3.3 Coughing in Horses 2
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
LRT: undifferentiated bacterial pneumonia causes & clinical signs
causes: strep zooepidemicus, also actinobacillus, klebsiella, staph aureus, bordetella, mycoplasma
clinical signs: auscultable changes, mild pyrexia, cough
undifferentiated bacterial pneumonia: diagnosis
history
clinical signs
mucopurulent exudate in trachea on endoscopy
bronchointerstitial pattern on radiography
BAL/tracheal aspirate neutrophils increased, degenerate, intracellular bacteria
undifferentiated bacterial pneumonia: treatment
-antibiotics (C&S, if not, ensure good against strep)
-rest
-dust free environment
URT & LRT: streptococcus equi equi (strangles)
gram positive
not normal inhabitant of URT
does not require viral infection for colonization
highly infectious, particularly weanlings & yearlings
equine specific
strangles: epidemiology
1-5 year olds
foals born from immune mares resistant for 3 months
morbidity 100%
mortality 10% without appropriate therapy
20% complication rate reported
immunity not lifelong (75% still immune after 3-4 years)
strangles: transmission
direct contact with nasal secretions or LN discharges, fomites, environment, only survives 1-3 days
asymptomatic chronic carriers-> guttural pouch, up to 56m
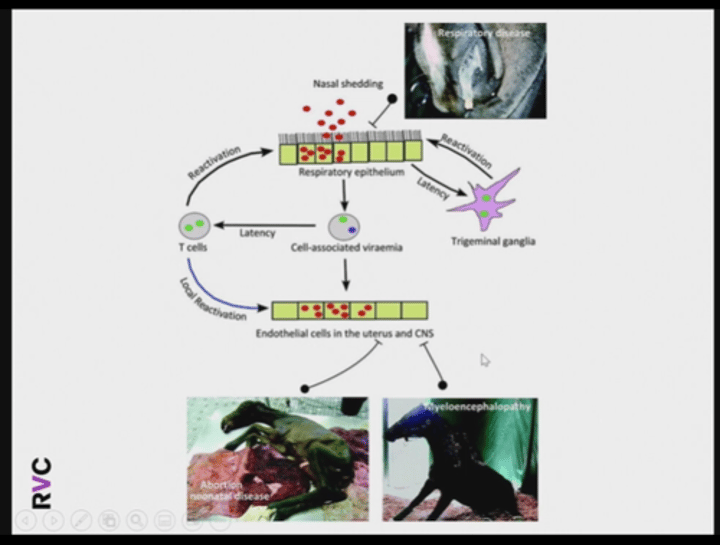
strangles: pathogenesis
incubation 3-14 days
recover over 2-3 weeks
nasal shedding continues for 2-3 weeks after disease
some horses for months or years (up to 10% become carriers)
3 clinical presentations: classic acute disease, atypical strangles, complications
classic acute disease: clinical signs
fever, depression, inappetence, lymphadenopathy
abscessation of mandibular, parotid, or retropharyngeal lymph nodes, rupture after 7-10 days
dyspnea & dysphagia if abscesses compress larynx or interferes with cranial nerve to pharynx
mucoid to purulent nasal discharge
cough
URT signs
atypical strangles: clinical signs
mild inflammation of URT
slight nasal discharge
cough
fever
self-limiting lymphadenopathy
probably dependent on bacterial strain & immunity & genotype of horses
importance of atypical strangles
looks like any other respiratory infection
samples not taken for culture
control & prevention not implemented
bacteria from atypical cases can cause classical strangle in others
strangles outbreaks with atypical cases usually go unrecognized until classical cases appear later
complications: internal abscessation
-intermittent colic
-pyrexia of unknown origin
-anorexia
-depression
-weight loss
-depends on site of abscess
complications: purpura hemorrhagica
-generalized vasculitis caused by type III HS reaction after 3-4 weeks
-1-2% of infected horses
-thrombosis of small arteries
-skin & muscle necrosis
-ventral & limb edema & petechial hemorrhages on mucous membranes
-death due to pneumonia, cardiac arrhythmia, renal failure, GI disorders

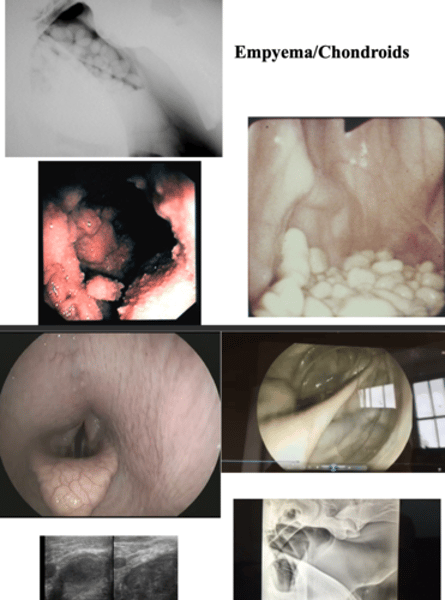
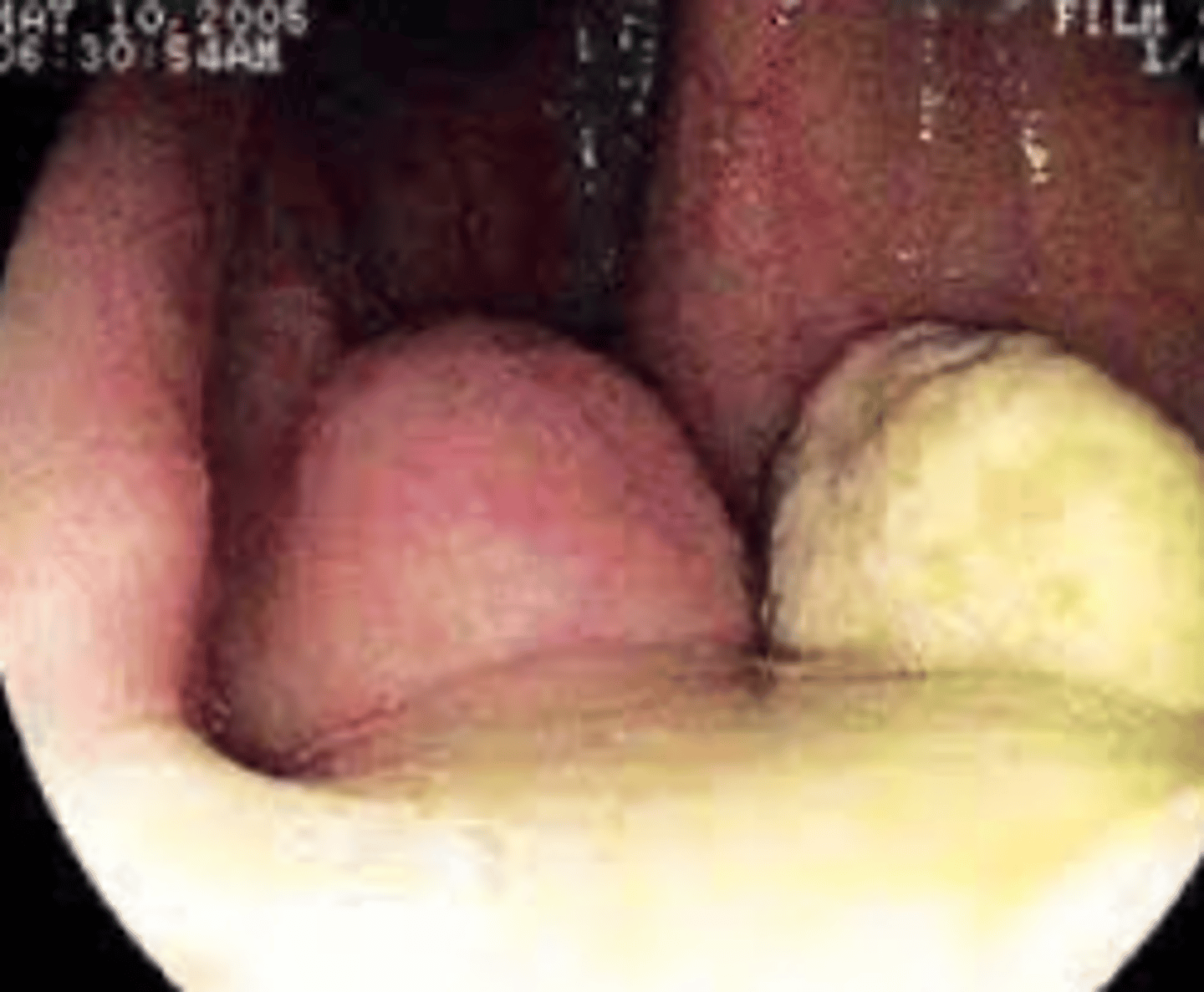
complications: guttural pouch empyema & chondroids
-purulent nasal discharge
-RP swelling
-dyspnea/dysphagia
strangles: diagnosis
clinical signs
leukocytosis, hyperfibrinogenemia/
high SAA
isolation (culture) or detection (PCR) of s. equi from LN pus, nasopharyngeal swab, GP lavage fluid
culture 3x of NP swab
guttural pouch lavage more sensitive than nasopharynx or nasal discharge swab
strangles: treatment (exposed, early signs, LN abscesses)
horses exposed to strangles: treat with penicillin, isolate from infected horses, will not become immune
horses with early clinical signs (rhinitis/pharyngitis phase): penicillin, may inhibit natural immunity so may contract disease again with continued exposure, general nursing, anti-pyretics, soft food
horses with LN abscesses: poulticing & draining of abscesses, antibiotics may prolong resolution of abscess, general nursing, anti-pyretics, soft foods
strangles: treatment (complications)
abdominal abscesses
diagnosis: US or rectal
treatment: long term antibiotics (penicillin +/- TMPS up to 6 weeks)
guttural pouch empyema +/- chondroids
diagnosis: endoscopy, radiography
treatment: drainage via pharyngeal openings or surgical drainage-> instill antibiotics
purpura hemorrhagica
diagnosis: skin biopsy
treatment: penicillin, dexamethasone or prednisolone, fluids, palliative measures (hydrotherapy, massage)
strangles: management of outbreaks
isolate premises, create 3 groups of horses
red: presumed infected, clinical signs, confirm resolution of disease once clinical signs have resolved (3x negative cultures or PCR of NP swabs, taken 7 days apart as shed intermittently or 1x negative GP washing)
amber: direct or indirect contact with red horse
green: no contact or clinical signs
amber & green: take temp daily, if pyrexic move to red group, screen using blood test for carriers (IgG vs 2 strep equi specific antigens- A & B, takes 2 weeks), if positive-> isolate & test via 1 CP lavage or 3 NP swabs, if positive, treat as carrier
strangles: carriers
identification & treatment
-endoscopic GP lavage
-retrieve chondroids via GP +/- surgery
-instill topical benzylpenicillin in gelatin
-repeat GP lavage & PCR after 2 weeks
strangles: prevention
modified live vaccine available in UK in 2005- withdrawn due to adverse reactions
new recombinant protein (strangvac)-> reduce clinical signs & number of URT LN abscesses
isolate new horses for 3-4 weeks + test for carrier status
rhodococcus equi
gram positive, pleomorphic coccobacillus
widespread in environment
survives in GIT of mares (no disease)
survives & multiples in GIT of foals (disease)
survives in GIT of earthworms (reservoir)
survives in soil for at least 12 months in hot dry conditions-> common in USA, Australia, & Ireland?
rhodococcus equi: epizootiology
spread via inhalation of soil/feces, also detected in exhaled air from infected foals
amplified with high risk management practices (concentrated facilities, dusty paddocks & stables, incomplete manure removal)
seasonal- late spring/summer-> high aerosol challenge & high number of susceptible foals
occurs sporadically & endemically
in endemic farms, morbidity 15-60%, mortality 1-12%
rhodococcus equi pneumonia
foals 1-6 months
inhalation of contaminated dust
scavenged by alveolar macrophages but not killed
destruction of macrophages-> pyogranulomatous response
bronchopneumonia with widespread abscess formation

rhodococcus equi pneumonia: clinical signs
anorexia, depression, fever, dyspnea, tachypnea, cough, varies from insidious to extremely acute onset, subacute form rare & may be found dead or with acute respiratory distress & pyrexia leading to death in 48 hours
rhodococcus equi: extrapulmonary signs
common: diarrhea, ulcerative enterotyphlocolitis, intra-abdominal abscesses, intra-abdominal lymphadenitis, immune-mediated synovitis
less common: bacteremia, cellulitis/lymphangitis, meningitis, IMHA, intracranial abscesses, osteomyelitis, peritonitis, pleuritis, septic arthritis/synovitis
often concurrent with pneumonia, can be found alone, can have >1 EP disorder concurrently, decreases prognosis
rhodococcus equi pneumonia: diagnosis
fibrinogen, neutrophilia, tracheal wash (culture, gram-stain cytology, PCR VapA gene), US, radiography (less sensitive than US), serology (not sensitive or specific enough), post mortem
rhodococcus equi pneumonia: treatment
total US abscess diameter <8cm & mild clinical signs=> 75% recover without treatment
do not treat if no clinical signs, WCC <20x10^9/L, abscess score <10cm
treat if mild signs & abscess score >10cm
treat if moderate to severe signs
rhodococcus equi treatment: antibiotic selection
clarithromycin OR azithromycin with rifampin
short & long term outcome better with clarithromycin
some clinicians no longer add rifampin, but still recommended to reduce resistance
treat until there is radiographic resolution of lesions & CBC & fibrinogen are normal->
4-12 weeks
treatment is expensive
4% resistance
rhodococcus equi: prevention via husbandry
difficult since pathogen shed in feces
increase ventilation & decrease dusty conditions
avoid dirt paddocks & crowding
rotate pastures to minimize grass destruction
vacuum or collect manure
isolate sick foals
rhodococcus equi: prevention via prophylaxis
hyperimmune plasma-> decreased farm incidence by 30-40% in some studies, no effect in others
will not prevent disease in every foal
optinal timing & dose not clear
surveillance mechanisms & environmental changes still necessary
prophylactic azithromycin not beneficial
no effective vaccine for mare or foal
rhodococcus equi: prevention via early diagnosis
daily observation by breeder
weekly vet exam: PE, US, WCC
WCC> 13x10^9/L= suspicious
>15x10^9/L= highly suspicious
parascaris equorum
not a major pathogen
eggs on ground from previous year's foal crop
can cause transient nasal discharge & cough as larvae migrate through lungs
diagnosis via FEC
treatment via anthelmintics
