Urinalysis and Body Fluids Problem Solving | Quizlet
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
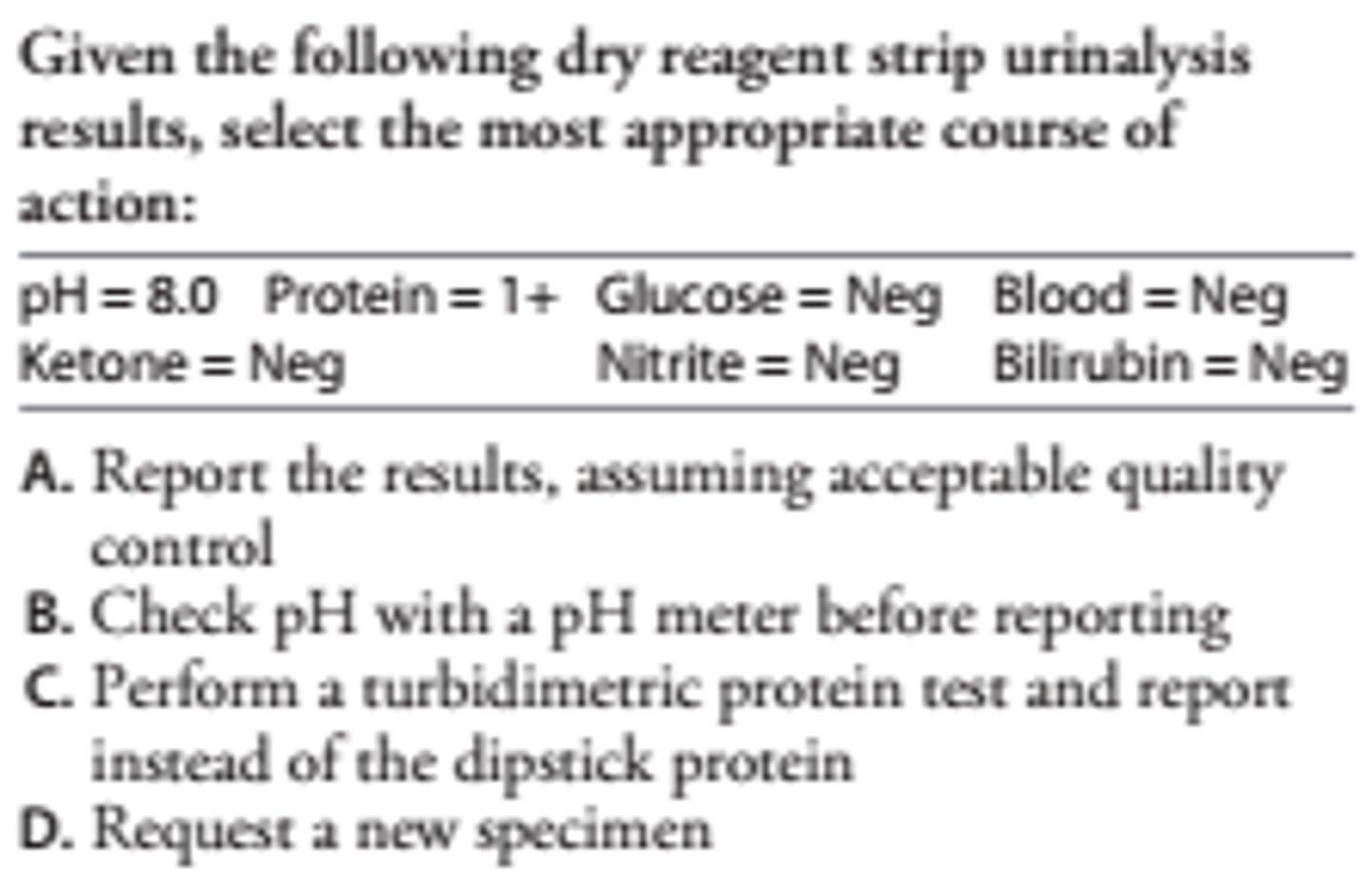
C
Highly buffered alkaline urine may cause a false-positive dry reagent strip protein test by titrating the acid buffer on the reagent pad. The turbidimetric test with SSA is not subject to positive interference by highly buffered alkaline urine.
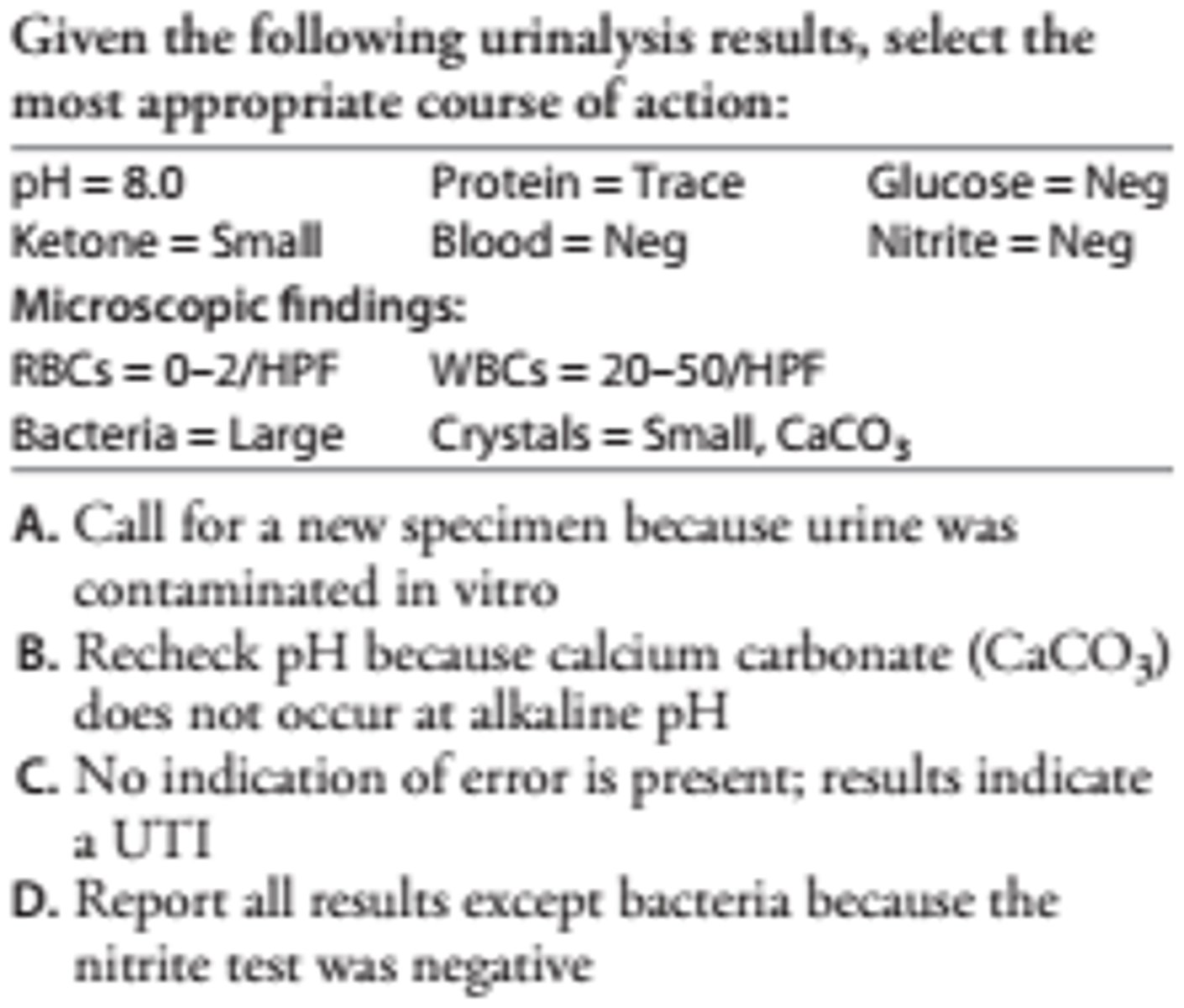
C
A positive nitrite requires infection with a nitrate-reducing organism, dietary nitrate, and incubation of urine in the bladder. The test is positive in about 70% of UTI cases. Alkaline pH, bacteriuria, and leukocytes point to UTI.
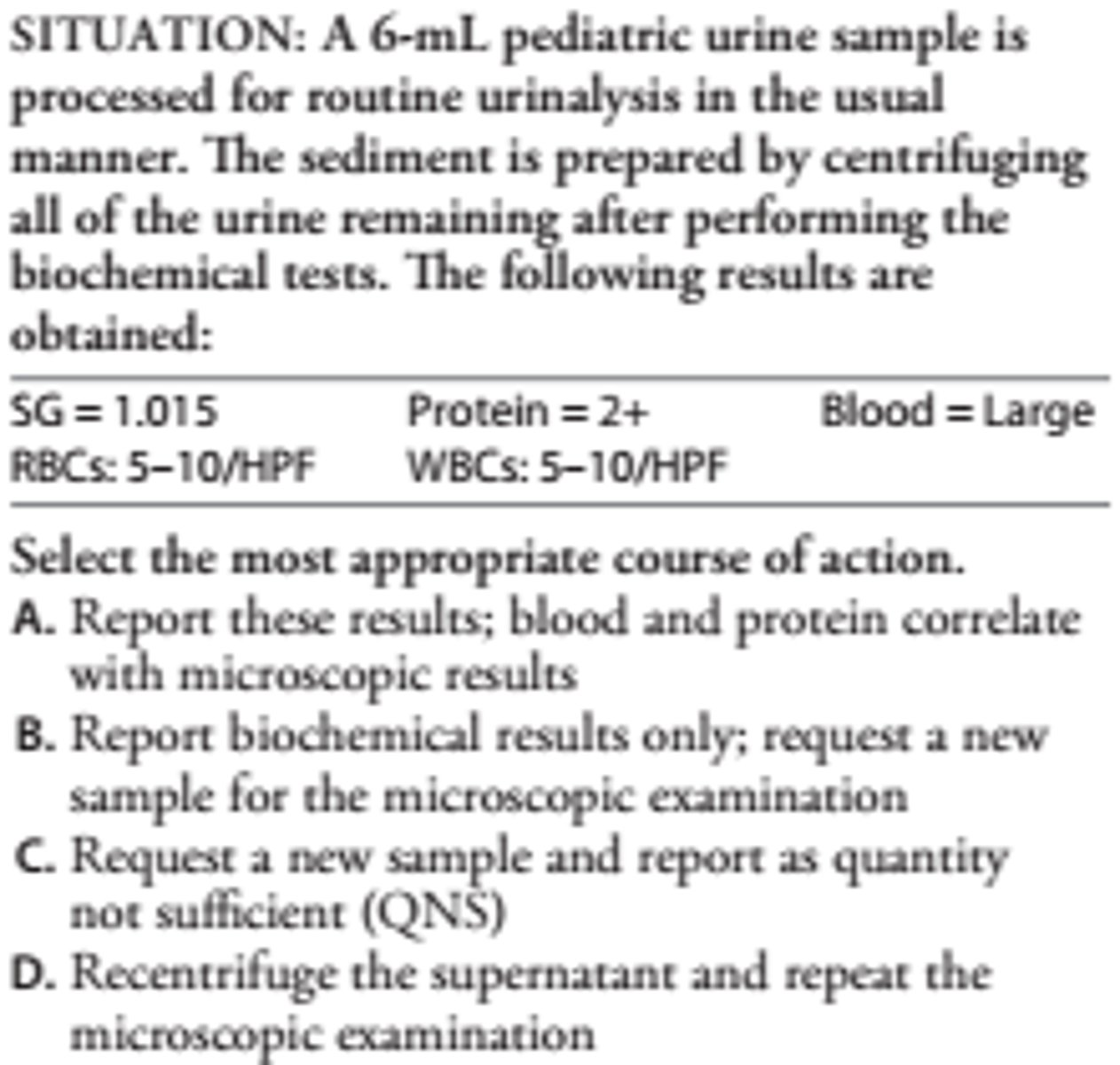
B This discrepancy between the blood reaction and RBC count resulted from spinning less than 12 mL of urine. When volume is below 12 mL, the sample should be diluted with saline to 12 mL before concentrating. Results are multiplied by the dilution (12 mL/mL urine) to give the correct range.
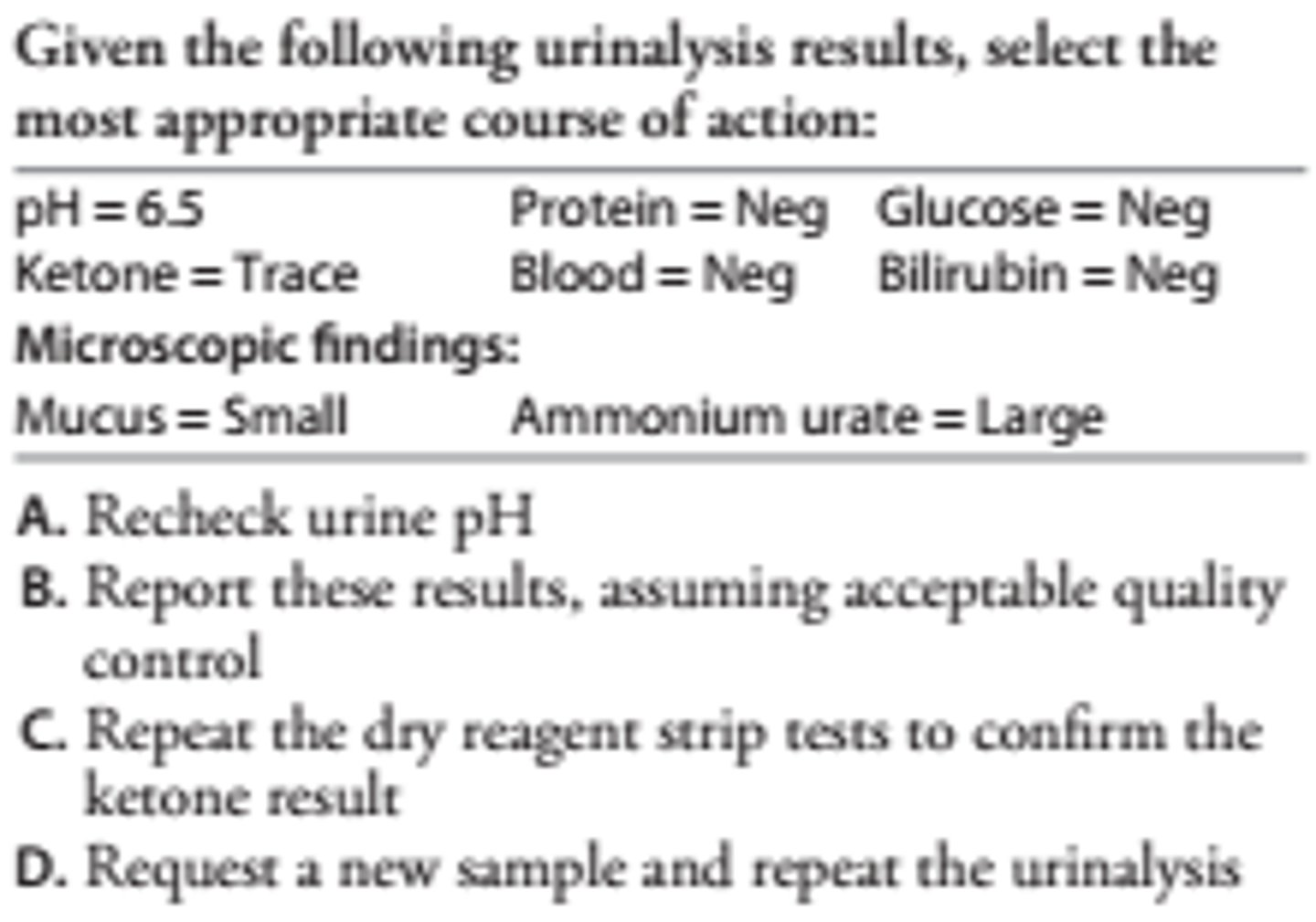
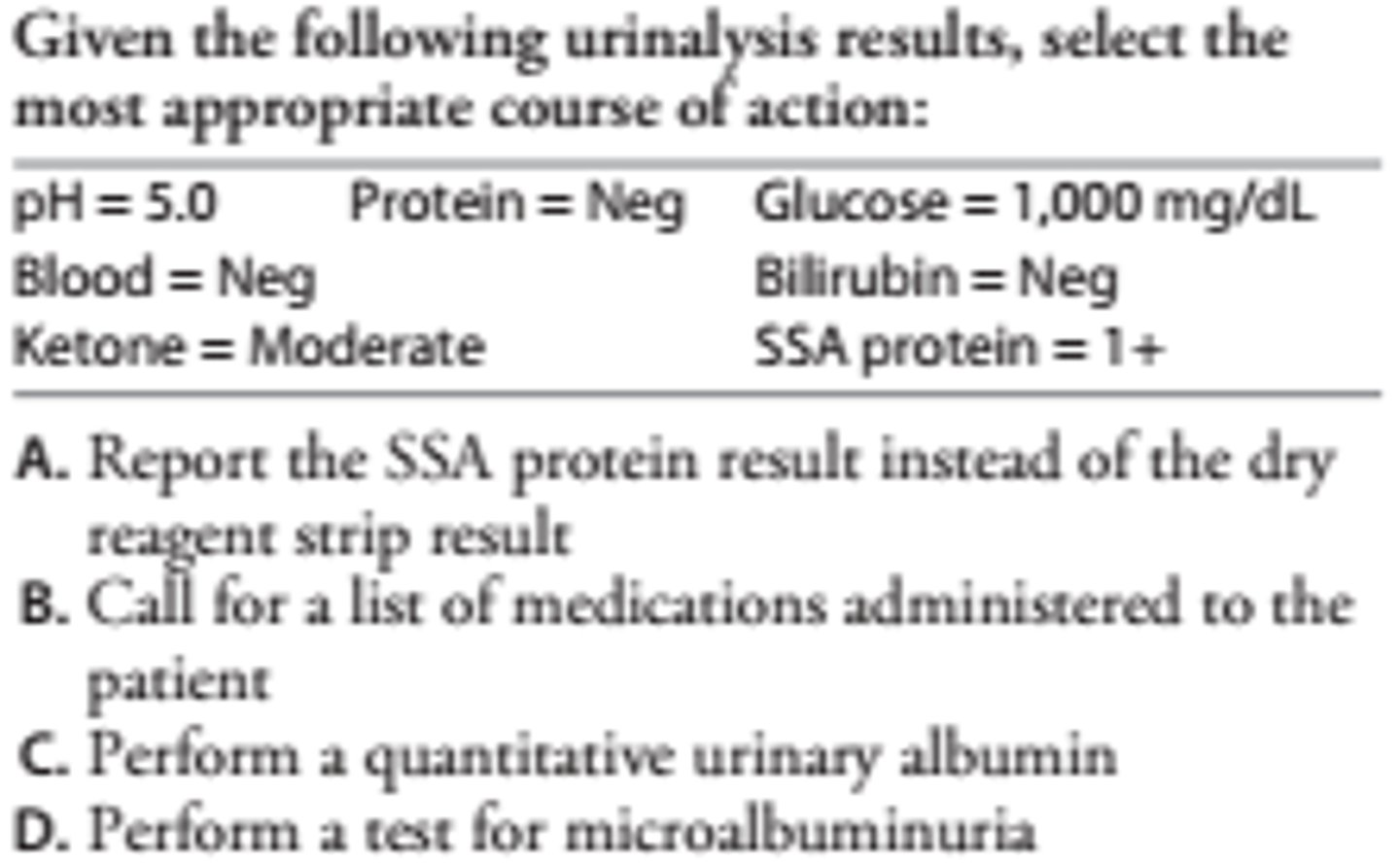
A-Ammonium urate crystals occur at alkaline pH only. The pH should be checked, and if below 7.0, the crystals should be reviewed in order to identify correctly. The trace ketone does not require confirmation, provided that the quality control of the reagent strips is acceptable.
A
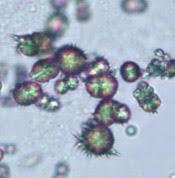
Bilirubin crystals cannot occur in urine without bilirubin. The tablet test is more sensitive than the dry reagent test and will confirm the presence of bilirubin. If negative, the crystals should be reviewed before reporting. Abnormal crystals occur only in acid or neutral urine.
A biochemical profile gives the following results:
Creatinine = 1.4 mg/dL
BUN = 35 mg/dL
K = 5.5 mmol/L
All other results are normal and all tests are in control. Urine from the patient has an osmolality of 975 mOsm/kg. Select the most appropriate course of action.
A. Check for hemolysis
B. Repeat the BUN and report only if normal
C. Repeat the serum creatinine and report only if elevated
D. Report these results
D. Report these results
Patients with prerenal failure usually have a BUN:creatinine ratio greater than 20:1. Reduced renal blood flow causes increased urea reabsorption and high urine osmolality. Patients are usually hypertensive and show fluid retention and hyperkalemia.
A 2 p.m. urinalysis has a trace glucose by the dry reagent strip test. A fasting blood glucose drawn 8 hours earlier is 100 mg/dL. No other results are abnormal. Select the most appropriate course of action.
A. Repeat the urine glucose and report if positive
B. Perform a test for reducing sugars and report the result
C. Perform a quantitative urine glucose; report as trace if greater than 100 mg/dL
D. Request a new urine specimen
A. Repeat the urine glucose and report if positive
The urine glucose is determined by the blood glucose at the time the urine is formed. The postprandial glucose (2 p.m.) level exceeded the renal threshold, resulting in trace glycosuria. Tests for reducing sugars are not used to confirm a positive urine glucose test.
Following a transfusion reaction, urine from a patient gives positive tests for blood and protein. The SG is 1.015. No RBCs or WBCs are seen in the microscopic examination. These results:
A. Indicate renal injury induced by transfusion reaction
B. Support the finding of an extravascular transfusion reaction
C. Support the finding of an intravascular transfusion reaction
D. Rule out a transfusion reaction caused by RBC incompatibility
C. Support the finding of an intravascular transfusion reaction
RBCs usually remain intact at a SG of 1.015. The absence of RBCs, WBCs, and casts points to hemoglobinuria caused by intravascular hemolysis rather than glomerular injury. A positive protein reaction will occur if sufficient hemoglobin is present.
A urine sample taken after a suspected transfusion reaction has a positive test for blood, but intact RBCs are not seen on microscopic examination. Which one test result would rule out an intravascular hemolytic transfusion reaction?
A. Negative urine urobilinogen
B. Serum unconjugated bilirubin below 1.0 mg/dL
C. Serum potassium below 6.0 mmol/L
D. Normal plasma haptoglobin
D. Normal plasma haptoglobin
The plasma free hemoglobin will be increased immediately after a hemolytic transfusion reaction, and the haptoglobin will be decreased. The hemoglobin will be eliminated by the kidneys, but the haptoglobin will remain low or undetectable for 2-3 days. Normal urine urobilinogen and serum unconjugated bilirubin help in ruling out extravascular hemolysis. Pretransfusion potassium is needed to evaluate the contribution of hemolysis to the posttransfusion result.
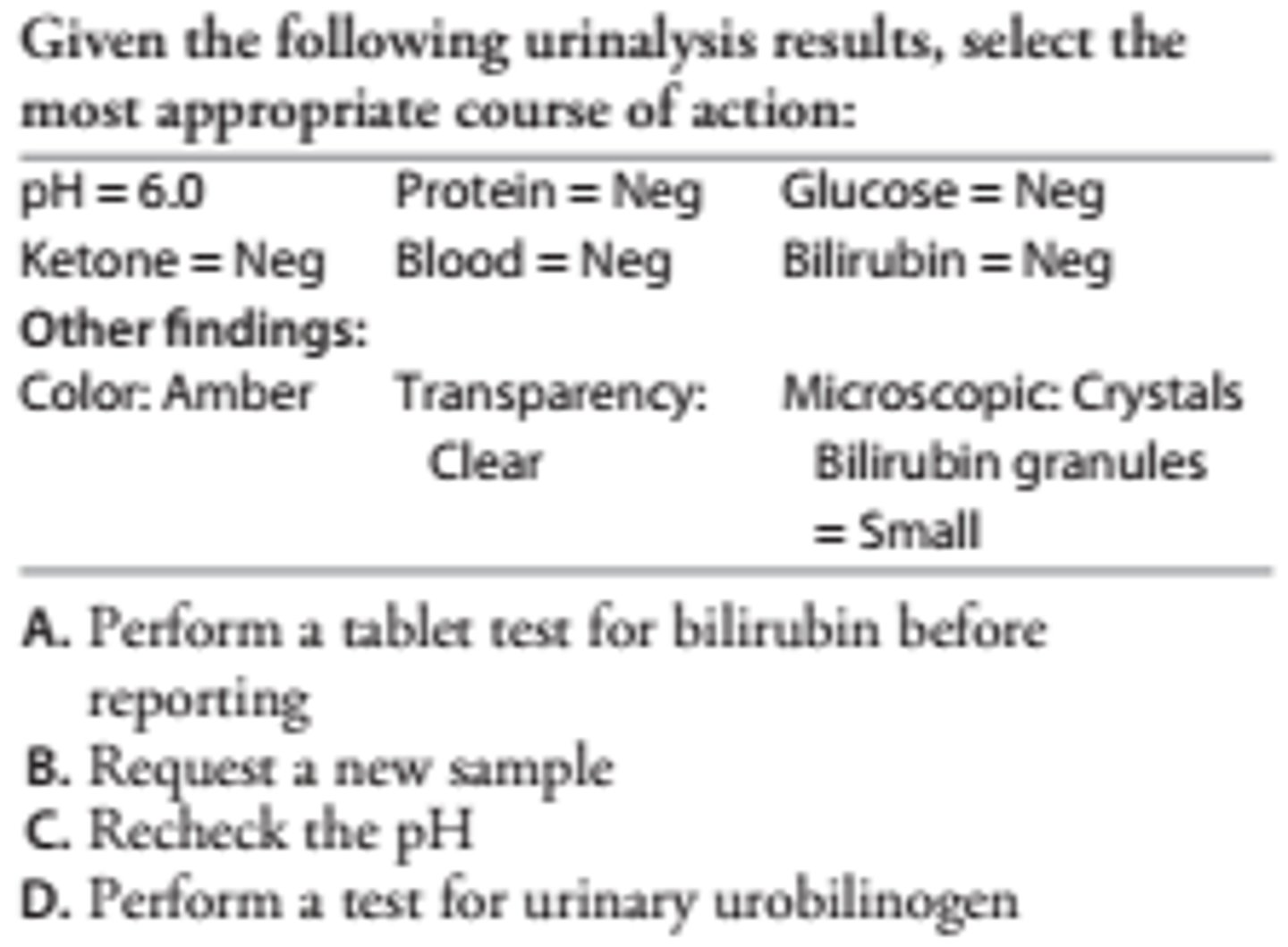
B
The combination of glucose- and ketone-positive urine points to a patient with insulin-dependent diabetes. A false-positive SSA test is likely if tolbutamide (Orinase) has been administered.
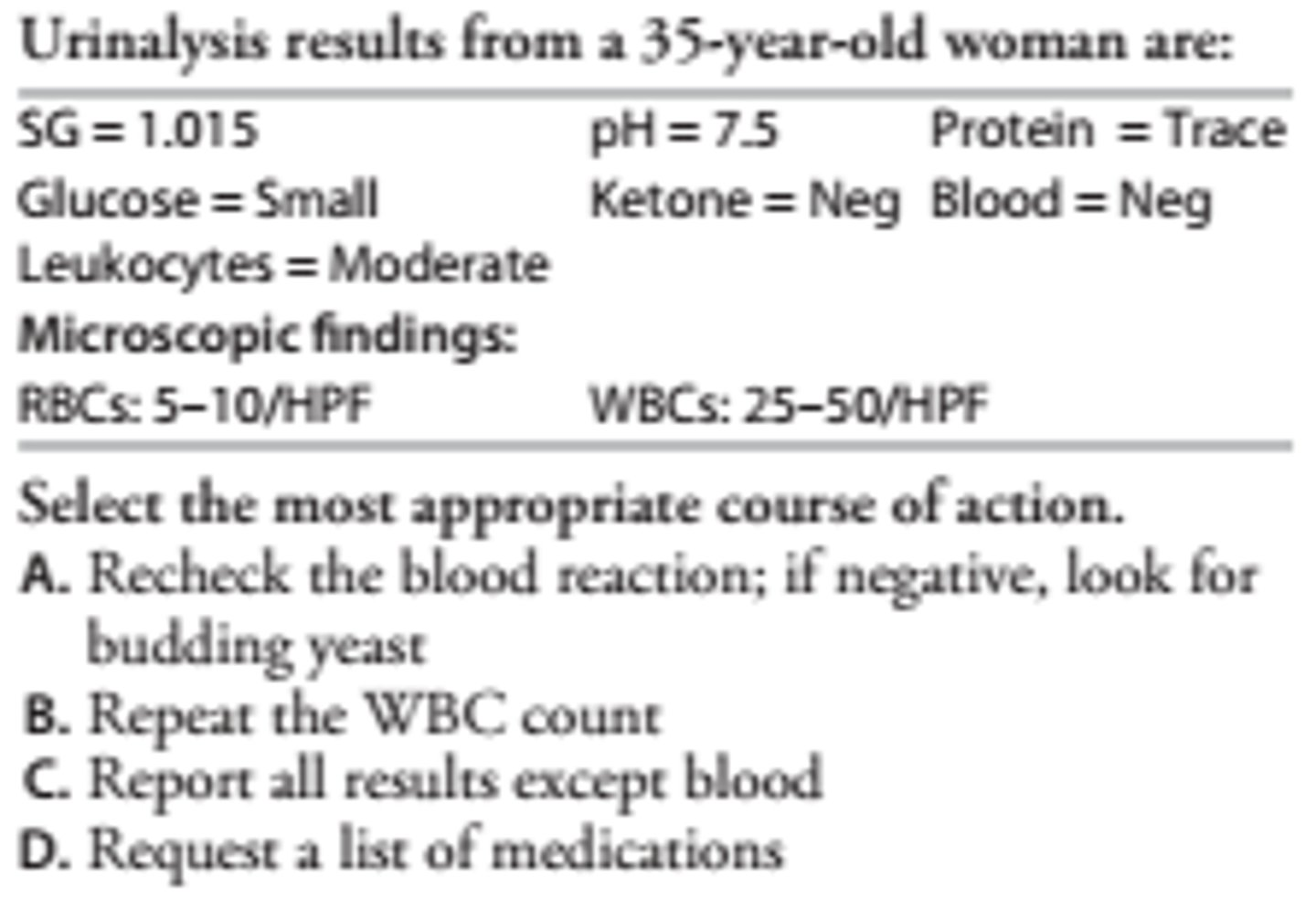
A-A nonhemolyzed trace may have been overlooked and the blood test should be repeated. A false negative (e.g., megadoses of vitamin C) rarely occurs. Yeast cells often accompany pyuria and glycosuria and are easily mistaken for RBCs.
C
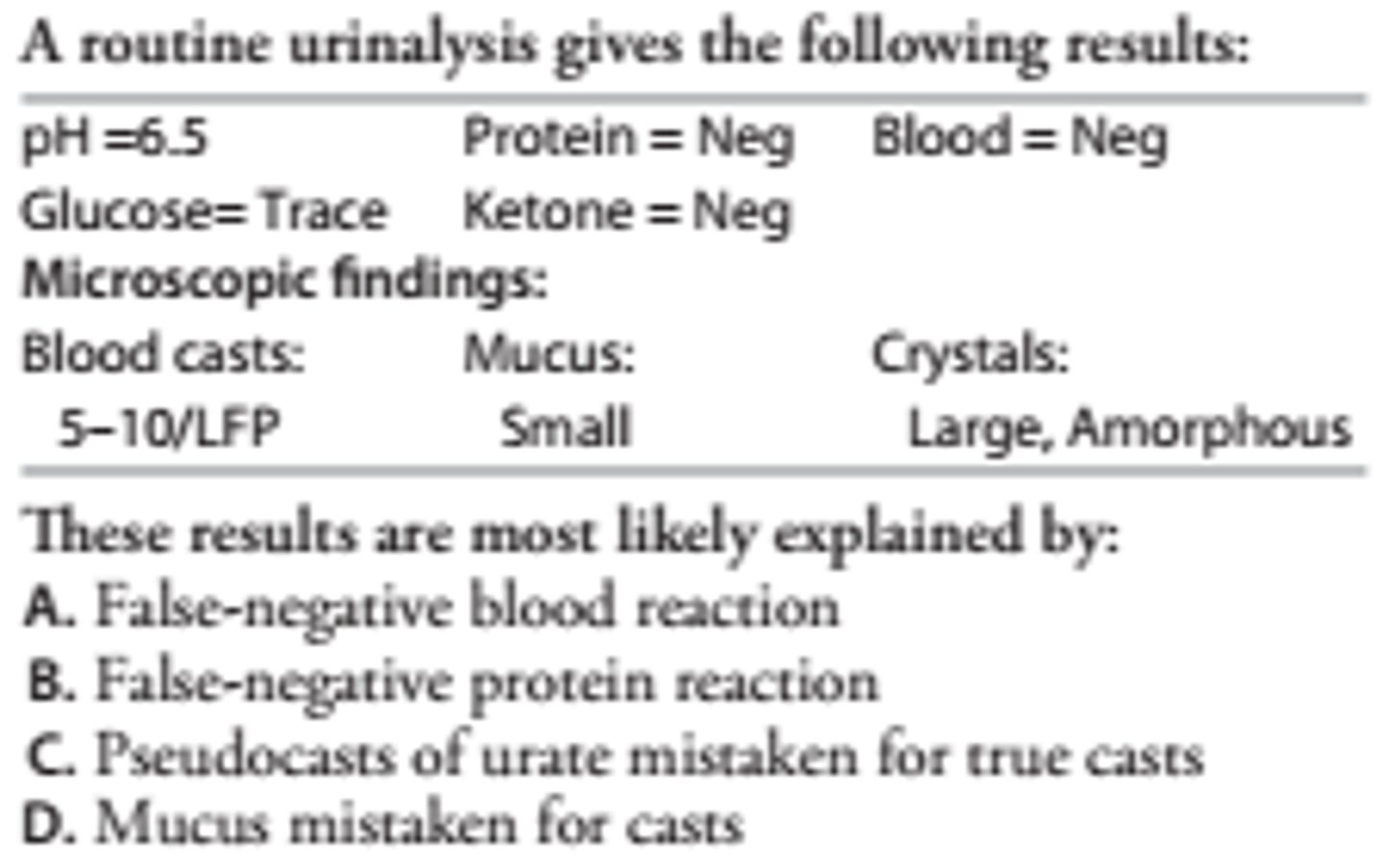
At pH 6.5, amorphous crystals are most often urate. These form yellow- or reddish-brown refractile deposits sometimes resembling blood or granular casts. The number of blood casts reported could not have occurred with negative protein and blood tests.
SITUATION: A urine specimen is dark orange and turns brown after storage in the refrigerator overnight. The technologist requests a new specimen. The second specimen is bright orange and is tested immediately. Which test result would differ between the two specimens?
A. Ketone
B. Leukocyte esterase
C. Urobilinogen
D. Nitrite
C. Urobilinogen
Urinary urobilinogen is increased in persons with extravascular hemolysis or hepatocellular liver disease. A freshly voided specimen is needed to detect urobilinogen because it is rapidly photooxidized to urobilin. This is accompanied by a color change from orange to brown. Urobilin does not react with 2,4 dimethylaminobenzaldehyde or 4-methoxybenzene diazonium tetrafluoroborate, which are used to detect urobilinogen. Consequently, the urobilinogen test in the first sample will be normal, but will be increased in the second sample if tested immediately after collection. The best sample for detecting urobilinogen is a 2-hour timed urine sample collected in the midafternoon, when urobilinogen excretion is highest. Ketones and nitrites do not alter the pigment of the urine sample. Leukocytes cause the urine to be turbid but do not cause abnormal color. These three tests are stable for 24 hours when urine is refrigerated within 30 minutes of collection.
A patient's random urine consistently contains a trace of protein but no casts, cells, or other biochemical abnormality. The first voided morning sample is consistently negative for protein. These findings can be explained by:
A. Normal diurnal variation in protein loss
B. Early glomerulonephritis
C. Orthostatic or postural albuminuria
D. Microalbuminuria
C. Orthostatic or postural albuminuria
Protein and other constituents of urine will often be highest in the first morning void. A normal first-voided sample makes glomerular disease highly unlikely. Orthostatic albuminuria is a benign condition sometimes seen in adolescents who are tall and have bent posture that puts back pressure on the kidneys. The quantity of albumin excreted into the urine is small. Diagnosis is made by demonstrating a positive test after the person is erect for several hours, and the absence of proteinuria when the person is recumbent. Microalbuminuria seen in diabetic persons is usually accompanied by a positive test for urinary glucose.
A urine sample with a pH of 8.0 and a specific gravity of 1.005 had a small positive blood reaction, but is negative for protein and no RBCs are present in the microscopic examination of urinary sediment. What best explains these findings?
A. High pH and low SG caused a false-positive blood reaction
B. The blood reaction and protein reaction are discrepant
C. Hemoglobin is present without intact RBCs due to hemolysis
D. An error was made in the microscopic examination
C. Hemoglobin is present without intact RBCs due to hemolysis
RBCs will lyse in alkaline or dilute urine, and this sample displays both. The blood test is sensitive to as little is 0.015 mg/dL hemoglobin, and the protein test is significantly less sensitive. As a result, a trace to small positive blood and negative protein test are commonly encountered.
A urine sample has a negative blood reaction and 5-10 cells per high-power field that resemble red blood cells. What is the best course of action?
A. Mix a drop of sediment with 1 drop of WBC counting fluid and reexamine
B. Report the results without further testing
C. Repeat the blood test and if negative report the results
D. If the leukocyte esterase test is positive, report the cells as WBCs
A. Mix a drop of sediment with 1 drop of WBC counting fluid and reexamine
When 5-10 RBCs/HPFs are seen, the blood test should show a nonhemolyzed trace. Therefore, it is likely that the cells are not RBCs. RBCs are easily confused with nonbudding yeast and may also be mistaken for WBCs. RBCs will lyse in dilute acetic acid but yeast and WBCs will not. If a yeast infection is present, then the leukocyte esterase test will likely be positive; therefore, the leukocyte esterase test cannot be used to determine the identity of the cells. Sternheimer-Malbin stain can be used to differentiate WBCs from RBCs and yeast.
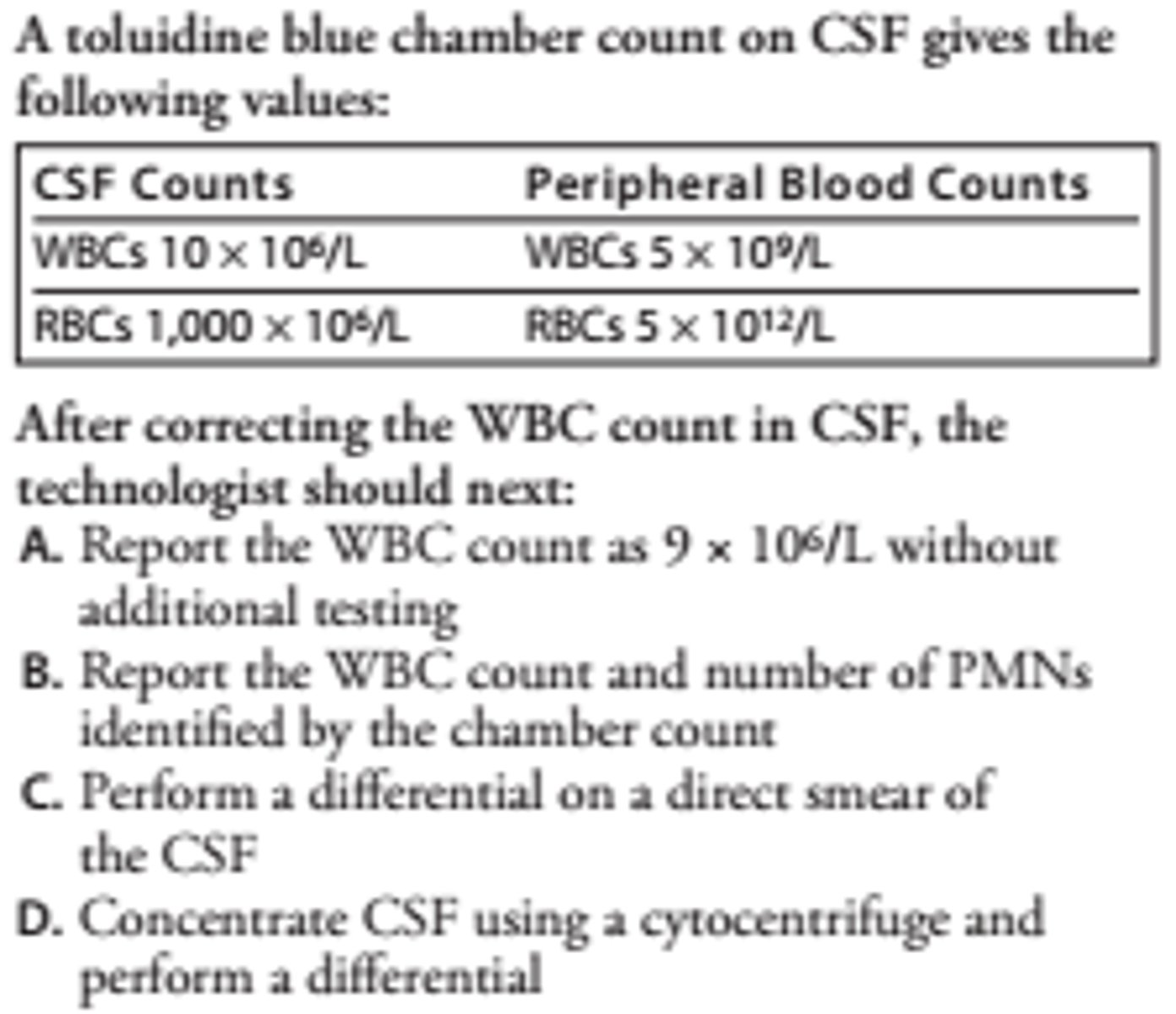
D-A differential is performed using CSF concentrate on all neonatal samples and whenever the WBC count is > 5μL. A toluidine blue chamber count of PMNs is not sufficiently sensitive to detect neutrophilic pleocytosis.
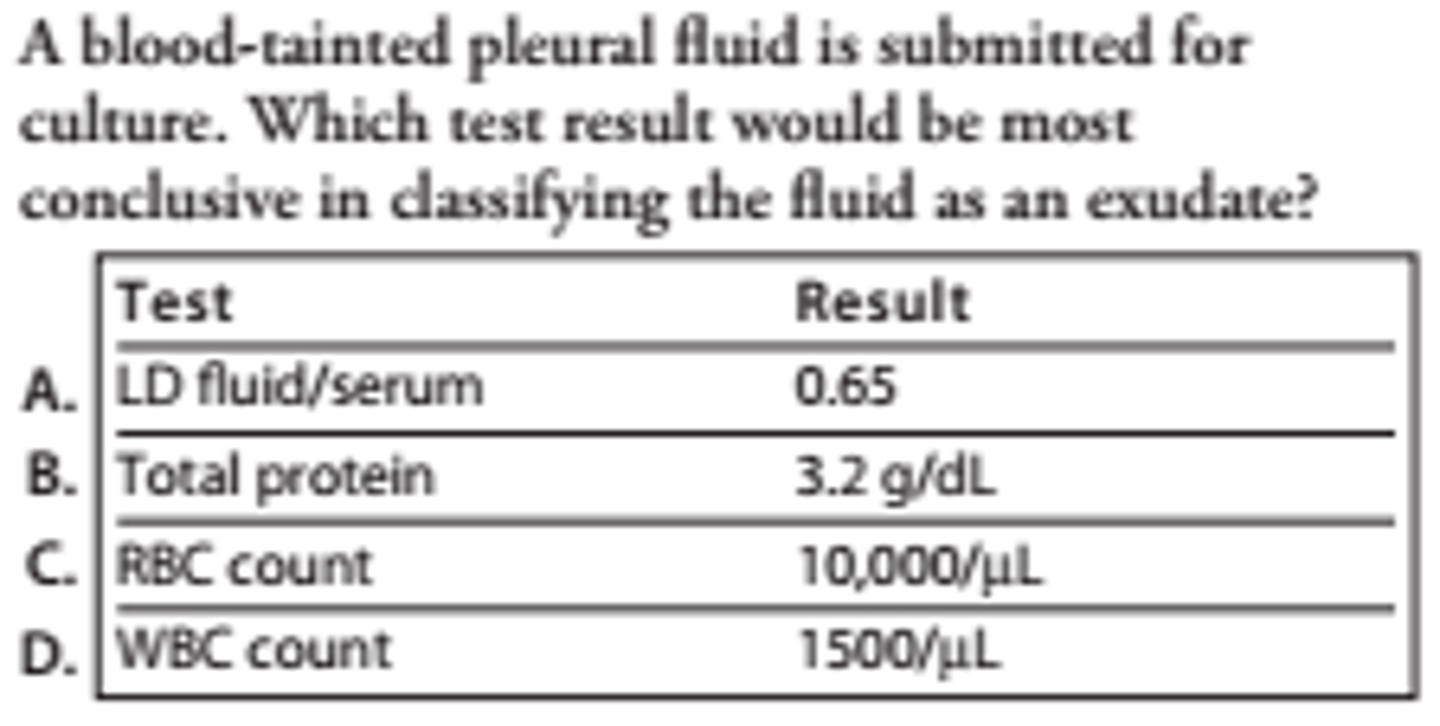
A-A traumatic tap makes classification of fluids difficult on the basis of cell counts and protein. The values reported for protein, RBCs, and WBCs can occur in either an exudate or bloody transudate, but the LD ratio is significant.
A WBC count and differential performed on ascites fluid gave a WBC count of 20,000μL with 90% macrophages. The gross appearance of the fluid was described by the technologist as "thick and bloody." It was noted on the report that several clusters of these cells were observed and that the majority of the cells contained many vacuoles resembling paper-punch holes. What do the observations above suggest?
A. Malignant mesothelial cells were counted as macrophages
B. Adenocarcinoma from a metastatic site
C. Lymphoma infiltrating the peritoneal cavity
D. Nodular sclerosing type Hodgkin's disease
A. Malignant mesothelial cells were counted as macrophages
Bloody, exudative fluids with a preponderance of a singular cell type are suggestive of malignancy. The cellularity in malignancy is variable but lymphocytosis occurs in about half of cases. Mesothelial cells normally comprise less than 10% of the cells in serous fluid. They may be resting cells, reactive, degenerated, or phagocytic in nonmalignant conditions. In inflammatory conditions, they are often increased and resemble macrophages. However, clusters or balls of such cells and paper-punch vacuoles throughout the cytoplasm and over the nucleus are characteristics of malignant mesothelial cells. Such cells secrete hyaluronic acid, making the fluid highly viscous. The gross appearance of this fluid suggests malignancy. The description of these cells points to mesothelioma, and this specimen should be referred for cytological examination in order to confirm the diagnosis.
Harr, Robert R. Medical Laboratory Science Review (Page 376). F.A. Davis Company. Kindle Edition.
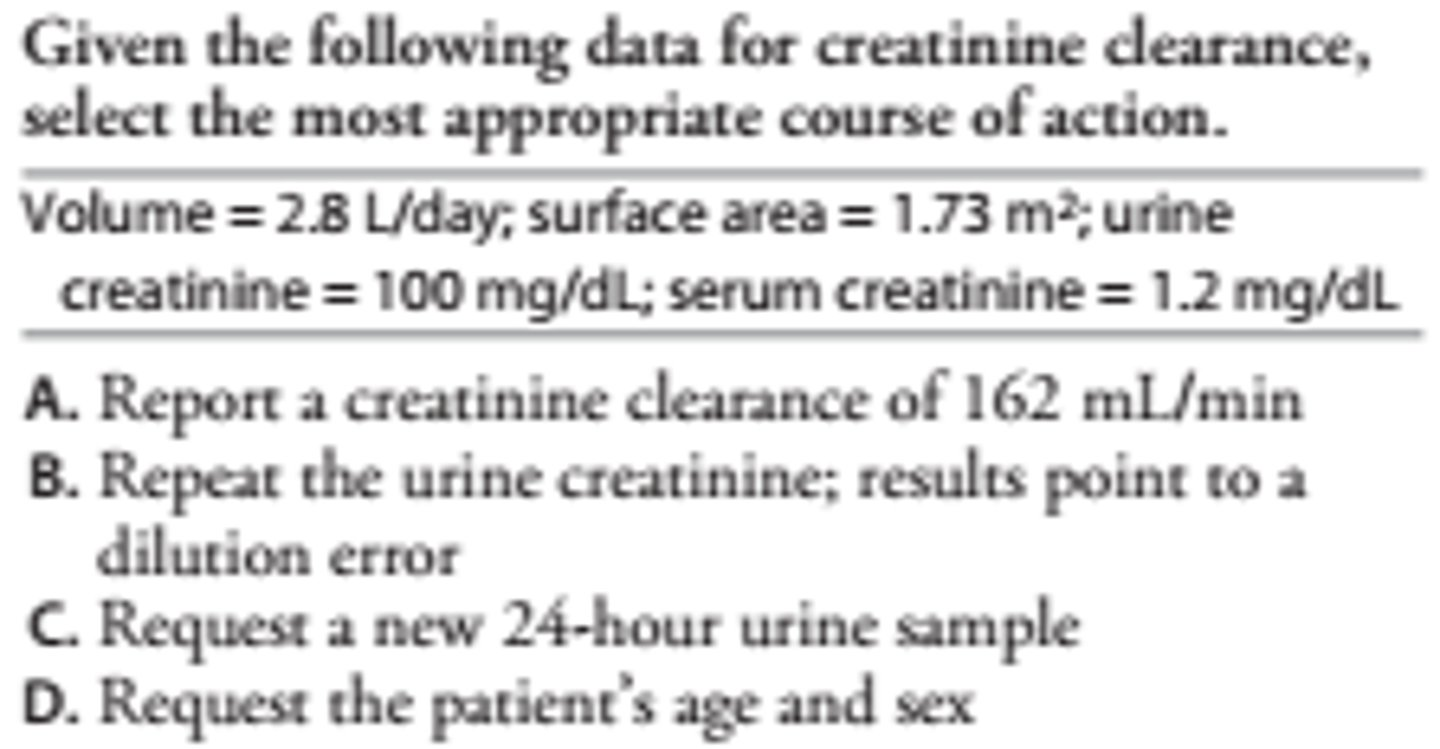
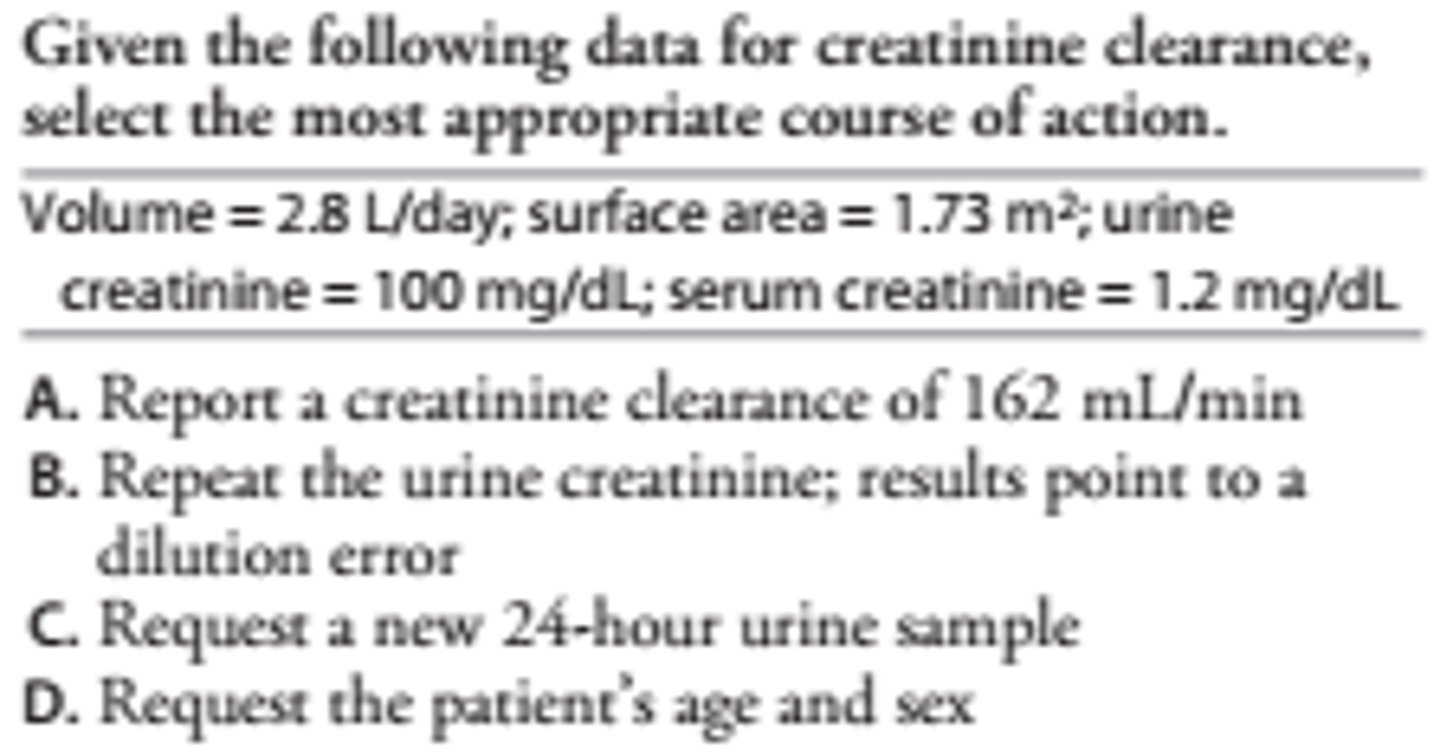
C
A calculated clearance in excess of 140 mL/min is greater than the upper physiological limit. The high volume per day suggests addition of H2 O to the sample. The result should be considered invalid.
An elevated amylase is obtained on a stat serum collected at 8 p.m. An amylase performed at 8 a.m. that morning was within normal limits. The technologist also noted that a urine amylase was measured at 6 p.m. Select the most appropriate course of action.
A. Repeat the stat amylase; report only if within normal limits
B. Repeat both the a.m. and p.m. serum amylase and report only if they agree
C. Request a new specimen; do not report results of the stat sample
D. Review the amylase result on the 6 p.m. urine sample; if elevated, report the stat amylase
D
Serum amylase peaks 2-10 hours after an episode of acute pancreatitis and this may have caused the elevated serum amylase at 8 p.m. Urinary amylase parallels serum amylase; therefore, a positive urine test at 6 p.m. makes sample collection error unlikely.
Harr, Robert R. Medical Laboratory Science Review (Page 377). F.A. Davis Company. Kindle Edition.
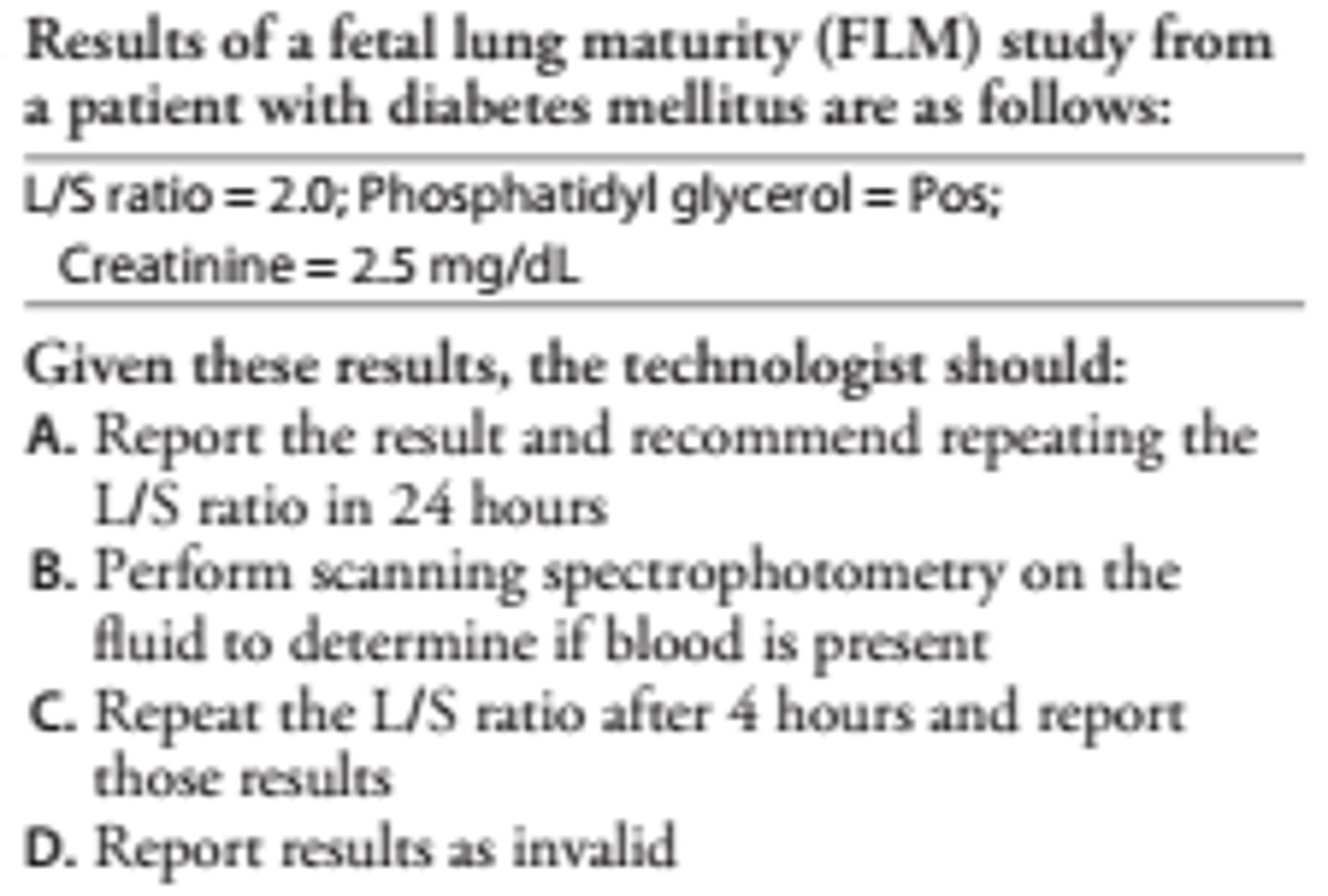
A-In patients with diabetes, lung maturity may be delayed and an L/S ratio of 2:1 may be associated with respiratory distress syndrome. A positive PG spot correlates with an L/S ratio of 2:1 or higher and rules out a falsely increased result caused by blood contamination. The best course of action is to wait an additional 24 hours and perform another L/S ratio on a fresh sample of amniotic fluid because an L/S ratio of 3:1 would indicate a high probability of fetal lung maturity.
A 24-hour urine sample from an adult submitted for catecholamines gives a result of 140 μg/day (upper reference limit 150 μg/day). The 24-hour urine creatinine level is 0.6 g/day. Select the best course of action.
A. Check the urine pH to verify that it is less than 2.0
B. Report the result in μg catecholamines per mg creatinine
C. Request a new 24-hour urine sample
D. Measure the VMA and report the catecholamine result only if elevated
C. Request a new 24-hour urine sample
Urine creatinine of less than 0.8 g/day indicates incomplete sample collection. The patient's daily catecholamine excretion would be misinterpreted from this result.
A 5-hour urinary D-xylose test on a 7-year-old boy who was given 0.5 g of D-xylose per pound is 15%. The 2-hour timed blood D-xylose is 15 mg/dL (lower reference limit 30 mg/dL). Select the most appropriate action.
A. Request that a βcarotene absorption test be performed
B. Repeat the urinary result because it is borderline
C. Request a retest using a 25-g dose of D-xylose
D. Request a retest using only a 1-hour timed blood sample
D. Request a retest using only a 1-hour timed blood sample
Urinary xylose excretion is less reliable in children under the age of 10, and peak blood levels occur sooner than in adults. A 60-minute blood sample should have been used. A serum D-xylose level greater than 30 mg/dL at 1 hour is considered normal. Tests for anti-tissue transglutaminase and other antibodies produced in celiac disease have resulted in diminished use of the D-xylose absorption test.
A quantitative serum hCG is ordered on a male patient. The technologist should:
A. Perform the test and report the result
B. Request that the order be cancelled
C. Perform the test and report the result if negative
D. Perform the test and report the result only if greater than 25 IU/L
A. Perform the test and report the result
hCG may be produced in men by tumors of trophoblastic origin, such as teratoma and seminoma, and is an important marker for nontrophoblastic tumors, as well.
SITUATION: A lamellar body count (LBC) was performed on an amniotic fluid sample that was slightly pink in color within 1 hour of specimen collection. The sample was stored at 4°C prior to analysis. The result was 25,000/μL, classified as intermediate risk of respiratory distress syndrome. The physician waited 24 hours and collected a new sample that was counted within 2 hours of collection on the same instrument. The LCB count of the new sample was 14,000/ μL and the patient was reclassified as high risk. Which statement best explains these results?
A. Loss of lamellar bodies occurred in the second sample because of storage
B. Blood caused a falsely elevated result for the first sample
C. The fetal status changed in 24 hours owing to respiratory illness
D. The difference in counts is the result of day-to-day physiological and instrument variance
B. Blood caused a falsely elevated result for the first sample
Lamellar bodies are small particles containing pulmonary surfactants that are made by Type II pneumocytes, and their number in amniotic fluid increases as the concentration of phospholipids increases. They are about the same size as platelets and are counted in the platelet channel of cell counters. If the amniotic fluid sample is contaminated with blood, platelets will falsely raise the lamellar body count. Amniotic fluid samples for LBC are stable for several days when stored at 4°C. However, cutoffs for fetal lung maturity need to be established by each laboratory since there are significant differences in LBCs between different counters.
When testing for drugs of abuse in urine, which of the following test results indicate dilution and would be cause for rejecting the sample?
A. Temperature upon sample submission 92°F
B. Specific gravity 1.002; Creatinine 15 mg/dL,
C. pH 5.8; temperature 94°C
D. Specific gravity 1.012, creatinine 25 mg/dL
B. Specific gravity 1.002; Creatinine 15 mg/dL
Tampering with a sample submitted for abuse substance testing can be either by dilution or substitution. Substance Abuse and Mental Health Services Administration (SAMHSA) certified workplace drug testing labs are required to test for both, and reject samples based on SAMHSA cutoffs. A specimen is too dilute for testing if the creatinine is below 20 mg/dL and specific gravity below 1.003. A sample is considered substituted if the creatinine is below 5.0 mg/dL and the specific gravity less than 1.002. Values above for pH and temperature are within acceptable limits.
SITUATION: A urine specimen has a specific gravity of 1.025 and is strongly positive for nitrite. All other dry reagent strip test results are normal, and the microscopic exam was unremarkable, showing no WBCs or bacteria. The urine sample was submitted as part of a preemployment physical exam that also includes drug testing. Which most likely caused these results?
A. A viral infection of the kidney
B. A urinary tract infection in an immunosuppressed person
C. An adulterated urine specimen
D. Error in reading the nitrite pad caused by poor reflectometer calibration
C. An adulterated urine specimen
Urine validity testing for drugs of abuse includes tests for nitrite, glutathione, pyridinium dichromate, and peroxide in addition to pH, specific gravity, and creatinine. These substances are known to cause negative interference in the EMIT immunoassay. A viral infection of the kidney would be associated with high numbers of renal tubular epithelial cells and leukocytes. An infection in an immunosuppressed person would still produce urinary WBCs. While laboratory error is possible, a false positive caused by reflectometer error would be suspected if the test pad were negative when reading it manually.
A CSF sample submitted for cell counts has a visible clot. What is the best course of action?
A. Count RBCs and WBCs manually after diluting the fluid with normal saline
B. Tease the cells out of the clot before counting, then dilute with WBC counting fluid
C. Request a new sample
D. Perform a WBC count without correction
C. Request a new sample
CSF samples will not clot as a result of a subarachnoid hemorrhage. While the sample is still suitable for microbiological analysis, it will not give reliable cell counts or biochemistry results owing to extensive contamination with peripheral blood.
Total hemolytic complement and glucose are ordered on a synovial fluid sample that is too viscous to pipet. What is the best course of action?
A. Dilute the sample in saline
B. Add 1 mg/mL hyaluronidase to the sample and incubate at room temperature for 30 minutes
C. Warm the sample to 65°C for 10 minutes
D. Request a new specimen
B. Add 1 mg/mL hyaluronidase to the sample and incubate at room temperature for 30 minutes
Joint fluid too viscous to pipet accurately cannot be diluted accurately. Complement is heat labile and total hemolytic complement is destroyed when the sample is heated to 56°C for 5 minutes. Joint fluid is difficult to collect and a new sample is likely to have the same problem.
A CSF CytoPrep smear shows many smudge cells and macrophages with torn cell membranes. What most likely caused this problem?
A. Failure to add albumin to the cytospin cup
B. Failure to collect the CSF in EDTA
C. Centrifuge speed too low
D. Improper alignment
A. Failure to add albumin to the cytospin cup
Cellular distortion caused by centrifugation is a common problem, and can be reduced by adding 22% bovine albumin or 10% dextran to the cytospin cup along with the sample. CSF does not clot because it contains no fibrinogen, and the sample can be collected and counted without anticoagulant.
An automated electronic blood cell counter was used to count RBCs and WBCs in a turbid pleural fluid sample. The WBC count was 5 × 1010/L (50,000/μL) and the RBC count was 5.5 × 1010/L (55,000/ μL). What is the significance of the RBC count?
A. The RBC count is not significant and should be reported as 5,000/μL
B. The RBC count should be reported as determined by the analyzer
C. A manual RBC count should be performed
D. A manual RBC and WBC count should be performed and reported instead
A. The RBC count is not significant and should be reported as 5,000/μ
Electronic cell counters are validated for body fluid cell counts with specific minimum detection limits. For most counters, this is 50-200 WBC/μL and 10,000 RBC/μL. Since the RBCs are lysed in the WBC bath, the WBC count represents the number of nucleated cells present. However, WBCs are not lysed in the RBC bath and would be counted as RBCs. In this case, the empyemic fluid would cause the RBCs count to be erroneously elevated, and this should be corrected before reporting by subtracting the WBC count from the RBC count.