MAIN Review NURS 2450 Exam 2 (Nylas)
1/341
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
342 Terms
What is MS?
- a chronic, progressive, degenerative disorder of the CNS
- onset 20-50 years of age
- women 2-3x more than men
- 5x more prevalent in temperate climates (northern US, Canada, Europe)
- average life expectancy 25-30 years from diagnosis (7-year difference from someone w/o MS)
Describe the physiological process in MS.
3 pathological processes:
- chronic inflammation
- demyelination
- gliosis in the CNS
- autoimmune process orchestrated by activated T cells
- onset: insidious, vague Sx, and intermittent
What are the etiologies of MS?
- unknown, but unlikely that there is just one cause
- geographical and genetic factors
- genetic predisposition w/ infectious and immunologic factors
What are some triggering factors of MS and why?
infection, smoking, emotional stress, physical injury, excessive fatigue, pregnancy, poorer state of health
What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: motor
- motor: weakness/paralysis of limbs/trunk/head, diplopia, scanning speech, muscle spasticity (interferes w/ speech, gait)
What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: sensory
- numbness
- tingling
- blurred vision
- vertigo
- tinnitus
- decreased hearing
- chronic neuropathic pain
- Lhermitte's sign
- patchy blindness
- pain in thoracic/abdominal regions
Lhermitte's sign
transient sx described as electrical shock radiating down spine to limbs; can occur w/ neck flexion
What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: cerebellar
- nystagmus
- ataxia (gait instability)
- dysarthria
- dysphagia
What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: fatigue
usually assoc. w/ increased energy needs (heat, humidity)
What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: bowel and bladder
- constipation (insufficient fluid, decreased activity, slow motility)
- spastic bladder (most common; small capacity for urine)
- flaccid bladder (large capacity for urine, but no sensation/pain/desire to void)

What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: sexual dysfunction
- ED r/t spinal cord dysfunction
- decreased libido
- decreased vaginal lubrication
- painful intercourse
What are the clinical manifestations of MS and how might they affect function? How does this vary for patients of different ages and developmental stages?: emotional changes
- depression
- anger
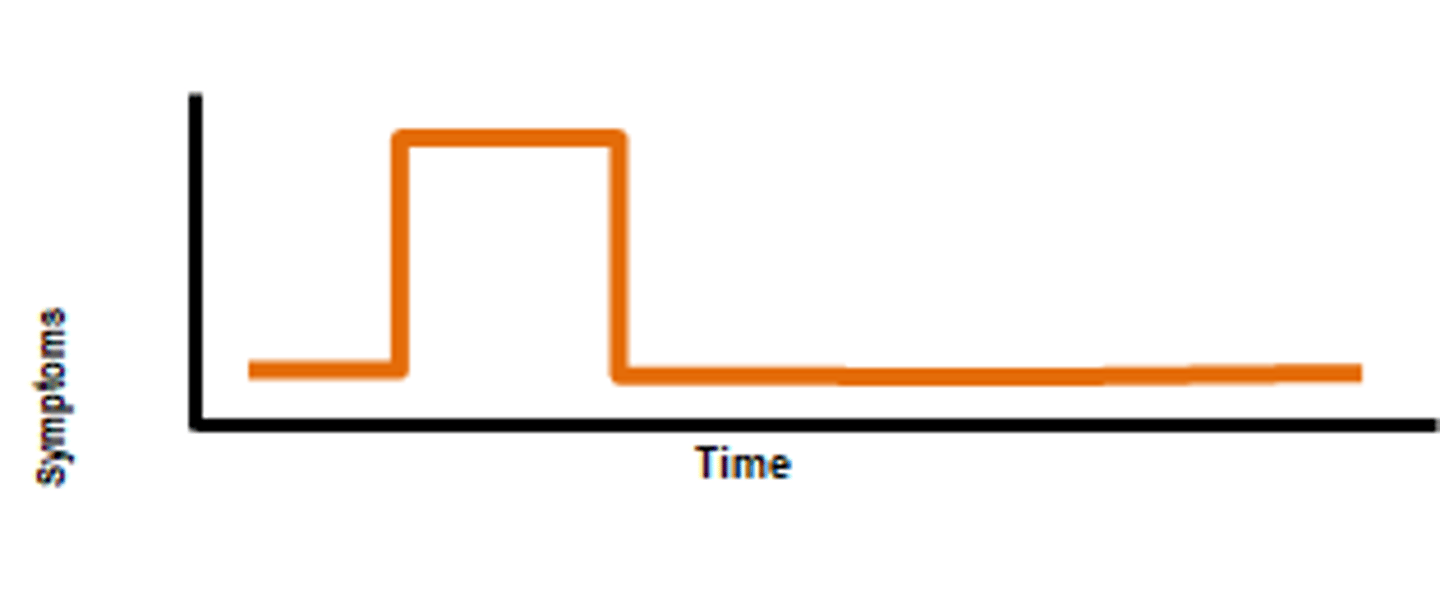
Describe the clinical courses of MS: relapsing-remitting
clearly defined relapses w/ a full recovery or slight residual deficit upon recovery; 85-90% initial dx; minimal disease progression
Describe the clinical courses of MS: primary-progressive
accumulation of disability from disease onset (slowly worsening neuro function from beginning, but no distinct relapse or recovery); 10%
Describe the clinical courses of MS: secondary-progressive
initially relapsing-remitting, then progression w/ or w/o relapse; 50% w/ relapse-remitting develop this after 10 years
What are some potential causes of pseudo-exacerbation of MS?
stress, fatigue, illness, heat
- does not cause new damage, is very distressing to patients, must treat underlying cause
How is MS diagnosed?
- no definitive diagnostic test
- diagnosis of exclusion: based on hx, clinical manifestations, imaging studies (MRI, CSF analysis, evoked potentials - simple sensory, visual, brain stem auditory; 50-90% have abnormal visual responses)
- McDonald's criteria: 1) lesions in 2 different locations 2) damage/attack interval 3) rule out other conditions
clinically isolated syndrome (CIS)
- first clinical episode that is suggestive of MS
- pt reported corresponding sx, objective findings that reflect demyelination
- develops acutely or sub-acutely w/ duration of at least 24 hrs
- w/ or w/o recovery
- would occur in absence of fever or infection
- resembles typical MS relapse
- no evidence of previous demyelination in PMH
What are common symptom and disease management strategies for MS?: goals and interdisciplinary management
- goals: neuromuscular function, maintain independence, fatigue management, psychosocial wellbeing, adjust to the illness, decrease factors that precipitate exacerbations (ex. heat)
- interdisciplinary management: pharmacological therapy seeks to slow progression, provide symptomatic relief, tailored to disease pattern; promoting function through rehabilitation, providing emotional support, complementary and alternative medicine (aerobic exercises)
What are common symptom and disease management strategies for MS?: disease modifying therapy (DMT)
Injection, PO, IV; goals: decrease relapse rate, slow accumulation of brain lesions on MRI; will not heal scarring, may not improve current functioning, may have some effect on progression, consideration of side effects
What are common symptom and disease management strategies for MS?: adjunctive pharmacologic therapy
o Acute exacerbations: glucocorticoids (methylprednisolone, prednisone; at site of inflammation), plasma exchange
o Anticholinergics: bladder sx
o CNS stimulants: fatigue
o Muscle relaxants: spasticity (also Botox)
o Nerve conduction enhancer: improve walking speed (selective K+ channel blocker); caution w/ seizure disorder and CKD
o Tricyclic antidepressants, AEDs: chronic pain syndromes
o Antispasmodic (baclofen)
How might the nurse prioritize care of a patient with MS?
- Nursing assessment: subjective: PMH (viral infections, geographic location), medications, functional health patterns (malaise, weight loss, difficulty chewing, numbness); objective: integumentary, neurological, musculoskeletal, diagnostic findings
- nursing diagnoses: impaired physical mobility, impaired urinary elimination, interrupted family processes, risk for falls, risk for infection
- nursing management: trigger identification, support, patient education; good balance of exercise and rest, nutrition, tx regimen, self-cath, adequate fiber intake, emotional adjustments, lifestyle changes
What is ALS?
amyotrophic lateral sclerosis (Lou Gehrig's disease)
- rare and progressive disorder characterized by loss of motor neurons (degenerate, then unable to send impulses to muscle fibers)
- sporadic (90-95% of cases) or familial (dominant inheritance; 50% pass it on)
- onset at 40-70 years
- men 2x more than women
Describe the pathophysiological process of ALS.
- unknown patho
- gradual degeneration of motor neurons
- sensation and cognition are not affected
What are some potential causes of ALS?
- thought to be gene mutations, elevated glutamate levels, autoimmune
What are the clinical manifestations of ALS? Differentiate between upper and lower motor neuron clinical manifestations.
- typical: muscle weakness, dysarthria, dysphagia, upper vs lower motor neuron
- other: pain, sleep disorders, spasticity, drooling, emotional lability, depression, esophageal reflux, constipation
- sequelae: muscle wasting, fasciculations
- UMN (transmit info from brain to SC) Sx: loss of dexterity/ability to coordinate, weakness, spasticity, hyperreflexia (affect movement rather than muscle itself)
- LMN (no signals arriving at muscle) Sx: weakness, paralysis, hyporeflexia, fasciculations (twitching), flaccidity, muscle cramps
- involuntary muscles affected: heart, GI tract, bladder (indirect r/t immobility)
How is ALS diagnosed?
- difficult to dx; thorough neuro exam is key; dx of exclusion
- electrodiagnostic test, blood and urine studies, x-rays, spinal tap, MRI, myelogram of cervical spine, muscle/nerve biopsy
- El Escorial criteria
What are common symptom and disease management strategies for ALS?
- prognosis: no cure, death occurs secondary to respiratory tract infection 2-6 years post-dx (hospice vs ventilator)
- interdisciplinary management: PT, OT, speech and swallow evaluation, neuro, pharmacological, nursing
-pharmacological: not curative; Riluzole (Rilutek): inhibits glutamate, slows progression of disease; Edaravone (Radicava): neuroprotective agent, prevents oxidative stress damage, slows functional deterioration
Overall care of an individual with neuromuscular disease
Nursing interventions
- facilitating communication: slow down and over-articulate, limit distractions, sit face-to-face in well-lit room, yes/no systems
- aspiration precautions: appropriate food consistency (honey), coughing and deep breath exercises, secretion management (coughalator, chest physiotherapy), IS, suctioning
- early ID of respiratory insufficiency, pain management
- falls precautions: bed alarm, bed in lowest position, lifts, wheelchair safety, promote safety mobility
- nutritional needs: small bites, eat slowly, positioning after eating, small frequent meals, high fiber, hydration, G tube, PN as disease progresses
- diversional activities
What are some nursing concerns related to care of an individual with impaired mobility? How might the nursing assessment, management, and evaluation be individualized for patients of different ages and developmental stages?
aspiration, falls precautions, nutritional needs
Which interprofessional team members are helpful in the care of an individual with neuromuscular disease and how might these individuals all work together?
PT, OT, neuro
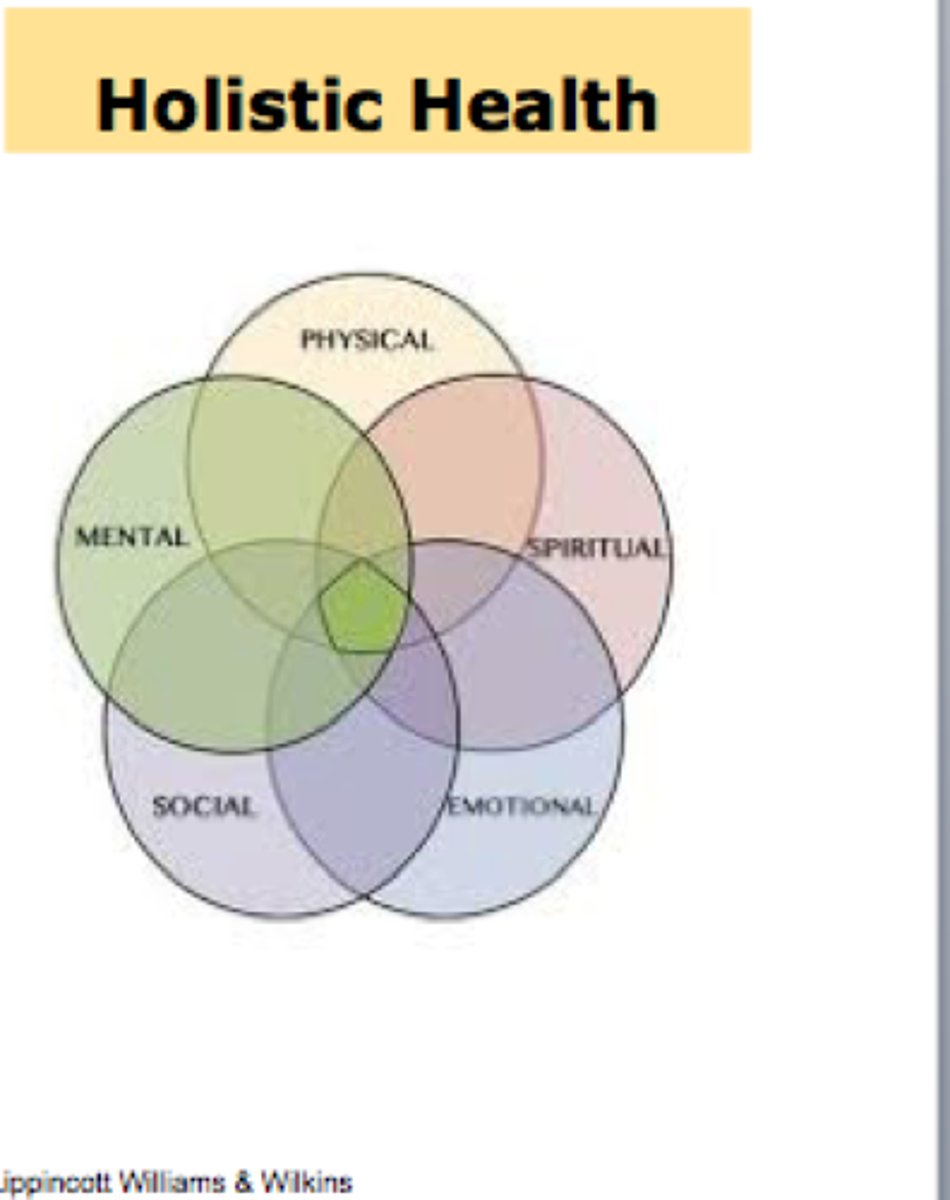
What does holistic care mean and how is it achieved?
the provision of care to patients that are based on a mutual understanding of their physical, psychological, emotional, and spiritual dimensions
How is adaptation and maximizing function best achieved in all settings, including but not limited to home, hospital, assisted living, and long-term care?
COME BACK TO THIS
What are the different types of Lupus? How would you differentiate between each type?
- systemic lupus erythematosus (SLE)
- cutaneous lupus: only affects skin (rashes, photosensitivity)
- drug-induced lupus: mimics S/Sx of SLE but no organ involvement; commonly caused by hydralazine and procainamide, takes months/years to develop; S/Sx disappear within months of stopping med
- neonatal lupus: rare but present at birth, Abs passed from mother to baby; NOT the infant form of SLE; generally a skin rash is present, sometimes heart block
What is Systemic Lupus Erythematosus (SLE)?
an autoimmune disease that occurs when your body's immune system attacks your own tissues and organs
Describe the pathophysiology of SLE.
- in healthy immune system, B and T cells work to attack Ags both directly and concurrently
- in SLE, autoreactive B and T cells are produced (autoantibodies); type III hypersensitivity response
- tissue damage occurs secondary to Ag-Ab complexes
- reactions can be local or systemic
What is the etiology of SLE?
exact cause unknown
What are some risk factors of SLE?
- genetics
- hormones (estrogen)
- environmental: sun/UV exposure, stress, viruses, chemicals/toxins (pesticides, asbestos), medications (Bactrim can cause photosensitivity)
What are some clinical manifestations of SLE?: General
- fever, weight loss, joint pain, excessive fatigue; generally experienced on daily basis, but also w/ exacerbations (flares)
- most commonly involved tissues: skin and muscle, lining of lungs, heart, nervous system, kidneys
What are some clinical manifestations of SLE?: dermatologic
- malar/"butterfly" rash
- alopecia (hair loss w/o scalp lesions)
- mouth ulcers (folic acid helps)
- photosensitive rashes (use zinc oxide; protects against UVA and UVB)
What are some clinical manifestations of SLE?: musckuloskeletal
- arthritis (swelling, pain, stiffness, deformity, subluxation)
-> ulnar deviation
-> swan neck of fingers (flexion of outermost joint)
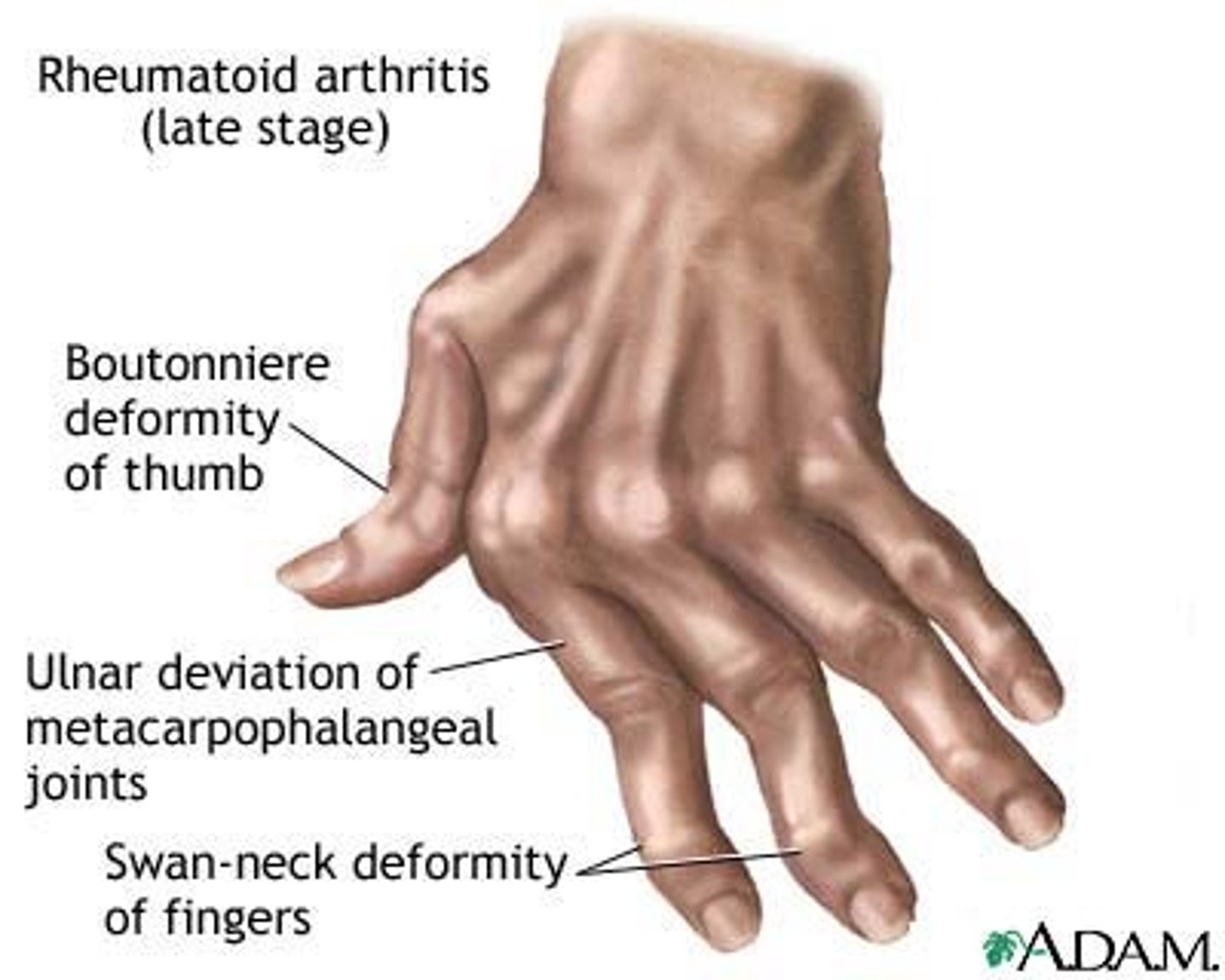
sublaxation
partial dislocation of a joint
What are some clinical manifestations of SLE?: pulmonary
pleurisy
What are some clinical manifestations of SLE?: cardiac
- pericarditis
- myocarditis
- endocarditis
- fibrosis of SA (bradycardia) and AV (heartblock) nodes
- antiphospholipid syndrome
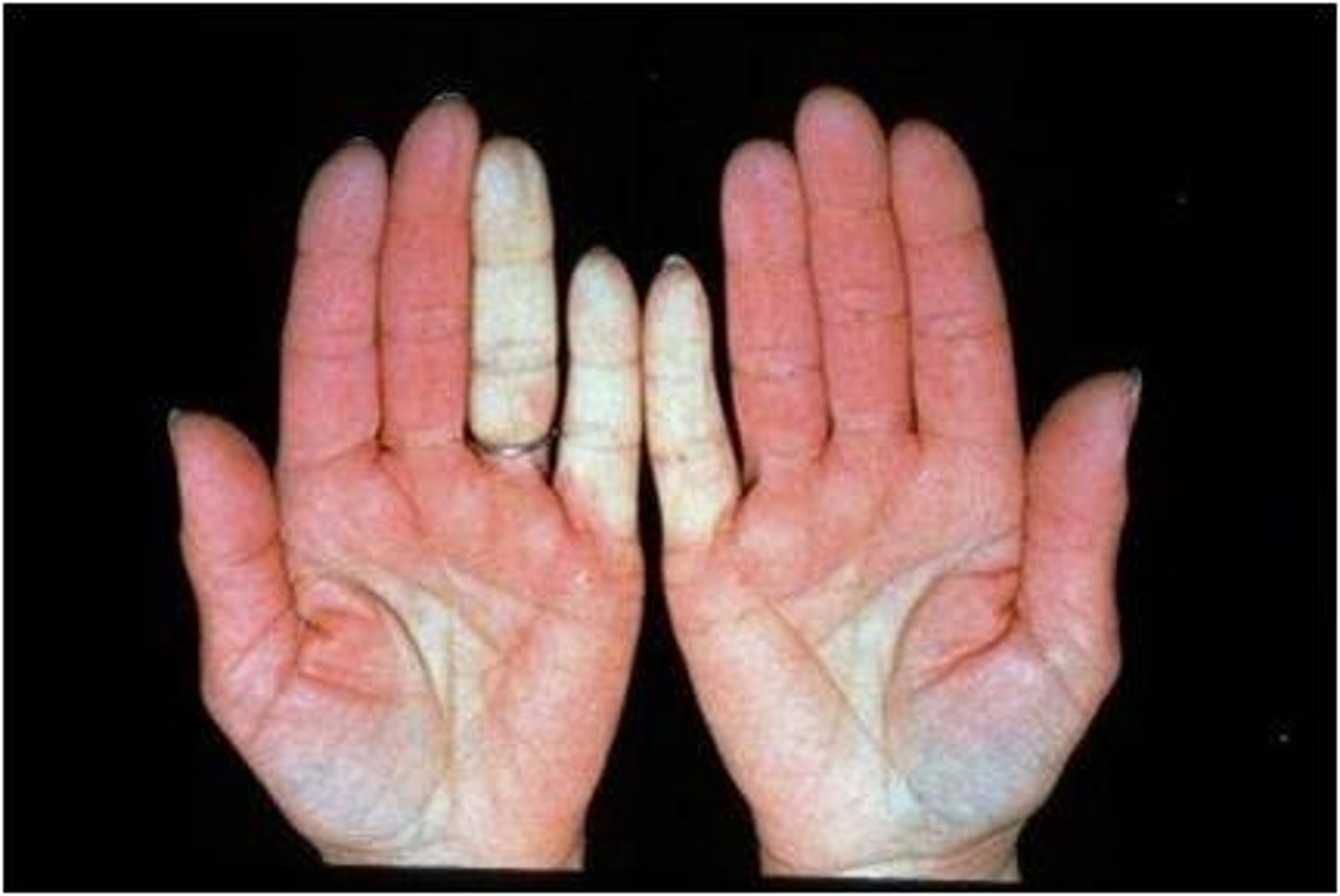
- Raynaud's phenomenon
irregular rhythm caused by fibrosis of pacemaker thus dysfunction of SA node can cause
bradycardia
fibrosis in AV node can lead to
heartblock
Antiphospholipid syndrome
proteins in blood are attacked, leading to blood clots in arteries, veins, organs
Raynaud's phenomenon
- fingers, toes, ears, tip of nose affected when blood vessels spasm and block blood flow
- appear white, blue, red
- triggered by: cold temps, anxiety, and stress
What are some clinical manifestations of SLE?: renal
- 40-50% experience this
- mild proteinuria (left alone if mild, if severe warrants a kidney biopsy)
- glomerulonephritis (autoantibodies go after glomerulus and cause fibrosis, tubular damage,, interstitial inflammation.)
s/sx:
- decreased urine production
- hematuria
- proteinuria
- face puffiness
What are some clinical manifestations of SLE?: nervous system
- seizures
- headaches
- peripheral neuropathy
- cognitive problems (disordered thinking, disorientation, memory deficits)
- depression
- anxiety (may be related to stress of having chronic illness, rather than actual disease)
What are some clinical manifestations of SLE?: hematologic
- anemia
- leukopenia
- thrombocytopenia- coagulation disorders
What is a lupus flare?
common sx:
- pain (joint, muscle, chest (upon a deep inspiration)
- headaches
- rashes (butterfly rash on face)
- fever
- alopecia
- mouth sores
- constant fatigue
- SOB/dyspnea
- swollen glands
- swelling in arms, legs, or face
- confusion
- blood clots

List some triggers that cause lupus flares.
stress, temperature changes, infections, sun exposure
How is SLE diagnosed? What lab and diagnostic tests are used?
look for the presence of autoantibodies:
- antinuclear antibody (ANA)
- anti-double stranded DNA (anti-DSDNA)
- anti-smith Ab
- antiphospholipid Abs
- x-ray, ECG if CV involvement suspected
- SLE diagnostic criteria: confirmed if score of 10 or greater
What is glomerulonephritis or lupus nephritis?
tubular damage caused by interstitial inflammation/fibrosis; leads to decreased urine production, hematuria, proteinuria
- can cause intravascular volume expansion, edema, and systemic HTN
List potential complications that are associated with SLE.
- infections
- end-stage renal disease
- stroke (interruption of blood supply to brain d/t antiphospholipid syndrome or htn)
- heart attack (50x greater risk in ages 35-44 d/t CVD
- atherosclerosis, etc.)
- pregnancy complications
- skin scarring (discoloration d/t sun and rashes)
Why do complications occur during pregnancy?
immunocomplexes deposited in placenta can cause spontaneous abortions, stillbirth, intrauterine growth restriction; disease should be inactive for at least 6 months prior to pregnancy
Describe the interprofessional care involved in SLE.
drug therapy, nutrition, exercise (goal is to prevent damage to inflamed joints/muscles while maintaining muscle strength; low-impact activities such as walking, swimming, yoga, pilates, cycling)
What dietary considerations should be included in patient teaching for someone with SLE?
- no special diet
- mild-moderate alcohol use
- monitor fat and salt intake ( espeacially in the presence of hypertension or if recieveing corticosteroids treatment)
- calcium intake to offset corticosteroids (since they can cause/worse osteoporosis)
- avoid alfalfa and garlic (associated w/ lupus-like flares; muscle pains, etc)
exercises for SLE
low impact!!
- walking
- swimming
- yoga
- pilates
- cycling
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: NSAIDS
function: reduces inflammation
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: antimalarial agents
- hydroxychloroquine
- chloroquine
- decrease Ab production
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: corticosteroids
treat inflammation
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: steroid-sparing medications/immunosuppressants
- methotrexate
- suppress immune system
- control inflammation
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: anticoagulants
- monoclonoal antibodies
- increase blood clotting time
- route: IV or SQ
- inhibit B cells
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: respiratory corticotropin injection
- acthar
- used after others have failed
- believed that it triggers cortisol production which helps reduce inflammation
Discuss the pharmacologic treatment used in SLE. What class of medications are used and how do they work?: for chronic pain management
- opioids
- medical marijuana/CBD oil
- vitamin D (high prevalence of insufficiency in SLE population; but limited evidence that this is clinically beneficial for those with fatigue)
List the overall goals of nursing management.
- pain mgmt
- patient education
- maintain optimal role function
- positive self-image
What nursing interventions would you consider and why?
(an online list to consider)
1. Improving Skin Integrity
2. Managing Acute Pain and Providing Relief and Comfort
3. Decreasing Fatigue
4. Initiating Patient Education and Health Teachings
5. Administer Medications and Provide Pharmacologic Support
6. Monitoring Results of Diagnostic and Laboratory Procedures
7. Assessing and Monitoring for Potential Complications
What is the leading cause of death in individuals 5 - 34 years of age?
motor vehicle crashes
What are some examples of primary prevention in trauma?
- seatbelts are the most effective way to reduce injury in MVC (50%)
- helmets prevent 37% of fatal motorcycle injuries
Why is early intervention key in the care of a trauma patient?
- the golden hour: the first hour after injury will largely determine a critically injured person's chances for survival
- platinum 10 minutes: no more than 10 minutes of on-scene stabilization prior to initiation of transport -> "scoop and run" approach encourages rapid transport to the local trauma center BUT life-saving interventions should not be delayed
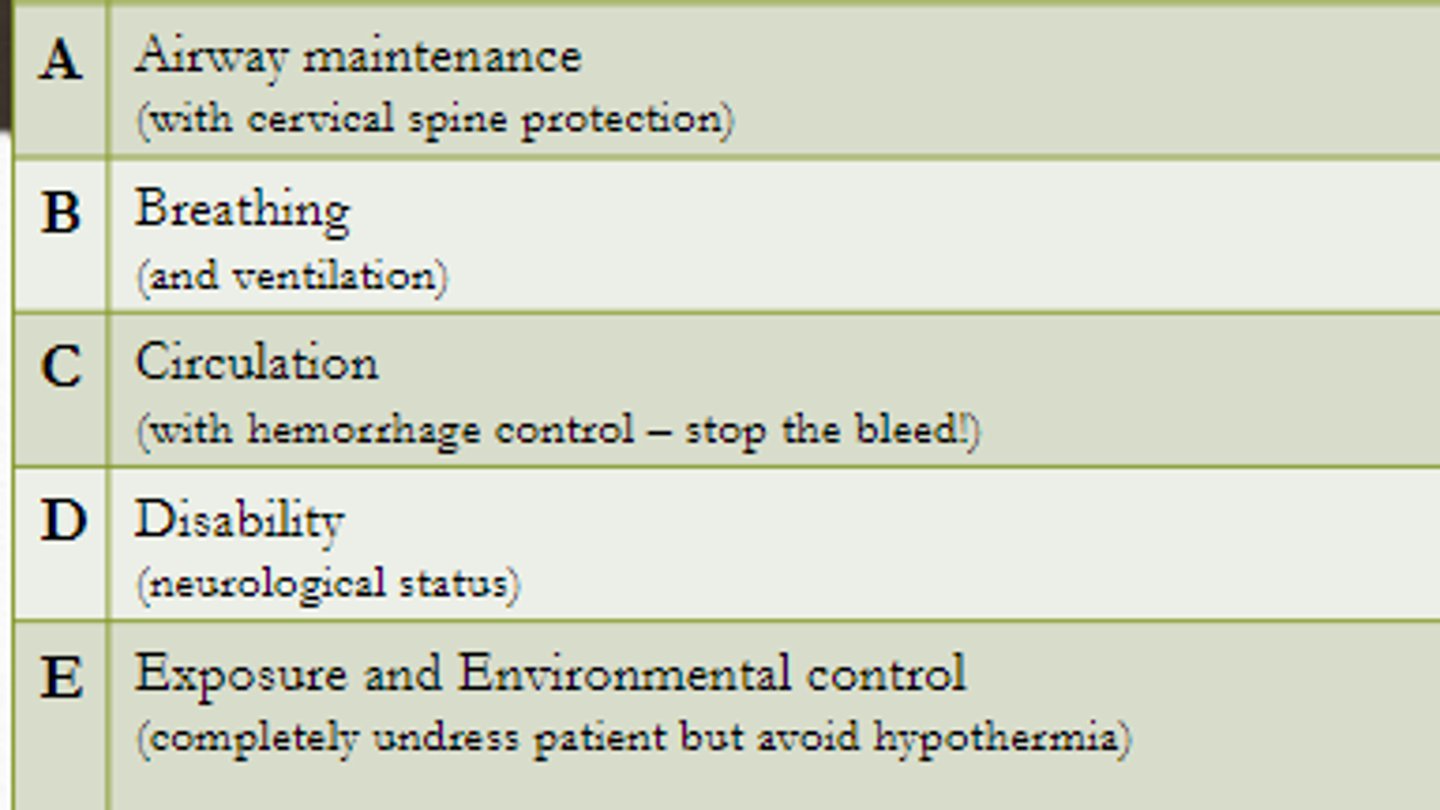
Describe the steps in the trauma primary survey.
ABC (w/ hemorrhage control)
D (disability; neuro status)
E (exposure and environmental control; completely undress patient to ensure no injuries are missed, avoid hypothermia)
What is the role of the nurse in the trauma bay during the primary survey?
COME BACK TO THIS
Trauma nurses need to be able to start IVs, draw blood, place urinary catheters, place patients on cardiac monitoring, set up breathing treatments for patients and hook patients up to monitors. They also need to be able to recognize subtle changes in patient condition and react accordingly.
(study.com)
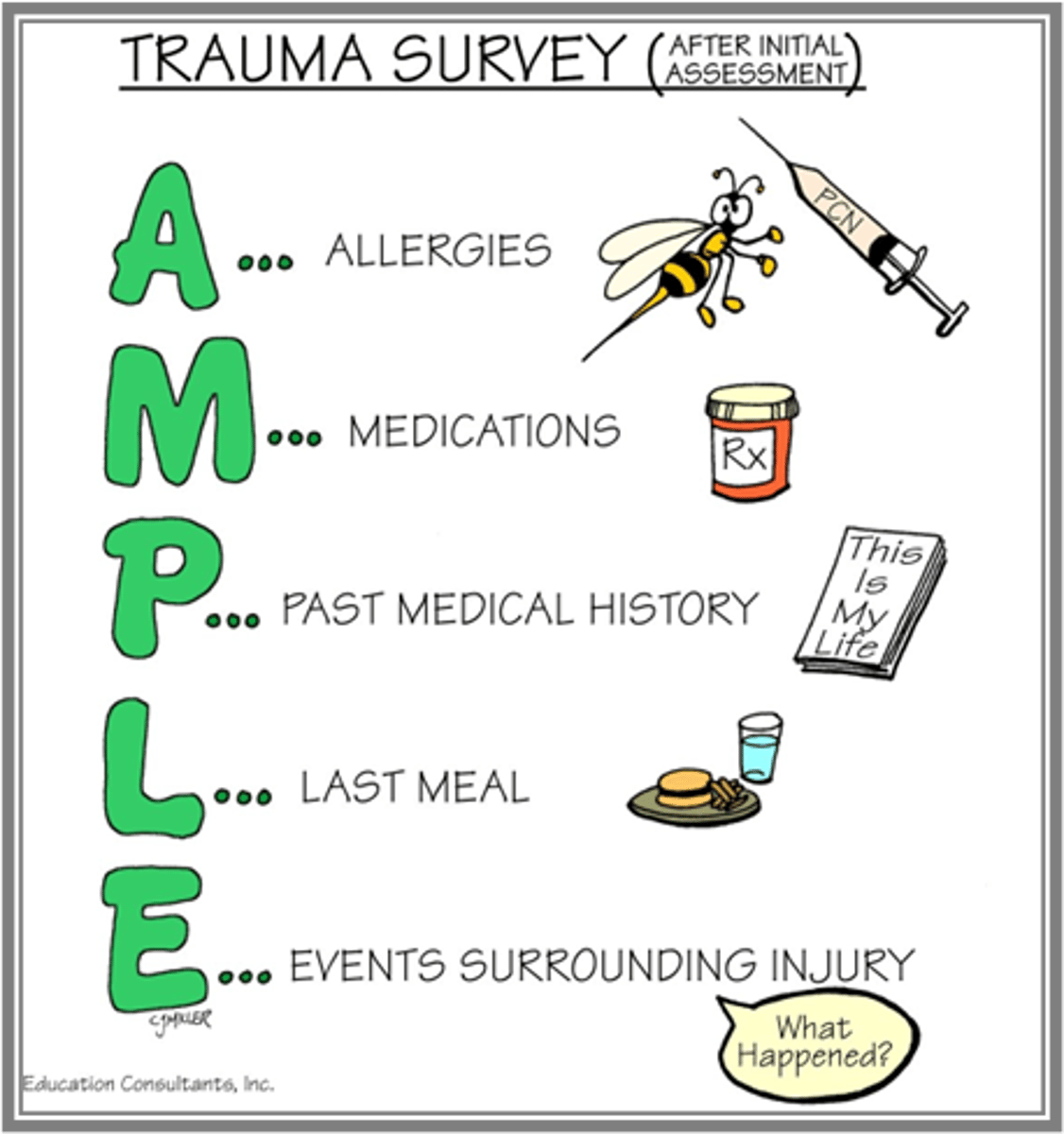
Describe the trauma secondary survey.
Allergies
Medications
PMH
Last meal
Events surrounding injury
- for quick focused history
- perform in series and in parallel w/ primary survey
What is the role of the nurse during the secondary survey?
attempts to obtain pertinent info and to evaluate/treat injuries not found during the primary survey, documentation and repositioning of the patient
List potential causes of blunt abdominal trauma.
- motor venhicle crash (MVC)
- motorcycle crash (MCC)
- pedestrian vs car
- assault w/ blunt force
- fall
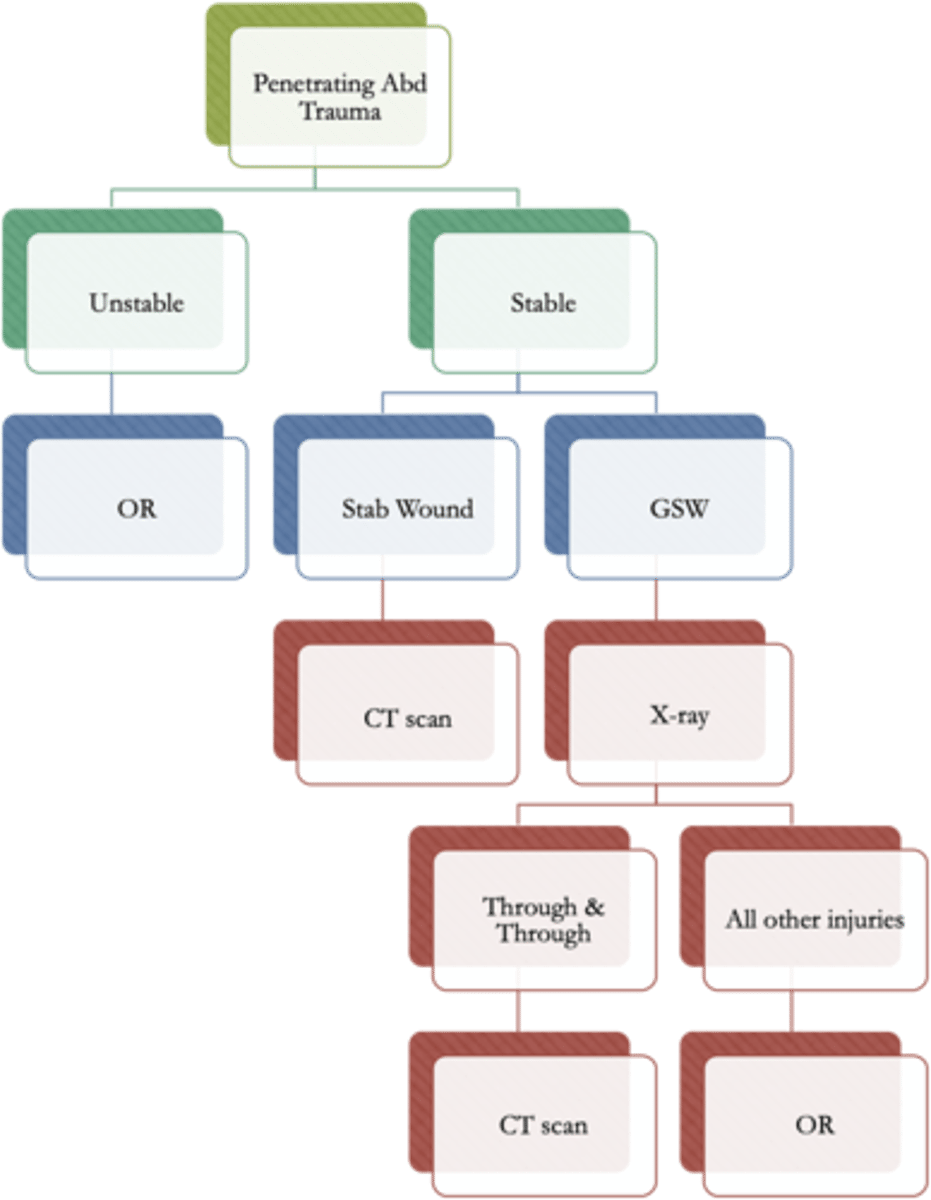
List potential causes of penetrating abdominal trauma.
- stab wound (better prognosis)
- GSW
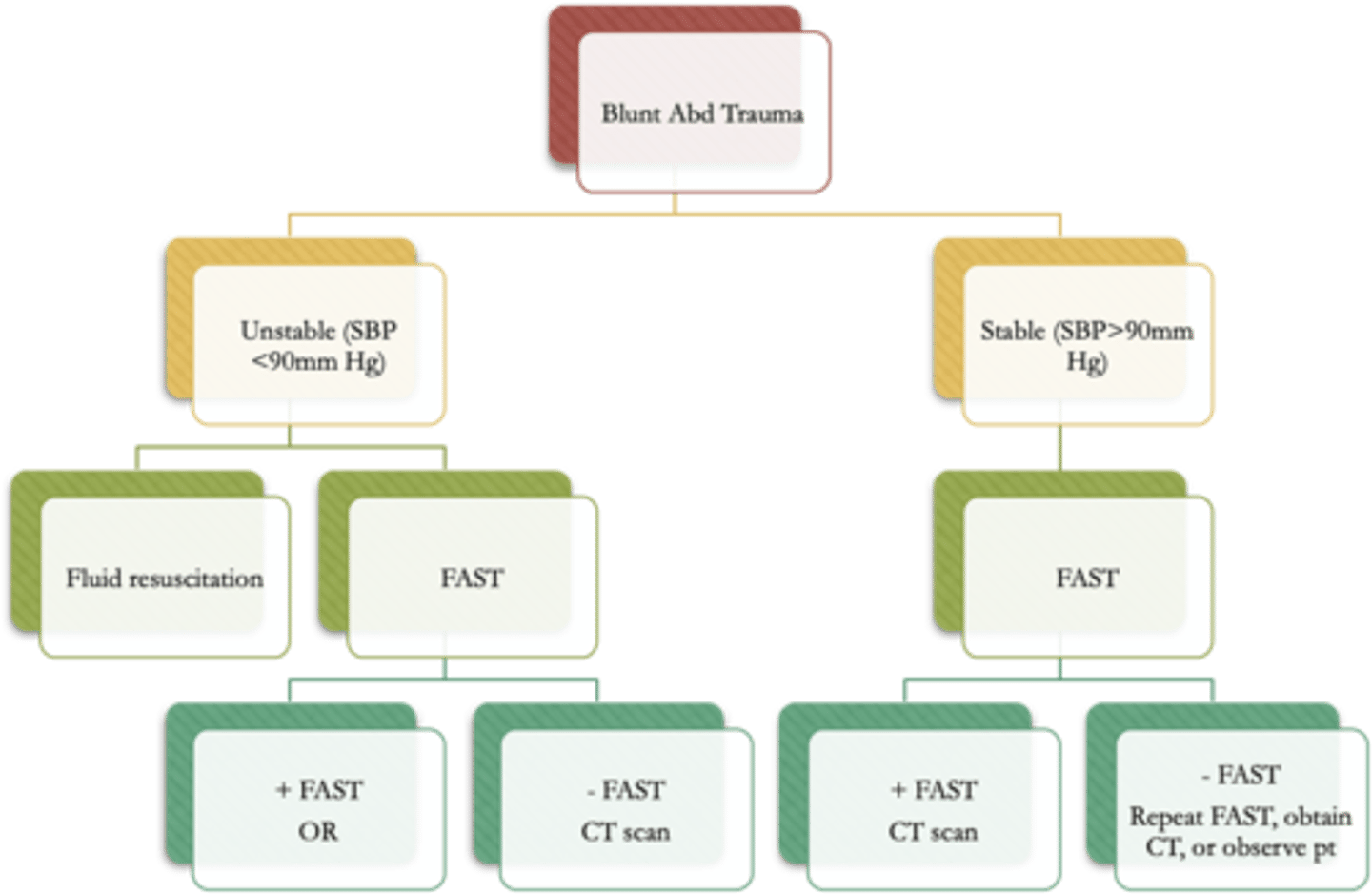
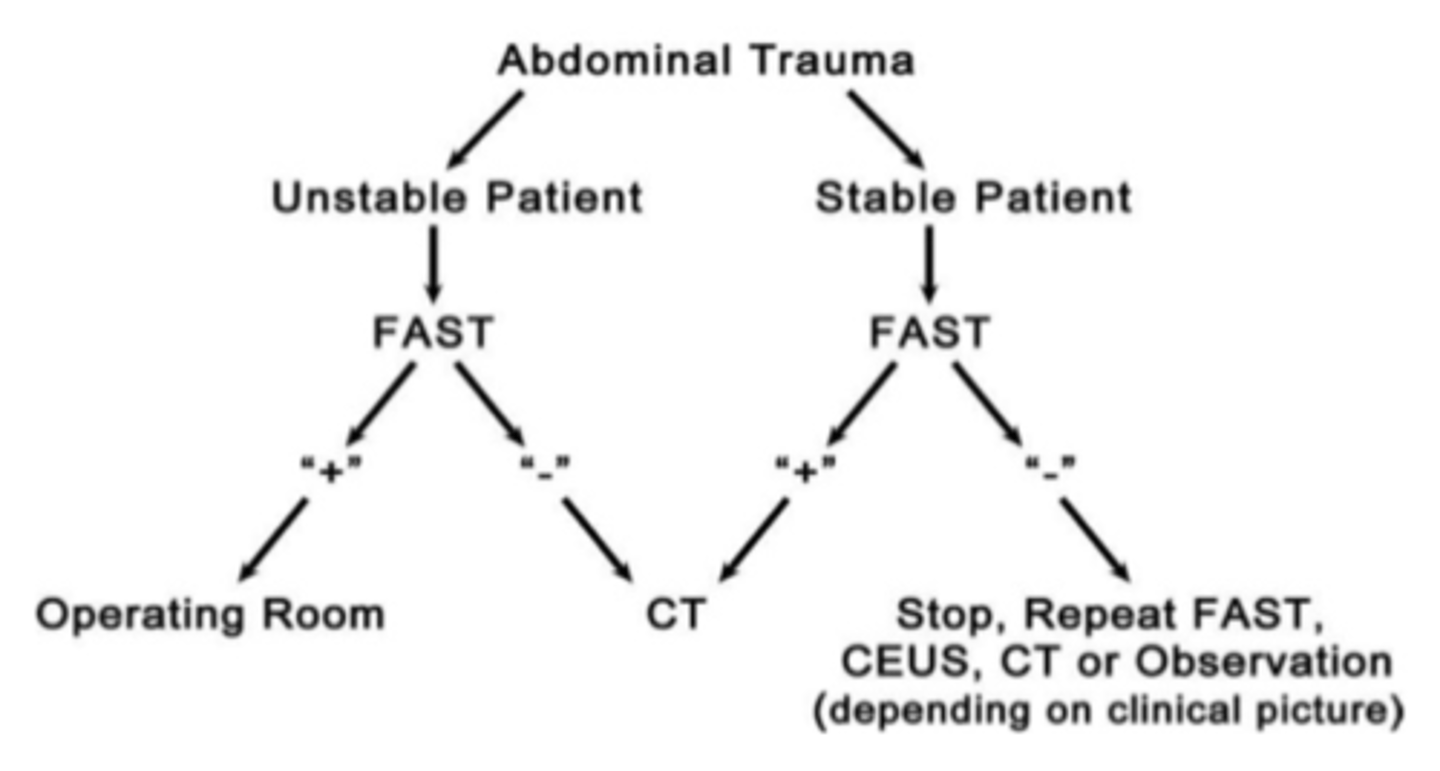
*management is shown in the picture
(depends on the object used and the hemodynamic stability of the patient)
- indication for surgery is AUTOMATICALLY hemodynamic instability (then after later eval CT scan and X-ray)
hollow viscous injury
any injury to the GI system
*usually associated with GI injury and requires exploration
Identify common injuries associated with blunt abdominal trauma.
- liver/splenic/renal laceration
- bowel/pelvic/retroperitoneal hematoma
*management is shown in the picture
Describe the pre-operative nursing management priorities of abdominal trauma.
- prep for surgical intervention
- fluid resuscitation
- protection and monitoring of ABCs
- pain management
- prevent the lethal triad
- frequent abdominal assessment (observe for distention, palpate for pain and firmness --> could be signs of intrabdominal HTN, which could lead to abdominal compartment syndrome (ACS))
focused assessment with stenography and trauma (FAST)
- emergent management of abdominal trauma
- ultrasound protocol developed to assess for peritoneal bleeding
- should not delay resuscitative measures for patients
in an unstable patient:
- positive --> transferred to the OR for laparotomy
- negative --> CAT scan performed for more diagnostic information
in a stable patient:
- positive --> CAT scan performed for more diagnostic information
- negative --> 3 options depending on clinical picture
1. repeat FAST
2. CAT scan
3. Continue to monitor the patient
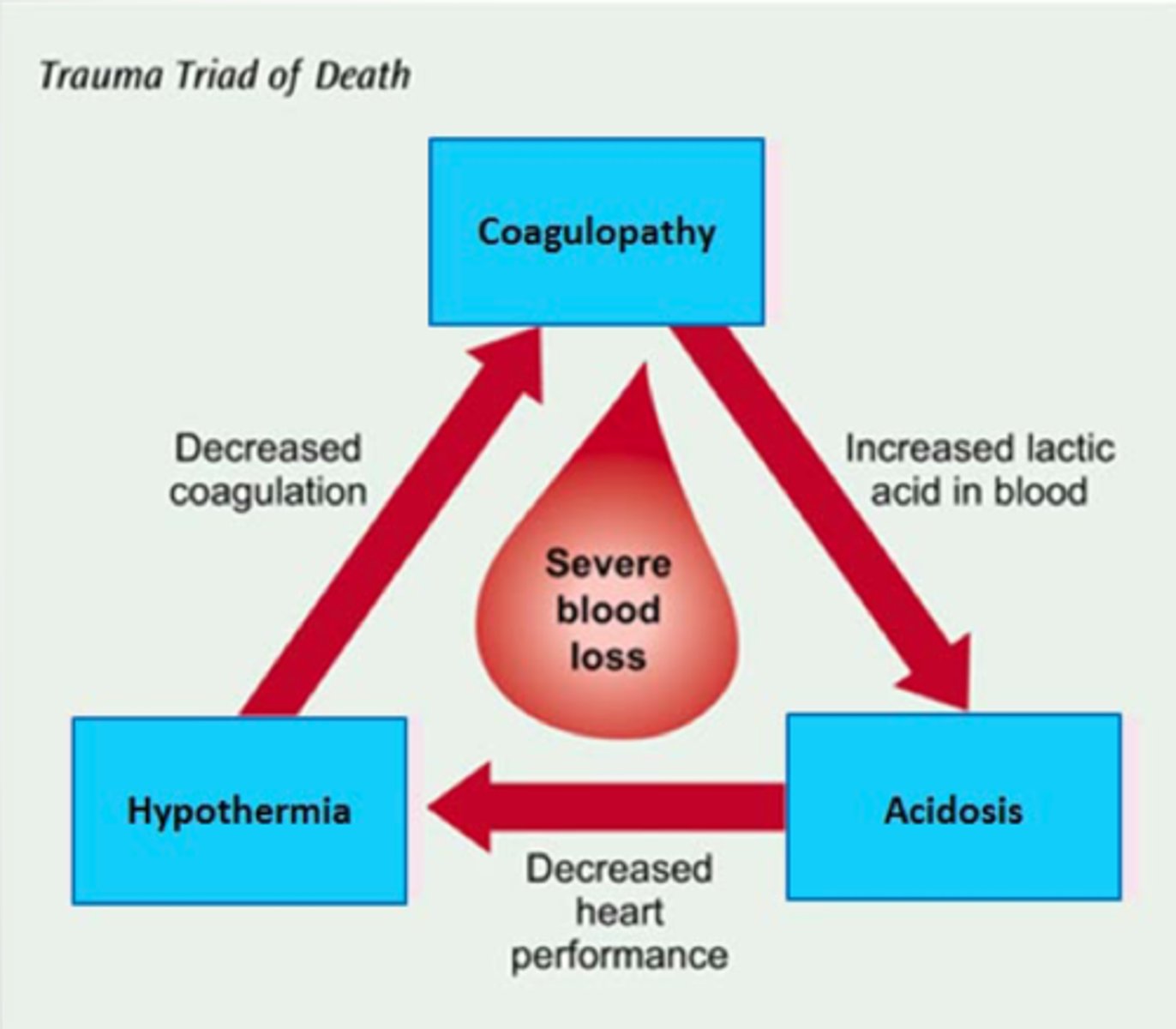
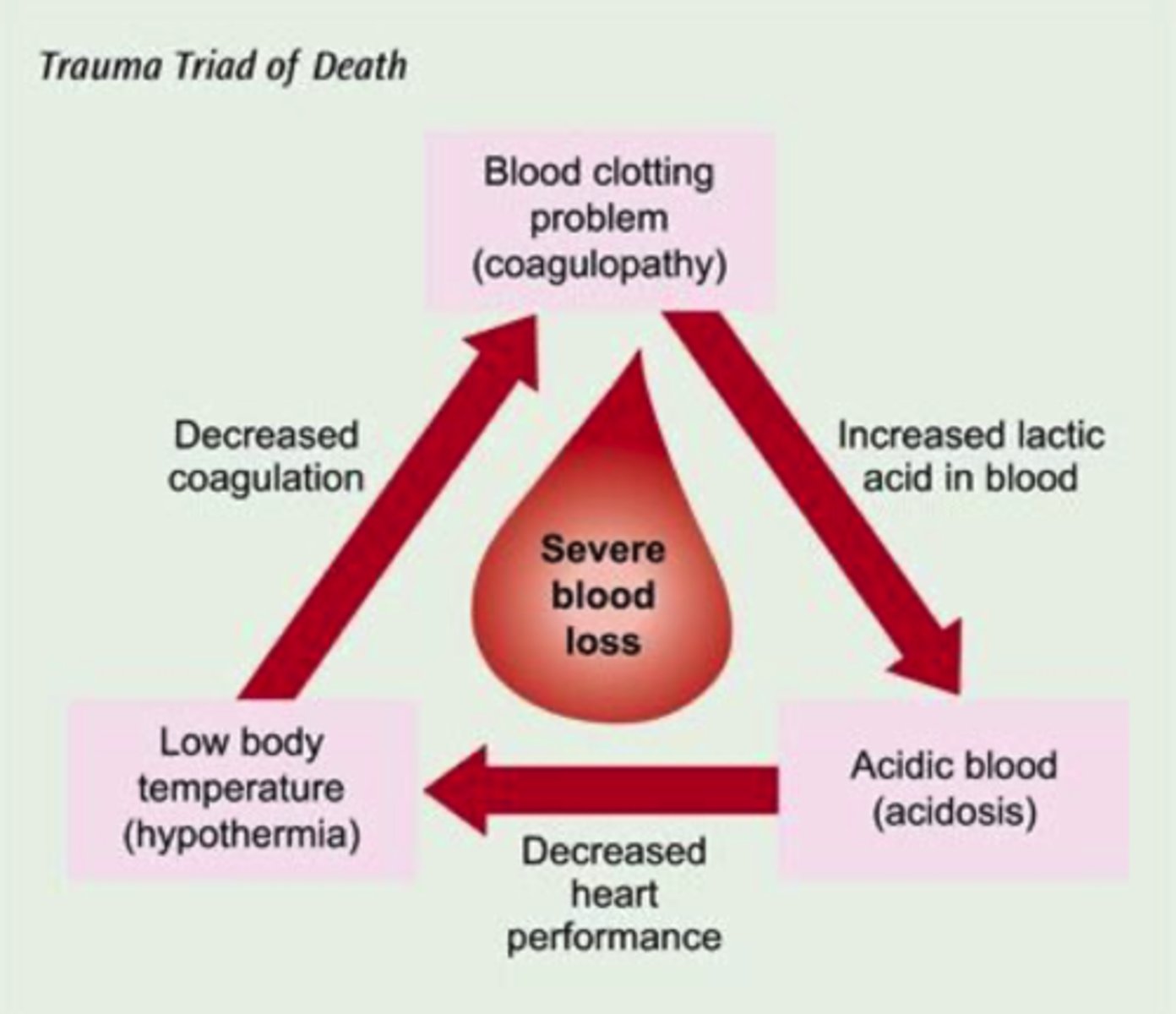
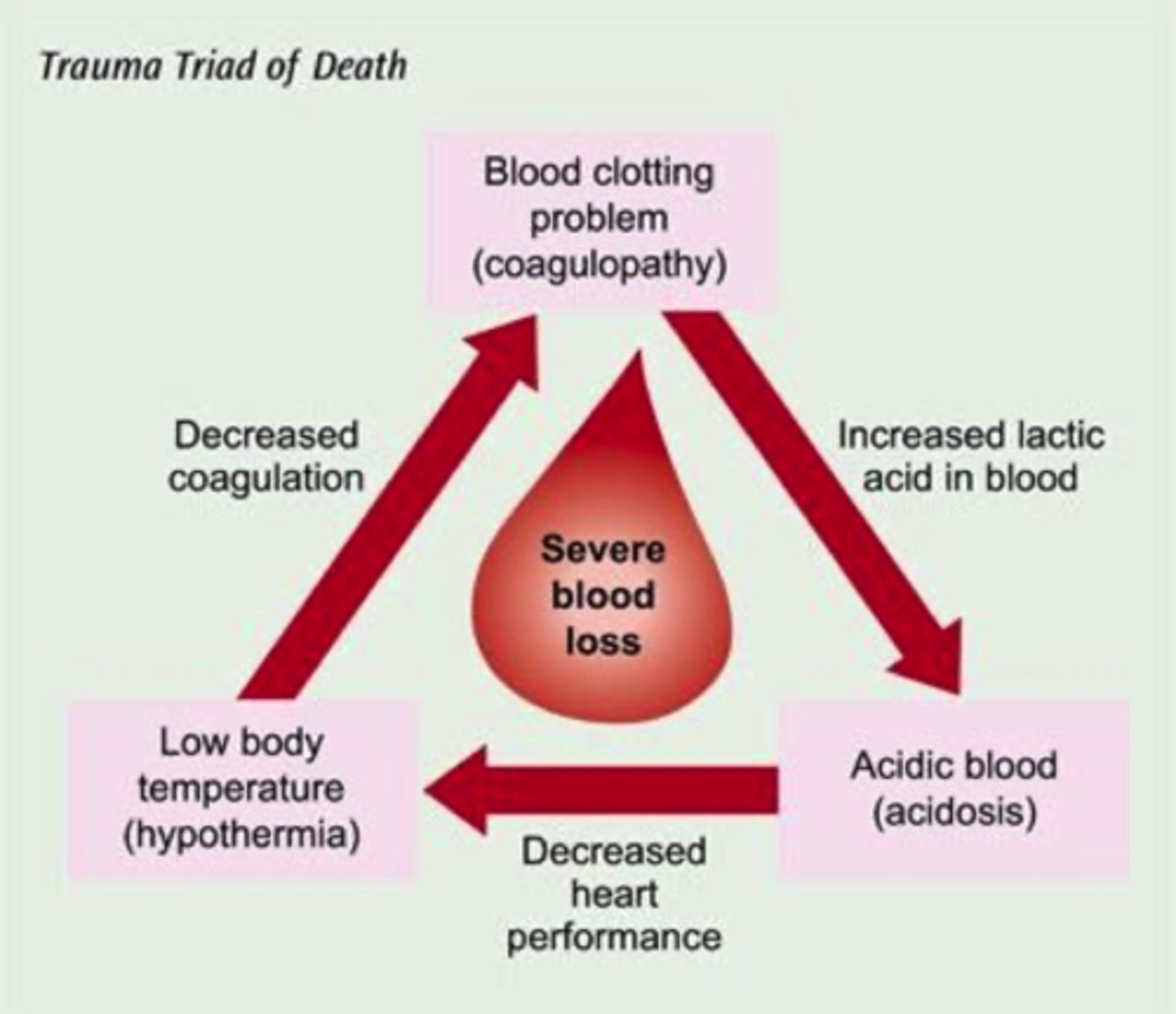
Explain the trauma triad of death.
coagulopathy, hypothermia, and acidosis
- begins and ends w/ bleeding: stop bleeding, administer warm fluids, monitor and maximize oxygenation
- hypothermia (core temp < 95F) leads to decreased coagulation
- coagulopathy occurs d/t losing clotting factors (through hemorrhage), leads to increased lactic acid in blood
- acidosis (arterial pH < 7.35) largely caused by poor tissue perfusion
management:
- find and stop the bleeding
- keep warm --> limit exposure when assessing
- admin. crystalloid and colloid fluids
- monitor and maximize oxygenation
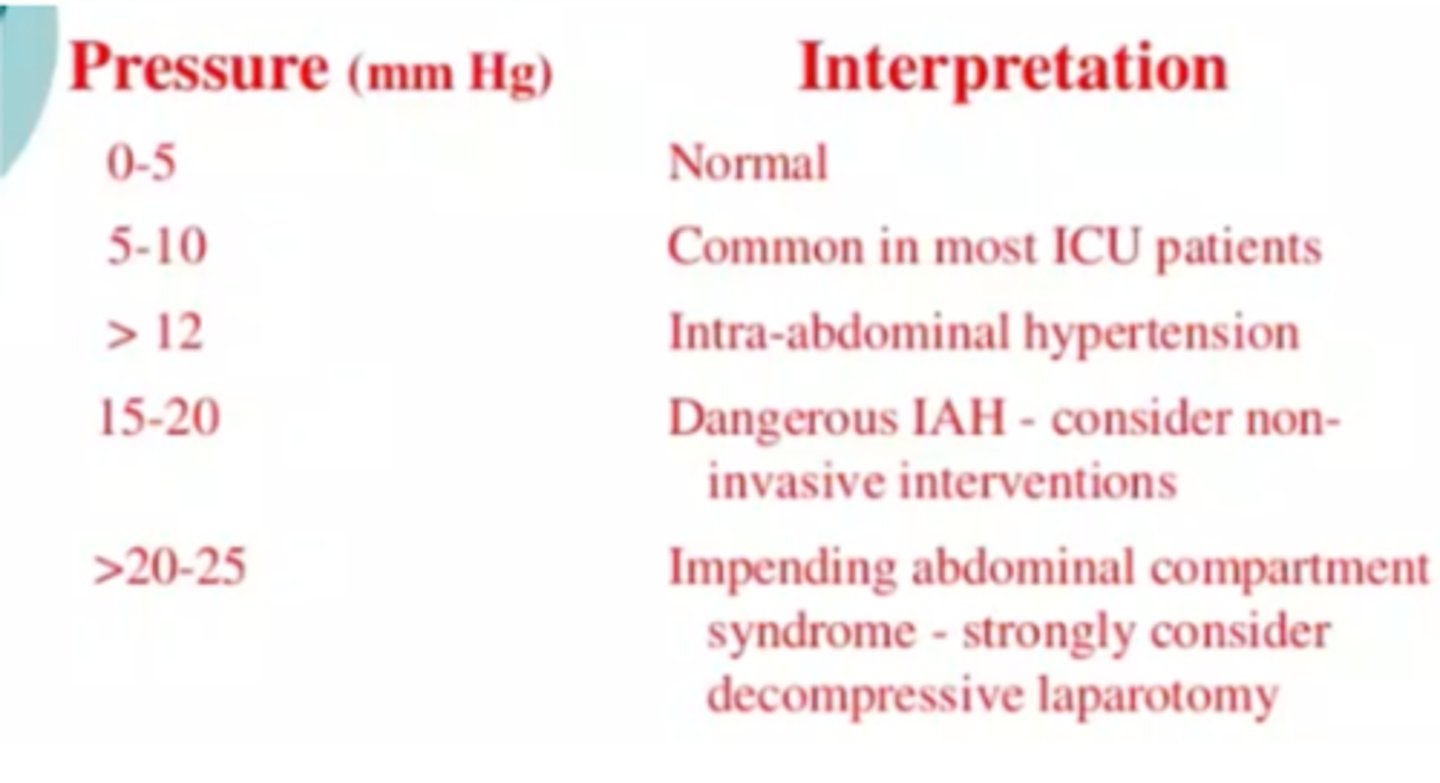
What is the significance of intraabdominal pressure monitoring?
- normal pressure should be b/w 0-5 mmHg
- use of indwelling urinary cath is only reliable if pt is heavily sedated or chemically paralyzed
- intraabdominal HTN (> 12 mmHg) can lead to abdominal compartment syndrome
- abdominal compartment syndrome is a medical emergency that requires immediate exploratory laparotomy and relief of pressure
trauma triad of death: coagulopathy
- dependent on temperature and pH b/c of its complex enzymatic properties and reactions, which help to form blood clots to stop internal/external bleeding
- describes disease states of impaired blood clotting synthesis/thrombosis
- d/t hypothermia, acidosis, AND loss clotting factors through hemorrhage and hemodilution --> which leads to an overuse by the body (which further depletes clotting factors)
- leads to continued hemorrhage in the bleeding trauma pt
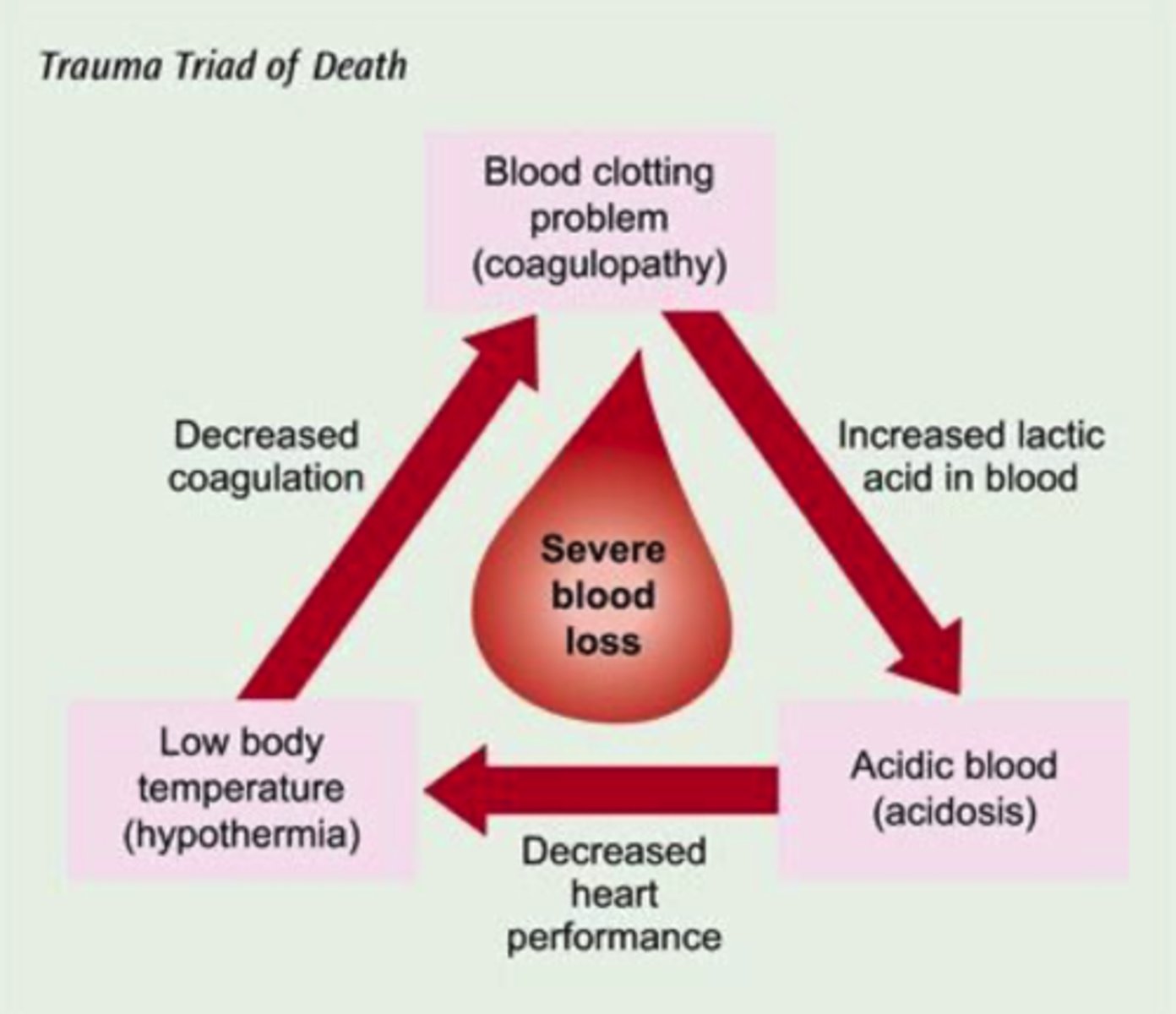
trauma triad of death: acidosis
- arterial pH less than 7.35 (normal pH 7.35-7.45)
- d/t for perfusion in tissues (in trauma)
damage control surgery
- pt only get life-threatening injuries addressed during their first OR visit
- staged approaca to post-trauma fixation allowed for shorter OR times and prevents a cytokine storm/overreactive immune response
- now a standard of care around the world
Surgery whose objective is to stop hemorrhage and prevent sepsis without attempting reconstruction or anatomical continuity.
trauma triad of death: hypothermia
- core temp less than 95 degrees farenheit (normal temp 96-98.6)
- even mild hypothermia can be devestating
- affect coagulation system (since it is temp and pH dependent_
Describe the post-op nursing management associated with abdominal trauma.
- respiratory: protect and monitor patency of airway and breathing for optimal lung expansion; monitor color and character of secretions (suction in case since its hard to cough after surgery)
- CV: hemodynamic stability.
IV isotonic and hypertonic crystalloid fluids 20-30 mL/kg, such as LR or NSS
colloids intravascular longer, rapidly expand plasma volume, such as fresh frozen plasma and albumin
vasopressors for vasoconstriction, e.g., synthetic ADH
monitor I & Os (think about impact on heart)
- monitor mental status
- hematologic: stop the bleed; prevent trauma triad of death, keep patient warm, crystalloid and colloid fluids. monitor and maximize oxygenation
- GI: frequent abdom assessments (inspect, ausculate, ask/palpate for pain and firmness of adbomnial wall), trend bladder pressures via indwelling urinary catheter, nutrition helps keep the brush barrier active to fight infections, 1.5-2.5 g/kg/day of protein, weekly labs, daily weights, advocate for TPN within 48 hours of initial damage control procedure if TEN contraindicated
*normal abdominal pressure: 0-5 mL of Mercury (only reliable when pt is sedated
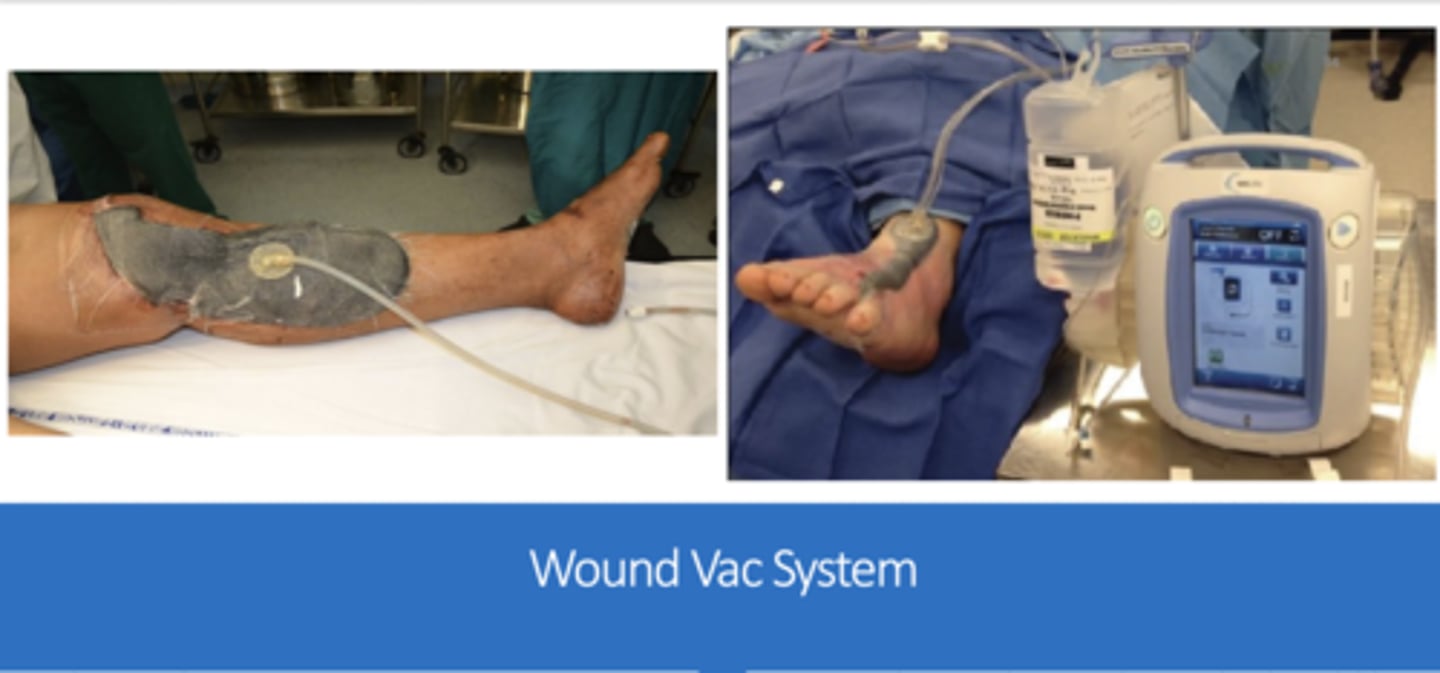
surgical site incision can be
a) midline incision w/ full abdominal closure
b) partial closure (fascia closed, skin open)
c) open abdomen w/ ABThera VAC
indications for open abdomen:
Damage control surgery
Abdominal compartment syndrome
Massive fluid replacement
Requirement for second-look surgery ->To assess bowel viability or to evaluate and treat continued intra-abdominal contamination
negative system wound therapy/vacuum assisted wound closure
signs of decreased perfusion
- CNS/brain: restlessness/anxiety -progressing to-> agitation/confusion
- cardiac: increased HR, decreased BP
- GI: decreased motility, then ileus, then mesenteric ischemia
- renal: decreased urine output -then-> oliguria -then-> anuria
- skin: decreased cap refill, cold extremities -then-> mottled, cyanotic, cold extremities
Explain the potential complications in abdominal trauma: general
the longer the delay of abdominal closure, the greater the risk; abdominal viscera become immobilized and cocoon-like (frozen abdomen) within 14-21 days
- when dealt with it statistically decreases times in the hospital
Explain the potential complications in abdominal trauma: abdominal compartment syndrome (ACS)
- intrabdomnial hypertension (results in MODS)
- abnormally increased pressure within the abdomen that is assoc. w/ organ dysfunction
- risk factors: trauma, surgery, infection
- causes: brain swelling/ischemia, decreased cardiac output, IVC blood flow obstruction (diminished BF to LE), arterial hypoxemia/hypercarbia, impaired venous damage (major cause of renal impairment), hypoperfusion/ischemia of bowel d/t decreased mesenteric blood flow
- clinical manifestations: abdominal distention/tense, rigid abdomen; disproportionate abdominal pain; tachypnea and/or dyspnea
- treatment: Emergency!! Immediately to OR for exploratory laparotomy, NEED TO RELIEVE THIS PRESSURE
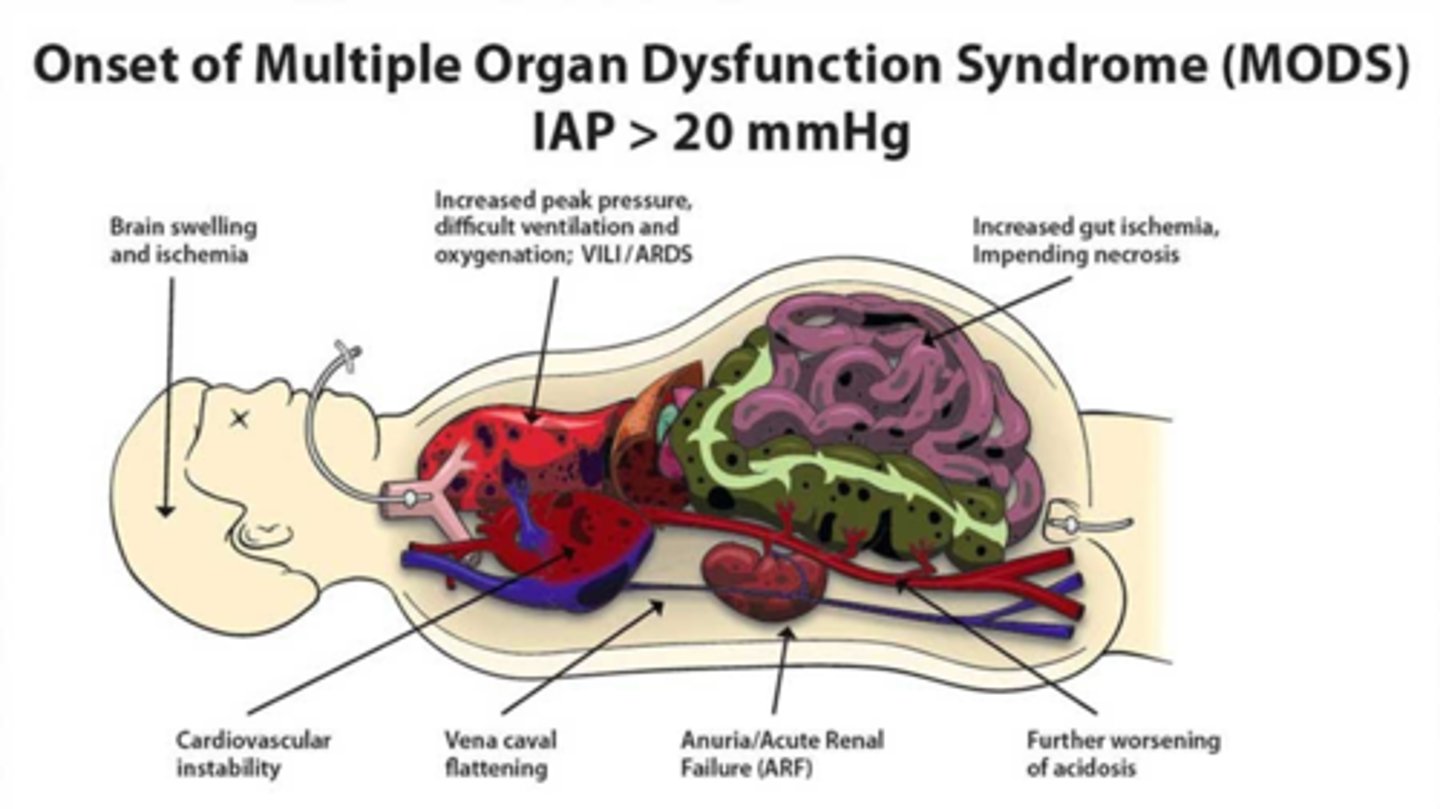
concerning intrabdominal pressures
> 12 mmHg = intra-abdominal hypertension
15-20 mmHg = dangerous -> consider non-invasive interventions
> 20-25 mmHg = impending ACS (consider decompressive laparotomy)
0-5 mmHg = normal
5-10 mmHg = common in ICU pt
Explain the potential complications in abdominal trauma: renal injury
(look at this, but not a lot of time is spent on this since we already talked about this)
- causes: pre-renal (secondary to impaired perfusion, e.g. hypovolemic shock), intra-renal (secondary to prolonged hypotension; antibiotics, IV contrast dye)
- ursing interventions: monitor urine output (notify if < 0.5 mL/kg/hr), monitor Cr, BUN, electrolytes
Explain the potential complications in abdominal trauma: infection
(look at this, but not a lot of time is spent on this since we already talked about this)
major infections in 10-15% of abdo trauma patients; highest risk factor in hollow, viscous injury
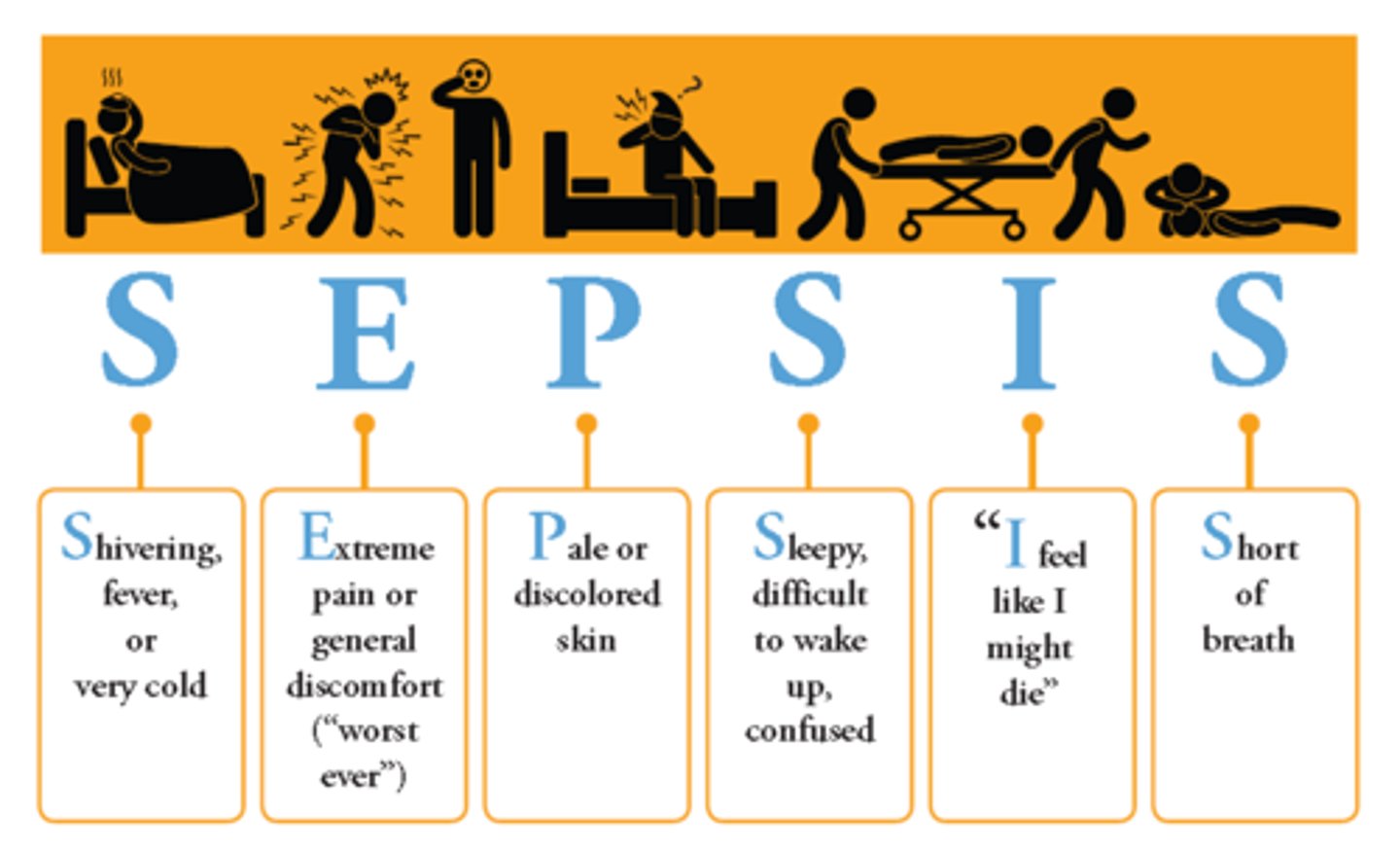
- monitor for SEPSIS (shivering/fever, extreme pain/general discomfort, pale/discolored skin, sleepy/difficult to arouse/confused, statements such as "I feel like I might die," SOB)
- Abx: prophylaxis (post-op) vs tx (active or suspected infection; always look at culture data)
SEPSIS
Describe the anatomy of the brain. If a lesion was present in any one area of the brain, what findings/deficits might you see in the patient?
cerebrum
- frontal lobe: concentration, planning, speech, smell, motor control
- parietal lobe: touch and pressure, taste, body awareness
- temporal lobe: hearing, facial recognition
- occipital lobe: vision
cerebellum: coordination
brain stem: autonomic function (breathing, HR, BP, sleep)
Review the history and physical examination related to the neurological system (cranial nerves, motor, sensory, reflexes, Glasgow Coma Scale, mental status). What are normal and abnormal findings? How might findings vary per patient age?
ABCDE
Glasgow coma scale: objective level of the patient's conscious state
-