L5: Exercise, haemorrhage and hypoxia: the cardiovascular responses to specific stresses
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
The cardiovascular response to exercise: what happens and needs to be regulated
Increased metabolic demand on muslces
→ requires incrased blood flow (functional hyperaemia)
→ primarily regulated by local mechanism
Changing blood flow in muscles
blood flow can increase from resting levels
2-3ml-1min-1100g-1→35 (x17 increase)
→ causes a 17 fold DECREASE in ABP
However, the problem is that skeletal muscles makes up 40% of body mass so… (TPR)
synamic exercise involving multiple muslces would
PROFOUNDLY influence TPR
What happens in INTENSE exercise
TPR may drop to 20% of resting value
THEREFORE: why is it important to regulate
catastropic drop in ABP to 20% of resting value!
THEREFORE: need cardiovascular homeostatic mechanisms
What type of mechanisms are responsible for maintaining ABP and cardiovascular homeostasis
SYSTEMIC MECHANISMS
(despite this drop in TPR)
The systemic responses can result in…
5 fold INCREASE in cardiac output
(3 fold increase in heart rate)
(50% increase in stroke volume)
May also partially oppose the locally-mediated vasodilatation in muscle
such that increase in blood flow through muscles exercised in isolation can exceed the flow through the same muscle during whole-body exercises
Cardiovascular response (LOCAL): Functional hyperaemia→ what is it
Blood flow to active muscles incrases very rapidly
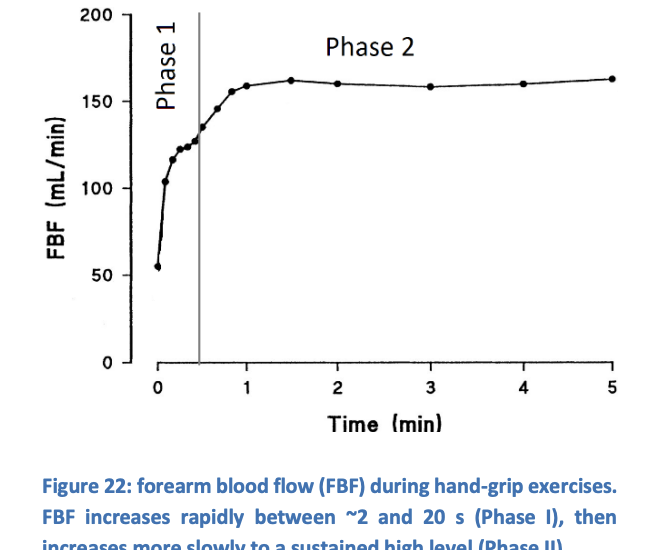
Functional hyperaemia: distinct phases
PHASE 1: blood flow increases very rapidly
2 to 15-20s after initiation of contraction
PHASE II: from 20s after initiation of contraction
there is a sow increases in blood flow to sustained high levels
Functional hyperaemia: What causes this to happen
Activity in muscle→ wide range of local changes influecing arteriolar diameter:
reduced PO2
increased PCO2
decreased pH
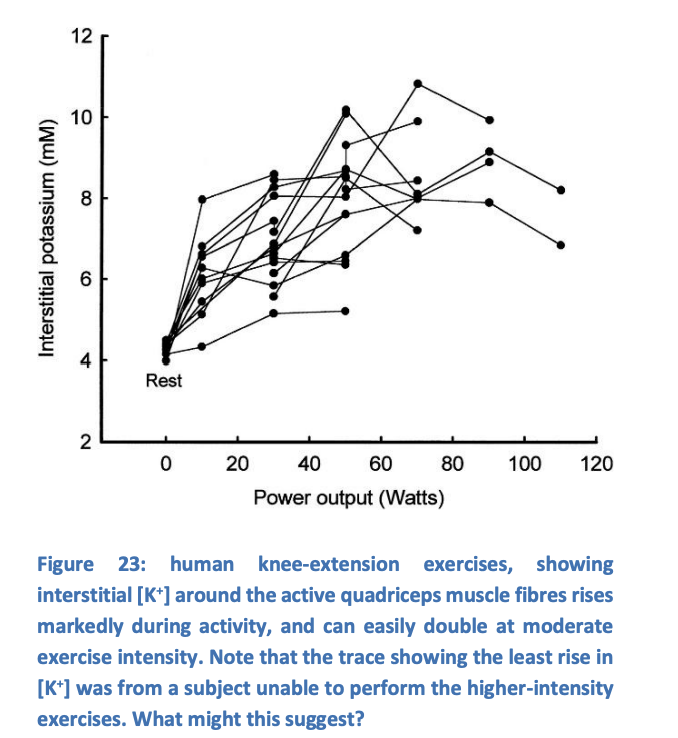
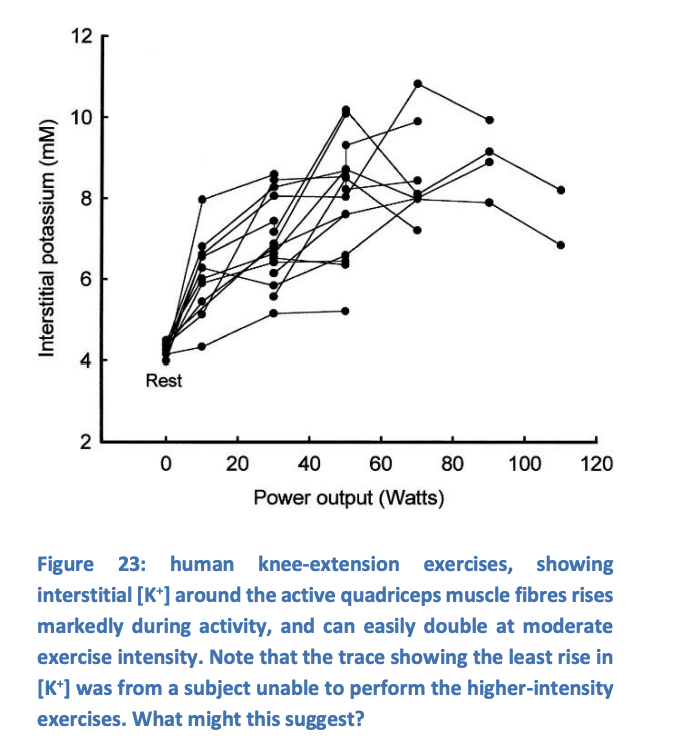
increased extracellular K+
lactic acid production
increased extracellular ADP, AMP and Adenosine
Are some of these more important than others?
PHASE 1: important factors
easy to see which factors affect this coz, most of the rest are slow apart from:
K+ ions
muscle action potential produce immediate and fast increases in extracellular [K+']
as much as 10mM
depending on activity levels
within 5-10s
Muscle pump
(in some animals but not humans) Neurogenic vasodilatiion
Adrenaline? (anticipatory)
![<p><em>easy to see which factors affect this coz, most of the rest are slow apart from:</em></p><ol><li><p>K+ ions</p></li></ol><ul><li><p>muscle action potential produce immediate and fast increases in extracellular [K+']</p><ul><li><p>as much as 10mM</p></li><li><p>depending on activity levels</p></li><li><p>within 5-10s</p></li></ul></li></ul><ol start="2"><li><p>Muscle pump</p></li><li><p>(in some animals but not humans) Neurogenic vasodilatiion</p></li><li><p>Adrenaline? (anticipatory)</p></li></ol><p></p>](https://knowt-user-attachments.s3.amazonaws.com/00f19820-24f5-4754-b11a-b4a5b95b40f5.png)
PHASE 1: cause 1: effect of rise in intersitial [K+]
hyperpolarises arteriolar smooth muscle
this closes voltage-gated Ca2+ channels
relaxes the muscle
PHASE 1: why doesn’t the etracellular [K+] cause depolarisation?
Due to two effects of raised extracellular [K+] :
enchances Na+/K+-ATPase activity
enhances activation of inwardly-rectifying K+ channels (KIR) look at AP diagram
THEREFORE: increased intracellular K+ and increased K+ permeabbiliy
→ hyperpolarisation
![<p>Due to two effects of raised extracellular [K+] :</p><ol><li><p>enchances Na+/K+-ATPase activity</p></li><li><p>enhances activation of<strong> inwardly-rectifying K+ channels</strong> (KIR)<em> look at AP diagram </em></p></li></ol><p></p><p>THEREFORE: increased intracellular K+<strong> and</strong> increased K+ permeabbiliy</p><p>→<strong> hyperpolarisation</strong></p><p></p>](https://knowt-user-attachments.s3.amazonaws.com/044831f3-e8dc-478a-816b-86364061557a.png)
PHASE 1: pharmacologic bloackde of either of these routes for K+ entry…
e.g ouabain or barium:
attenuates vasodilation by approx 50%
PHASE 1: cause 2→ muscle pump
muscle contraction accelerate venous return
enhances CO
but also
may reduce local venous pressures
→ enhancing the pressure gradient through muscle capillaries
PHASE 1: cause 3→ neurogeneic vasodilataion (not in humans)
sympathetic cholinergic nerves directly cause rapid incrase in blood flow to muscle at start of exercise
PHASE 1: cause 4→ Adrenaline
also cause vasodilatation
but
not fast enough to contribute to phase 1
but
may be released as part of an anticitpatory response
PHASE II: why difficult to identify mechanisms
multiple redundancies mean:
when one substance is inhibited, the magnitude of hyperaemia can change little
because other factors then make larger contribution
THEREFORE:
chnages in some key concentration profoundly influence others
PHASE II: chnages in some key concentration profoundly influence others examples…
Reduced Po2 clearly alters skeletal muscle metabolsim
resultant metabolic products chaneg
therefore, difficult to separate direct responses to Po2 from responses to its downstream influences
PHASE II: some factors of the response have been identified:
Raised extracellular K+
Adrenaline
O2
Adenosine and decreased pH
PHASE II: raised extracellular K+
Similar affect to in PHASE 1
PHASE II: adrenaline
actiavtes beta2 receptors
on vascular smooth muscle in skeletal muscles
by circulating adrenaline
→ VASODILATORY effect
PHASE II: O2→ direct effect of reduced Po2?
unlikey that there is a direct effect of reduced pO2 on muscle arterioles
because…
although pO2 falls in muscle capillaries in exercise
it as not been shown to fall in the vicinity og arterioles
PHASE II: O2→ effect of increased offloading of O2 from haemoglobin
RESULT:
release of ATP and NO from RBCs
low O2 ALSO→ enhances activity of ectonucleotideases
→ produce vasodilatory adenosine from ATP
i.e can get an idea as to how these factors are interconnected in phase 2
PHASE II: Adenosine and decreased pH
Adenosine ALSO accumulates arounf active muscle fibres
source may be ATP released by active muscle
acted on by extracellular ectonucleotides
→ THIS RELEASE of ATP is at least partly via CFTR channels
in response to reduced intracellular pH
linking pH changes to vasodilatation
(reduced pH→ CFTR channel response→ ATP release→ acted on extraceullar ectonucleotideases→ adenosine accumulates→ vasodilatation)
PHASE II: how does adenosine work
Strong vasodilator
acting on A2A receptors
increase cAMP levels in smooth muscle
activates protein kinase A (PKA)
opens Katp channels
hyperpolarises cell (by same mechanism as K+ accumulation)
may therefore act synergistically with increased K+
PHASE II: lactic acid?
not been shwon to have direct effect
that is distinct from its effect on pH
Summary of functional hyperaemia
complex and not completely understood
CLEAR EFFECTS
exercising muscles receive a bloody supply closely matched to its metabolic demans
increase in blood flow results largely or wholly from local vasodilatory influences
BUT NOW, the systemic control procresses must prevent the resultatn reduction in TPR from having dire consequences
Systemic circulatory control in exercise: dealing with the consequences of functional hyperaemia: problem being face
TPR drops
as little as 20% of its resting value in intense exercise
→ this is mean the ABP will change (which we want to keep constant)
What needs to be done to solve this problem
increase CO
to maintain ABP
How is this acheived: (seen in L4 + one more)
sympathetic venoconstriction→ increase MSFP
recuced cardiac vagal stimulation→ increase HR
increase cardiac sympathetic stimulation→ increase HR and myocardial contracility
Muscle pump action of contracting muscles on nearby veins
pushes blood towards heart due to presence of venous valvves
Effect of ‘muscle pump’ action
blood pushed towrads heart
reduced resistance to venous return RVR
increasing VR at given MSFP
MSFP may increase 3-fold yet VR and CO may ncrease 6-fold
→ THEREFORE: muscle pump activity must be halving RvR
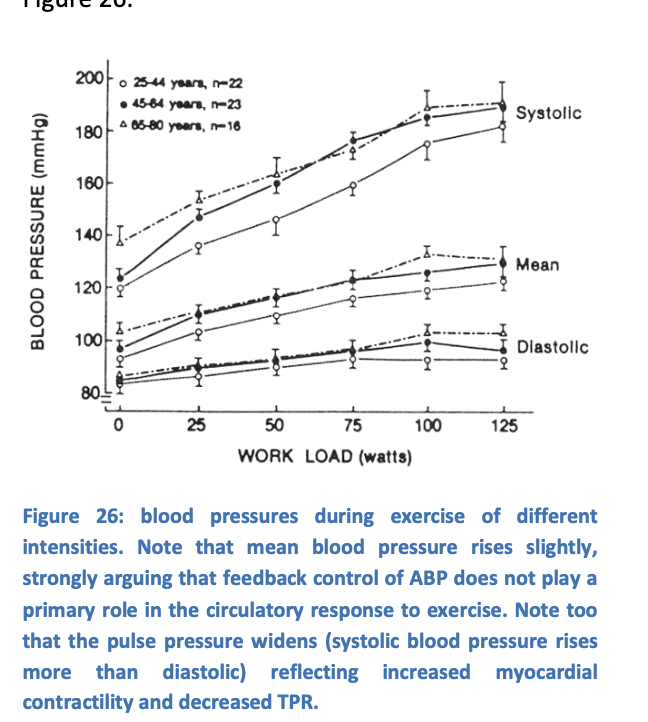
NET RESULT: causes mean ABP to rise slightly in exercise
What produces:
incrased sympathetic acticty
reduced cardiac vagal activity?
Cardiac centre in medulla→ from three inputs
How is cardiac centra in medulla well positioned to coordinate response to circulatory changes in exercise:
Receives input from
higher brain centres involved in ‘decising’ to exercise
muscle and join sensors that respond to movements
arterial baro- and chemoreceptors
but which is most important?
How to figure out which factor is most important
separate cental command to exercise from actual occurrence of exercise
use curare to block neuromuscular junction
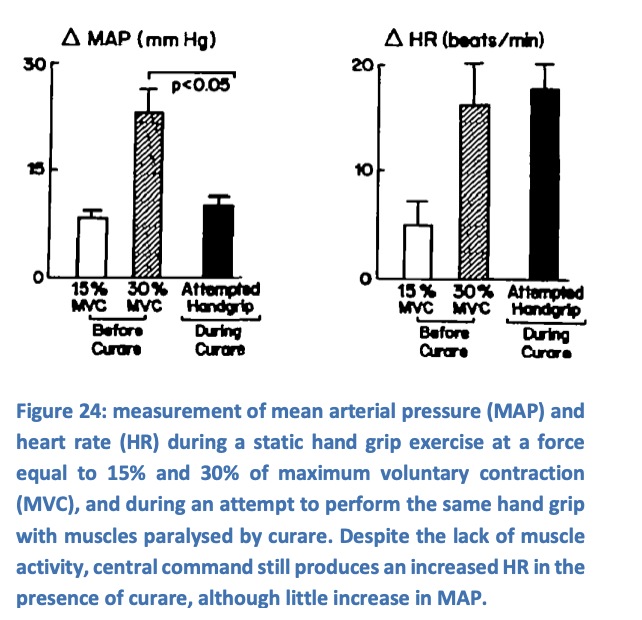
What does this demonstrate
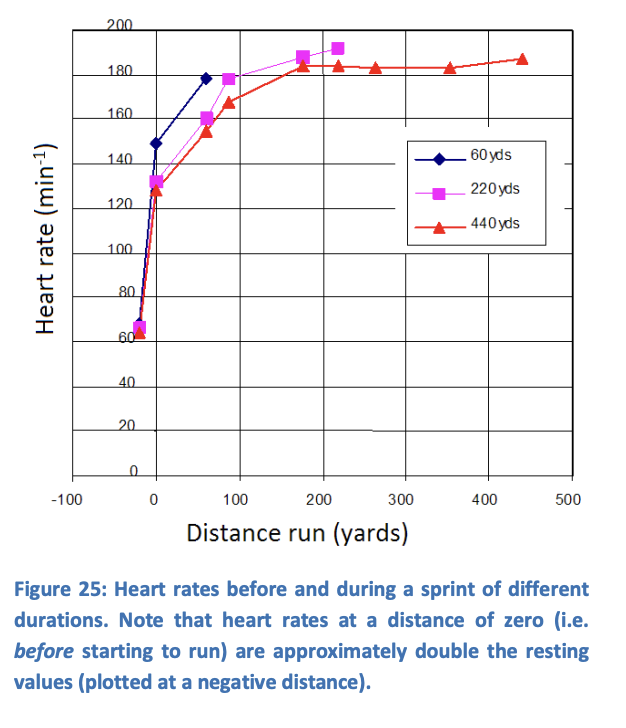
increase in heart rate during exercise can occur without any actual exercise occuring
such centrally-mediated cardiovascular responses correlate with the perceived effor of exercise
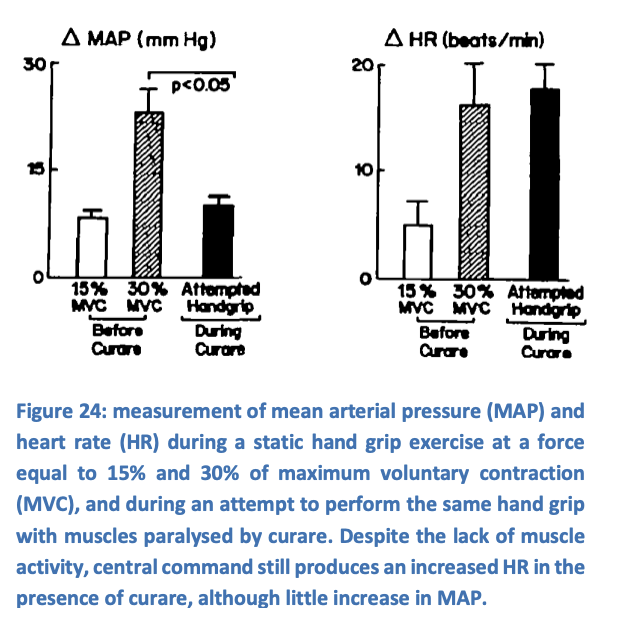
Indeeed, it is possible to record increased heaert rate even before exercise begins
hen what is the role of barpreceptors in exercise?
unknown centrally-commanded mechanism:
to reset
possibly in part due to joint and position sensors competing with baroreceptors inputs to the nucleus tractus solitarious
What is the effective result of this?
baroreceptors then maintain the stability of blood pressure
around a slightly raised set point
Limiting factors in exercise: The highest cardiac outputs are seen in exercise→ there for does cardiac output…
limit maximum performance
or
is maximum performance limited by some other factor?
What are the other factors that may limit maximum performance?
ability of muscles to perform work
rate of O2 uptake in the lungs
How do we know what actual factor is limiting?
depends on a person’s level of fitness…
Fitness level: Normal lungs
O2 uptake is not limiting
→ shown by measuring perfoance at normal and raised levels of Po2:
raised inhaled Po2 does not significantly improve performance
Fitness level: reasonably fit
ability of muscles to perform work is not limiting by comparing power output
when pedalling an exercise bike with one vs two legs
Power output with 2 legs is less than double power output with just one leg
What does this suggest
during 2 legged cycling:
muscles are not able to produce their maximum power output
Explanantion of what is happening here (From the lecture)
with diagram
I think it was saying
each leg in the double cycling→ gets less blood→ has to work faster→ must have increased resistance→ vasoconstri ion to maintain ABP→
Fitness level: less fit people
may not have sufficient muscle aerobic capacity to produce this effect
may instead be limited by their unfit muscles
Together this suggests…
circulation provides the ultimate limitation on whole-body power output during exercise
Note: this limitation exists despite…
mean blood pressure being sustained even in mos intensive exercise
THEREFORE
it is not possible to exerise so hard that ABP drops
This suggests that
there is a central regulation of activity levels according to circulatory requirments
aka:
one component of feeling of fatigue must relate
althouhg ideirectly
to circulatory capacity
Exercise in disease states:
ability of relative circulatory inadequacy to regulate activity levels
and
produce the feeling of fatigue has important consequences in disease
sates involving reduced maximum cardiac output
This particulalrly includes:
heartfailture for which fatigue may be a prominent feature
Heamorrhage: what happens
Blood loss
decrease MSFP
decrease VR and CO
decrease ABP
Heamorrhage: (rapid) response
Reduced blood volume (feedback)→ vasoconstrictory (among other things)
pain/emotional state (feed foward)
rapid response in seconds
main aim is to→ increase MSFP, HR and TPR
Feedback → Reduced blood volume baroreceptors
Arterial baroreceptors (carotid sinus and aortic arch) and low-pressure baroreceptors (terminal great veins and atris)→ detect changes
Medulla:
reduced cardioinhibitory
increase vasomotor
increases sympathetic
increases vagal tone
renal effects
increase MSFP, increase HR and increase TPR
helping direct blood to where you want it
Feedback→ reduced blood volume→ microvasculature changes
reverse stress relaxation→ smooth muscle contracts when stretch is reduced
decrease downstream capillary pressure
autotransfusion (fluid from tissue into cap) (0.5-1L)
mobilisation of tissue fluid
due to reduced capillary pressures shift the balance of starling filtration-reabsorption forces
towards reabsorption of fluid
increase MSFP
Feedback→ hormonal effects
catecholamines
agiostensin II
ADH
are released, effect:
VASOCONSTRICTORY effects especially in high concentrations
Feed forward→ pain response
higher brain centres (cortex and hypothalamus)
stimulates areas as a response to pain or fear
increases HR itself
Haemorrahage: less rapid response
24-48 hours: plasma protesins replaced by synthesis in liver
5-7 days: increasd RBC production→ restore those lost
Haemorrghage: less rapid response (stimulates by)
release of erythropoietin from the kidneys
in response to reduced oxygen delivery
Hypoxia: two reasons for this happening
Lack of O2 due to stop breaking→ (diving)
Lack of O2 due to reduced concnetraion in inhaled air
Hyposixa: two reasons have two different responses
note: chronic lung disease may combine aspects of both stresses
conservation of O2→ conserve for brain (if not getting anything else)
Increased blood flow to tissues→ still get some O2 so just incrase cardiac ouput to compensate (O2 delivery = flow x concentration) so need to increase flow
Hypoxia response: 1. why need a different mechanism for conservation of O2
direct effect of recuded Po2
produces metabolic vasodilation in tissues
HOWEVER: in diving this is not ideal→ it would allow other tissues other than the brain to use O2 faster→ want to conserve O2 for the brain!
Hypoxia response: 1. Reduced Po2 is detected by
carotid and aortic bodies
and in central chemoreceptors and integrated in the medulla
Hypoxia response: 1. this causes a reflex response…
slowed heart rate→ mediated by cardiac vagal reflex
systemic vasoconstriction> mediated by sympathetic nervous system
This is called: diving reflex or the primary chemoreceptor response
Hypoxia response: 1. what is the overall effect of this response
reduces cardiac work to a minimum
sympathetic drive overwhelms the metabolic vasodilatation
to divert the available blood to those tissues
with little sympathetic vasoconstrictor innervation
→ the brain and heart
Hypoxia response: 1. In diving animals (seals)
response is very well developed
→ but also observed in humans especially in cold-water immersion
Where the heart rate can drop to as low as 20-30 beats per minute
Hypoxia response 2: how can the body generate a different response at altitude from that during diving??
reduced Po2 must surely activate the same pathways
whether there is low oxygen concentration vs when there is reduction total oxygen amount
Answer: secondary chemoreceptor response
Hypoxia response: 2. Secondary chemoreceptor response
when reduced Po2 produces an increased rate and depth of breathing
→ as it normally does if breathing is not restricted
pulmonary stretch receptors send afferent impulses via vagus nerve
to the medulla
stimulate vasomotor centre
→ venoconstriction
increase MSFP
increase CO
inhibits cardio-inhibitory centre
increases HR
causes pattern of vasodilataion/constriction that favors vital tissues
NET RESULT: rise in cardiac output→ allow tissue oxygen needs to be met, despite reduced blood oxygen concentrations
Hypoxia: animal models have shown…
animal models of obstructive sleep apnoae
→ suggest that chronic hypoxia may lead to chronic hypertension by this mechanism