VM 577 Midterm Part II
1/108
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
109 Terms
Which of the following would be an appropriate choice for initiating insulin therapy for a canine patient with uncomplicated diabetes? Select all that apply
A. NPH insulin: 6 U SQ, q12h
B. Insulin glargine: 12 U SQ q24h
C. Insulin glargine: 6 U SQ q12h
D. Insulin detemir 6 U SQ q12h
E. Vetsulin insulin: 6 U SQ q12h
A. OR E.
Which of the following would be an appropriate choice for initiating insulin therapy for a feline patient with uncomplicated diabetes? Select all that apply
A. NPH insulin: 1 U SQ, q12h
B. Regular insulin: 1 U SQ q12h
C. Insulin glargine: 1 U SQ q24h
D. Insulin glargine 1 U SQ q12h
E. Prozinc insulin: 1 U SQ q12h
D. OR E.
An 18-year-old neutered male Siamese cat (2.9 kg, BCS 2/9) was diagnosed with diabetes mellitus 2 months ago. He is currently being treated with ProZinc 1.5 U SQ q12h and a high-protein diet. He is being evaluated for persistent clinical signs. On physical exam, he is thin but otherwise unremarkable. A spot blood glucose taken 4 hours post-insulin is 187 mg/dL.
What action do you take?
A. Increase the dose to 2 U BID
B. Decrease the dose to 1 U BID
C. Switch to a longer acting insulin
D. Switch to a shorter acting insulin
E. None of the above
E. → can’t tell unless we have a curve
What is the value of a spot glucose in the management of a diabetic dog/cat?
A. If > 300 mg/dL, it indicates that the pet needs more insulin.
B. If < 40 mg/dL, it indicates that pet has received too much insulin.
C. If value is normal 4-6 hours after insulin treatment, it indicates therapy is adequate.
D. There is no value in spot blood glucose checks.
B.
How do you interpret a negative urine glucose when managing a diabetic patient:
A. The pet was possibly hypoglycemic.
B. The pet was possibly normoglycemic.
C. The pet was possibly hyperglycemic.
D. Choices A and B
E. All of the above
E.
What is the glucose renal tubular threshold in: cats vs dogs
Cats: 250-300 mg/dL
Dogs: 180-200 mg/dl
Dog is mildly PU/PD and polyphagic, but maintaining weight. Great energy level. Insulin at 8:05 am. Blood glucose curve (80-120mg/dL):
• 8:00 am – 340 mg/dL
• 10:00 am – 190 mg/dL
• 12:00 pm – 99 mg/dL
• 2:00 pm – 128 mg/dL
• 4:00 pm – 248 mg/dL
• 6:00 pm – 301 mg/dL
• 8:00 pm – 398 mg/dL
What is your recommendation:
A. Increase the insulin dose
B. Decrease the insulin dose
C. Switch to Vetsulin insulin
D. Switch to Detemir insulin
E. Switch to Regular insulin
A. AND C → benefit from a longer lasting insulin but increasing dose is not a wrong choice
What would happen if you administered a drug that inhibits proximal renal tubular reabsorption to a diabetic cat?
A. Clinical signs and disease status would remain unchanged
B. Blood sugar levels would reduce, but PU/PD and other clinical signs would worsen.
C. Blood sugar levels would be unaffected but clinical signs would improve.
D. Blood sugar levels and clinical signs would improve
D. → SGLT2 inhibitors block glucose reabsorption in the proximal tubule, promoting glucosuria.
Which of the following correctly lists insulins by duration of action from shortest to longest?
a) Vetsulin, NPH, Glargine/Lantus
b) Regular, NPH, ProZinc/PZI
c) ProZinc/PZI, Glargine/Lantus, Vetsulin
d) Regular, ProZinc/PZI, Vetsulin
B.
Which of the following insulins SHOULD NOT be used in the at-home management of diabetes mellitus in dogs?
a) NPH
b) Regular
c) ProZinc
d) Vetsulin
B.
Which of the following monitoring tests SHOULD NOT be used when making a decision to increase an insulin dose?
a) Freestyle Libre monitoring system
b) Fructosamine
c) Blood glucose curve
d) Spot blood glucose sample
d.
Which of the following is an expected complication in the majority of dogs diagnosed with diabetes mellitus?
a) Diabetic coma
b) Cataract formation
c) Progressive renal failure
d) Limb amputations
b.
Bear, a 4-year-old spayed female mixed breed dog (6.8 kg), presents with acute onset of lethargy, incoordination, and two presumed grand mal seizures.
She has a 4-month history of diabetes mellitus and is currently receiving NPH insulin 9 U BID and is fed Hill’s w/d.
On presentation, her mentation is dull, and her spot blood glucose is 29 mg/dL.
What is the most appropriate next step in management?
A. Dextrose bolus, in-hospital treatment with IV fluids with 2.5–5% dextrose supplementation
B. Dextrose bolus, monitor BGs for 2–4 hours, discharge if BG > 80 mg/dL
C. No dextrose bolus, but hospitalize on IV fluids with 2.5–5% dextrose supplementation
D. Apply Karo syrup to gums, no additional treatment if BG normalizes
A.
What is the best method to document PU/PD?
A. Owner’s assessment of water intake
B. Quantify water intake
C. Evaluate urine specific gravity
D. All of the above
E. None of the above
B.
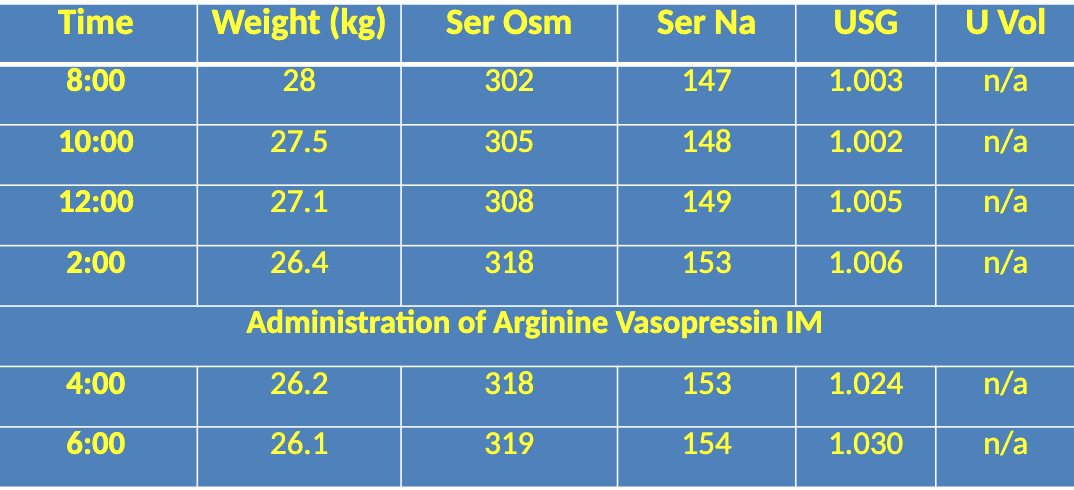
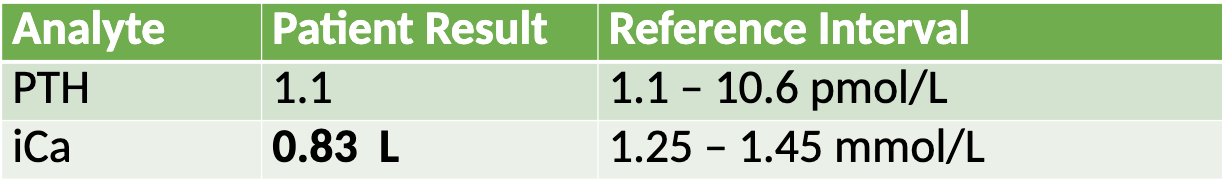
Interpret this water deprivation test
A. Central DI
B. Nephrogenic DI
C. Psychogenic DI
D. Equivocal
A.
The metabolic acidosis in a dog with DKA is most consistent with?
A. Endogenous acid production
B. Exogenous acid consumption
C. Gastrointestinal bicarb loss
D. Renal bicarb loss
A.
Which statement about DKA is true?
A. DKA occurs more commonly in dogs than cats
B. DKA is most common in animals that are already receiving insulin therapy as opposed to newly diagnosed diabetics
C. DKA is more common in females than males
D. DKA can often be managed on an out- patient basis to decrease client costs
A.
Which of the statements is true concerning the management of DKA?
a) Hospitalization costs often exceed $2500 when treating DKA.
b) Most dogs can be managed on an outpatient basis with minimal care.
c) Insulin therapy is not needed in some dogs.
d) Less than 25% of dogs diagnosed with DKA survive.
A.
Which of the following is a correct list of differentials for hypoglycemia?
a) Sepsis, Cushing’s disease, xylitol toxicity
b) Addison’s disease, liver failure, sepsis
c) Insulin overdose, smooth muscle tumors of the GI tract, hypothyroidism
d) Liver failure, xylitol toxicity, ethylene glycol toxicity
B.
Which of the following would be a clue that a dog has primary PU as opposed to primary PD?
a) Mild increase in plasma sodium concentration
b) Frequent need to go outside and urinate
c) A urine specific gravity of 1.012
d) Mild decrease in plasma potassium concentration
A.
How should DDAVP be administered for the initial treatment of central diabetes insipidus?
a) In the conjunctival sac
b) As a nasal mist
c) As a SQ injection
d) By mouth
A.
What is the net effect of PTH on Ca and P?
Increase Ca and decrease P
You are investigating a increased serum total calcium on a patient and decide to measure iCa which comes back increased, what is your next step?
Measure PTH
Name the most common clinical signs seen with hypercalcemia
PUPD
Anorexia
Lethargy
Weakness
Maggie, 16yo miniature Dachshund, Wellness exam, no clinical signs, Bloodwork: ↑TCa, ↓P
What is your diagnosis?
A. Primary hyperparathyroidism
B. Parathyroid-independent hypercalcemia
C. Hypercalcemia of malignancy
D. Idiopathic hypercalcemia
E. These are equivocal results
A.
Bloodwork findings for Primary hyperparathyroidism
Increased T/iCa
Normal or increased PTH
Normal or decreased P
Post-surgical parathyroidectomy, why is hypocalcemia a concern?
A. The patient typically doesn’t feel well, doesn’t eat after surgery
B. The remaining non-adenomatous PTG are atrophied
C. There is a compensatory drop in 25-hydroxyvitamin D after surgery
D. There is typically immune-mediated destruction of remaining PTG
B.
In primary hyperparathyroidism, what is the most likely explanation for the low phophorus?
A. Decreased dietary intake due to malaise from 1HPTH
B. Loss through the gut due to reduced calcitriol production
C. Enhanced renal excretion of phosphorus due to increase PTH
D. Increased bone deposition due to increase PTH
C.
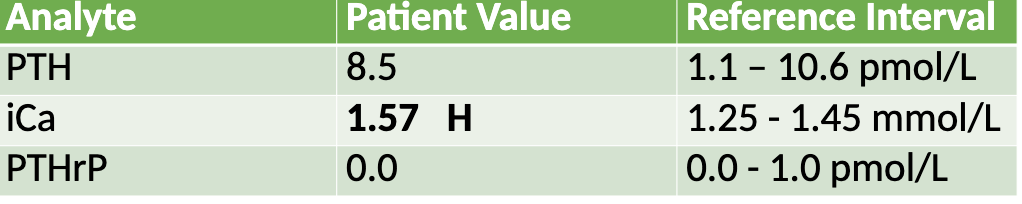
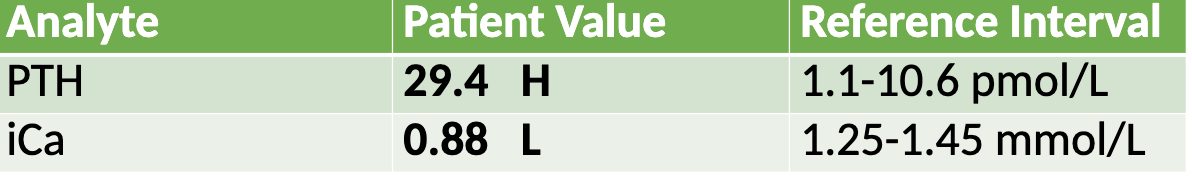
Apollo, 11yo CM Siberian Husky, 3-year history of ionized hypercalcemia, PU/PD for last 1.5 years
What is your diagnosis?
A. Primary hyperparathyroidism
B. Parathyroid-independent hypercalcemia
C. Hypercalcemia of malignancy
D. Idiopathic hypercalcemia
E. These are equivocal results
A. → PTH in upper-end of normal, chronic hypercalcemia
What would you measure to rule-out hypercalcemia of malignancy?
A. iCa
B. PTH
C. PTHrP
D. Calcitriol
C.
Name common malignancies that would cause hypercalcemia
Lymphoma (dogs/cats)
AGASACA (dogs)
Various carcinomas (dogs/cats)
A dog with confirmed hypercalcemia of malignancy has the following lab findings:
↑ PTHrP
↓ PTH
↑ ionized calcium
↑ phosphorus
Worsening azotemia
Which of the following best explains the elevated phosphorus in this patient?
A. PTHrP stimulates phosphorus reabsorption
B. The tumor is producing phosphorus directly
C. Renal dysfunction is decreasing phosphorus excretion
D. Hypercalcemia directly increases phosphorus levels
C.
A dog presents with polyuria and polydipsia and is found to have elevated ionized calcium. Which of the following best explains why hypercalcemia leads to PU/PD?
A. Hypercalcemia stimulates excess aldosterone production, increasing urine output
B. Hypercalcemia causes osmotic diuresis by increasing glucose filtration
C. Hypercalcemia impairs ADH function, leading to nephrogenic diabetes insipidus
D. Hypercalcemia increases aquaporin-2 expression, reducing water loss
C.
Quinn, 8yo FS DSH cat
• History of chronic weight loss
• Only abnormality on bloodwork = hypercalcemia
• Ultrasound – no significant findings
What might you suspect, based upon history/labs?
A. Parathyroid-independent hypercalcemia
B. Hypervitaminosis D
C. Hypercalcemia of malignancy
D. Idiopathic hypercalcemia
E. These are equivocal results
D.
What would be your first treatment of choice with a diagnosis of idiopathic hypercalcemia in cats?
A. High fiber diet
B. Alenodrate once a week
C. Prednisolone
D. Alenodrate with Prednisolone
A.
A 5-year-old mixed-breed dog presents with lethargy, vomiting, and polyuria. Bloodwork shows:
Total calcium: 14.5 mg/dL (↑)
Ionized calcium: mildly increased
Phosphorus: normal
Na:K ratio: 22:1
Creatinine: mildly elevated
PTH: normal
Calcitriol: normal
Which of the following is the most likely cause of this dog’s hypercalcemia?
A. Primary hyperparathyroidism
B. Vitamin D toxicosis
C. Addison’s disease (hypoadrenocorticism)
D. Hypercalcemia of malignancy
C.
What is the net effect of Vit D on Ca and P?
Increases C and P
How does the FGF-23/Klotho complex regulate calcitriol (active vitamin D) levels in the body?
A. By stimulating 1α-hydroxylase and inhibiting 24-hydroxylase
B. By stimulating both 1α-hydroxylase and 24-hydroxylase
C. By inhibiting 1α-hydroxylase and stimulating 24-hydroxylase
D. By blocking intestinal absorption of vitamin D
C.
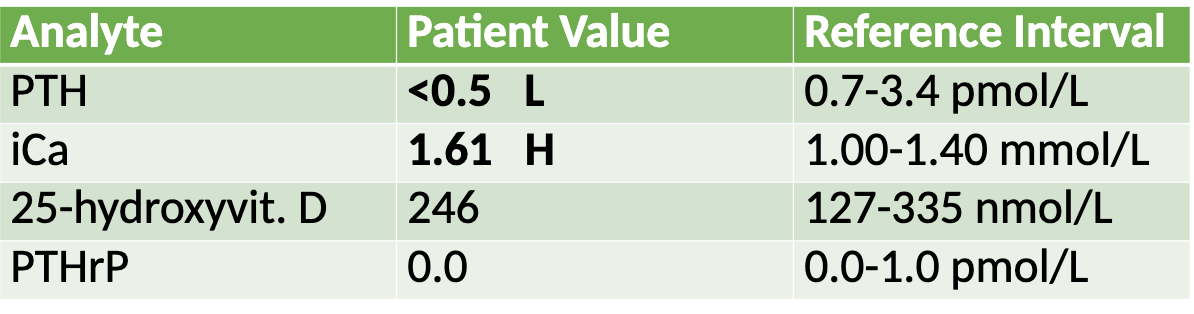
Hank, 5yo Miniature Schnauzer
• ~2-week history of muscle twitching, lifting of L front leg
• ↓TCa 6.1 mg/dL (8.9 – 11.4 mg/dL)
• ↑P 7.6 mg/dL (2.5 – 6.0 mg/dL)
What is your diagnosis?
A. Primary hyperparathyroidism
B. Primary hypoparathyroidism
C. Renal 2HPTH
D. Nutritional 2HPTH
E. These are equivocal
B.
Daisy, 10yo FS Chihuahua
• Chronic weight loss, intermittent vomiting, hyporexia
• Progressive non-regenerative anemia, azotemia, hypocalcemia (total
and ionized), marked hyperphosphatemia
What is your top differential diagnosis?
A. Primary hypoparathyroidism
B. Renal 2HPTH
C. Nutritional 2HPTH - dietary insufficiency
D. Nutritional 2 HPTH - GI disease/malabsorption
B.
Which of the following is true regarding parathyroid hormone (PTH)?
A. PTH production is inhibited by high total calcium
B. PTH directly stimulates intestinal calcium uptake
C. PTH promotes renal tubular calcium reabsoption
D. PTH inhibits renal formation of calcitriol
C.
__________ is the most reliable indicator of overall vitamin D status, while _________ is the most bioactive naturally occurring metabolite.
25-OH-D, calcitriol
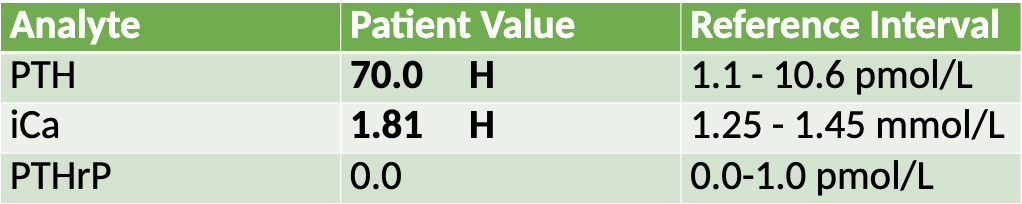
"Sparty" is a 14-year-old CM English Springer Spaniel dog who presented for routine bloodwork. High total calcium (14.7 mg/dL) and low phosphorus (2.4 mg/dL) were the only abnormalities. Below are his endocrinology results:
Analyte | Patient Value | Reference Interval |
Parathyroid Hormone (PTH) | 8.2 | 1.1 – 10.6 pmol/L |
Ionized Calcium (iCa) | 1.67 H | 1.25 – 1.45 mmol/L |
Parathyroid Hormone Related Protein (PTHrP) | 0.0 | 0.0 – 1.0 pmol/L |
What is your diagnosis?
A. Idopathic hypercalcemia
B. Hypercalcemia of malignancy
C. Primary hyperparathyroidism
D. Equivocal resutls
C.
Which of the following reflects the expected underlying pathophysiology in chronic kidney disease (P = phosphorus, FGF-23 = fibroblast growth factor-23)?
A. ↑P → ↑FGF-23 → ↓calcitriol → ↓iCa → ↑PTH
B. ↓P → ↑FGF-23 → ↑calcitriol → ↓iCa → ↑PTH
C. ↑P → ↑FGF-23 → ↓calcitriol → ↑iCa → ↓PTH
D. ↓P → ↓FGF-23 → ↑calcitriol → ↑iCa → ↓PTH
A.
What cell in the pancreas produces insulin and amylin?
Beta-cell in the Islets of Langerhans
What is glucotoxicity in the context of feline diabetes mellitus?
Cellular damage in beta cells due to sustained high glucose levels, leading to hydropic degeneration and apoptosis
Which of the following is FALSE about feline diabetes mellitus?
A) Obesity is a major risk factor due to its role in insulin resistance
B) Diabetic remission is possible with early and aggressive management
C) Diet is an integral part of disease management
D) Cats are unable to go into remission and will be diabetic for life
D
List the 4 cardinal signs of DM in dogs and cats
PU
PD
Polyphagia
Weight loss
Which of the following is recommended during the initial evaluation of a cat or dog newly diagnosed with diabetes mellitus (DM)?
A) Abdominal ultrasound
B) Serum fructosamine
C) Urine culture
D) ACTH stimulation test
C.
Criteria necessary to establish a diagnosis of DM
Do they have the 4 consistent clinical signs?
Do they have concurrent fasted hyperglycemia and glycosuria?
Name alternative diabetic monitoring options for cats who are prone to stress hyperglycemia
Owners get urine at home
Measure fructosamine
Preferred diets for DM: dogs vs cats
Dogs: Low carbs, high fiber, avoid simple sugars
Cats: Low carbs, high protein
Which of the following is a possible complication of diabetes mellitus (DM)?
A) Pancreatitis
B) Otitis externa
C) Tracheal collapse
D) Hypothyroidism
A.
T/F: If you are consistently getting negative glucose on urine dipstick, this means you are over treating
False → may not always mean this, but paired with clinical signs and values of hypoglycemia then yes
How can you utilize fructosamine to monitor DM?
Measures average blood glucose concentration over previous 2-3 weeks
Not ideal in the initial monitoring phase
Fractious kitties?
Which of the following would NOT be an appropriate indication to perform a glucose curve in a diabetic patient?
A) 7–14 days after changing the insulin dose
B) When hypoglycemia is suspected
C) At least four times per year for routine monitoring
D) After first dose of new insulin
E) All of these are appropriate indications
E.
A diabetic dog receiving NPH insulin presents with persistent PU/PD and weight loss. A glucose curve shows values above the reference interval from 8–10 am, a drop below 50 mg/dL at 12 pm, followed by elevated glucose levels for the rest of the day. What is the most appropriate next step in management?
A) Increase the dose of NPH insulin
B) Add a second insulin injection in the evening
C) Switch to Vetsulin for longer duration of action
D) Decrease food intake to reduce postprandial glucose
C.
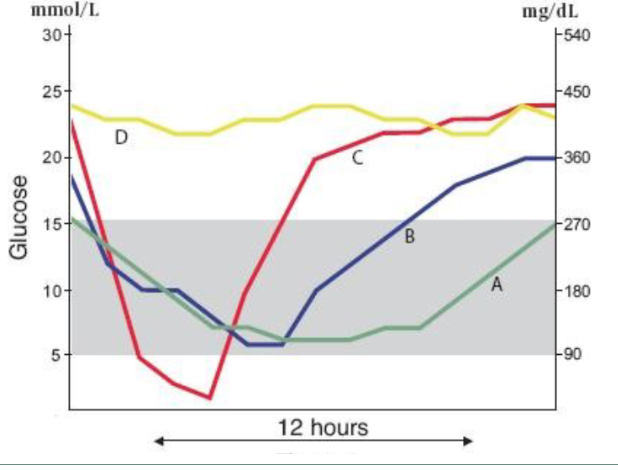
Match the glucose curve results with the appropriate management protocol:
1. Ideal
2. Increase insulin dose
3. Needs a longer acting insulin
4. Decrease insulin dose ± change insulins
A. 1.
B. 3. OR could leave alone if no clinical signs present
C. 4.
D. 2.
T/F: Canned friskies is an appropriate diet for a diabetic cat
True
Indications to change insulin types include
Insulin >1.5 U/kg BID in dogs, 5 U/kg BID in cats
Unacceptable nadirs with poor overall control
Insulin >2 U/kg BID in dog with unaddressed insulin resistance
What patient population is Bexacat (SGLT2 inhibitor) recommended for management of DM?
Newly diagnosed, clinically stable
No comorbidities
Never have used insulin
Describe the pathogenesis of DKA
Lack of insulin or poor regulation
Decreased glucose utilization and increased glucose production
Hyperglycemia and glycosuria
Solute diuresis and dehydration
Recruitment of alternate energy sources (fat and protein)
Ketone production exceeding buffering capacity → ketoacidosis
Chemistry findings that are common in DKA
Hyperglycemia
Ketosis
Metabolic acidosis with a high anion gap
Electrolyte abnormalities
Low sodium, phosphorus and magnesium
Elevated liver enzymes
What is the major circulating ketone in DKA?
B-hydroxybutyrate
Which of the following fluids would NOT be appropriate for DKA management?
A. LRS
B. Norm-R
C. Plasmalyte
D. 0.45% saline
D.
Which of the following is the MOST priority treatment in the stabilization of DKA?
A. IVF therapy
B. Potassium supplementation
C. Initiating insulin
D. Central line placement
A.
How does the treatment and prognosis of Hyperosmolar Hyperglycemic State differ from Diabetic Ketoacidosis in diabetic dogs?
HHS patients have low-level insulin that prevents ketosis but not hyperglycemia
Treatment is similar to DKA but must be done more slowly, with gradual glucose reduction over 24 hours
Prognosis is more guarded to poor due to neurologic signs and concurrent disease.
Hypoglycemia is characterized by what value?
Persistent < 50-60 mg/dl
Which of the following is incorrectly matched causes for hypoglycemia?
A. Artifact due extreme leukocytosis
B. Iatrogenic due to incorrect insulin administration
C. Decreased glucose production due to sepsis
D. Decreased glucose production due to transient juvenile hypoglycemia
E. Excess insulin due to insulinoma
F. Ethanol toxicity blocking gluconeogenesis
C. → excess glucose consumption NOT production
Neuroglycopenia is a clinical sign at what glucose level?
< 45 mg/dl
What is the most common islet-cell neoplasia in dogs?
B-cell neoplasia → insulinomas
T/F: Insulinomas are almost always malignant
True → almost 100% of patients have mets
Long-term management of insulinoma includes:
Surgical resurrection
Dietary modifications: small, frequent meals, high proteins, fat and complex cars, avoid simple sugars
Prednisone
4 major categories of diseases that can result in PUPD
Osmotic diuresis
DM
Medullary washout
CKD
Central diabetes insipidus
Lack of ADH
Nephrogenic diabetes insipidus
Renal insensitivity to ADH
What is the biggest stimulator of antidiuretic hormone (ADH) release?
Changes (increased) in plasma osmolality
What is the primary action of antidiuretic hormone (ADH)?
A. Increases sodium excretion in the proximal tubule
B. Stimulates aldosterone release to retain sodium
C. Promotes water reabsorption in the collecting ducts
D. Inhibits renin release from the juxtaglomerular apparatus
E. Enhances glucose reabsorption in the proximal tubule
C.
What is the cause of Central Diabetes Insipidus (DI)?
A. Deficiency of antidiuretic hormone (ADH) due to damage to the hypothalamus or pituitary gland
B. Resistance to ADH in the kidneys, leading to decreased water reabsorption
C. Excess secretion of ADH, causing water retention
D. Increased production of aldosterone, leading to excessive sodium reabsorption
A.
What is the most common cause of central DI?
Primary pituitary neoplasia
Name drugs/molecules/electrolytes that can antagonize the effects of ADH
Glucocorticoids
Electrolyte abnormalities
E. coli endotoxin
Phenobarbital
Less commonly: infections, neoplasia
T/F: With primary PD, there will be a subclinical dehydration, increased Hct, and isosthenuric urine
False → primary PU
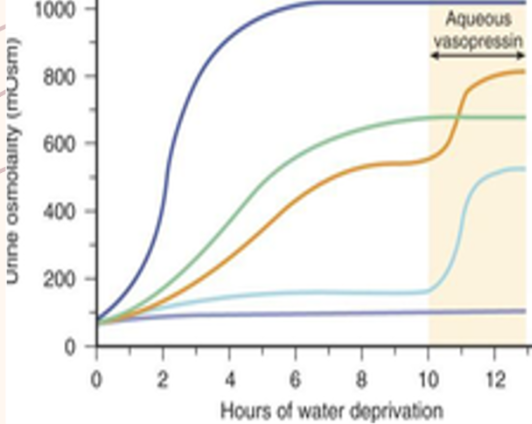
Match the water deprivation test results with the diagnosis:
Dark blue
Light blue
Purple
Psychogenic
CDI
NDI
*orange and green are partial
What is a safer alternative to water deprivation test in cats?
DDAVP trial → caution with possibility for water intoxication due to promoting reabsorption of free water
Most important medical treatment for dogs with CDI?
Desmopressin acetate
Most common clinical signs of hypercalcemia in dogs
PUPD
Anorexia
Lethargy/weakness
Why is PU/PD a common clinical sign of primary hyperparathyroidism?
Hypercalcemia causes autophagy of aquaporin-2 channels, reducing renal response to ADH
What is the preferred treatment for primary hyperparathyroidism?
Surgical parathyroidectomy
Biochemistry pattern with hypercalcemia of malignancy
High Ca with low to normal PTH and P
PTHrp increased
T/F: Hypercalcemia in Addison’s disease in mostly mild to moderate
True
Biochemistry pattern seen in Vitamin D toxicosis
Increased T/iCa and decreased PTH with high P in many cases
Canine schistosomiasis infection can cause:
A. Hypocalcemia
B. Hypercalcemia
C. Hyperkalemia
D. Hypophosphatemia
E. Hyponatremia
B,
Most clinical signs of hypocalcemia are associated with:
neuromuscular system
Which of the following clinical signs is NOT seen with hypocalcemia?
A. Muscle fasciculations, tremors
B. Oral chomping
C. Hypersensitivity
D. Vomiting
E. Aggressive
D.
Biochemistry pattern for primary hypoparathyroidism
Decrease t/iCa with normal to low PTH, normal to high P
T/F: Treatment of primary hypoparathyroidism includes administration of 10% calcium gluconate SQ
False - NEVER give calcium SQ!
How does AKI cause hypocalcemia?
Due to high levels of P
Decreased P excretion = ↑ Phosphorus + ↓ Renal response to PTH = Hypocalcemia in AKI
Biochemical pattern for secondary hyperparathyroidism
Increased PTH with normal to decreased iCa
Biochemical pattern for nutritional secondary hyperparathyroidism
Increased PTH, decreased iCa, decrease calcidiol
Which of the following statements best describes Type 2 vitamin D–dependent rickets in dogs and cats?
A. It is caused by a defect in 1α-hydroxylase, leading to decreased calcitriol levels
B. It results in low calcidiol and low calcitriol levels
C. It is due to a vitamin D receptor defect, leading to high calcitriol but impaired function
D. It has a better prognosis than Type 1
E. It is an autosomal dominant inherited disorder
C.
What is the primary mechanism leading to increased parathyroid hormone (PTH) in renal secondary hyperparathyroidism?
Decreased GFR causes phosphorus retention → ↑ serum phosphorus → ↓ calcitriol (via inhibition of 1α-hydroxylase and FGF-23) → ↓ ionized calcium → ↑ PTH.
Which of the following clinical or radiographic signs is most consistent with advanced renal secondary hyperparathyroidism?
A. Calcinosis cutis
B. Urolithiasis
C. Floating teeth on dental radiographs
D. Ascites
E. Petechiation
C.