Chapter 18: The circulatory system: Blood
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
99 Terms
Describe Hematology
Study of blood, blood forming tissues +the disorder associated with them
What are the three main functions of blood?
1. Transport
- lungs->o2->co2->lung
-metabolic waste--> kidneys
- Hormones
2. Protection
-Inflammation → Fights infection
-White Blood Cells (WBCs)
-Antibodies → Destroy pathogens
-Platelets → Blood clotting
3. Regulation
-Maintains body temperature
-Blood vessel constriction & dilation
-Blood proteins act as buffers to maintain pH balance
How does blood transport?
-O2 from the lungs to the body cells, Co2 from the body cells to the lungs
-Metabolic waste to Kidneys for removal
-Hormones from endocrine glands to target organ
How does blood protect?
-Blood clots protecting against excessive bleeding after injury
-White blood cells protect against disease by phagocytizing pathogens
-Blood proteins like antibodies, inter neurons help, protect against disease and variety of ways
How does blood function do Regulation?
-Maintains body temperature
-Helps maintain homeostasis of all body fluids
-Blood osmotic, pressure influences water content of cells (isotonic, hypotonic, and hypertonic solutions)
-Helps regulate through use of buffers
Which blood component is responsible for transporting hormones?
-Transport
What percentage of blood plasma is water?
About 91.5% water and 8.5% solutes (mostly proteins)
* Proteins: Albumin Globulins, and fibrogin
* Solutes: electrolytes, nutrients, regulatory substance, waster products
What are the three main components of blood?
Platelets, Plasma Proteins, White blood cells
Plasma being mostly h2o is important. Rember h2o is most important ______ h20 also controls ________and blood pressure
-Solvent
-Blood volume
Which plasma protein helps maintain osmotic pressure?
-Albumin → Regulates water balance, osmotic pressure, and viscosity
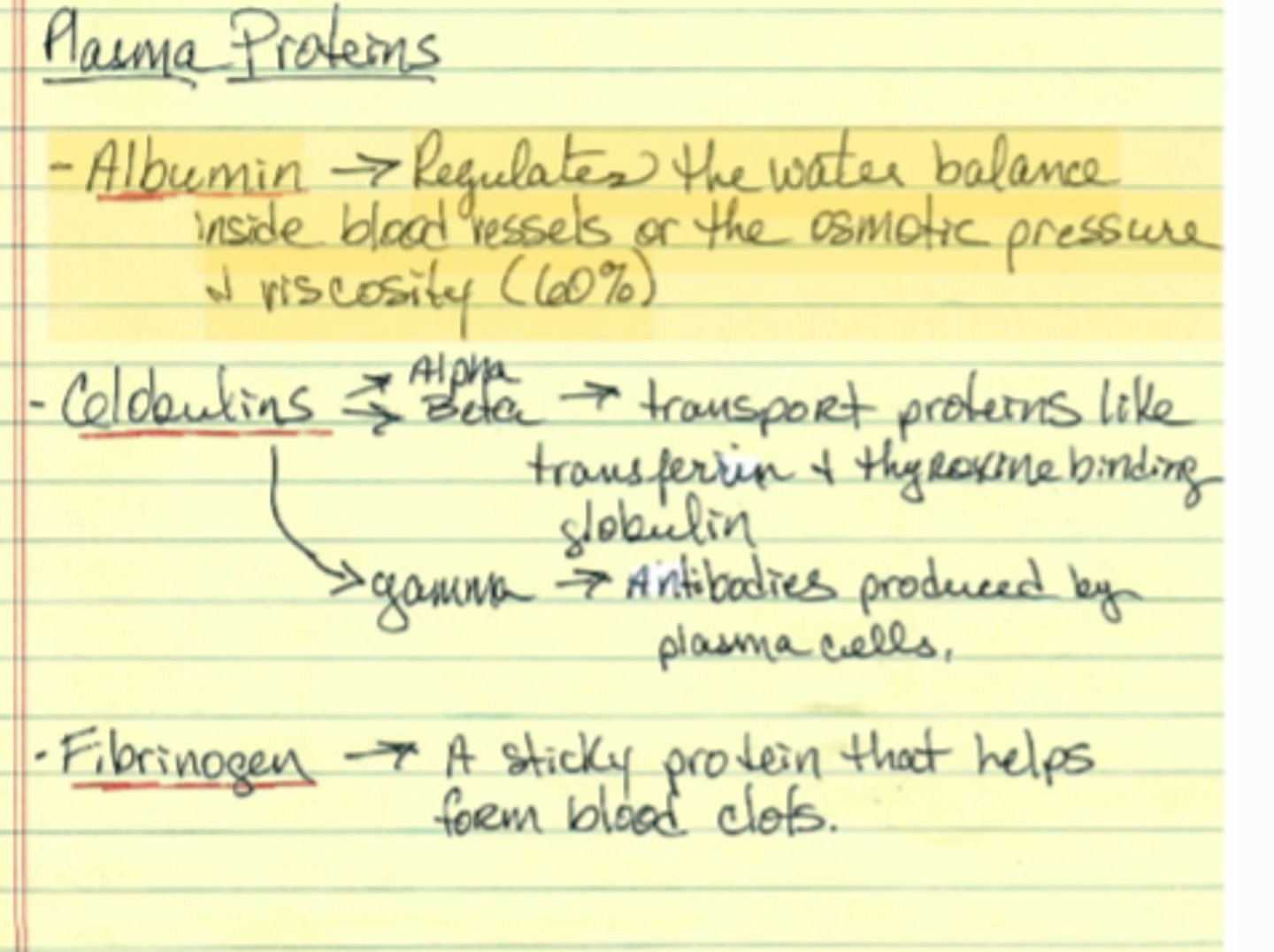
What is the primary role of Fibrogen?
A sticky protein that helps form blood clots
Role of _________ is one of the 3 plasma proteins that contain alpha and beta. Then transferrin + thyroxine binding goblin
- Gamma--> antibodies produced by plasma cells
Globulins
What is the primary function of erythrocytes (RBCs)?
Transports o2 and co2
-Erythrocytes (RBCs) No nucleus, no organelles
-97% hemoglobin → Binds and releases O₂
-Hemoglobin Structure:
-2 alpha proteins
-2 beta proteins
-and 4 Heme molecules & each with a iron molecule
-also NO metabolic activities
Name the five types of White Blood Cells (WBCs). Leukocytes
Granulocytes → Neutrophils, Eosinophils, Basophils
Agranulocytes → Lymphocytes (B cell, Tcells), Monocytes
Which of the following is NOT a formed element of blood?
a) Erythrocytes
b) Leukocytes
c) Platelets
d) Plasma
d) Plasma
RBC life cycle- Why do RBC not have a nucleus?
They did at first but they get rid of it to make room for the hemoglobin + o2 they carry
What is the process of blood cell formation called?
a) Hemostasis
B) Hematopoiesis
B Hematopoiesis
Where does hematopoiesis primarily occur in adults?
Red bone marrow
What is the lifespan of an RBC?
120
What is the name of the hormone that regulates RBC production?
Erythropoietin (EPO) → Hormone that regulates RBC production
Where are RBCs broken down?
RBC breakdown:
- Spleen (RBC graveyard), Liver, Bone marrow (macrophages recycle parts)
- Globin → Broken down into amino acids
- Iron → Stored in liver
- Heme → Converted to bilirubin → Liver → Bile → Feces
What happens to the heme portion of hemoglobin after RBC breakdown?
- Heme → Converted to bilirubin → Liver → Bile → Feces
What stimulates the production of erythropoietin (EPO)?
What is the shape of RBC's
biconcave and no nucleus or any organelles--> gives them more surface area for gas exchange
Hematopoiesis (Blood Cell Production)- Notes
1. Starts with stem cell hemocytoblast (stem cell)
2. Differentiates into early erythroblast → Produces ribosomes → Starts making hemoglobin
3. When enough hemoglobin is made → Nucleus discarded (some ribosomes remain and creates biconcave shape)
4. Reticulocyte → Leaves the bone marrow + enters the blood streams--> ribosomes left behind degrade whcih is now a erythrocyte!
5.Rbc travels around body doing its job for 4 months (120 days)
How are rbc replaced?
They are removed from circulation + destroyed by macrophages in the spleen, liver + bone marrow
- Then the recyclization begins by:
(1)Hemoglobin is broken down--> Globin + Heme
(2) Globin --> Amino Acids which are used in other proteins
(3) Iron is removed form heme+ is wither stored in liver or carried back to red bone marrow to be used in new heme
(4) the non -iron portion of heme is converted to bilirubin transported to the liver + released as bile
(5) Bile goes to intestine. Some is excreted in urine and some is converted to urobillnogen + excreted in the feces
What is hematopoiesis?
Process of producing gall blood cells
What is erythropoietin? Ero
Production of rbc
Rbc production and erythropoiesis (production of RBC) proceed at the same rate. - NOTE
- Regulated by hormone Erythropoiesis or EPO produced mostly by kidneys but also in liver + is constantly circulating in the blood
If HYPOXIA occurs them a negative feedback system kicks in to INCREASE RBC production.
Then stimulated kidneys to increase ERYTHROPIETIN realse speeding up production of RBC
* Hypoxia can have causes: anemia, bleeding, iron deficiency
What is a reticulocyte count? -NOTE
Is a test to measure the number of retics in the blood. It helps to assess how well bone marrow is producing new RBC
- In a clinic- abnormal level indicates anemia or bleeding where the body needs to produce more RBC faster (normal range .5-2.5%)
Which lab test measures the number and size of RBCs and WBCs?
- CBC (Complete Blood Count) → Measures number & size of RBCs, WBCs
What test assesses liver function by measuring ALT and AST levels?
- Blood Enzyme Test → Assesses changes in body function
-ALT & AST → Liver function
-Troponin & Creatine Kinase → Heart & skeletal muscle function
common lab test like Chem 20 Metabolic Panel test for?
Tests for glucose, creatinine, calcium, nitrogen, sodium
What is polycythemia vera?
A form of blood cancer leading to excessive RBC production.
- Hemocrit may be 65%
- Increased viscosity--> Harder to pump and may lead to INCREASE BP + stroke pump
- No cure
Name the normal hematocrit in males and females
male- 40-54%
female - 38- 46%
What are the causes of secondary polycythemia and what it is?
A rare disease involved by overproduction of RBC due to a number of reasons:
---->sleep apnea, obesity, COPD, dehydration, smoking
What are the dangers in increased blood volume, bp, and viscosity?
Cause a dangerous strain on heart, risk of embolism, stroke and heart failure
What is anemia and what is its three main categories?
Deficiency of RBC or hemoglobin
-Hemorrhagic anemia, Hemolytic anemia, and inadequate erythropoiesis
Inadequate erythropoiesis EPO is 1/3 anemias what does it do?
-Nutritional deficiency like (vit B2+c), Iron deficiency, renal deficiency,
- Pernicious anemia--> deficiency of intrinsic factory (no absorb vit B2)
- Hypo plastic + Aplastic --> destruction of myeloid tissue
Hemorrhagic is 2/3 anemia what does it do?
Hemophilia, bleeding , trauma, bleeding disorders
Hemolytic is 3/3 anemia what does it do ?
drug reactions--> penicillin aery
poisoning --> mushrooms, snakes, spiders
Parasite-->
-Hemoglobin defects--> sickle cell thalassemia
blood type incompativility--> Jemolytic diseas of newborn transfuction reactions
How does iron deficiency cause anemia?
1. Inadequate Erythropoiesis (EPO Deficiency) →pernicious anemia
2.Iron Deficiency
3. Nutritional Deficiencies → Lack of folic acid and essential vitamins
Pernicious Aneia - Not having or making enough ___________factor leads to inability to absorb ________
Intrinsic
vit b12
What is the primary cause of sickle cell anemia?
Caused by a genetic hemoglobin defect, leading to sickle-shaped RBCs.
Hydro plastic Anemia type of EPO what does it do ?
Erythropoiesis declines
Aplastic Anemia is a type of EPO what does it do?
-->Erythropoiesis stops all together
-blackening of the skin due to necrosis
Causes: Immune system dysfunction -->may be type of auto immune disorder
What is a characteristic symptom of aplastic anemia?
-Complete cessation of erythropoiesis.
-Leads to skin blackening due to necrosis.
-Most commonly caused by immune system disorders.
-Life expectancy: 1-5 years if untreated.
______________ Anemia - Hemoglobin defect
- mostly among people form Africa, middle east, India, Asia.
-Sickle cell
Sickle cell anemia- Hemoglobin defect
--> caused by ____________ ________ that causes RBC to have a sickle shape
-recessive gene
sickle cell anemia-notes
-caused by recessive gene that causes RBC to have a sickle shape
*Sickle cells are sticky + get caught in small blood vessel
* Very pain full can lead to kidney failure, heart failure, strokes, joint pain or paralysis
*Tissues don't get enough oxygen
* Anemia happens because sickled cells die sooner than regular RBC's
treatments of sickle cell anemia
Pain meds, blood transfusions, folic acid, new gene therapies+ bone marrow transfusions
--> Deadly PSSITIVE FEEDBACK loop Hypoxia--> trigger more sickling to occur
What is the universal blood donor type?
O negative
How does the Rh factor impact pregnancy?
- If Rh-+mother carries an Rh + positive baby, problems may arise in the second pregnancy.
-RH- mom develops antibodies to Rh+ baby when baby's blood cells cross the placenta + mix with mom's cells typical during delivery
* Moms immune system recognize the RH protein on baby's cells as foreign + produces antibodies against it
- First pregnancy: No major issues as maternal and fetal blood are separate.
- To prevent future problems with pregnancy Rhogam is given --> works by binding to any RH antibodies in moms system/ prevents agglutination of baby's blood.
- RhoGAM Injection: Given after the first birth to prevent antibody formation.
What determines a Persons's ABO blood type?
The hereditary presence or absence of antigens A and B on RBC
What injection is given to prevent hemolytic disease of the newborn?
RhoGAM Injection
Which type of WBC is most abundant and helps fight bacterial infections?
Neutrophils (60-70%)
-Phagocytize bacteria.
-Contain lysosomes.
What is the general function of leukocytes?
Retain their nucleus + organelles for protein synthesis
-Protect against infection
-Produce antibodies
-Promotes inflammation
-Regulates immune response
What are the two types of granules found in leukocytes?
Granulocytes and agranulocytes
What are the three types of granulocytes and their primary functions? N____________ 1/3
-Neutrophils: most common 60-70%
*go to site of infection --> phagocytize bacteria
- Granules contain lysozyme + other hydrolytic enzymes
What are the three types of granulocytes and their primary functions? E____________s 2/3
-2-4%
-secret chemical to destroy para sites
- phagocytize inflammatory chemicals, antigen-antibody complexes +allergens
What are the three types of granulocytes and their primary functions? Ba___________ 3/3
Basophils-1% of WBC
- secrete histamine (vasodilator) + heparin (anti-coagulant)
Wat are two types of agranulocytes?
Lymphocytes and Monocytes
What are the two types of agranulocytes and their primary functions? L___________ 1/2
Lymphocytes--> 3 cell types 25-33%
B cells
T cells
NK= Natural Killer cells
What are the two types of agranulocytes and their primary functions? M___________ 2/2
Monocytes-8%
- leave the blood stream + become macrophages in tissue
- Phagocytize pathogens + dead neutrophils
What are the three leukocyte disorders WBC's?
-Leukopenia
-Leukocytosis
-Leukemia
WBC disorder- Leukopenia
Low WBC count, below 5,000/uL caused by Radion, poisons + infectious disease
WBC disorder- Leukocytosis
High WBC count above 10,000/ml causes infection, allergy + disease
WBC disorder- Leukemia
Cancer of hemopoietic tissue usually producing increase of leukocytes
WBC leukemia
1) Myeloid leukemia- uncontrolled granulocyte production
2) Lymphoid leukemia- uncontrolled lymphocytes or monocyte production
3) Acute Leukemia- appears suddenly progress rapidly
4) Chronic Leukemia- undetected for months, survival time 3 years from diagnosis
1) myeloid leukemia
uncontrolled granulocyte production
2) Lymphoid leukemia
uncontrolled lymphocytes or monocyte production
3) Acute Leukemia
appears suddenly progress rapidly
4) Chronic Leukemia
undetected for months, survival time 3 years from diagnosis
Platelets-Notes
Involved in Hemostasis ---> the body natural process of stopping bleeding + repairing itself after an injury
- Doesn't happen without thrombocytes
thrombo--> means clotting cyte = cell
--but they arn't really a cell but actually a cell fragment --> more specifically a Megakaryocyte Cell Fragment
What is hemostasis and what formed element is involved?-slide
The cessation of bleeding involves platelets
What is a normal platelet count?
150-450k/ml
skipped the process of hemostasis
Look at notes
What keeps blood from clotting at any given time? (1/3)
(1) Nitric oxide+ prostaglandin (PGI)--> these both inactivate platelets
What keeps blood from clotting at any given time? (2/3)
(2) Heparin Sulfate --> this inactivates factor prothrombin II, IX, X
What keeps blood from clotting at any given time? (3/3)
(3)- Thrombomodulin binds thrombin which activates protein C--> degrades factor V,VIII
What are the 5 Mechanisms of clotting (Hemostasis)
1. Vascular spasm
2. Platelet plug formation
3. Coagulation
4. Clot retraction +repair
5.Fribrinolysis
Name 1/5 Mechanisms of clotting? Va__________ sp_______
(1) Vascular spasm- the most immediate protection from blood loss after injury occurs
- smooth muscle in vessel walls contract constricting the vessel redirecting blood flow
- Pain receptors are activated enhancing vasoconstriction
- Platelets release serotonin
Name 2/5 Mechanisms of clotting? Platelet Plug formation.
- Von Willebrand factor is secreted by injured cells
- Platelets bond with VWF secreted by injured cells
- Platelets stick to each other + to wound site.
-Platelet aggregation- positive feedback loop increase vasoconstriction
Name 3/5 Mechanisms of clotting? C_____________
Hint fastest way to stop bleeding!!
Coagulation - clotting cascade
- many clotting factors (made by liver) are in circulation but remain inactive until they circulate over a platelet plug
1) Factor XII is first one activated
2) XII activates XI --> activates IX--> activates VIII
*Factor IX + VIII need PF3 + Ca2+ to interact with one another
3) Prothrombin Activator --> converts prothrombin--> thrombin (Factor II)
4) Thrombin also reacts with fibrinogen to convert it to fibrin
***Thrombin also reacts with FACTOR XIII which allows fibrin strands to cross link forming mesh over platelet plug--> prevents clot from breaking away causing embolism
Name 4/5 Mechanisms of clotting? Clot____________+ Repair
Clot retraction + repair-
1) Platelets contraction --> platelets pull torn ends together
2) Platelets secrete growth factor (PDGF)
--> trigger mitosis in smooth muscles cells
--> produces connective tissue patches
3) also secrete vascular endothelial growth factor ( VEGF)--> Regenerates the endothelial lining.
Name 1/5 Mechanisms of clotting? F______________
Fibrinolysis - clot busting
1) Factor XII--> converts prekallikrein--> kallikrein-- coverts plasminogen to plasmin
* Plasmin degrades fibrin mesh.
-POSITIVE FEED BACK LOOP
What is Thrombocytopenia? CD
Clotting disorder that has to few platelets
- May cause blood vessels to leak, easy bruising, bleeding from germs or nose, enlarged spleen
Causes: Bone marrow disorder, leukemia, taking certain meds, idiopathic
What is THROMBOCYTOSIS?
Too many platelets
Cause: often time cancer (may be the 1st sign)
- Lung, ovarian, breast or gastrointestinal
What is THROMBOSIS?
Abnormal clotting
* Problematic with older age
* Embolism--> Piece of clot breaks away +travels to some other place --> blocks blood flow from that point on. (cerebral, coronary + pulmonary arteries)
What is HEMOPHILIA?
Sex linked genetic disorder
- Predominately affects males
* deficiency of factor VIII (classic) factor + Factor XI
What is VONWILLEBRANDS DISEASE? CD
Abnormally slow to clot-
* interferes with platelet aggregation
What is DISSEMINATED INTRAVASCULAR COAGULATION (DIC)
* Abnormal clots form inside vessel s using up clotting factors which leads to massive bleeding in other parts.
- Treatment may be blood thinners to keep blood from clotting. --> this may cause more bleeding
-Replacing platelets --> may cause clotting, using up clotting factors,
--> bleeding occurs elsewhere
--> viscous circle--> often times life threatening
Diagnostic test- D-dimer
Detects clotting disorder such as deep vein thrombosis (DVT) or pulmonary embolism (PE)
** D-dimer is a protein fragment that is released when blood clot breakdown
-marker for fibrinolysis
Diagnostic test- PT/PTT
Prothrombin time= measures the extrinsic system
** Partial thromboplastin = measure the intrinsic system --> how long it takes the blood to clot
Blood thinners- for heart disease or temporary after some surgeries
Antiplatelet--> aspirin make blood less viscous
Anticoagualnt drugs--> delay clot formation --> like Heparen
Aspirin inhibits __________. Prostacyclin is a _____________ re________--> they wont stick to ____________smooth vessels
-Prostacyclin
-platelet repellent
-healthy
What is the difference between acute and chronic leukemia?
-->Acute leukemia → Develops suddenly, progresses quickly, fatal within months.
-->Chronic leukemia → Develops slowly, can go undetected for months.
What are the two pathways of blood clotting?
Intrinsic Pathway → Activated by damage to the blood vessel itself.
Extrinsic Pathway → Activated by tissue damage outside the blood vessels.