Developmental Anatomy Wk 1
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
When does male gametogenesis commence?
at puberty, age 9 to 14
Where are male gametes produced?
in the seminiferous tubules of the testis and then move to the epididymis where it matures and becomes motile. the motile spermatozoa are stored within the epididymis until ejaculation
What is the anatomy of the spermatozoa?
the head of the spermatozoa contains the nucleus and the acrosome/acrosomal cap contains digestive enzymes that aids in fertilisation
What does the female urogenital tract involve?
ovaries, uterine tube (oviduct), uterus, cervix of the uterus, and the vagina
When are female gametes produced?
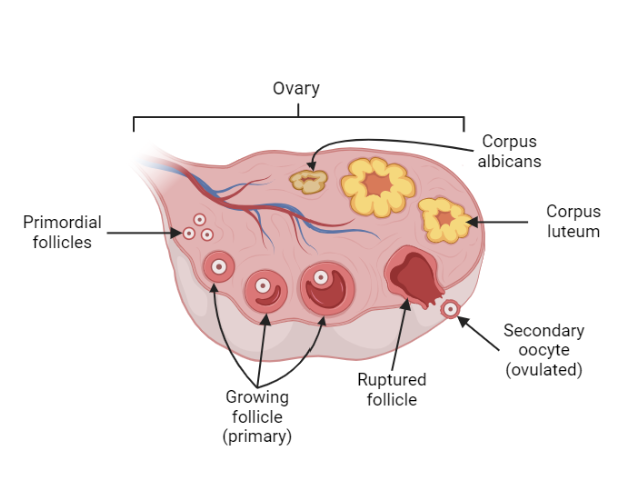
produced in the ovaries and after menarchy (first period). 20 primordial follicles undergo development until only one oocyte erupts from the ovary each month (ovulation)
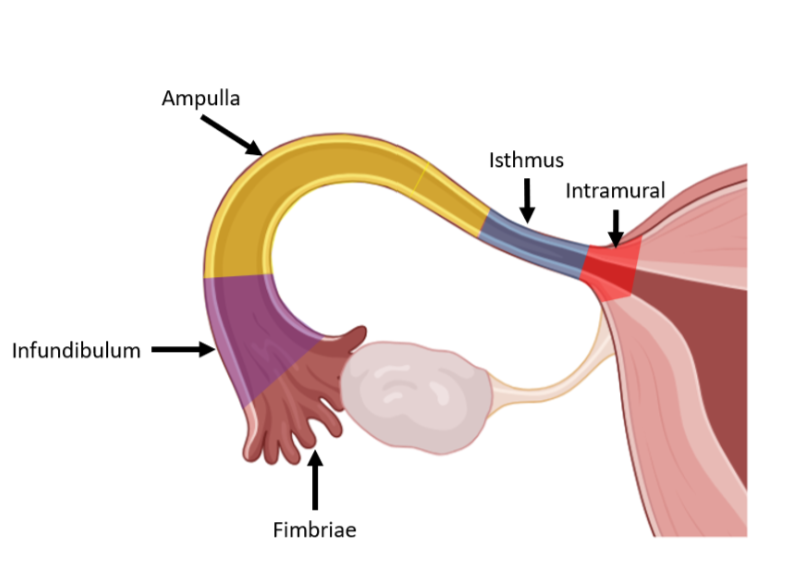
What are the five parts of the oviduct (uterine tube)?
fimbriae, infundibulum, ampulla, isthmus, and intramural parts
When does female gametogenesis commence?
at the 5th month of foetal development but undergo mitotic arrest until puberty (8 to 13 years)
How to primordial follicles develop into primary follicles?
then only one mature/graffian follicle (secondary follicle) will erupt from the follicle. the remaining ruptured follicle will develop into the corpus luteum
What does the male gamete (spermatozoa) do in the initial stage of fertilisation?
it becomes hypermobile and ascend towards the ampulla of the uterine tube (oviduct)
What is process of the spermatozoa initial fertilise?
1. it wriggles between the corona radiata and the acrosomal enzymes within the acrosome contact the zona pellucida. the enzymes dissolve the zona pellucida and the sperm reaches the oocyte. 2. the nuclei of both male and female gametes fuse resulting in a zygote 3. cortical granules of the oocyte then cause the zona pellucida to become impenetrable to other sperm, therefore preventing polyspermy
What does polyspermy mean?
fertilisation of the oocyte by more than one spermatizoon
What happens after fertilisation?
the zygote undergoes a series of mitotic cell divisions, called cleavage, each division results in a doubling of cell number
What is a morula?
when the embryo consists of 16 to 32 cells
How are blastocytes formed?
formation of a fluid-filled cavity in the morula marks the change to the blastocyte phase. the differentiated cells are now called trophoblast that form an outer ring of cells and the embryoblast or inner cell mass forming a cluster of cells on one side of the embryo
How do blastocytes hatch?
on day 6 the blastocyst has arrived in the body of the uterus, hatches from the zona pellucida and is ready to implant. outside of the zona pellucida, the blastocyst is ‘sticky’ and will implant on the first surface it comes into contact with. the blastocyst hatches by enzymatically boring a hole through the zona pellucida and squeezes out
What does implantation describe?
the attachment of the embryo to the uterine wall where maternal nutrient transfer is established
What is the process of early implantation?
the trophoblast is the precursor of the placenta and penetrated the epithelial cells of the uterine wall to initiate proliferation of blood vessels to provide nutrition to the embryo. the embryoblast differentiated into the epiblast and the hypoblast
What is complete implantation?
at day 10 the blastocyst is now located deep within the uterine endometrium. the trophoblast start secreting human chorionic gonadotropin (hCG). hCG promotes the continued production of progesterone from the corpus luteum of the ovary stimulating uterine changes to accomodate the growing embryo/foetus
What does human chorionic gonadotropin (hCG) do?
common for pregnancy tests as a positive indicator of pregnancy. it is the increased levels of progesterone that stimulate a thickening of the endometrium and myometrium of the uterus during pregnancy
What does the trophoblast differentiate into in complete implantation?
into two layers: (1) the cellular cytotrophoblast and (2) a multinucleated and expanding syncytiotrophoblast. the uterus, cytotrophoblast and syncytiotrophoblast together initiate the formation of the placenta
What does ectopic pregnancy mean?
pregnancies that occur outside the typical location of the body of the uterus
What does Gonadotropin releasing hormones do (GnRH)?
released by the hypothalamus and stimulates the anterior pituitary gland to produce and secrete luteinising and follicle stimulating hormones
What does Luteinising hormone (LH) do?
produced by the anterior pituitary gland and is involved in triggering ovulation
What does Follicle stimulating hormone (FSH)?
produced by the anterior pituitary gland and is involved in stimulating follicular growth and ovulation
What does progesterone do?
produced by the corpus luteum to stimulate glandular development, increase blood vessel size and shape (coils), to proliferate and increase endometrial thickness
What does Human chorionic gonadotropin (hCG)?
produced by syncytiotrophoblast to stimulate continued production of progesterone by the corpus luteum