Immunology Lec1
0.0(0)
Card Sorting
1/121
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
122 Terms
1
New cards
Immunology
study of a host’s reactions when foreign substances are introduced into the body.
2
New cards
antigens
A foreign substance that induces such an immune response is called _____________
3
New cards
immunity
the condition of being resistant to infection
4
New cards
1960s
It was not until the ______ that the cells responsible for the immune response were identified and characterized.
5
New cards
smallpox scab
The first written records of immunological experimentation date back to the 1500s, when the Chinese developed a practice of inhaling powder made from ________s in order to produce protection against this dreaded disease.
6
New cards
variolation
The prac tice of deliberately exposing an individual to material from smallpox lesions was known as ________
7
New cards
Edward Jenner
An English country doctor by the name of___________discovered a remarkable relationship between exposure to cowpox and immunity to smallpox.
8
New cards
vaccination
This procedure of injecting cellular material became known as ________
9
New cards
vacca
Vaccination came from the latin word _____ which means cow
10
New cards
cross-immunity.
\
The phenomenon in which exposure to one agent produces protection against another agent is known as ________.
The phenomenon in which exposure to one agent produces protection against another agent is known as ________.
11
New cards
Attenuation
may occur through heat, aging, or chemical means, and it remains the basis for many of the immunizations that are used today.
12
New cards
Louis Pasteur
In working with the bacteria that caused chicken cholera, _____________, a key figure in the development of both microbiology and immunology, accidentally found that old cultures would not cause disease in chickens
\
\
13
New cards
rabies
Pasteur applied the same principle of attenuation to the prevention of _________, a fatal disease at that time.
14
New cards
Elie Metchnikoff
a Russian scientist, observed that foreign objects introduced into transparent starfish larvae became surrounded by motile cells that attempted to destroy these invaders. He called this process phagocytosis.
15
New cards
Phagocytosis
Process by which cells eat cells.
16
New cards
Almoth Wright
In 1903, an English physician named ____________linked the two theories by showing that the immune response involved both cellular and humoral elements
17
New cards
opsonins
Wright observed that certain humoral, or circulating, factors called _____________acted to coat bacteria so that they became more susceptible to ingestion by phagocytic cells.
18
New cards
antibodies, acute-phase reactants
These serum factors include specific proteins known as _________and nonspecific factors called___________________ that increase nonspecifically in any infection.
19
New cards
Natural, or innate immunity
is the ability of the individual to resist infection by means of normally present body functions.
No prior exposure is required, and the response does not change with subsequent exposures.
No prior exposure is required, and the response does not change with subsequent exposures.
20
New cards
Acquired immunity
is a type of resistance that is characterized by specificity for each individual pathogen, or microbial agent, and the ability to remember a prior exposure, which results in an increased response upon repeated exposure.
21
New cards
External
_______defense system is designed to keep microorganisms from entering the body.
22
New cards
inflammation
The process of________ brings cells and humoral factors to the area in need of healing
23
New cards
external defense system
is composed of structural barriers that prevent most infectious agents from entering the body.
24
New cards
lactic acid in sweat and fatty acids from sebaceous glands
maintain the skin at a pH of approximately 5.6. This acid pH keeps most microorganisms from growing.
25
New cards
urine
he flushing action of ______, plus its slight acidity, helps to remove many potential pathogens from the genitourinary tract
26
New cards
Lysozyme
is an enzyme found in many secretions such as tears and saliva, and it attacks the cell walls of microorganisms, especially those that are gram-positive.
27
New cards
competitive exclusion
In many locations of the body, there is normal flora that often keeps pathogens from establishing themselves in these areas. This phenomenon is known as
28
New cards
Internal defense system
is designed to recognize molecules that are unique to infectious organ- isms.4 This typically involves recognizing a carbohydrate such as mannose that is found in microorganisms and is not evident on human cells.
29
New cards
Phagocytosis
This process destroys most of the foreign invaders that enter the body, and it is the most important function of the internal defense system.
30
New cards
acute-phase reactants
Phagocytosis is enhanced by soluble factors called __________________.
31
New cards
Acute-phase reactants
are normal serum constituents that increase rapidly by at least 25 percent due to infection, injury, or trauma to the tissues.5
32
New cards
hepatocytes
liver parenchymal cells
33
New cards
hepatocytes
Acute phase reactant are produced by _________.
34
New cards
12-24
Acute phase reactant are produced within _________.hours
35
New cards
cytokines
intercellular signaling polypeptides
36
New cards
IL-1β, IL-6, TNF-α
Most common cell messengers
37
New cards
monocytes and macrophages
IL-1β, IL-6, TNF-α are produced by ______at the sites of inflammation
38
New cards
C-reactive protein
is a trace constituent of serum originally thought to be an antibody to the c-polysaccharide of pneumococci. It increases rapidly within 4 to 6 hours following infection, surgery, or other trauma to the body.
39
New cards
19 hours
Plasma half-life of C-Reactive Protein
40
New cards
age
C-Reactive Protein is directly proportional to ___
41
New cards
118,000 daltons
C-reactive protein is a homogeneous molecule with a molecular weight of _____________ and a structure that consists of five identical subunits held together by noncovalent bonds.
42
New cards
C-Reactive proteins
acts somewhat like an antibody, as it is capable of opsonization (the coating of foreign particles), agglutination, precipitation, and activation of complement by the classical pathway.
43
New cards
phosphocholine
common constituent of microbial membranes.
44
New cards
phosphocholine
main substrate of CRP
45
New cards
CRP
an be thought of as a primitive, nonspecific form of antibody molecule that is able to act as a defense against microorganisms or foreign cells until specific antibodies can be produced.
46
New cards
CRP
The most widely used indicator of acute inflammation
47
New cards
1\.5 mg/L for men to 2.5 mg/L for women
Normal levels CRP for men and women, respectively
48
New cards
Serum amyloid A
It is an apolipoprotein that is synthesized in the liver and has a molecular weight of 11,685 daltons
49
New cards
30ug/ml
Normal circulating levels are approximately of Serum Amyloid A is
50
New cards
serum amyloid A
By removing cholesterol from cholesterol-filled macrophages at the site of tissue injury, _________contributes to the cleaning up of the area.
51
New cards
Alpha1-Antitrypsin
general plasma inhibitor of proteases released from leukocytes, especially elastase.
52
New cards
Elastase
Is an endogenous enzyme that can degrade elastin and collagen.
53
New cards
alpha1-antitrypsin
acts to “mop up” or counteract the effects of neutrophil invasion during an inflammatory response.
It also regulates expression of proinflammatory cytokines such as tumor necrosis factor-alpha, interleukin-1�, and interleukin-6, mentioned previously.
It also regulates expression of proinflammatory cytokines such as tumor necrosis factor-alpha, interleukin-1�, and interleukin-6, mentioned previously.
54
New cards
premature emphysema
Alpha1-antitrypsin deficiency can result in ___________-
55
New cards
Homozygous inheritance of this most severe variant gene may lead to development of cirrhosis, hepatitis, or hepatoma in early childhood.6
56
New cards
Fibrinogen
is the most abundant of the coagulation factors in plasma, and it forms the fibrin clot.
57
New cards
100 to 400 mg/dL
Normal levels of fibrinogen
58
New cards
340,000
Fibrinogen, is a molecule , is a dimer with a molecular weight of _______ daltons
59
New cards
thrombin
A small portion of fibrinogen is cleaved by________ to form fibrils that make up a fibrin clot.
60
New cards
Haptoglobin
is an alpha2-globulin with a molecular weight of 100,000 daltons. Its primary function is to bind irreversibly to free hemoglobin released by intravascular hemolysis.
61
New cards
de novo synthesis
The rise in plasma haptoglobin is due to__________ by the liver and does not represent release of previously formed haptoglobin from other sites
62
New cards
40 to 290 mg/dL
Normal plasma concentrations range from ___________________
63
New cards
Haptoglobin
____________ plays an important role in protecting the kidney from damage and in preventing the loss of iron by urinary excretion
64
New cards
free hemoglobin
a powerful oxidizing agent that can generate peroxides and hydroxyl radicals
65
New cards
Ceruloplasmin
consists of a single polypeptide chain with a molecular weight of 132,000 daltons.6 It is the principal copper-transporting protein in human plasma, binding 90 to 95 percent of the copper found in plasma by attach- ing six cupric ions per molecule.
66
New cards
Wilson’s disease
A depletion of ceruloplasmin is found in _________, an autosomal recessive genetic disorder characterized by a massive increase of copper in the tissues.
\
\
67
New cards
Complement
refers to a series of serum proteins that are normally present and whose overall function is mediation
68
New cards
Mannose-Binding Protein
is a trimer that acts as an opsonin, which is calcium-dependent. It is able to recognize foreign carbohydrates such as mannose and several other sugars found primarily on bacteria, some yeasts, viruses, and several parasites.
69
New cards
granulocytes
Neutrophils, eosinophils, and basophils are considered _________.
70
New cards
Neutrophil
represents approximately 50 to 70 percent of the total peripheral white blood cells.
71
New cards
Neutrophils
These are around 10 to 15 µm in diameter, with a nucleus that has between two and five lobes They contain a large number of neutral staining granules, which are classified as primary, secondary, and tertiary granules.
72
New cards
azurophilic granules
Primary granules, also called _______________, contain enzymes such as myeloperoxidase; elastase; proteinase 3; lysozyme; cathepsin G; and defensins, small proteins that have antibacterial activity.2
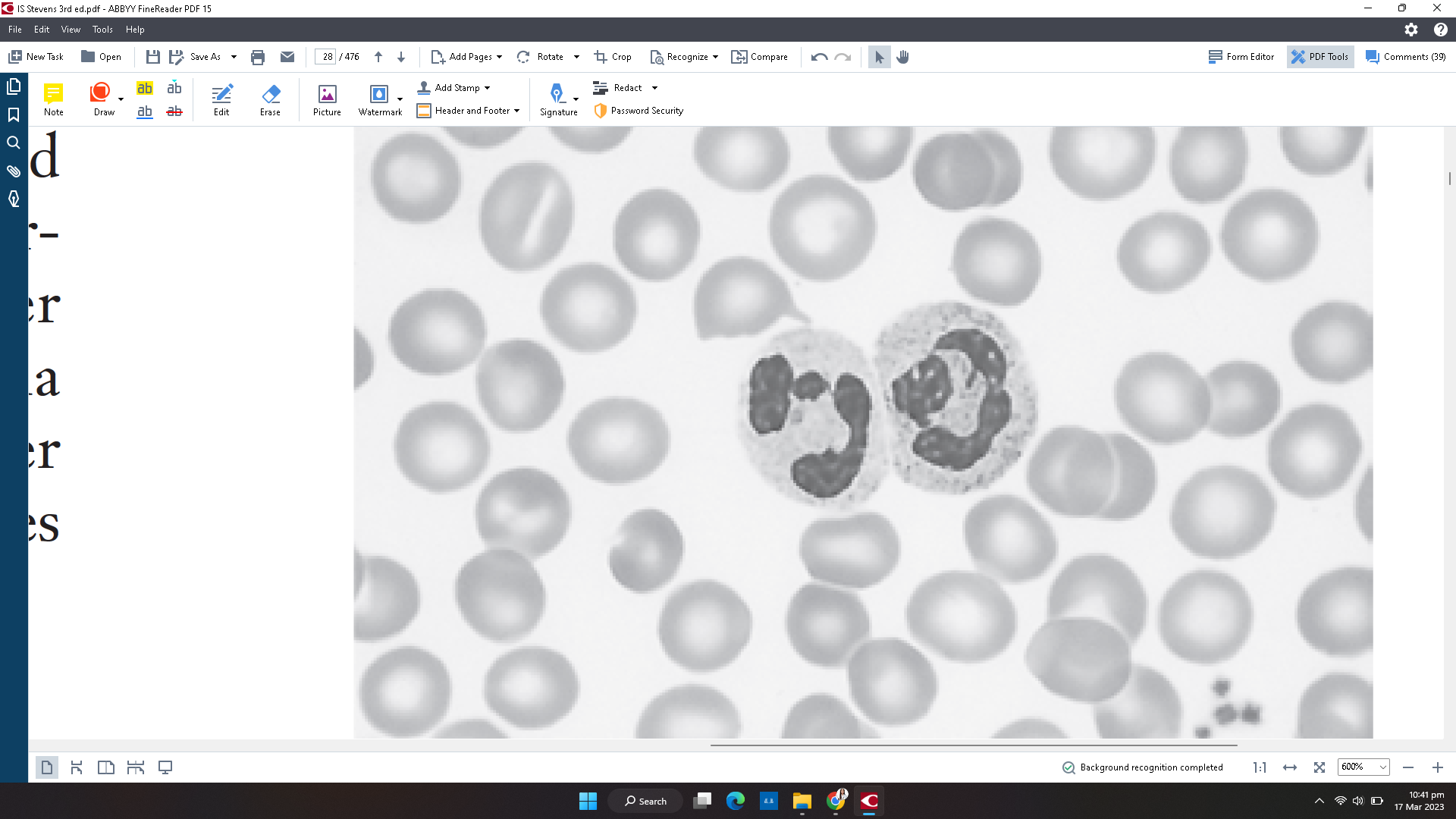
73
New cards
Secondary granules
are characterized by the presence of collagenase, lactoferrin, lysozyme, reduced nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, and other membrane proteins normally associated with the plasma membrane.
74
New cards
lysosomes
Acid hydrolases are found in separate compartments called
75
New cards
diapedesis
Marginating occurs to allow neutrophils to move from the circulating blood to the tissues through a process known as ___________, or movement through blood vessel walls.
76
New cards
selectins
Receptors known as selectins help make neutrophils sticky and enhance adherence to______________ that make up the vessel wall.
77
New cards
Chemotaxins
are chemical messengers that cause cells to migrate in a particular direction.
78
New cards
5
Once in the tissues, neutrophils have a life span of about __days
79
New cards
Eosinophil
are approximately 12 to 15 µm in diameter, and they normally make up between 1 and 3 percent of the circulating white blood cells in a nonallergic person. Their number increases in an allergic reaction or in response to many parasitic infections.
80
New cards
Eosinophil
The nucleus is usually bilobed or ellipsoidal and is often eccentrically located
81
New cards
eosinophil
Their most important role is neutralizing basophil and mast cell products and killing certain parasites
82
New cards
Basophils
are found in very small numbers, representing less than 1 percent of all circulating white blood cells. The smallest of the granulocytes, they are between 10 to 15 µm in diameter and contain coarse, densely staining deep-bluish- purple granules that often obscure the nucleus
83
New cards
Basophils
Constituents of these granules are histamine, a small amount of heparin, and eosinophil chemotactic factor-A, all of which have an important function in inducing and maintaining immediate hypersensitivity reactions
84
New cards
Histamine
Is a vasoactive amine that contracts smooth muscle
85
New cards
Tissue mast cells
___________ resemble basophils, but they are connective tissue cells of mesenchymal origin. They are widely distributed throughout the body and are larger than basophils, with a small round nucleus and more granules
86
New cards
9 to 18 months
Lifespan of mast cells
87
New cards
enzyme content
How can you distinguish basophils from mast cells?
88
New cards
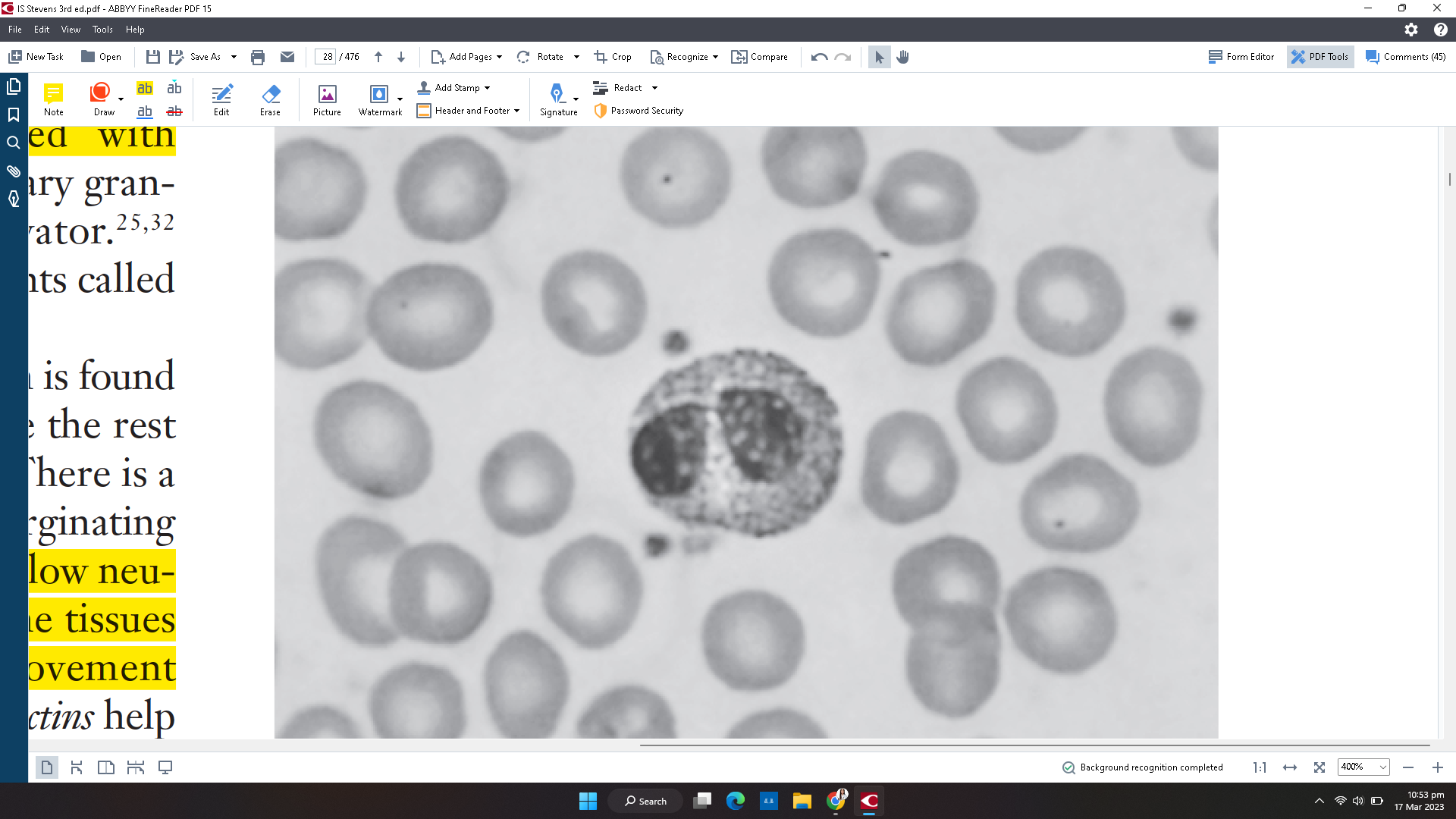
IgE
the immunoglobulin formed in allergic reactions
89
New cards
Monocyte
are the largest cells in the peripheral blood, with a diameter that can vary from 12 to 22 µm; they have an average size of 18 µm
90
New cards
horse-shoe shaped nucleus
What is the distinguishing feature of monocyte?
91
New cards
Monocyte
The abundant cytoplasm stains a dull grayish blue and has a ground-glass appearance due to the presence of fine dustlike granules.
92
New cards
70
Monocyte stays in peripheral blood for __ hours
93
New cards
macrophages
Monocyte stays in peripheral blood for hours and then migrate to the tissues and become knows as _________
94
New cards
monocyte
Macrophage precursor
95
New cards
alveolar macrophages
Macrophages in the lung are
96
New cards
Kupffer cells
Macrophages in the liver
97
New cards
microglial cells
Macrophages in the brain
98
New cards
histiocytes
Macrophages in the connective tissue
99
New cards
cytokines
Killing activity is enhanced when macrophages become “activated” by con- tact with microorganisms or with chemical messengers called ______, which are released by T lymphocytes during the immune response.
100
New cards
Dendritic
____________cells are so named because they are covered with long membranous extensions that make them resemble nerve cell dendrites.