oropharynx
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
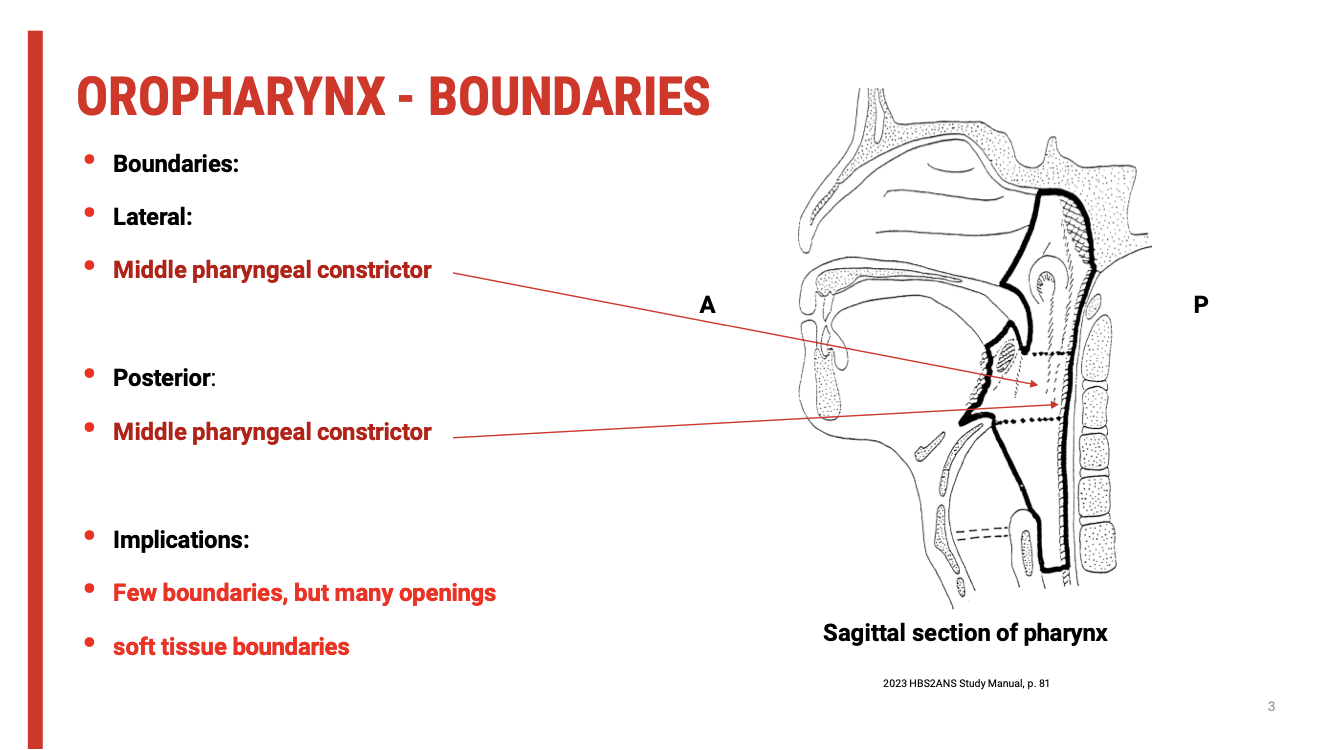
Oropharynx Boundaries
Lateral & Posterior Boundaries:
Middle pharyngeal constrictor muscles
These muscles form much of the oropharyngeal wall and play a key role in propelling the bolus during swallowing.
Superior, Anterior, and Inferior Aspects:
Characterised by openings rather than rigid anatomical boundaries.
These include:
Superior: opening to the nasopharynx
Anterior: opening to the oral cavity via the oropharyngeal isthmus
Inferior: opening to the laryngopharynx
Clinical Implication
Soft tissue boundaries dominate:
Unlike rigid bony boundaries, these are dynamic and muscular.
This makes coordination critical during swallowing, as precise timing and movement are needed to prevent aspiration and ensure bolus transit.
Swallowing relies heavily on muscular coordination, especially between:
Soft palate (velopharyngeal closure)
Tongue base retraction
Pharyngeal wall constriction
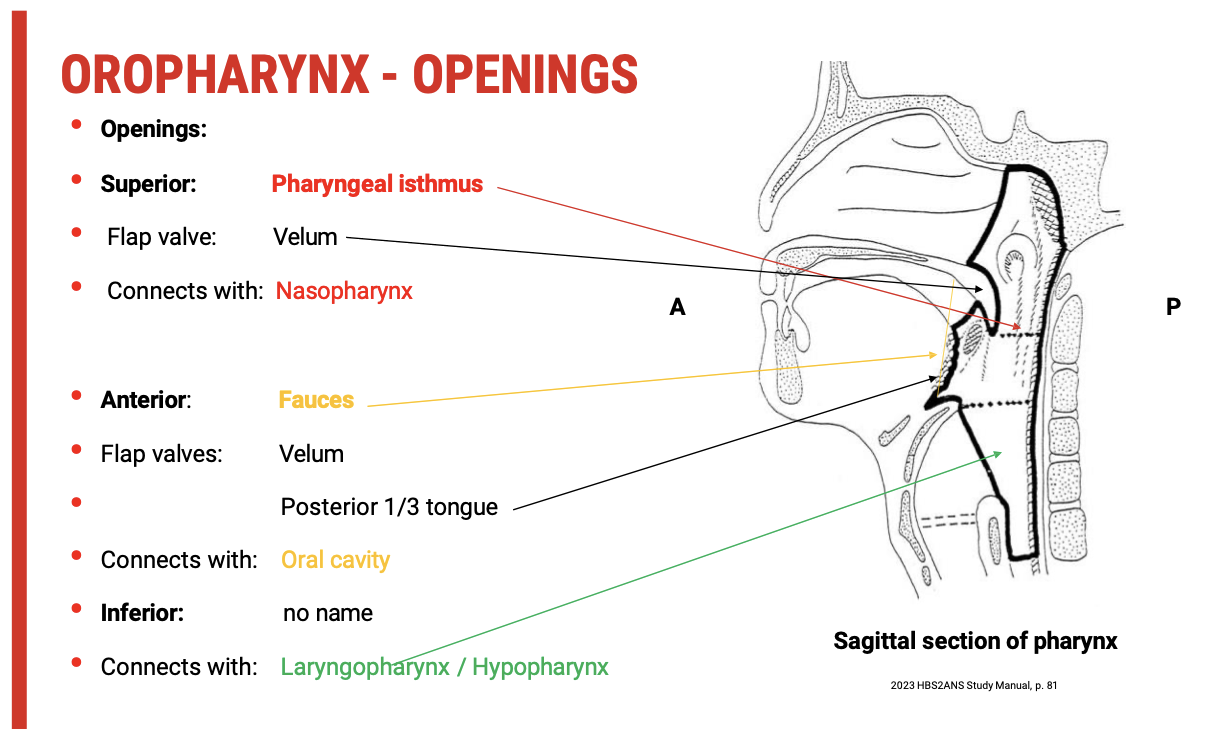
Openings of the oropharynx
1. Superior Opening
Structure: Pharyngeal isthmus
Leads to: Nasopharynx
Guarded by:
Soft palate (vellum) acting as a flat valve
Function:
During swallowing, the soft palate elevates to close off the nasopharynx, preventing food or liquid from entering the nasal cavity (velopharyngeal closure).
2. Anterior Opening
Structure: Fauces
Leads to: Oral cavity
Guarded by:
Soft palate (vellum)
Posterior third of the tongue
Function:
Acts as a gate between the oral cavity and oropharynx, essential for bolus control and swallow initiation.
3. Inferior Opening
Structure: Unnamed opening
Leads to: Laryngopharynx (hypopharynx) and then to the oesophagus
Guarded by: No distinct valve structure, but protected during swallowing by laryngeal elevation and epiglottic inversion
Function:
Allows passage of bolus toward the oesophagus while coordinating with airway protection mechanisms
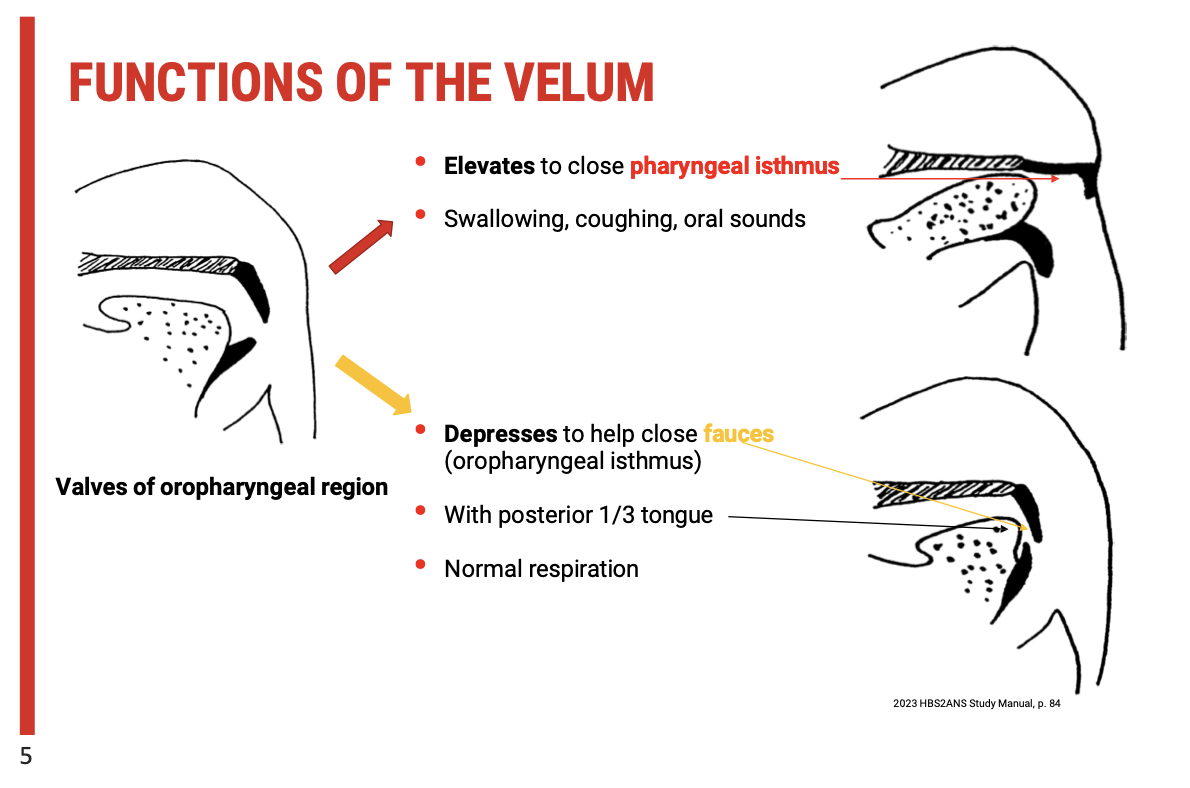
Functions of the Velum (Soft Palate)
1. Velar Elevation
Action: The velum elevates to contact the posterior pharyngeal wall.
Purpose:
Closes the pharyngeal isthmus (between the nasopharynx and oropharynx).
Prevents food or liquid from entering the nasal cavity during:
Swallowing
Coughing
Production of certain oral speech sounds (e.g. plosives, fricatives)
Key Function: Facilitates velopharyngeal port closure for airway protection and sound clarity in speech.
2. Velar Depression
Action: The velum lowers toward the tongue.
Purpose:
Helps close the fauces (aka oropharyngeal isthmus) with the posterior third of the tongue.
Occurs during normal nasal breathing (respiration).
Key Function: Maintains an open passage between the oral and nasal cavities for airflow during rest.
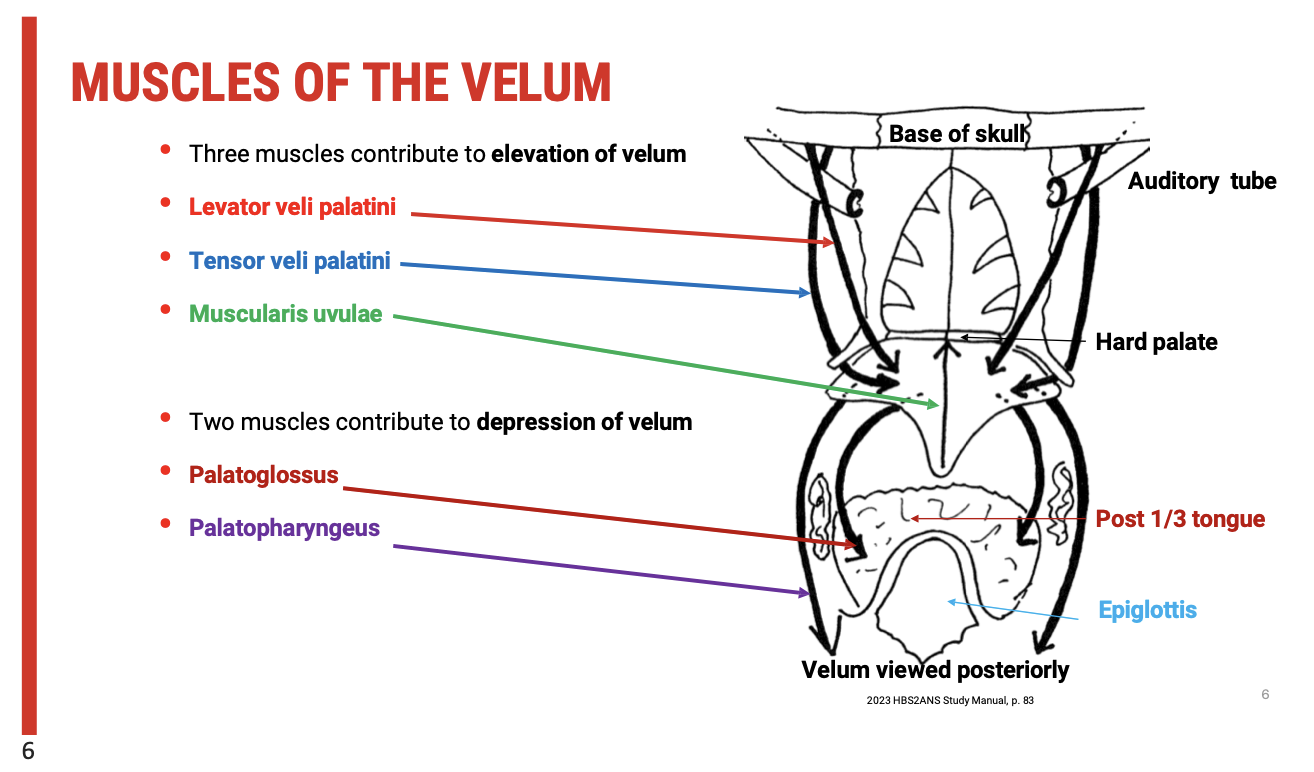
Muscles of the Velum (Soft Palate)
Muscles That Elevate the Velum (Located Superiorly)
Muscle | Function |
Levator veli palatini | Primary elevator of the soft palate; lifts the velum for closure of the pharyngeal isthmus |
Tensor veli palatini | Tenses and then elevates the velum; also opens the Eustachian tube |
Musculus uvulae | Shortens and stiffens the uvula; assists with velopharyngeal closure |
Muscles That Depress the Velum (Located Inferiorly)
Muscle | Function |
Palatoglossus | Depresses the velum and narrows the oropharyngeal isthmus; elevates the posterior tongue |
Palatopharyngeus | Depresses the velum and helps guide the bolus into the pharynx; also contributes to pharyngeal wall movement |
These muscles work in coordination to regulate velopharyngeal port function—essential for swallowing, breathing, and speech.
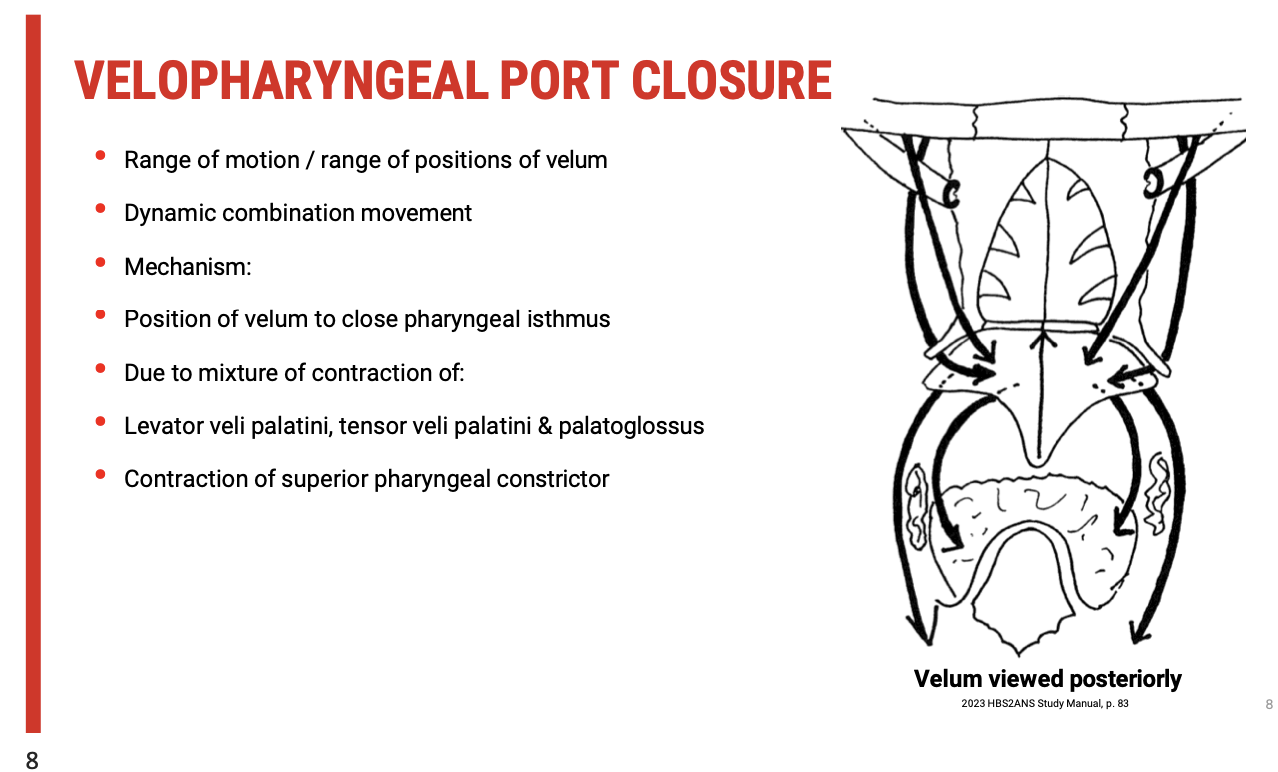
Velopharyngeal Port Closure and its Importance in Swallowing
The velopharyngeal port is a crucial anatomical structure that separates the nasopharynx from the oropharynx. For effective swallowing, it's essential to close the velopharyngeal port to prevent food or fluid from entering the nasopharynx and ensuring that the bolus moves correctly into the oropharynx and further down the digestive tract. Here’s a recap of the muscles involved in this process:
Muscles Contributing to Velopharyngeal Port Closure
Levator Veli Palatini
Function: Elevates the soft palate (vellum) to close off the nasopharynx from the oropharynx.
Tensor Veli Palatini
Function: Tenses and helps to elevate the velum, playing a role in the overall closure of the nasopharynx during swallowing.
Musculus Uvulae
Function: Shortens and stiffens the uvula, assisting in further sealing the nasopharyngeal passage.
Depressor Muscles (Palatoglossus and Palatopharyngeus)
These muscles work to depress the velum, which contributes to the opening of the oropharyngeal isthmus during swallowing and speech production but also assists in adjusting the velopharyngeal port closure.
Coordination for Swallowing
The soft tissue boundaries—created by these muscles—are flexible, which means their function must be well-coordinated to ensure proper swallowing.
The velopharyngeal port closure must happen in synchrony with other swallowing mechanisms to prevent nasal regurgitation and ensure that food and liquids are directed into the esophagus rather than the nasal cavity.
Dynamic Function of the Velopharyngeal Port in Swallowing
Dynamic Function of the Velopharyngeal Port in Swallowing
One of the critical concepts is understanding that velopharyngeal port closure is not a simple "open or shut" mechanism. Instead, it involves a dynamic range of motion and precise positioning of the velum (soft palate). This movement is coordinated by multiple muscles that work together in varying degrees to adjust the closure according to the needs of swallowing, speech, and even respiration.
Key Muscles in Velopharyngeal Port Closure
Levator Veli Palatini: Elevates the soft palate, contributing to sealing the nasopharynx during swallowing.
Tensor Veli Palatini: Tenses and assists in the elevation of the velum.
Palatoglossus: Plays a role in depressing the velum, influencing the overall closure mechanism.
Superior Pharyngeal Constrictor: This muscle surrounds the velum and contracts to assist in sealing the pharyngeal isthmus, ensuring the food moves forward rather than backward.
Dynamic Combination of Movements
The velopharyngeal port closure is a combination of muscle contractions and movements. These muscles must work together to achieve the proper positioning of the velum to ensure the separation of the nasopharynx from the oropharynx during swallowing. This coordinated action prevents the nasal regurgitation of food and directs the bolus toward the esophagus.
Postoperative Considerations for Emma
In the case of Emma's postoperative course, if she’s experiencing swallowing difficulties, the issue may lie in her ability to coordinate these muscles effectively. Potential factors include:
Weakness or dysfunction in the levator or tensor veli palatini, which could hinder effective velum elevation and closure.
Difficulty in superior pharyngeal constrictor contraction, which would impair the overall process of swallowing.
Impaired coordination of these movements, leading to disrupted swallowing dynamics.
Implications for Clinical Management
Rehabilitation of the velopharyngeal mechanism could involve targeted exercises to improve the strength and coordination of these muscles.
Therapies such as speech or swallow exercises might focus on improving the muscle coordination and ensuring the dynamic movement of the velum is restored.
Walls of the Oropharynx
The oropharynx, like the oral cavity, is lined by squamous mucosa. This is a type of squamous epithelium that serves as a protective layer, providing durability and resistance to mechanical stress during swallowing.
Pharyngeal Constrictors
The pharyngeal constrictors play an important role in the mechanics of swallowing, helping to propel food and liquid from the oropharynx into the esophagus. These muscles are arranged in an overlapping manner, providing strength and coordination during the swallowing process. There are three main pharyngeal constrictors that surround the pharynx in a sequential fashion:
Superior Pharyngeal Constrictor
Surrounds the nasopharynx.
Plays a role in sealing off the nasopharynx during swallowing, preventing food from entering the nasal cavity.
Middle Pharyngeal Constrictor
Surrounds the oropharynx.
Involved in the peristaltic contraction that moves the bolus from the oropharynx toward the laryngopharynx.
Inferior Pharyngeal Constrictor
Surrounds the laryngopharynx.
Plays a key role in moving the food bolus into the esophagus during swallowing.
Implications for Dysphagia
The proper function of these overlapping constrictors is crucial for effective swallowing. If there is dysfunction in one or more of these muscles, it can lead to dysphagia, where the bolus is not efficiently moved through the pharynx.
Conditions affecting the swallowing mechanism, such as Parkinson’s disease or after surgical interventions, may impact the coordination of these muscles, causing difficulty in swallowing and potential aspiration.
Innervation of the Oropharynx

The innervation of the oropharynx involves both sensory (afferent) and motor (efferent) components, with contributions from key cranial nerves:
Sensory Innervation (General Visceral Afferent):
Glossopharyngeal Nerve (CN IX):
Provides sensory innervation to the oropharynx, which includes general visceral afferent functions. This nerve is responsible for conveying sensations such as touch, pain, and temperature from the oropharynx.
It plays a role in monitoring the presence of food or liquids in the oropharynx during the swallowing process, contributing to the protective reflexes during swallowing.
Motor Innervation (General Visceral Efferent):
Vagus Nerve (CN X):
The vagus nerve supplies motor innervation to the muscles of the pharynx, including the constrictor muscles, and muscles of the soft palate (e.g., levator veli palatini, palatoglossus).
It is responsible for coordinating the movement of the muscles during swallowing, which helps propel the bolus down the pharynx and prevents food from entering the nasopharynx or larynx.
Blood Supply of the Oropharynx
The blood supply to the oropharynx is primarily derived from branches of the external carotid artery, which include:
The Tonsillar Branch:
Supplies blood to the palatine tonsils and surrounding pharyngeal structures.
The Ascending Pharyngeal Artery:
Supplies the posterior and lateral aspects of the pharynx, including the oropharynx.
The Lingual Artery:
Provides blood to the base of the tongue and the anterior portion of the oropharynx.
These vascular structures ensure that the oropharynx receives adequate blood flow to support the highly dynamic processes of swallowing.
Implications for Dysphagia and Dysfunction
Damage to the glossopharyngeal nerve (e.g., from stroke or surgical procedures) can result in sensory deficits in the oropharynx, potentially causing issues with swallowing reflexes and increasing the risk of aspiration.
Dysfunction in the vagus nerve can lead to motor impairments in the muscles of the oropharynx, which may affect the ability to coordinate swallowing, leading to dysphagia.
Poor blood supply (e.g., due to vascular disease or surgery) could also impact the health of the tissues in the oropharynx, impairing muscle function and healing after injury or surgery.
Blood Supply and Venous Drainage of the Oropharynx
The blood supply and venous drainage of the oropharynx are essential for maintaining the health and function of the tissues in this region. The area is highly vascular, which is important for both normal function and wound healing, especially in surgical contexts.
Blood Supply
Tonsillar Artery (Branch of the Facial Artery):
The tonsillar artery is the main source of blood supply to the oropharynx, running deep to the palatine tonsils.
This artery is a branch of the facial artery, which also supplies blood to various structures in the face, including the oral cavity and the palate.
Ascendancy of the Blood Flow:
The vascular nature of this area is important for wound healing in cases like tonsillectomies or surgeries involving the soft palate or oropharynx.
Venous Drainage
External Palatine Vein:
The external palatine vein drains blood from the oropharynx. It is closely associated with the tonsillar artery and travels through the pharyngeal structures.
Pharyngeal Venous Plexus:
This vein empties into the pharyngeal venous plexus, which is a network of veins surrounding the pharynx.
Internal Jugular Vein:
The venous plexus drains into the internal jugular vein, which then returns deoxygenated blood from the head and neck to the heart.
This well-developed venous drainage ensures that the oropharynx and surrounding tissues are efficiently drained of blood, helping to maintain proper tissue pressure and preventing venous congestion, which could affect swallowing or other functions.
Lymphatic Drainage
Rich Lymphatic Drainage:
Given the vascularity of the oropharynx, it is logical to expect a rich lymphatic drainage as well.
The lymphatic vessels in this region help to filter out pathogens and facilitate immune responses.
These lymphatic vessels converge towards lymph nodes in the neck, including the jugulodigastric lymph nodes (also known as the tonsillar nodes) which are important in immune surveillance and inflammation.
Implications for Swallowing and Health
High Vascularity:
The vascular nature of the region supports rapid healing after surgeries like tonsillectomies, but also means that bleeding is a potential concern. Surgeons must be careful to control bleeding during procedures.
Lymphatic Drainage:
The rich lymphatic system helps in defending against infections but can also contribute to the spread of infections or cancers from the oropharynx to lymph nodes in the neck.
Dysphagia (Swallowing Difficulties):
Venous congestion or lymphatic obstruction can affect the muscle coordination and tissue health, leading to difficulty with swallowing or other complications.
Lymphatic Drainage and Cancer Spread in the Oropharynx
The oropharynx and surrounding regions have multiple pathways for lymphatic drainage, which plays a crucial role in the spread of cancer from these areas. Understanding these pathways is vital for diagnosing, staging, and treating head and neck cancers.
Lymphatic Pathways for Cancer Spread
Oral Cavity and Oropharynx to Lymph Nodes:
Cancer in the oral cavity or oropharynx can spread through the lymphatic system to the submental lymph nodes (under the chin).
Further spread can involve the submandibular lymph nodes, which are located below the jawline.
As the cancer spreads more posteriorly, it can reach inferior deep cervical lymph nodes in the neck.
Key Lymph Node: Jugular Omohyoid Lymph Node
The jugular omohyoid lymph node is a critical landmark in cancer staging. If this node is involved, it suggests that the cancer has spread further, possibly indicating more advanced stages.
This lymph node serves as a significant marker in assessing the risk of metastasis.
Implications for Cancer Treatment
Thorough Staging:
When assessing patients with head and neck cancer, clinicians must consider multidisciplinary workup, including imaging and clinical evaluation to determine the spread of cancer to lymph nodes.
Proactive Lymph Node Removal:
If there is evidence of significant spread, surgeons may decide to proactively remove lymph nodes. This helps prevent further metastasis and facilitates better outcomes.
Multidisciplinary Team Approach:
Head and neck cancer treatment involves various specialists working together to ensure comprehensive care:
ENT surgeons, plastic surgeons for reconstruction
Radiation oncologists and oncologists for chemotherapy and radiation therapy
Radiologists and pathologists for accurate diagnosis and staging
Head and neck cancer nurses to provide ongoing care
Speech pathologists play an essential role in swallowing rehabilitation, as the oropharynx is crucial for this function.
Role of Speech Pathologists
Speech Pathologists’ Role in Swallowing Assessment:
As key members of the team, speech pathologists contribute significantly to the overall function of the oropharynx, especially regarding swallowing and speech function.
They help assess swallowing difficulties (dysphagia) and provide therapy to ensure patients maintain their ability to swallow effectively post-surgery or post-treatment.
By ensuring a thorough and comprehensive approach to diagnosis, treatment, and rehabilitation, the multidisciplinary team can significantly improve outcomes for individuals with head and neck cancer, particularly with swallowingfunction being a primary focus.