Pathophys Module 9
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
90 Terms
Gastroesophageal Reflux Disease (GERD)
Pathophys: the esophageal sphincter is weak and does not close completely after food enters the stomach, which allows the backflow of gastric juices from the stomach to enter the esophagus. Caused by a lifetime of “bearing down” during bowel movements, or holding your breath when weight lifting.
Key S/S of GERD
Heartburn within 30-60 minutes of meals. This causes inflammation of the esophageal mucosa and tissue erosion (causing Esophagitis).
Pain is worse when lying down or bending over (patients will complain of sleeping in a recliner or with the head of the bed elevated).
NOTE: Pain can mimic a heart attack because the stomach is so close to the heart.
May develop respiratory s/s due to gastric reflux entering larynx.
GERD risk factors
Obesity
Pregnancy
Smoking
Hiatial Hernia
Fatty Foods
Alcohol
Chocolate
Rx for GERD
Take acid-suppressing meds (Proton-pump inhibitor like omeprazole).
Stop smoking (even avoiding 2nd hand smoke).
Stop caffeine
Check for gluten intolerances
Maintain and high-protein, low fat diet.
Sleep with head of bed elevated.
Stay upright for 2-3 hrs after eating.
Nissen wrap/fundoplication (wraps the top part of the stomach aroung the esophagus to make a tighter sphincter.
What is a “cardiac cocktail?”
A combination of medications containing an acid suppressing liquid (mylanta) and usually a numbing medication like viscous lidocaine.
This is given to patients presenting with chest pain to rule out a myocardial infarction.
If the pain goes away after giving this cocktail, then the pain can be diagnosed as G.I. and not cardiac.
What can heartburn lead to?
CANCER
What is Barrett’s Esophagitis?
GERD causes tissue of the throat to develop precancerous dysplasia (Barrett’s Esophagitis) and could develop into esophageal cancer.
Hiatal Hernia
Pathophys: protrusion of the upper part of the stomach through the diaphragm into the thorax causing congestion of the blood flow and ischemia.
This pressure weakens the opening that the esophagus enters through the diaphragm at the “hiatus,” hence the name.
Key S/S of HH
Rarely causes s/s unless GERD is present.
HH pain can mimic a M.I. so chest pain has to be carefully evaluated to rule out cardiac causes for any chest pain first before treating as a G.I. problem.
HH Risk Factors
Exact cause unknown, may be a weaking of the supporting tissue which allows the diaphragm ring to widen and allow stomach to rise up through it.
Age
Pregnancy
Obesity
Habitual vomiting (like eating disorder)
weight training
smoking
alcohol
Rx for HH
Acid suppressing medication
Surgery if severe enough
HH can be observed through endoscopic exam
Peptic Ulcer Disease (PUD)
Pathophys: Erosion of the stomach lining. The bacteria Helicobacter Pylori (H. Pylori) are present in more than 90% of duodenal ulcers and about 80% of stomach ulcers.
Describe stress ulcer
Common in hospitalized patients (proactively given acid-supressing med by IV to prevent)
due to burn trauma
head injuries
critically ill patients
Multifactorial cause but shock is a known cause (loss of perfusion to stomach)
Treated with PPI (pantoprazole [protonix]).
PUD Risk Factors
Smoking (2nd hand included)
Alcohol use
NSAID use (aspirin, ibuprofen, naproxen, etc)
S/S of PUD
Epigastric (substernal pain) that starts about 2 hours after eating or in the middle of night when stomach is empty.
Pain is often relieved by eating.
Ulcers may self resolve or worsen and cause internal bleeding (UGIB - upper gastrointestinal bleeding) or stomach and/or duodenal perforation.
** A common finding in patients who have unexplained low hematocrit/hemoglobin.
List some dangers of PUD
Anemia
Profuse bleeding
Stomach cancer
Test for PUD and UGIB
CBC
Hematocrit & Hemoglobin
H Pylori test
Occult blood smear
EGD (esophagogastroduodenoscopy) to visualize and possibly stop the GI bleed.
Biopsy of stomach tissue (to test for h pylori) - done during EGD procedure.
Rx for PUD/UGIB
Combination drug therapy = antibiotics to kill the h pylori along with acid suppressing medication.
ULCERS ARE CURABLE
Active UGIB can be cauterized during endoscopy.
Characteristics of Duodenal Ulcers
25-50 years old: any age, usually early adulthood.
Men are more likely to get them
Hyperacidity is increased
Caused by increased use of alcohol/tobacco
Often caused by h pylori
Pain relieved by eating, common nocturnal remissions and exacerbations.
Hemorrhage is common
Characteristics of Gastric Ulcers
55-70 years old
Men are more likely
Hyperacidity is normal/low
Caused by moderate use of alcohol/tobacco
Gastritis may be present (common)
Bacterial infection may be present.
Pain relieved by eating, uncommon nocturnal remissions and exacerbations.
hemorrhage is less common
Characteristics of Stress Ulcers
Any person with severe stress or trauma is likely
Can affect both genders
Stress factors are increased
Hyperacidity is increased
Increased used of alcohol, ASA, and NSAIDS
Gastritis is acute and common
Bacterial infection is not a factor
Pain is asymptomatic until hemorrhage or perforation
Hemorrhage is very common
UGIB and LGIB
Can be either slow/chronic or sudden and life threatening.
If an ulcer perforates through the stomach lining, acid enters peritoneal cavity where it will cause sudden agonizing pain and a rigid abdomen. Can progress to sepsis and shock due to loss of blood or systemic infection.
Slow ulcer bleed may cause anemia and fatigue without realizing.
Occult GI Bleeding
A positive fecal occult blood test will result when there is no evidence of visible blood in feces.
Overt GI Bleeding
May manifest as hematemesis, melena, or hematochezia.
Hematemesis
Bleeding is from UGT, usually from esophagus, stomach, or proximal duodenum.
Bright Red Emesis
IS A MEDICAL EMERGENCY and a very dangerous sign.
Usually bleeding from esophagus.
Coffee Ground Emesis
Due to partial digestion of blood in the stomach by acids.
Melena
Black “sticky” stools that look like tar (and smell awful). Is caused by the partial digestion of blood in the small/large intestines (where alkaline digestive enzymes break down the blood). Melena can originate from a bleeding site in the stomach or intestines.
Hematochezia
Bright red blood from the rectum from anal fissures, hemorrhoids, diverticulosis, or infection.
While your patient might think this is an emergency, it usually is not.
Irritable Bowel Syndrome (IBS)
Pathophys: Considered a “functional gastrointestinal disorder” because there are changes in how the GI tract works, but it does not cause damage to the GI tract (unlike Crohn’s and UC).
IBS is a group of symptoms that occur together, not a disease.
IBS has previously been called colitis, mucous colitis, spastic colon, nervous colon, and spastic bowel.
** Can be caused by both physical and mental factors.
What is a defining characteristic of IBS?
Pain that is relieved by defecation.
IBS S/S
Is diagnosed when a person has abdominal pain or discomfort at least three times a month for the last 3 months without other disease or injury to explain the pain. Changes in stool frequency or consistency and can be relieved by a bowel movement. Altered bowel function w/o GI damage. Varying complaints of flatulence, bloating, nausea, anorexia, constipation, or diarrhea.
** IBS accompanies anxiety or depression.
RX for IBS
Dietary management is focused on FODMAP foods that seem to cause hyperstimulation of the intestines.
General diet recommendations are to eat smaller, more frequent meals, reduce fat content, avoid dairy/alcohol/caffeine, avoid gas producing foods, stress management, medications such as laxatives/antidiarrheal or antidepressants,
Inflammatory Bowel Disease (IBD)
Crohn’s Disease
Ulcerative Colitis
IBD is an umbrella term that includes Crohn’s and Ulcerative Colitis since both diseases product bowel inflammation.
Crohn’s Disease
Is a painful autoimmune disorder with no medical cure. It results in inflammatory lesions anywhere in the GI tract (mouth to anus) but is often in the ascending colon and terminal ileum.
Describe Crohn’s
Lesions involve all layers of the bowel wall and can cause fistulas (tunnels) to other organs or parts of the body.
Patient is susceptible to fluid and electrolyte imbalances as well as malabsorption of vitamins/minerals.
Characterized by “skip lesions” and a “cobblestone” appearance of intestinal lining.
Complications of Crohn’s Disease
Chronic inflammatory condition of the bowel.
Malabsorption (folic acide → anemia, Calcium/vit D → bone weaknesses)
Fluid and electrolyte imbalance
Diarrhea and dehydration
Anal fissures
Bowel wall becomes congested and thick which leads to abscesses and fistulas.
Scar tissue interferes with chyme movement and perforation or obstruction can occur.
Acute complications:
intestinal obstruction or perforation
Perianal abscesses or fistulas
May require removal of the inflamed intestine requiring an “ostomy.”
Ulcerative Colitis
Also an autoimmune disease.
Describe Ulcerative Colitis
Lesions occur only in the colon → chronic dehydration (↓ water reabsorption) and malnutrition.
Ulcerative lesions only involve the mucosal layer.
May lead to cavity formation with small hemorrhages and abscesses.
Wall of bowel thickens and ulcerations are fibrotic in later stages.
Complications of Ulcerative Colitis
Complications of Ulcerative Colitis:
- Intestinal obstruction
- Dehydration, Fluid, and electrolyte imbalances
- Malabsorption, Iron deficiency anemia
- Chronic bloody diarrhea mixed with mucus
- Weight loss
- Abdominal cramping and pain
- Nausea vomiting and the urge to defecate
- Acute complications = hemorrhage, toxic megacolon* and possible colon perforation.
- HIGH RISK FOR COLORECTAL CANCER due to development of dysplasia. Requires frequent colonoscopy screening
What is toxic megacolon
Damage to the nerve plexus, resulting in colonic dysmotility, dilation, and eventual infarction and gangrene.
Characterized by a thin-walled, large, dilated colon that may eventually become perforated.
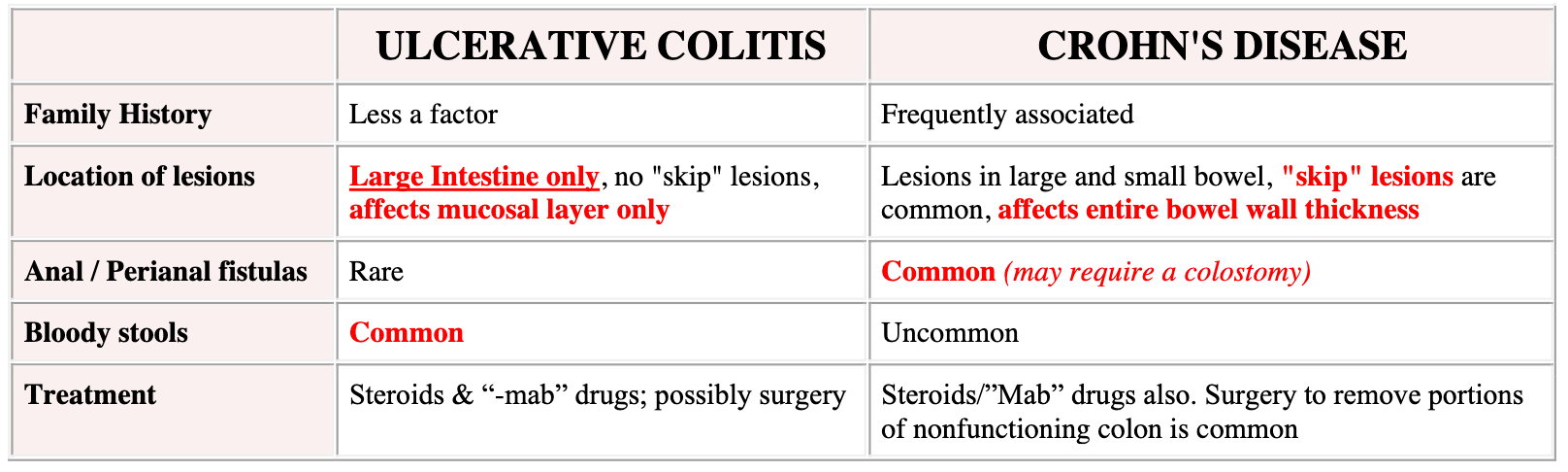
Crohn’s vs U.C.
They both have similar S/S such as abdominal pain, diarrhea, malabsorption of
nutrients, dehydration (colon not absorbing water). Both are diagnosed with Colonoscopy and tissue biopsies.
Colorectal cancer
Second leading cause of cancer-related deaths in the U.S. and third most common cancer in men and women.
Is increasing rapidly in the 40-50 year age range.
Risk factors for Colorectal Cancer
Age - 50+
Gender - greater in men than women
Race - black and caucasian
Family history - 25% of colon cancer
Medical Hx - of crohn’s and UC
Diet - unhealthy fats, refined sugars and flour, low fiber, and low vitamins
Other - obesity/lack of exercise; smoking; alcohol
Pathophys of Colorectal Cancer
Most colorectal cancers begin as a growth called a polyp on the inner lining of the colon or rectum.
Some polyps change into cancer over the years while others don’t.
Two types of Polyps
Adenomatous Polyp (adenomas) - these polyps sometimes change into cancer. Because of this, they are called a pre-cancerous condition. (A in cAncer).
Hyperplastic polyps and inflammatory polyps - more common, generally are not pre-cancerous.
S/S of colorectal cancer
In the early stages, there are none. Later stages of colon cancer might have the below:
➢ Changes in bowel movements, including constipation or diarrhea that don’t seem to go away
➢ Feeling like can’t empty bowels completely or urgently need to have a bowel movement
➢ Rectal bleeding or cramping
➢ Dark patches of blood in or on stool; or long, thin, "pencil stools"
➢ Abdominal discomfort or bloating
➢ Unexplained fatigue, loss of appetite, and weight loss
➢ Pelvic pain, which can happen in the later stages of the disease
DX testing for colorectal cancer
Fecal occult blood test because cancerous polyps bleed small enough amounts that it does not show in the stool but can be detected with stool smear.
Colonoscopy (to locate, biopsy, and remove polyps). Colonoscopies should begin at age 50 or sooner with family hx or high risk groups.
**note - the U.S. preventive services recommends taking low-dose aspirin to prevent colorectal ca.
Hepatic Pathologies
1. Prehepatic: < BEFORE> portal vein → thrombosis, cancer, enlarged
lymph nodes, compression.
2. Intrahepatic: <WITHIN> conditions that cause obstruction of blood
flow within the liver such as alcoholic cirrhosis.
3. Post hepatic: < AFTER> any obstruction to flow through the hepatic veins
beyond the liver lobules, either within or distal to the liver such as right sided
heart failure or thrombosis of hepatic veins
Liver functions
“People Drink So Much”
Produces ABCs
Albumin (plasma protein in charge of oncotic/osmotic pressure)
Bile (transports bilirubin (blood breakdown byproduct) and cholesterol
- buildup of bilirubin in the tissues → jaundice (yellow) in skin and sclera and buildup of cholesterol (hyperlipidemia)Detoxes - especially ETOH and drugs
Storage - glycogen (glucose package) stored in the liver for release as needed by the body
Metabolism - of protein. Protein digested in small intestine → ammonia byproduct → liver and metabolized into urea → sent to kidney for removal in urine.
Cirrhosis
Cirrhosis is scarred liver tissue and does not function normally.
Can also be caused by viral hepatitis or hepatotoxic drugs, I.e. acetaminophen (tylenol).
The most common cause of cirrhosis is..
chronic alcohol use (alcoholic hepatitis). ETOH is oxidized by the liver to acetaldehyde which damages hepatocytes.
Cirrhosis …
Scar tissue.
Prevents normal blood flow through the liver causing back-up that leads to portal hypertension.
Damaged liver tissue cannot synthesize protein so there is not enough protein in the blood to pull fluids out of the tissues leading to acites.
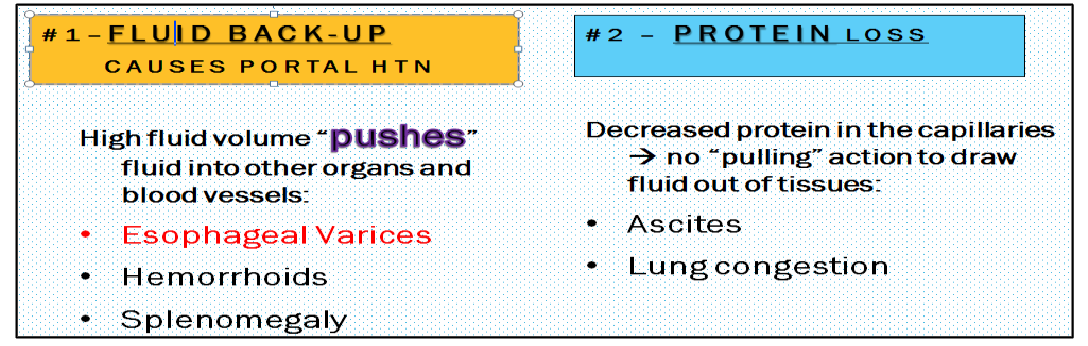
Portal Hypertension Pathophys
Obstructed flow in liver causes backup of fluid in Portal Veins
→ vein & organ engorgement. Most often due to cirrhosis. Increased vein pressure causes fluid to back up into vital organs causing those organs to stop functioning (i.e., splenomegaly). Portal HTN also causes the veins in the esophagus to engorge with blood, causing the veins to distend (esophageal varices) and possibly to burst – Bright red blood vomit (hematemesis) is a sign this has happened - Emergency action necessary. Pressure in the portal vein forces fluid out of the vein into the
abdomen which contributes to ascites.
Portal Hypertension Manifestation
Esophageal /
stomach varices,
splenomegaly,
ascites, hemorrhoids
Ascites pathophys
Free Fluid in the abdomen caused by two problems:
#1- Portal hypertension increases capillary hydrostatic pressure
(“PUSHES” fluid out of vessels into the gut) and,
#2 – damaged liver does not synthesize serum protein → decreased oncotic pressure (no protein in vessels to “PULL” the fluid out of the gut back intothe veins).
Ascites manifestation
Abdominal
distension, displaced
diaphragm leading to
dyspnea, peritonitis.
Treatment: Paracentesis
Hepatic Encephalopathy Pathophys
Damaged liver will not break down or synthesize protein which results in elevated ammonia levels. Ammonia is brain-toxic and high levels will cause changes in LOC. Increased ammonia and toxins unable to be processed by the liver are shunted from the GI tract into the circulation. Many toxins freely cross the blood-brain barrier causing neurologic S/S.
Hepatic Encephalopathy Manifestation
Confusion,
asterixis*(see below),
apraxia, stupor,
seizures, coma
Jaundice pathophys
Damaged liver cannot break down the bilirubin found in RBCs. The
bilirubin deposits in the skin and sclera of the eyes – turning the skin and
sclera “yellowish orange.” Causes intense pruritis (itching).
-Hemolysis of RBC's increases Bilirubin levels.
-Obstruction of bile flow from liver increases reabsorption
-Intrahepatic disease inhibits Bilirubin conjugation and
excretion
Jaundice Manifestations
Jaundice – aka,
“Icterus,”
S/S = Yellow orange
sclera/skin, dark urine
"coke syrup", light color
stools "clay colored",
anorexia, fatigue,
pruritus
Hepatorenal Syndrome Pathophys
1- Decreased circulating blood volume leads to decreased renal
perfusion triggering the renin-angiotensin system →vasoconstriction
and increased B/P
2- Hepatic failure prevents removal of excess Angiotensin so the process is not reversed and HTN gets worse.
3- Following the kidney damage, less urine is removed from the body, so waste products that contain nitrogen build up in the bloodstream (azotemia).
Prognosis is poor because renal failure is irreversible unless liver
transplantation is performed. Overall, the mortality of patients with liver failure is substantially worse if they develop hepatorenal syndrome. Without therapy, most patients die within weeks of the onset of the renal impairment
Hepatorenal Syndrome Manifestations
Na+ and H2O
retention
Oliguria
Increased BUN and
Creatinine levels
What is Asterixis?
Asterixis [“flapping tremor” of the hand] is an early sign of hepatic
encephalopathy. The hand will flap involuntarily when the wrist is extended; caused by metabolic encephalopathy of any cause, but especially decompensated liver failure; aka, “Liver Flap”: Counting the number of “flaps” per minute correlates with the degree of
severity of HEPATIC ENCEPHALOPATHY.
Paracentesis
Paracentesis is a procedure to aspirate fluid [ascites] that has collected in the abdomen (peritoneal fluid).
Paracentesis also may be done to take the fluid out to relieve intraabdominal pressure that is causing pain in people with cancer or cirrhosis, or to allow the person to breath better.
As much as a gallon of fluid (4 liters) can be taken out. This results in severe LOW BLOOD PRESSURE! This can lead to shock or KIDNEY damage (remember ATN?!?). This procedure is not
currative – the ascites will return if caused by cirrhosis of the liver.
Lab Tests
LFT (liver function tests)
CBC
Ammonia
Bilirubin
PT, PTT, INR
Occult Blood Smear
LFT
specifically the liver enzymes ALT and AST] increase when liver tissue has been damaged allowing the enzymes to escape into the blood.
CBC
is also done to check RBCs and platelet status.
Ammonia
levels are monitored due to the liver’s decreased ability to break down protein. High ammonia
levels cause encephalopathy (brain damage).
Bilirubin
if liver does not make bile, bilirubin [blood breakdown byproduct] is not cleared from the blood
PT, PTT, INR
will be drawn to test for bleeding problems.
Occult Blood Smear
(aka, Hemoccult or Guaiac) tests stool samples for occult blood
Viral Hepatitis
Chronic viral hepatitis slowly attacks the liver over many years without causing
symptoms. When s/s do appear, they are vague and nonspecific, so Hepatitis can go undetected until significant liver damage is present.
An estimated 4.4 million Americans are living with chronic (lifelong) hepatitis. Most do not know they are infected.
Viral Hep S/S
❑ Can be either Acute or Chronic
❑ Fatigue, weakness, loss of stamina
❑ Nausea, vomiting, diarrhea, anorexia
❑ Fever and flu-like symptoms
❑ Dark colored urine
❑ Jaundice of skin and sclera (aka, icterus)*
❑ Intense Pruritis due to icterus*
These are the only s/s that are specific to liver disease
*Hepatitis is difficult to recognize and diagnose because S/S are so
vague/nonspecific. Liver damage is often far advanced by the time the problem is diagnosed.
Viral Hep and Liver Cancer
The major cause of liver ca is is hep B & C. These heps develop silently as the liver becomes cirrhotic.
Diagnostic tests include blood tests, ultrasound exam, CT, and MRI scan. However, liver CA is lethal even when found early.
What are the viral hepatitides?
Hep A
Hep B
Hep C
Hep A
Oral-fecal (food borne) - most common type of Hepatitis in the US. Havrix vaccine* (must be given 3 weeks prior to exposure); IgG immunoglobulin is given after an exposure to unvaccinated patient.
Hep B
Blood/body fluid borne. Most common cause in US is through unprotected sex, but can also be spread by needle sticks, Mom-to-baby, etc. - Heptavax vaccine* (must complete series of 3); IgG immunoglobulin and Interferon (Intron-A) can be given to unvaccinated patient. If a chronically infected mother gives birth, 90% of the time her infant will be infected and develop chronic hepatitis B, usually for life. This may give rise to serious complications of liver disease later in life such as liver damage, liver failure, and liver cancer.
Hep C
Blood/body fluid borne. – No Vaccine available. Treated with antiviral med - Interferon (Intron A). With acute hepatitis C, the virus is eliminated in 25% of people. The other 75% become chronically infected and later may develop serious complications such as liver failure and liver cancer.
Vaccines vs IgG (Gammaglobulin)
*Vaccines are given before exposure to prevent hepatitis (A or B)
*IgG (Gammaglobulin) immunoglobulin shot is a short-term general antibody that can be given after exposure to hepatitis to strengthen the immune system and help the body fight the hepatitis virus – it is not a cure for hepatitis.
Pancreatic Disease (pancreatitis) pathophys
Injury or obstruction of pancreas causing digestive enzymes to leak into pancreatic tissue --> auto- digestion of tissue OR formation of cysts. PRIMARY CAUSE IS ALCOHOL ABUSE, followed by blockages caused by gallstones.
• Alcohol abuse – ETOH stimulates pancreatic enzymes and causes obstruction of pancreatic duct/sphincter.
• Gallstones – get into common bile duct and block pancreas excretion.
Pancreatic Disease (pancreatitis) S/S
PPPPAAAAIIIINNNN !!!! Especially epigastric pain, fever, leukocytosis, nausea and vomiting, abdominal distention, increased bowel sounds, hypotension, and shock (look up “WHY” in textbook). Can mimic a heart attack, so it is necessary to rule out cardiac causes for pain (just like for GERD and Ulcers, etc.) because the pancreas is so near to the heart.
Pancreatic Disease (pancreatitis) Stool
“Foamy floaters” – bulky unformed stools, unusually foul-smelling, greasy stools (steatorrhea). The stool is light-colored and may even contain oil droplets. This is caused because pancreas enzymes are not breaking down fat in the intestines
Pancreatic Disease (pancreatitis) Rx
GI rest (nothing by mouth or NG tube until condition is controlled because food causes the pancreas to try excreting digestive enzymes which increases the patient’s pain. Primary goal is pain control and treat underlying cause (possibly with antibiotics). If patient is without food for a week, may consider giving nutrients via an IV.
What should you never give a patient with epigastric/abdominal pain?
ANYTHING TO EAT OR DRINK!!! They may need surgery and if you give them water to drink you may be delaying an emergency surgery!
Cholecystitis (gallbladder) etiology
Associated with cholelithiasis (gallbladder stones composed of cholesterol and bile) and may be “superimposed” on chronic Cholecystitis (inflammation of the gallbladder). In the majority of cases, acute cholecystitis is caused by gallstones or biliary sludge getting trapped at the gallbladder's opening. Can also be caused by infection, injury, or tumor.
6 F’s (risk factors) of Cholecystitis
Fair
Fat
Fertile
Female
Forties
Family HX
Other cholecystitis risk factors
Crohn’s disease
Diabetes
Hyperlipidemia
Pregnancy
Long laber
RAPID weight loss
What is the hallmark symptom of Cholecystitis?
Pain IMMEDIATELY after eating (especially fatty foods).
(NOTE: this is different than ulcer pain that is relieved with eating food). Pain can mimic heart attack.
Light color or Clay-colored stools
Cholecystitis Rx
Dietary modification (a no-fat diet), or Surgery - a laparoscopy procedure called a cholecystectomy or “Lap Chole” for short, if the gallbladder is not swollen/infected, otherwise will need to have a traditional gallbladder surgery.