delivery.
Key Indicators of Labor Progress
Cervical Dilation:
Most reliable indicator of labor progress (measured in cm).
Factors Affecting Labor Progress:
Size of the fetal head.
Fetal presentation (e.g., head-first or breech).
Fetal lie (alignment of the fetus with the maternal spine).
Fetal attitude (flexion or extension).
Fetal position in the pelvis.
Contraction Characteristics:
Frequency, duration, and strength of contractions are critical for:
Fetal descent (lightening)
Cervical dilation.