5.0 Allergic respiratory disease
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
30 Terms
Allergic Respiratory Disease
an altered state of health caused by the generation of IgE antibodies to airborne allergens leading to various clinical manifestations in the upper and/or lower airway
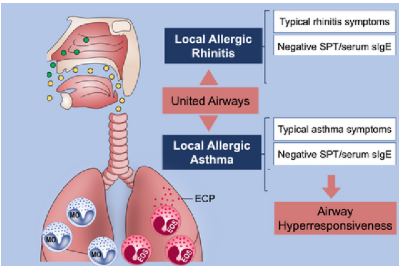
ARD is based on the theory that there is one airway, one disease as the conceptual basis of the management of patients diagnosed with rhino-conjunctivitis and/or asthma
where the definition of ARD as a single entity would facilitate the management of all the diseases it encompasses, especially when allergy is its main cause.
The concept of ARD is based on the allergic origin of the disease, and its clinical spectrum includes
conjunctivitis, rhinitis, and/or asthma.
Not all clinical manifestations must occur simultaneously in ARD patients,
although the risk of developing the other clinical manifestations of ARD in the future is greater if you present with one of the clinical manifestations than in the general population, e.g., allergic rhinitis is a risk factor for asthma.
Therefore Patients with persistent allergic rhinitis should be evaluated for asthma by history, chest examination and, if possible and when necessary, the assessment of airflow obstruction before and after bronchodilator,
while Patients with asthma should be appropriately evaluated (history and physical examination) for rhinitis.
For treatment a combined strategy should ideally be used to treat the upper and lower airway diseases in terms of efficacy and safety.
The immediate allergic reaction, referred to as Type-1 hypersensitivity,
is an evolved protective mechanism against invasion by parasites that when directed against otherwise harmless allergens, turns pathogenic
This is characterised by a shift in the dominant T-cell type from T helper type-1 (Th1) to T helper type-2 (Th2) cells, to generate what is termed as Type-2 inflammation.
The Th2 cells are directed against perceived threats, i.e. allergens, resulting in Th2 cytokine production and the priming of the allergic cascade, the phenotypic hallmark of which is production of elevated levels of allergen-specific IgE that can be detected by either serologic or skin-prick testing.
Responses to allergens are driven by both the environment and genetics.
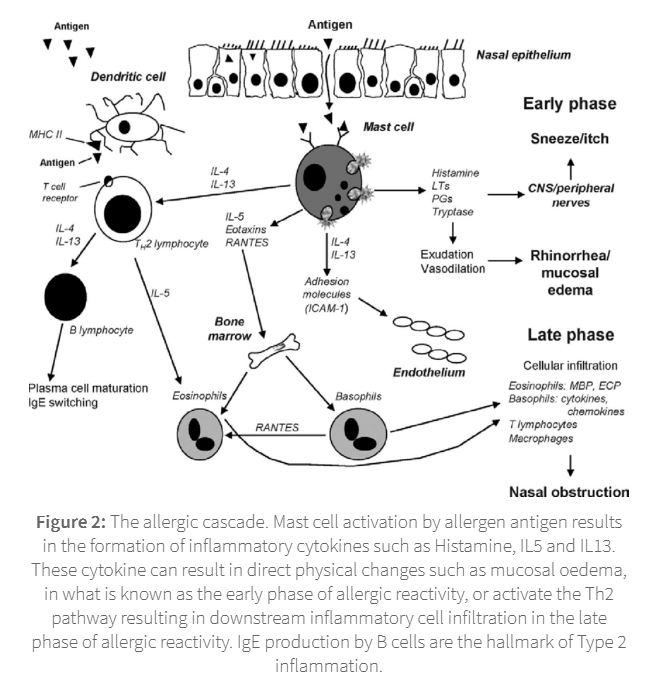
Some examples of allergens that may trigger the allergic cascade specifically within the respiratory system include:
Pollen
Pet dander
Dust
Mould and mildew
Latex
Allergic disease is identified through allergy testing, which can be either topical (skin) or peripheral (blood):
skin prick test
blood test

skin pric test
The most reliable of the tests, which involves scraping a small section of skin with an allergen, usually by subcutaneous injection, and monitoring whether the skin reacts within a 15 - 20 minute window. A positive reaction is identified by a red raised bump known as a wheal. The test indirectly measures IgE responses. Although the most reliable test of the possible two allergy tests, 50-60% of skin prick tests produce a false positive to at least one of the challenges.
blood test
Also defined as a radioallergosorbent (RAST) test, this measures allergy-specific antibodies in your blood. Although less accurate than the skin prick test, this assay is especially useful in individuals that do not tolerate a skin prick test, such as young children.
Allergic Rhinitis (Hay fever)
a major chronic respiratory disease due to its prevalence, impact on quality of life and economic burden. It can be intermittent (<4 days aweek or <4weeks)or persistent (>4 days a week and >4weeks) usually due to the the triggering indoor or outdoor allergen(s). It is clinically defined as a symptomatic disorder of the nose induced by an IgE-mediated inflammation after allergen exposure of the membranes lining the nose.
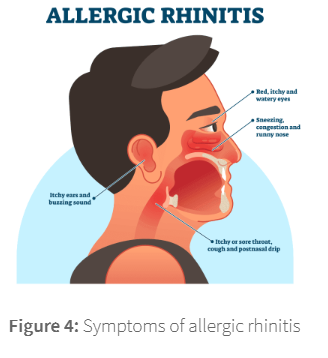
Symptoms include:
Rhinorrhoea
Itchy nose, mouth, throat, & eyes
Sneezing
Congestion
Red & watery eyes
Itchy ears and buzzing in the ears
The most common triggers of intermittent allergic rhinitis are plant and fungal spores, whose seasonal release drives the seasonality of the condition. Examples include:
Tree pollen (present in the early Spring)
Grass pollen (in the early Summer)
Ragweed (in the Autumn)
Mold (in the Autumn)
Persistent allergy triggers will generally be allergens released by continually present sources from usually indoor environments. Common triggers of persistent allergic rhinitis include:
pets
house dust mite
mould
cockroaches
pets
Allergens from mammalian pets (e.g. cats, dogs, rodents & rabbits) are found in skin cells the animals shed (dander), as well as in their saliva, urine and sweat and on their fur. In birds, feathers can produce allergens in addition to droppings and other secretions. Dander is a particular problem because it is very small and can remain airborne for long periods of time with the slightest bit of air circulation. It also collects easily in upholstered furniture and sticks to your clothes. Saliva can stick to carpets, bedding, furniture and clothing, while dried saliva can become airborne. The major cat and dog dander allergens are Fel d1 and Can f1 respectively.
house dust mite
driven by the two major allergens Der p1 and Der p2. The former is a cysteine protease, while the latter is a major IgE binding protein. Der p1 is common in Europe, while Der p2 is more common in the Americas.
mould
Not all mould types will cause allergic symptoms. Most allergic responses are driven by the following mould species - Alternaria, Aspergillus, Cladosporium & Penicillium
roaches
The saliva, feces and shedding body parts of cockroaches can trigger both asthma and allergies. These allergens act like dust mites, aggravating symptoms when they are kicked up in the air. Cockroach allergen proteins include Bla g1, Bla g2, Blag 4, and Bla g5.
Persistent allergy can also be triggered by chemical irritants that are not generally regarded as allergens. These include:
Smoke from fires
Cigarette and other second-hand smoke
Air fresheners
Perfume, hair spray, and other strongly-scented items
Smog and other environmental pollutants
Cleaning sprays
Pool chemicals, including chlorine
while allergic asthma is the most prominent form of asthma in children, an accurate diagnoses in children under the year of 5.
Allergic bronchopulmonary aspergillosis (ABPA) is an allergy or sensitivity to a fungus found in soil known as Aspergillus fumigatus. In this condition, there is both an allergic and an inflammatory response to the Aspergillus mould.
Symptoms may include severe wheezing, coughing and shortness of breath, much like asthma. People with asthma are at a higher risk of getting ABPA. The first sign of ABPA in people with asthma is a worsening of asthma symptoms. Other symptoms include:
Cough with brown flecks or bloody mucus
Fever
Weakness/malaise
watch video