Vitamins Clinical Chemistry
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
source and occurrence
Vitamin = Vital for Health
Organic compounds required in trace amounts
Necessary for normal metabolic functions, health and
growth
Vegetable or animal sources or can be synthesized
Function as cofactors for enzymatic reactions
Metabolically converted to a functional form
Vitamins categories, water soluble and fat soluble
vitamin deficiencies
Decreased Intake:
◦ malnutrition, starvation, alcoholism
Malabsorption:
◦ B12 and Folic acid deficiencies, gastrectomy
Malnutrition:
◦ Alcoholism, poverty, famine
Increased Requirements:
◦ infection, pregnancy, lactation, cancer, exercise
water soluble vitamins
As the name implies, these are soluble in aqueous medium
They are absorbed without the involvement of bile salts
They are not stored in the fat droplets
Water solubility allows them to be rapidly cleared by the
kidneys and excreted in the urine
For this reason, toxicity is rarely a problem
water soluble vitamins
B1 Thiamine
B2 Riboflavin
B3 Niacin
B5 Pantothenic acid
B6 Pyridoxine
B12 Cobalamine
C Ascorbic acid
H Biotin
M Folic Acid
fat soluble vitamins
A Retinol
D Calciferols
E Tocopherols
K Phylloquinones (Prothrombin factor)
thiamine B1
Functions:
Thiamine pyrophosphate is the biochemically active ester of
thiamine, involved in many important metabolic processes
including:
The decarboxylation of alpha-oxoglutaric acid in the citric
acid cycle
The conversion of alanine to pyruvic acid then to acetyl
coenzyme A
Active form, thiamin pyrophosphate (TPP)
Is essential for the releasing of energy from carbohydrate and
fat
Also involved in conduction of nerve impulses.
B1 deficiency
Principle Food Sources:
◦ Meats
◦ Whole grain cereals (present in the germ of the grain)
◦ Eggs
◦ Nuts
◦ Legumes
Results from inadequate intake of non enriched grains,
◦ Decreased intake, impaired absorption, increased requirements.
Deficiency: Beriberi (I can’t, I can’t)
◦ A disorders of the nervous and cardiovascular system
◦ Fatigue, peripheral neuritis, intelligence disturbance, double vision, drooping
eyelids, loss of recent memory
◦ Seen in underdeveloped countries or in the US from malnutrition
◦ Alcoholism (one of leading causes in US)
◦ Impaired absorption, diabetes, cancer and dialysis patients.
thiamine, B1 meausrement
◦ HPLC with UV detection
◦ Normal Serum concentrations: 0.2 to 0.43 ug/dl
◦ Best measured as whole blood
◦ Erythrocyte transketolase activity (ETK)
◦ Provides a more sensitive measurement of the functional activity
of B1
◦ Involves the measurement of ETK before and after the addition of
TPP
◦ EKT Reference values: 0.75-1.3 IU/g Hgb
riboflavin B2
Is an intermediary the transfer of electrons in the cellular
oxidation-reduction reactions which generate energy from
protein, carbohydrate and fat
The riboflavin coenzymes are also important for the
transformation of vitamin B6 and folic acid into their
respective active forms, and for the conversion of tryptophan
into niacin
Functions as two coenzymes in oxidative enzymatic
reactions:
◦ Flavin mononucleotide (FMN)
◦ Flavin adenine dinucleotide (FAD)
Riboflavin is often used as a colorant because of its bright
yellow color
Principle food sources:
◦ Riboflavin is present in all animal and plant cells
◦ Highest concentrations are in yeast and liver
◦ Milk and milk products, Egg whites, Meats , Leafy green vegetables ,
Egg yolks
Deficiencies:
◦ Known as ariboflavinosis
◦ Associated with alcoholism, poor nutrition, malabsorption and
starvation
◦ Stomatitis (mouth lesions)
◦ Glossitis (magenta tongue)
◦ Blepharospasm (eyelid spasm)
◦ Itching, skin rashes
riboflavin B2 assays
Riboflavin assays measured by HPLC
◦ Serum concentrations Levels are 4 - 24 ug/dl
◦ Urine: > 100 ug/d
Erythrocyte Glutathione (GTH) Reductase activity
◦ A more sensitive indicator of the functional activity of riboflavin
◦ GSH Reductase Activity increases with FAD: 0-20%
◦ Marginal Deficiency: 20-40%
◦ Deficiency: > 40%
Niacin B3 nicotinic acid
Niacin, pyridine nucleotide, nicotinic acid, nicotinamide.
Functions as a component of two coenzymes:
◦ In the blood, brain, kidney and liver it is converted to the coenzymes
nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine
dinucleotide phosphate (NADP)
◦ Involved in the generation of energy in cells
◦ Tryptophan is an amino acid which is a provitamin of niacin
◦ NAD and NADP, which are necessary for many metabolic process
◦ Respiration, fatty acid metabolism, and glycolysis
Dietary requirement can be met in part by the conversion from
tryptophan to niacin
niacin, nicotinic acid, nicotinamide sources and deficiency
Principle sources in food:
◦ Yeast extract, Liver , Meats , Oily fish , Nuts , Legumes , Green leafy vegetables ,
Milk and milk products
Deficiency is Known as Pellagra
◦ Characterized by dermatitis, delirium, and dementia , diarrhea
◦ Nervous disorders which can lead to paralysis of the extremities
◦ Deficiencies result from low levels of dietary niacin and tryptophan, alcoholism and
Hartnup’s disease
Pharmacologic doses of nicotinic acid are given to decrease serum lipid levels
Neither blood or urine levels are of clinical significance in assessing nutrition
pyridoxine B6
Family of pyridoxal phosphates
◦ Pyridoxine, pyridoxal, pyridoxol
Function as coenzyme in trans-amination reactions for AST and ALT
Best known for its role in the conversion of 5-tryptophan to 5-hydroxy
tryptamine (serotonin)
It is needed for:
◦ Metabolism of amino acids
◦ Cellular metabolism of carbohydrate, protein and fat
◦ Formation of neurotransmitters
◦ Production of nicotinic acid (vitamin B3)
pyridoxine deficiency
Principle food sources:
◦ Chicken , Liver , Yeast Extract ,
◦ Fish, particularly: Tuna , Trout , Herring , Halibut , Salmon
◦ Nuts, Whole grains ,
◦ Very few fruit and vegetables: Beans, Cauliflowers, Bananas, Raisins
Deficiencies rarely occur alone
◦ Most commonly seen with several B vitamin deficiencies
◦ Patients at risk are those with malignancy, chronic alcoholics, liver
disease and malabsorption syndromes
◦ Pyridoxine deficiencies are reported to cause dermatitis and
convulsions and a form of Sideroblastic anemia
pyridoxine assays
Assay by HPLC
The functional activity of B6 is measured by erythrocyte aspartate
aminotransferase (AST)
Normal value for B6 is 39% to 89% saturation
vitamin b12 cobalamins
B12 refers to a large family of cobalt containing compounds
These include:
◦ Hydroxocobalamin
◦ Adenosylcobalamin (active coenzyme form)
◦ Methylcobalamin (active coenzyme form)
◦ Cyancobalamin (synthetic form of vitamin B12 that can be transformed by the body
into the active coenzymes)
Intestinal absorption takes place in the ileum
Absorption from the intestine requires a binding protein:
◦ Intrinsic Factor (IF)
◦ Secreted by the parietal cells of the stomach
In 1934, Nobel prize in medicine for discovering the lifesaving properties of
vitamin B12
b12 cobalamine function and food sources
Function:
◦ Like the other members of the B-complex, vitamin B12 is involved in the
cellular metabolism of carbohydrate, protein and fat and in production of:
◦ Blood cells in the bone marrow
◦ Nerve sheaths
◦ Proteins
◦ Necessary for DNA synthesis in hematopoiesis
Principle food sources:
◦ The main dietary sources of vitamin B12 are animal products:
◦ Organ meats
◦ Fish
◦ Eggs
◦ Dairy products
b12 deficiency cause and seen with:
Most common cause:
◦ Deficiency results in impaired DNA synthesis
◦ Megaloblastic anemia
◦ Hypersegmented neutrophils
◦ Macrocytosis (MCV > 100 fl)
◦ Neuropathy , Damage to the nervous system
◦ Results from defect in the secretion of intrinsic factor (IF):
◦ Anti - intrinsic factor antibodies
◦ Anti - parietal cells antibodies
Deficiencies may also be seen with:
◦ Strict vegetarianism
◦ Malabsorption syndromes
◦ Gastrectomy (no IF)
◦ Ileectomy (no Absorption)
◦ Infection with fish tapeworm (D. latum)
What anemia
results from IF
deficiency?
b12 deficiency symptoms
Clinical Symptoms are:
◦ Anemia
◦ Peripheral neuropathy
◦ Jaundice
◦ Mental confusion
◦ Dementia
Bacteria in the gut synthesize vitamin B12 but in different
area to where absorption takes place, thus not providing a
source of the vitamin
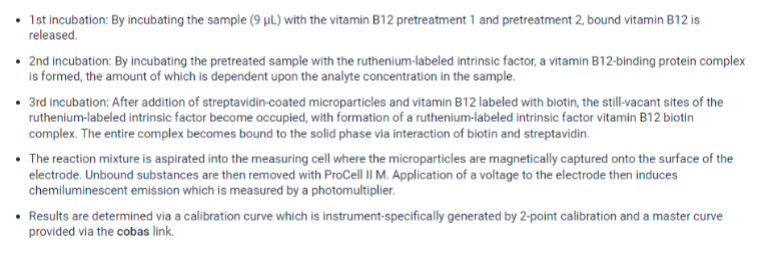
b12 laboratory measurement
Competitive binding Immunoassays
◦ RIA
◦ FPIA
◦ Chemiluminescence
◦ EMIT, EIA
Reference ranges for Serum B12
◦ 110 - 800 pg/ml
Stability: Vitamin B12 is heat stable, but is sensitive to light
◦ Protect from light
roshe VB12 chemiluminescent immunoassay
folic acid (folate) vitamin B9
Function:
◦ Essential for the formation of new cells
◦ It is involved in the metabolism of DNA and RNA
◦ Is required for normal growth, development and functioning of the fetus, nervous
system and bone marrow
Folate and B12 are closely related metabolically
Plays a role in reducing Homocysteine levels
◦ Homocysteine associated with increased risk of CAD
folate deficiencies
Principle food sources:
◦ Green leafy vegetables, Beans, Liver, Yeast Extract, Whole grains, Egg yolk
◦ Milk and milk products, Oranges and orange juice
◦ Beets, Whole meal bread, Beer
Results in impaired cell division
Alterations in protein synthesis
Hematologic changes
◦ are indistinguishable from B12 deficiency
◦ including Megaloblastic anemia
Associated with increased risk of CAD
◦ Deficiency of folic acid is quite common and can be caused by
inadequate intake, problems with absorption and metabolism or
increased requirements
◦ Alcoholism
◦ Malabsorption syndrome
◦ Carcinoma
◦ Liver disease
◦ Hemolytic anemia
◦ Folic acid inhibitors (Methotrexate)
◦ Anticonvulsant therapy used to treat epilepsy
◦ Isoniazid and cycloserin for tuberculosis
◦ Oral contraceptives
◦ Pregnancy
folate measurement
Competitive binding immunoassays
Measuring the Erythrocyte Folate levels
Serum Concentrations: 3 -16 ng/ml,
RBC Folate = 130 - 630 ng/ml
Deficiency: < 140 ng/ml
Stability
◦ Folic acid in food is very unstable and considerable losses occur during
short storage and cooking
vitamin C
vital for the production of Collagen
Collagen is the intercellular substance that gives bones,
teeth, cartilage, blood vessels and muscles their structure
Ascorbic acid is needed for synthesis of bile acids
It maintains skin elasticity
Aids in iron absorption
Improves resistance to infection
function of vitamin c, ascorbic acid
Functions in hydrogen ion transfers and oxidation-reduction
potentials
◦ Required for:
◦ Amino acid metabolism
◦ Synthesis of collagen
◦ Synthesis of catecholamine (adrenal hormones)
◦ Cholesterol metabolism
◦ Antioxidant activities
◦ Enhances the absorption of iron
vitamin c deficiency symptoms
Symptoms of beginning vitamin C deficiency include:
◦ Fatigue
◦ Insomnia
◦ Loss of Appetite
◦ Minor capillary bleeding
A long period of vitamin C deficiency leads to scurvy, the weakening of body structures
containing collagen
Scurvy Characterized by:
◦ weakness
◦ lassitude
◦ Widespread capillary bleeding
◦ Bleeding gums and loosening teeth
◦ Bone malformations in infants
◦ osteoporosis
◦ defective tooth formation
◦ swollen bleeding gums
◦ impaired wound healing
◦ anemia
vitamin c measurement
Measured by HPLC with electrochemical detection
Reference range: 0.4-0.6 mg/dl
Most animals can synthesize their own ascorbic acid within their liver,
with the exception of fish, primates (including humans) and Guinea pigs
Vitamin C is commonly added to foods as an antioxidant to protect color
and aroma
fat soluble vitamins
Their absorption depends
◦ adequate bile and pancreatic secretions
◦ healthy bowel mucosa
These are stored in the body's fat droplets
Therefore, deficiencies generally develop slowly
Toxicity is more apt to develop
Deficiency can develop due to absence of bile salts
necessary for fat absorption
vitamin A, retinol
Retinol (an alcohol) can only be found in animal sources and can be converted by
the body into retinal (an aldehyde) and retinoic acid (a carboxylic acid), other
active forms of vitamin A
A group of compounds essential for:
◦ vision
◦ cell differentiation
◦ growth
◦ reproduction function
◦ immune system function
Beta carotene, a hydrocarbon, is one of a family of dark pigments called
provitamin A carotenoids
Some can be converted to retinol by the body
In the liver, one molecule of beta carotene can be cleaved by an intestinal enzyme
into two molecules of retinol
Good food sources of beta carotene can also be good sources of retinol
vitamin A two natural forms
◦ Vitamin A, retinol (A1)
◦ Dehydroretinal (A2)
◦ Beta Carotene
sources of vitamin A
Liver
Egg Yolk
Oily fish such as:
◦ Herring, Pilchards, Tuna, Sardines
Whole Milk, Butter, Cheese
Good Sources of Beta Carotene include:
◦ Carrots
◦ Yellow and dark green leafy vegetables (e.g. spinach, broccoli,
watercress)
◦ Herbs such as: Basil, Coriander, Parsley
◦ Apricots, Pumpkin, Melon, Sweet Potatoes
◦ Mango, Papaya, Red Pepper, Guava
vitamin A absorption
Retinol and carotenes
◦ absorbed from the small intestines into the circulation
◦ via the lymphatic system
◦ as retinyl esters in chylomicron complex
◦ Retnyl esters are taken up and stored by the liver
◦ attached to RBP (retinol binding protein)
◦ After secretion into the circulation
◦ Vit A-RBP complex is joined to Prealbumin
vitamin a deficiency
Most common in children in non-industrialized countries
◦ Insufficient dietary intake
May also occur as a result of chronic fat malabsorption
Deficiency
◦ Night blindness - impaired vision in dim light
◦ Xerophthalmia - partial or total blindness due to damage of the cornea
from a severe deficiency
◦ Skin lesions
◦ Inhibited growth and bone development and loss of weight in the
young
◦ Increased susceptibility to infection
vitamin A and vision
oThe retina of the eye is made up of light receptor
cells, called rods
oAllow us to 'see' light and dark
oWithin these cells is a pigment called rhodopsin
which is a complex of opsin, a protein, and retinol
oOn exposure to light, this complex disintegrates and
releases electrical charges to the brain via the optic
nerve
oNew rhodopsin is then formed from opsin and retinol
vitamin A assays
Direct fluorometric (Neeld-Pearson Method)
HPLC
Mass Spectometry
Reference range:24 to 90 μg/dl
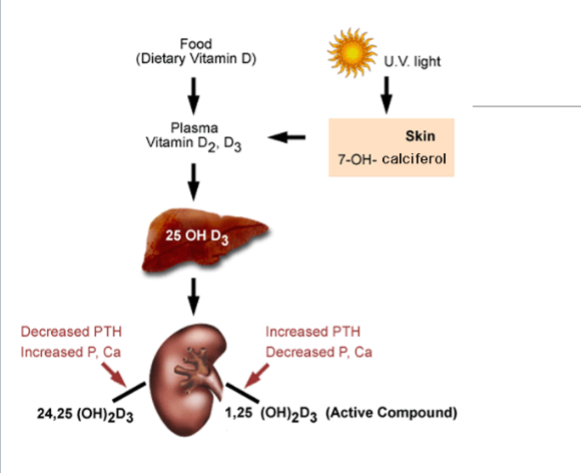
vitamin D
Chemistry: There are two chemical forms of vitamin D,
◦ Vitamin D2 (ergocalciferol)
◦ Vitamin D3 (cholecalciferol)
The natural form of vitamin D for animals and man is vitamin D3
Produced in their bodies from cholesterol and 7-
dehydrocholesterol
An alternative vitamin D2 is derived from the yeast sterol,
ergosterol by chemical procedures
vitamin D how it’s made
All steroid hormones and vitamin D3 are chemically related to cholesterol
◦ e.g. cortisol, estradiol, progesterone, aldosterone, and testosterone
Technically the molecule called vitamin D3 is not really a vitamin because it can be
produced by exposure of the skin (higher animals and humans) to ultraviolet light or
sunlight
The skin of many animals and man has a high concentration of the sterol cholesterol
which is converted by enzymes in the skin to the sterol 7-dehydrocholesterol
Exposure of skin to sunlight for regular intervals results in the photochemical conversion
of 7-dehydrocholesterol into vitamin D3
This sunlight- generated vitamin D3 is a precursor of the steroid hormone
◦ 1, 25-(OH)2 D3
vitamin sources and derived from
Vitamin D is derived from two sources:
◦ from food
◦ from the conversion of cutaneous 7-OH Calciferol by UV light
Dietary vitamin D is termed vitamin D2
◦ Is released into the plasma; after conversion of 7-OH Calciferol in the skin,
plasma D3 (the "Sunshine Vitamin") results
D2 and D3 are subject to 25-hydroxylation in the liver to form 25-OH
Vitamin D (the major circulating form of Vitamin D)
25-OH Vitamin D undergoes further hydroxylation in the kidney to form
active 1,25-(OH)2-Vitamin D
vitamin D in the body and what it does
Essential for bone development (mineralization)
Mineral homeostasis
Vitamin D3 enhances the effect of PTH
Intestine:
◦ Vit D3 increases Ca and PO4= absorption in the intestine
In the kidney,
◦ Vit D3 promotes renal reabsorption of Ca and PO4
vitamin D deficiency
Principle food sources:
◦ Vitamin D is only found naturally in animals and animal products; fruit
and nuts contain no vitamin D at all.
Deficiencies
◦ In children
◦ The name “rickets” is from the Old English “wrickken”, to twist
◦ causes deformation of the skeleton
◦ In adults
◦ Leads to under mineralization of bone
◦ Osteomalacia
vitamin D toxicity and benefits
Vitamin D is potentially toxic (Children)
Effects include:
◦ Hypercalcemia and hypercalciuria
◦ Calcium deposits in soft tissue
◦ Irreversible renal and cardiac damage
Vitamin D Benefits:
◦ Suppresses renin production (BP)
◦ Increases insulin sensitivity (Diabetes)
• Suppresses cellular proliferation (anti-cancer)
◦ Suppresses Anti angiogenic properties (anti-cancer)
◦ Stimulates innate immunity (+infections)
◦ Modulates self-tolerance (suppresses autoimmunity)
◦ Enhances killing of Mycobacteria
vitamin D assays
Measurement by either HPLC, RIA
Competitive immunoassay methods. (CLIA, EMIT, ELISA)
◦ Reference values for 25(OH)D3: 22-42 ng/ml
◦ 1,25(OH)2D3: 30-55 pg.ml
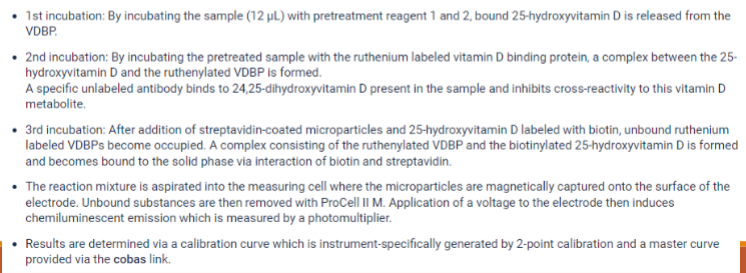
vitamin D assessment
Lab assays are available to measure both 25(OH)D and 1,25-D
25(OH)D closely reflects total amount of Vit D produced in the skin and
from diet
D2 and D3: have similar biological activity
Both D2 and D3 should be measured
25(OH)D concentration
To prevent deficiency
disease –
25 nmol / L
To prevent complications of
insufficiency –
> 50 nmol/L
For maximum bone health
and prevention of chronic
disease –
75 – 100 nmol/L
vitamin E, tocopherols
Not a single compound
Eight related compounds in two groups
◦ Alpha, beta, gamma, delta Tocopherols
◦ Tocotrienols
American diet sources are composed of
◦ 2/3 gamma Tocopherol
◦ 1/3 alpha Tocopherol: selective for oxygen free radicals
Diet supplements contain:
◦ D or D,L alpha Tocopherol
Biologically active form is: alpha-Tocopherol
tocopherol functions
Powerful antioxidant
◦ Is the primary defense against potentially harmful oxidants
◦ Prevents oxidation of unsaturated fatty acids by trapping free
radicals
◦ Prolonging the life of red blood cells
◦ Protecting body membranes
◦ Fertility function is questionable
vitamin E importance, storage, sources, and reference values
Also important for cell membrane integrity (stability), heme biosynthesis,
electron transport and neuromuscular function
Absorption of Vitamin E occurs primarily in the jejunum, where it is
attached to lipoprotein and transported via the lymphatics.
Vitamin E is stored in the liver
The most important sources of vitamin E are:
◦ Vegetable Oils
◦ Nuts
Synthetic vitamin E is produced from fossil plant material
Quantitated by using HPLC
Reference ranges: 5-18 mg/L
◦ 0.5 to 1.8 mg/dL
vitamin E deficiency
Deficiencies occur in:
◦ Premature, very low birth weight infants
◦ Patients who do not absorb fat normally
◦ Deficiencies are associated with:
◦ Mild hemolytic anemia (increased fragility of erythrocytes)
◦ Increased platelet aggregation
◦ Neurologic degeneration
Megadose of vitamin E does not produce toxic effects
May impair the adsorption of vitamin D and K
vitamin K, phylloquinones
Fat soluble vitamin
"K" is derived from the German word "koagulation"
Occurrence: 2 natural forms:
◦ KI: Phylloquinone
◦ found in plant and animal sources
◦ KII: Menaquinone
◦ synthesized by bacterial flora
Absorption is dependent on:
◦ normal pancreas & gal bladder
◦ Presence of bile salts
100 ug stored in the liver
◦ lungs, BM, kidneys and adrenals
vitamin K
Function:
◦ The only known biological role of vitamin K is that of the required
coenzyme for a vitamin K-dependent carboxylase that catalyzes the
carboxylation of the amino acid, glutamic acid, creates calcium binding
site for coagulation factors
Essential for the formation of
◦ Prothrombin (II)
◦ Coagulation factors VII, IX, X
◦ Protein C, and protein S
◦ Vitamin K is necessary to convert the precursor form to the functional
forms (Liver)
◦ Warfarin drugs (Coumadin) inhibit carboxylation
vitamin K sources
Dietary vitamin K is absorbed in the terminal ileum and possible the
colon
Intestinal bacteria synthesize vitamin K to provide about 50% of the
vitamin K requirement
Vitamin K is concentrated in the liver and then distributed among body
tissues
Principal dietary sources of vitamin K are:
◦ Green leafy vegetables such as:
◦ Spinach, Broccoli, Cabbage
◦ Soya Beans
◦ Liver
◦ Green tea
◦ Egg yolks
◦ Oats, Whole wheat
diet and coumadin therapy
Vitamin K - either in a multivitamin or liquid nutrition supplement
Certain foods (such as beef and pork liver, green tea, broccoli,
chickpeas, kale, turnip greens, and soybean products) contain large
amounts of vitamin K and can alter PT results
vitamin K deficiency
Deficiency of vitamin K is rare due to the bacterial synthesis
in the gut
Vitamin K is not routinely measured in the lab
Vitamin K deficiency can occur with malabsorption
syndrome and liver disease
The major sign of vitamin K is the defective clotting of blood
Deficiency increases clotting times for PT and APTT
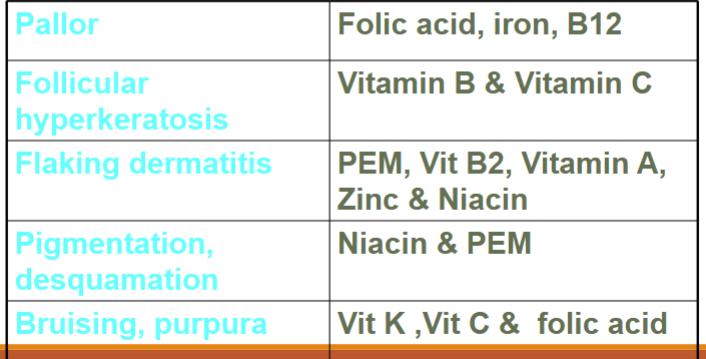
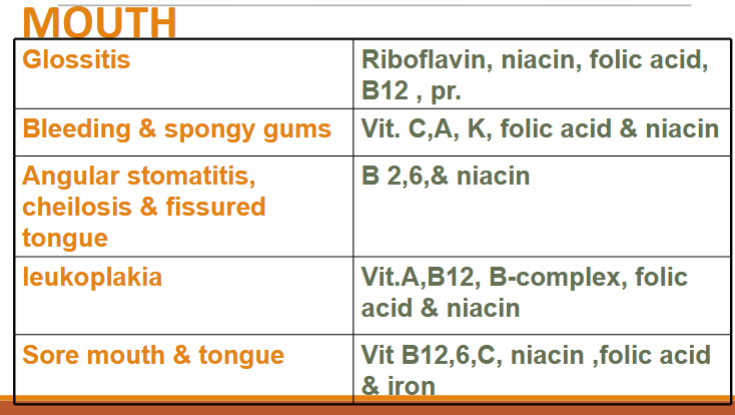
clinical signs of nutritional deficiency
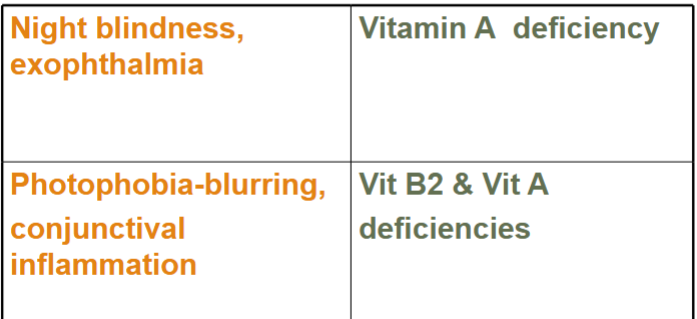
clinical signs of nutritional deficiency with eyes
clinical signs of nutritional deficiency with skin