The Digestive System
1/67
Earn XP
Description and Tags
Flashcards about the key components, functions, and processes of the digestive system, including the gastrointestinal tract (GIT) and accessory organs.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
Components of the Digestive System (Major (hollow) organs)
. Oral cavity & Pharynx
• Oesophagus
• Stomach
• Small Intestine
• Large Intestine, inc. rectum & anus
Components of the Digestive System (Accessory Organs)
Teeth & Tongue
• Salivary Glands
• Liver
• Gallbladder
• Pancreas
Functions of the Digestive System
The digestive system converts food into its simplest
components to be absorbed into the bloodstream or excreted
as waste It does this via: Ingestion, Mechanical digestion, Chemical digestion, Absorption, Elimination
Ingestion
Entry of food/liquids into the digestive tract via the oral cavity
Mechanical digestion
Crushing/shearing of ingested food
Chemical digestion (extraction of nutrients)
Enzymatic breakdown of food into substances that can be absorbed
Absorption
Movement of nutrients into the bloodstream
Elimination
Indigestible food is compacted into faeces and is excreted
Components of The Upper GIT (food breakdown)
Mouth / oral cavity
• Oesophagus
• Stomach
• Small intestine (duodenum only)
The Lower GIT (absorption, waste
compaction and excretion)
Small intestine (jejunum and ileum)
• Large intestine, inc. rectum & anus
Functions of the Accessory Digestive Organs: Teeth & Tongue function
Crushing/shearing of food and shaping of food into bolus
Functions of the Accessory Digestive Organs: Salivary glands function
Secretion of enzyme (amylase) to begin breaking down carbohydrates
Functions of the Accessory Digestive Organs: Liver function
Secretion of bile to breakdown fats, detoxification of the blood, storage of iron, glucose and fat-soluble vitamins
Functions of the Accessory Digestive Organs: Gallbladder function
Storage of bile
Functions of the Accessory Digestive Organs: Pancreas function
Secretion of pancreatic enzymes to breakdown protein, fat and carbohydrates
Oral cavity digestion
Mechanical digestion (mastication) and mixing of food with saliva; enzymes in saliva begin the process of chemical digestion
Oesophagus digestion
A fibromuscular tube that transfers food (bolus) into the stomach
Stomach digestion
Chemical digestion: Bolus is mixed with gastric juices
(hydrochloric acid and digestive enzymes)
• Mechanical churning: Facilitates digestion, Bolus is converted into chyme
Small intestine (duodenum) digestion
Chemical digestion: Aided by digestive juices from the pancreas and gallbladder
Small intestine (jejunum and ileum) digestion
Where the bulk of chemical digestion and nutrient absorption occurs
Large intestine function
Cecum, ascending colon, transverse colon,
descending colon Reabsorption of water & some nutrients; compacts waste (faeces) for elimination
Rectum & anus function
Stores and eliminate waste (faeces)
General Structure of the GIT Wall Layers
From inside to out: Mucosa, Submucosa, Muscularis externa, Serosa/Adventitia
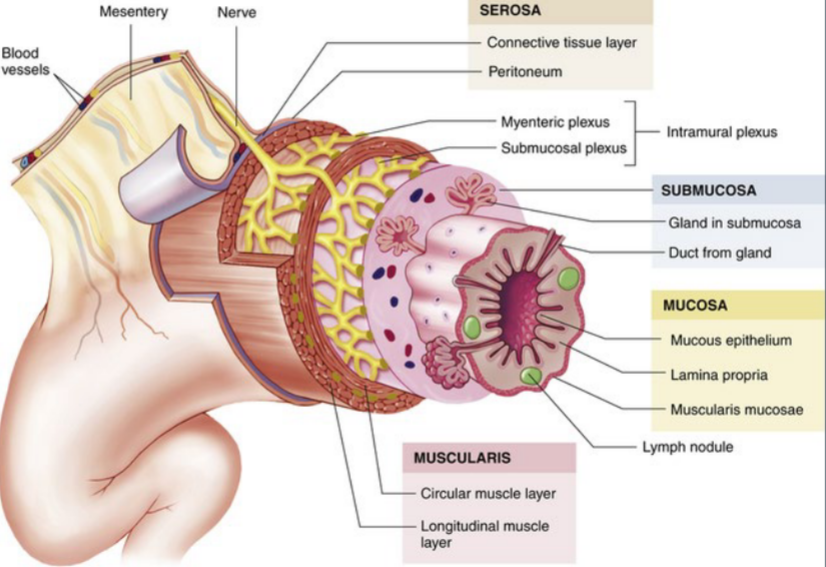
Mucosa
Innermost structure of the GIT wall consisting of three sublayers: epithelium, lamina propria, and muscularis mucosa
The Mucosa: 1. Epithelium
Stratified squamous (for protection): Mouth, oesophagus, rectum & anus;
Simple columnar (absorption): Stomach, small intestine & large intestine
Specialised epithelial structures in the GIT:
• Goblet cells: Secrete mucous to keep the
epithelium moist
• Microvilli: In the small intestine to increase
surface area for nutrient absorption
The Mucosa: 2. Lamina propria
Loose connective tissue that is a route by which nutrients are absorbed and supports epithelium
Contains:
• Cells, e.g. fibroblasts and macrophages
• Blood vessels
• Sensory nerve endings
• Lymphatic vessels
• Some mucous glands
• Mucosa-associated lymphatic tissue (MALT): protection
against infection
The Mucosa: 3. Muscularis mucosa
Thin layer of smooth muscle that causes folds to form in the mucosal layer, increasing local movements and absorption of nutrients
Submucosa
Loose connective tissue that provides physical support to the mucosa and connects it to the underlying muscularis externa
Contains:
• Large blood vessels
• Submucosal glands
• Large lymphatic vessels
• Submucosal (Meissner’s) plexus
• Sensory neurons and autonomic nerve fibres that innervate
the glands
• Stimulates secretion from glands
Submucosal (Meissner’s) plexus
Network of sensory neurons and autonomic nerve fibres that innervate the glands and stimulates secretion from glands
Muscularis Externa
Multiple muscle layers organized in circular and longitudinal layers that are essential for mechanical processing and moving materials along the GIT. Composition depends on location within the GIT:
The Muscularis Externa layer: Oesophagus
Contains inner circular and outer longitudinal layers
of muscle. Upper third is skeletal muscle (voluntary), while the rest
is smooth muscle (involuntary)
The Muscularis Externa layer : Stomach
Contains inner oblique, middle circular and outer
longitudinal layers of smooth muscle
The Muscularis Externa layer: Small and large intestines & rectum
Contains inner circular and
outer longitudinal layers of smooth muscle
The Muscularis Externa layer: Anus
Contains inner circular and outer longitudinal layers of
skeletal muscle (voluntary)
The Muscularis Externa also contains Myenteric plexus (Auerbach plexus)
Network of sensory neurons + autonomic nerve fibres located between the circular and longitudinal muscle layers that coordinates digestive muscle activity
Serosa
Outermost layer of GIT organs within the abdominopelvic cavity, continuous with the peritoneum, i.e. distal oesophagus, stomach and intestines. Composed of Loose connective tissue. Covered in serous fluid to prevent friction and allow movement
Adventitia
Outermost layer of GIT organs that lie outside of the abdominopelvic cavity, i.e. majority of the oesophagus and the anus. Composed of Dense (fibrous) connective tissue that anchors the organ in place
structure of GIT links to function
Function: Protection from abrasion
• Stratified squamous epithelium in the oesophagus and anus
Function: Vigorous mixing (mechanical disruption)
• Oblique muscle layer within the stomach
Function: Efficient absorption
• Simple columnar epithelium with microvilli in the small intestine
Oesophagus
Muscular tube that transports food (bolus) from mouth to stomach Runs posteriorly to the trachea
• Approx. 25cm long
• Contains upper and lower oesophageal sphincters
Upper oesophageal sphincter
At junction of pharynx and oesophagus; prevents airflow into oesophagus and also reflux of food into airway
Lower oesophageal sphincter
At gastro-oesophageal junction; controls entry of bolus into stomach and prevents backflow of gastric juice
Layers found in the Oesophagus
1. Mucosa
• Stratified squamous epithelium for protection
• Contains large folds that keep the lumen closed unless
swallowing is occurring, and allow for expansion when swallowing
2. Submucosa
• Large mucus glands for lubrication and to facilitate transport
3. Muscularis Externa
• Upper third is skeletal muscle (swallowing is voluntary)
• Middle third is a combination of skeletal and smooth muscle
• Lower third is smooth muscle
• 4. Adventitia*
• Connective tissue layer anchoring majority of the oesophagus to neighbouring structures
• *except distal portion, which is serosa
Stomach
Expandable muscular organ that stores food and mechanically and chemically breaks down food. Four anatomical regions: Cardia, Fundus, Body, Pylorus
Stomach contains: Rugae
Folds of the mucosa & submucosa that allow expansion of the stomach
Stomach Contains two sphincters: Pyloric sphincter
Distal end of the stomach that prevents early discharge of stomach contents
Stomach Contains two sphincters: Lower gastro-oesophageal sphincter
Controls entry of bolus into stomach and prevents backflow of gastric juice
Stomach layers
Mucosa
• Simple columnar epithelium
• Produces a layer of mucous for protection against gastric juices, and defence
• Contains deep folds that form gastric glands (contain
gastric pits)
• Contains numerous secretory cells that produce gastric
secretions
2. Submucosa
3. Muscularis Externa
• Inner oblique layer: Responsible for creating the churning motion to aid mechanical breakdown of food
• Middle circular layer
• Outer longitudinal layer: Responsible for moving the bolus
towards the pylorus (through muscular shortening)
4. Serosa
Stomach: Gastric Glands
Gastric glands open into the stomach through gastric pits in the mucosa. They secrete most of the acid and enzymes required for chemical digestion in the stomach. Contain specialised cells: The composition of these cells depends on the gland’s
location within the stomach
Specialised Cells in the stomach’s gastric glands: Mucous Cells
Secrete mucous and bicarbonate ions (alkaline) to protects stomach wall from damaging effects of gastric acid (hydrochloric acid: HCl), Prominent in the gastric pit and neck of gastric glands
Specialised Cells in the stomach’s gastric glands: Parietal Cells
Secrete hydrogen (H+) and Chloride (Cl-) ions that combine to form HCl. Kills microbes & denatures proteins
• Secrete intrinsic factor, which is necessary for Vitamin B12 absorption (in the small intestine)
• Located in upper regions of gastric glands
Specialised Cells in the stomach’s gastric glands: Chief Cells
Secretes pepsinogen (inactive), which is converted to pepsin (active) by HCl. Pepsin degrades proteins. Secretes gastric lipase, which breaks down lipids
• Located in lower regions of gastric glands
Specialised Cells in the stomach’s gastric glands: Enteroendocrine Cells
Produces and releases the hormone gastrin to Increases stomach motility, stimulates HCl/enzyme production, and Relaxes the pyloric sphincter
• Located at the base of gastric glands
what the stomach absorbs
The stomach doesn’t play a big role in absorption of food, but it
can absorb:
• Water (especially when dehydrated)
• Electrolytes
• Some drugs (especially aspirin)
• Alcohol
Small Intestine
Longest portion of the GIT (approx. 3-5 metres) and is the site of most enzymatic digestion & absorption Three anatomical regions:
• Duodenum: Approx. 5%
• Jejunum: Approx. 40%
• Ileum: Approx. 60%
Small Intestine layers
Mucosa
• Simple columnar epithelium
• Produces a layer of mucous for protection against acidic chyme, and defence
• Contains a series of finger-like projections called villi
2. Submucosa
3. Muscularis Externa
• Inner circular layer
• Outer longitudinal layer
4. Serosa
Small Intestine: Types of Movement: Segmentation
Local mixing of chyme with intestinal juices; repeated, involuntary contraction/relaxation (sloshing back & forth) of the inner circular muscularis externa layer; increases exposure time of chyme to absorptive surface
Small Intestine: Types of Movement: Peristalsis
Involuntary contraction/relaxation of both muscularis externa layers that propels chyme onwards through the tract
Large surface area of small intestines is achieved through: Plica circularis
Permanent folds within the mucosa. Present only until the mid-section of the ileum and submucosa that can’t stretch out like rugae (stomach)
Large surface area of small intestines is achieved through: Villi
The surface of the plicae circulares (pl.) contains small vascularised projections of mucosa
Large surface area of small intestines is achieved through: Microvilli
Cell surface feature sometimes referred to as a ‘brush border’
Specialised Cells of Small intestines: Enterocytes
Tall columnar cells at the top it contain brush border of microvilli and Absorb nutrients Secrete enzymes to aid in breakdown
of macronutrients for easier absorption
• Found across the entire surface of a villus
Specialised Cells of Small intestines: Goblet Cells
Produce mucins, which function to protect against highly acidic contents and to provide lubrication of the lining of the GIT, scattered between enterocytes
Specialised Cells of Small intestines: Enteroendocrine Cells
Secretes variety of hormones and aids in GIT motility, gastric emptying & mechanical digestion Located within the intestinal crypts
Specialised Cells of Small intestines: Paneth Cells
Contain the enzyme lysozyme with Antibacterial activity, Located in base of intestinal crypts (between villi)
Large Intestine
Approx. 1.5 metres in length, Site of absorption of water & salt, and
chyme conversion into faeces
Approx. 90% of water within chyme is reabsorbed
Extensive action of gut microflora (chemical digestion via bacteria)
Four anatomical regions:
• Caecum
• Colon (four regions)
• Rectum
• Anal canal/anus
Large Intestine layers
Mucosa
• Simple columnar epithelium (caecum and colon)
• Stratified squamous epithelium (rectum and anus)
• Mucosa drops down into intestinal glands that contain a lot of goblet cells for lubrication
2. Submucosa
3. Muscularis Externa
• Inner circular layer
• Outer longitudinal (incomplete) layer
• Arranged into ‘ribbons’ called taeniae coli
• Taeniae coli contract and gather the colon into a series of pouches known as haustra
4.Serosa*
• *except anus, which is adventitia
Absorption & Faeces Formation
Site of final absorption of water and salt (within the ascending colon) Remaining components are converted into faeces
• Faeces are semi-solid by time reaches transverse colon
• Components of faeces:
• Dead epithelial cells
• Undigested food, e.g. cellulose
• Bacteria
• Mucous
Control of the Digestive System
Both the nervous system and the endocrine system
control digestive processes
• The brain controls the responses of hunger and
satiety, via the ‘feeding centre’ and ‘satiety centre’
respectively, within the hypothalamus
• The endocrine system controls various glands and
the release of hormones and enzymes required for
digestion of food in the digestive tract, e.g. gastrin
and motilin