Chapter 16 after mid
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
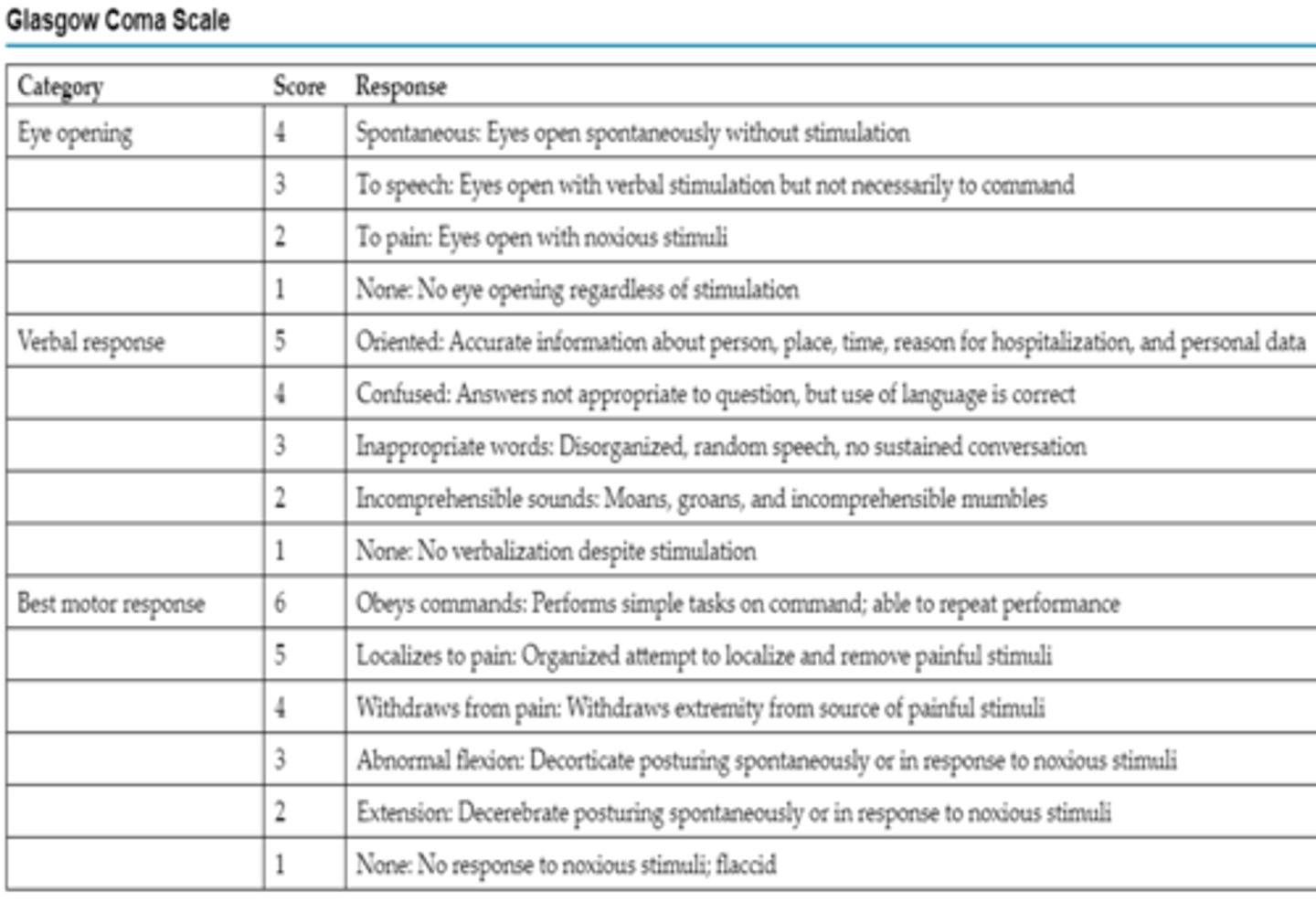
The nurse is caring for a patient with a closed head injury with a Glasgow Coma Scale (GCS) score of 6. What does this score indicate about the patient's neurologic status?
A. patient is in vegetative state
B. patient is a paraplegic
C. patient is in a coma
D. patient is able to obey commands
C. Patient is in a coma
GCS 7 or <7: Indicating Coma
Glasgow Coma Scale (GCS). This scored scale is based on evaluation of three categories: (1) eye opening, (2) verbal response, and (3) best motor response. The highest possible score on the GCS is 15, and the lowest score is 3. A score of 7 or less on the GCS usually indicates coma.
A patient with a serious head injury has been admitted. The nurse knows that certain neurologic findings can indicate the prognosis for the patient. Which finding indicates the most serious prognosis?
A. abnormal flexion
B. abnormal extension
C. localization
D. withdrawal
B. abnormal extension
A: Decorticate posturing
(Abnormal flexion), lesion above midbrain
B: Decerebrate posturing
(Abnormal extension), lesion in brainstem
C: Decorticate posturing (right side)
& Decerebrate posturing (left side)
The nurse knows that change in pupil size is a significant neurologic finding particularly in the patient with a head injury. How much of a size difference between the two pupils is still considered normal?
A. 1mm
B. 1.5 mm
C. 2 mm
D. 2.5 mm
A. 1 mm
Pupil diameter is documented in millimeters (mm) using a pupil gauge. Most people have pupils of equal size, between 2 and 5 mm. A discrepancy up to 1 mm between pupils is normal. It is called anisocoria and occurs in 16% to 17% of humans.
A patient is admitted immediately after a craniotomy. The patient has no history of eye surgery. When assessing the size and shape of the patient’s pupils, the nurse observes the patient’s left pupil is oval. What does this finding indicate?
A. Cortical dysfunction
B. Intracranial hypertension
C. Oculomotor nerve damage
D. Opioid overdose
C. Oculomotor nerve damage
Oculomotor nerve compression results in a dilated, nonreactive pupil.
1. Change or inequality in pupil size is a significant neurologic sign. It may indicate impending danger of herniation and should be reported immediately. Pupil size and reactivity play a key role in the physical assessment of intracranial pressure (ICP) changes and herniation syndromes.
2. In addition to CN III compression, changes in pupil size can occur due to cycloplegic agents, extreme stress, opioid overdose, lower brainstem compression, or bilateral damage to the pons. Pupil shape is included in the assessment of pupils. Although the pupil is normally round, patients who have undergone eye surgery or patients with the initial stages of CN III compression from elevated ICP may have an irregularly shaped or oval pupil.
A patient is admitted with an anoxic brain injury. The nurse notes abnormal extension of both extremities to noxious stimuli. This finding indicates dysfunction in which area of the central nervous system?
A. cerebral cortex
B. thalamus
C. cerebellum
D. brainstem
D. brainstem
A: Decorticate posturing
(Abnormal flexion), lesion above midbrain
B: Decerebrate posturing
(Abnormal extension), lesion in brainstem
C: Decorticate posturing (right side)
& Decerebrate posturing (left side)
The nurse is admitting a neurologically impaired patient. The patient's family is present. How comprehensive should the initial history be?
A. it should be limited to the chief complaint and personal habits.
B. it should be all-inclusive, including events preceding hospitalization.
C. it should be confined to current medications and family history.
D. it should be restricted to only information that the patient can provide.
B. it should be all-inclusive, including events preceding hospitalization.
The nurse is teaching a nursing student about the importance of assessing the patient's level of conscious (LOC). Which statement indicates the nursing student understood the information?
A. The LOC is the most prognostic indicator of the patient's neurologic outcome.
B. The LOC limited to the Glasgow Coma Scale making it the quickest part of the assessment.
C. The LOC is the easiest part of the neurologic exam and thus is generally performed first.
D. In most situations, the LOC deteriorates be
D. In most situations, the LOC deteriorates before any other neurologic changes are observed.
Content of consciousness is a higher level function, and appraisal of awareness is concerned with assessment of the patient’s orientation to person, place, time, and situation. Assessment of content of consciousness requires the patient to give appropriate answers to a variety of questions. Changes in the patient’s answers that indicate increasing degrees of confusion and disorientation may be the first sign of neurologic deterioration
The nurse is caring for a critically injured patient who can only be aroused by vigorous external stimuli. Which category should the nurse use to document the patient’s level of consciousness?
A. Lethargic
B. Obtunded
C. Stuporous
D. Comatose
C. Stuporous
A. Lethargic: difficulty maintaining a state of wakefulness but arouses to vocal stimuli.
B. Obtunded: blunted state of alertness when responding to stimulation other than pain.
C. Responsive only to painful stimuli that is forceful and continuous.
D. Unresponsive to painful stimuli.
The nurse is starting a peripheral intravenous catheter in the right hand of an unconscious patient.During the procedure, the patient reaches over with his left hand and tries to remove the noxious stimuli. How would the nurse document this response?
A. Decorticate posturing
B. Decerebrate posturing
C. Withdrawal
D. Localization
D. Localization
Purposeful movements towards painful stimuli.
The nurse is precepting a nursing student. The student asks about testing of extraocular eye movements. What should the nurse tell the student?
A. It tests the pupillary response to light
B. It tests function of the three cranial nerves
C. It test the ability of the eyes to accommodate to a closer moving object.
D. It tests the oculocephalic reflex.
B. It tests function of the three cranial nerves.
Testing CN 3, 4, 6, pt follows the direction of the examiner's finger.
on unconscious pt: we have the Dolls reflex.
The nurse is caring for a patient who has sustained a traumatic head injury. The practitioner has asked the nurse to test the patient’s oculocephalic reflex. What must the nurse verify before performing the test?
A. Absence of cervical injury
B. Depth and rate of respiration
C. Patient's ability to swallow
D. Patient's ability to follow a verbal command
A. Absence of cervical injury
(neck injury C1-C4, we can't move neck if injury is present)
In the unconscious patient, assessment of ocular function and innervation of the MLF is performed by eliciting the doll's eyes reflex. To assess the oculocephalic reflex, the nurse holds the patient's eyelids open and briskly turns the head to one side while observing the eye movement and then briskly turns the head to the other side and observes the eye movement again. If the eye movement deviates to the opposite direction in which the head is turned, the doll's eyes reflex is present, and the oculocephalic reflex arc is intact. If the oculocephalic reflex arc is not intact, the reflex is absent. This lack of response indicates significant brainstem injury. The reflex may also be absent in severe metabolic coma. An abnormal oculocephalic reflex is present when the eyes rove or move in opposite directions from each other. Abnormal oculocephalic reflex indicates some degree of brainstem in
The nurse is caring for a patient who has sustained a traumatic head injury. The practitioner has asked the nurse to test the patient's oculocephalic reflex. Which findings indicate that the patient has an intact oculocephalic reflex?
A. Patient's eye move in the same direction as the patient's head when turned.
B. Patient's eye move in the opposite direction as the patient's head when turned.
C. Patient's eyes move in opposite direction from each other when the patient's head is turned.
D. P
B. Patient's eye move in the opposite direction as the patient's head when turned.
•In the unconscious patient, assessment of ocular function and innervation of the MLF is performed by eliciting the doll’s eyes reflex. To assess the oculocephalic reflex, the nurse holds the patient’s eyelids open and briskly turns the head to one side while observing the eye movement and then briskly turns the head to the other side and observes the eye movement again. If the eye movement deviates to the opposite direction in which the head is turned, the doll’s eyes reflex is present, and the oculocephalic reflex arc is intact. If the oculocephalic reflex arc is not intact, the reflex is absent. This lack of response indicates significant brainstem injury. The reflex may also be absent in severe metabolic coma. An abnormal oculocephalic reflex is present when the eyes rove or move in opposite directions from each other. Abnormal oculocephalic reflex indicates some degree of brainstem injury.
The nurse is precepting a new graduate nurse. The new graduate asks about testing the oculovestibular reflex. What should the nurse tell the new graduate?
A. the test should not be performed on an unconscious patient because of the risk of aspiration.
B. an abnormal response is manifested by conjugate, slow, tonic nystagmus, deviating toward the irrigated ear.
C. this test should be included in the nursing neurologic examination of a patient with a head injury.
D. this test is performed by the p
D. this test is performed by the practitioner and one of the final clinical assessments of brainstem function.
Oculovestibular reflex (Cold caloric test)
-One of final brainstem assessments
-CN III, IV, VI, & VIII
-Conjugate nystagmus 30-120 sec then back to midline position responding to ice H2O (20-40ml)
-Abnormal or absent reflex:
•little or no brainstem function
-Temporarily absent in metabolic encephalopathy
The nurse is caring for a patient with a head injury and observes a rhythmic increase and decrease in the rate and depth of respiration followed by brief periods of apnea. What should the nurse document under breathing pattern?
A. Central neurogenic hyperventilation
B. Apneustic breathing
C. Ataxic respirations
D. Cheyne-Stokes respiration
D. Cheyne-Stokes respiration
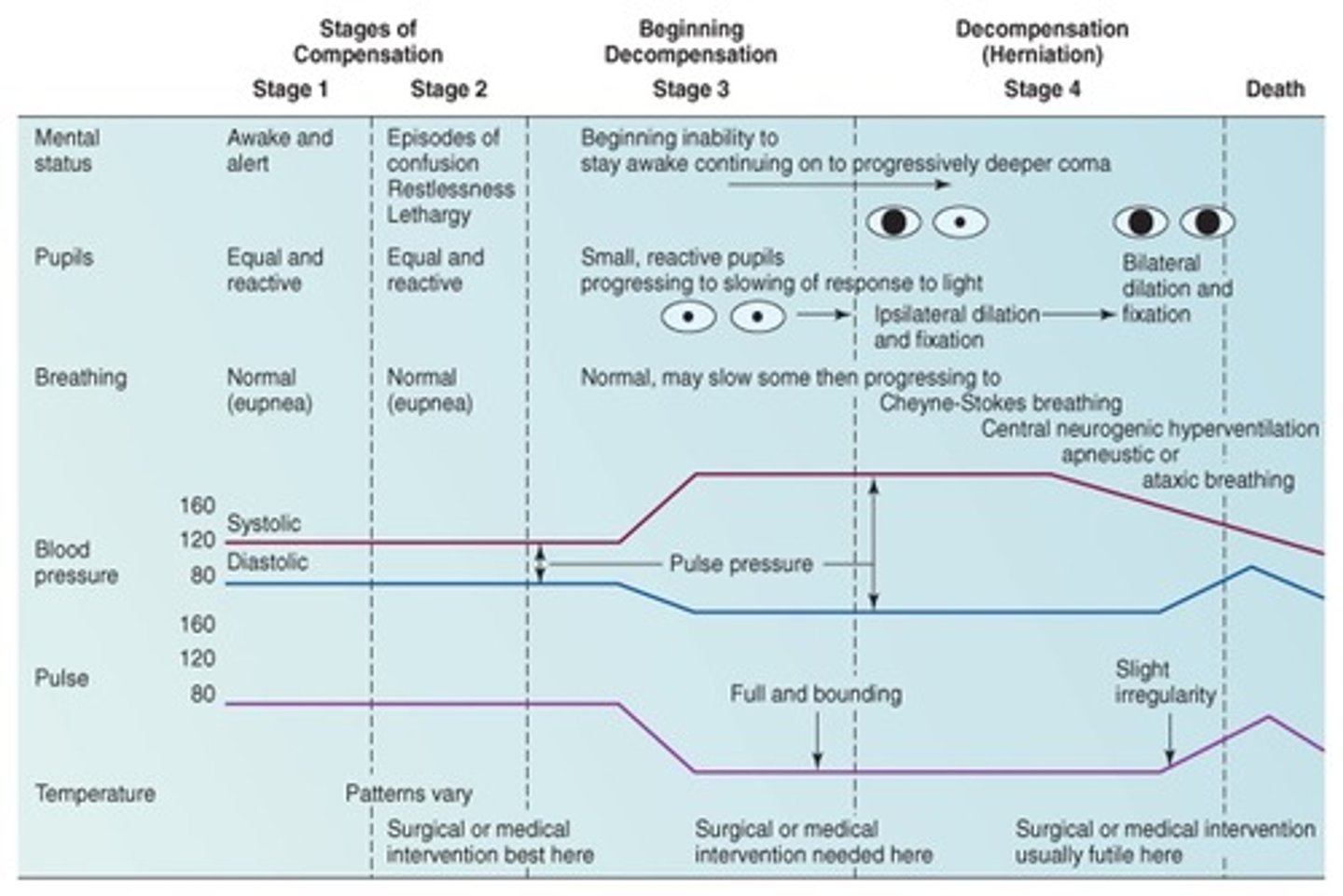
Changes in respiratory patterns are related to brainstem injury or dysfunction
Apneustic: prolonged inspiratory and/or expiratory pause of 2-3 seconds.
Ataxic: Irregular, random pattern of deep and shallow respirations with irregular apneic periods.
Central neurogenic hyperventilation: Very deep, very rapid respirations with no apneic periods.
The nurse is caring for a severely head injured comatose patient who is dying. The nurse knows the patient has entered the late stages of intracranial hypertension when the nurse observes which signs?
A. pupils are equal and reactivev
B. widening pulse pressure
C. eupnea
D. decreased intracranial pressure
B. widening pulse pressure
Cushing triad: 3 manifestations due to ↑ICP or Herniation
: Systolic HTN (↑Pulse pressure), Bradycardia, & Abnormal respirations
•Cushing reflex is a set of three clinical manifestations (systolic hypertension, bradycardia, and abnormal respirations) related to pressure on the medullary area of the brainstem. These signs may occur in response to intracranial hypertension or a herniation syndrome. The appearance of Cushing reflex is a late finding that may be absent in patients with severe neurologic deterioration. Attention should be paid to alteration in each component of the triad and intervention initiated accordingly.
The nurse is caring for a severely head injured comatose patient who is dying. The practitioner asks to be notified when the patient starts to exhibit signs of Cushing reflex. The nurse would call the practitioner when the patient starts to show which signs?
A. Bradycardia, systolic hypertension, and widening pulse pressure
B. Tachycardia, systolic hypotension, and tachypnea
C. Headache, nuchal rigidity, and hyperthermia
D. Bradycardia, aphasia, and visual field disturbances
A. Bradycardia, systolic hypertension, and widening pulse pressure
Cushing triad: 3 manifestations due to ↑ICP or Herniation
: Systolic HTN (↑Pulse pressure), Bradycardia, & Abnormal respirations
•Cushing reflex is a set of three clinical manifestations (systolic hypertension, bradycardia, and abnormal respirations) related to pressure on the medullary area of the brainstem. These signs may occur in response to intracranial hypertension or a herniation syndrome. The appearance of Cushing reflex is a late finding that may be absent in patients with severe neurologic deterioration. Attention should be paid to alteration in each component of the triad and intervention initiated accordingly.
The patient is ordered a CT scan with contrast. Which question should the nurse ask the conscious patient before the procedure?
A. are you allergic to penicillin?
B. are you allergic to iodine-based dye?
C. are you allergic to latex?
D. are you allergic to eggs?
B. are you allergic to iodine-based dye?
The nurse is caring for a patient who has just had a cerebral angiogram. Which intervention should be part of the nursing management plan?
A. Ensuring that the patient is adequately hydrated.
B. Maintaining the patient on an NPO status.
C. Administering antibiotics to the patient.
D. Keeping the patient flat in bed for 24 hours
A. Ensuring that the patient is adequately hydrated.
Nursing management priorities
Preparing the patient psychologically
•Teaching and answering questions as they arise
Preparing the patient physically
•Positioning the patient
Monitoring the patient’s responses to the procedure
•Observing for pain, anxiety, or hemorrhage
Assessing the patient after the procedure
•Observing for complications
•Medicating for discomfort
The nursing management plan for a patient undergoing an oil-based contrast myelogram should include intervention?
A. maintain the patient flat in bed for 4 to 8 hours
B. observe the puncture sight every 15 minutes for 2 hours for signs of bleeding.
C. keep the patient's head elevated 30 to 45 degrees for 8 hours.
D. administer a sedative to keep the patient from moving around.
A. maintain the patient flat in bed for 4 to 8 hours
The nurse is caring for a patient with an intracranial pressure monitoring device that provides access to CSF for sampling. Which type of device does the patient have?
A. Subarachnoid bolt
B. Epidural catheter
C. Intraventricular catheter
D. Fiberoptic catheter
C. Intraventricular catheter
Monitoring sites (Fig 16-7)
Intraventricular space
Subarachnoid space
Epidural space
Subdural space
Intraparenchymal space

The patient was admitted with a head injury and an intracranial pressure (ICP) monitoring device was placed. The nurse knows to notify the practitioner if what type of wave start to appear on the monitor?
A. A waves
B. B waves
C. C waves
D. D waves
A. A waves
A waves: Baseline of 20 or more, increased to 30-69, for 2-20min.
•Cause: vasodilation, ↑ CBF, ↓ venous outflow, fluctuations in PaCO2, ↓ CSF absorption
•Prolonged increased ICP associated with plateau waves may result in transient & permanent cell damage from ischemia
A critical care patient is diagnosed with massive head trauma. The patient is receiving brain tissue oxygen pressure (PbtO2) monitoring. The nurse recognized that the goal of this treatment is to maintain PbtO2:
A. > 20 mm Hg
B. < 15 mm Hg
C. between 15 and 20 mm Hg
D. between 10 and 20 mm Hg
A. > 20 mm Hg
Brain tissue oxygen pressure (PbtO2)
•Reliable cerebral oxygenation (Normal: 23-35mmHg)
•PbtO2 < 20: compromised brain O2 & intervention to be considered
•Complications: microtrauma, invalid values 30min-2hr p placement
What sites can be used for monitoring ICP? (SATA)
A. Intraventricular space
B. Epidural space
C. Jugular vein
D. Subdural space
E. Parenchyma
A. Intraventricular space
B. Epidural space
D. Subdural space
E. Parenchyma
Monitoring sites (Fig 16-7)
Intraventricular space
Subarachnoid space
Epidural space
Subdural space
Intraparenchymal space
A patient has been admitted with acute confusion and other focal neurologic signs. The practitioner performed a lumbar puncture. Which result is an abnormal finding? (SATA)
A. Fluid is clear and colorless
B. Glucose of 20 mg/dL
C. Protein of 20 mg/dL
D. Bloody fluid in first sample only
E. Pressure of 250 mm H2O
B. Glucose of 20 mg/dL
E. Pressure of 250 mm H2O
Pressure, Color, Blood, Volume, Specific gravity, WBCs, Glucose, Chloride, Culture & sensitivity, Serology for Syphilis, Protein, Osmolality, Lactate
•Bacterial meningitis: ↑ protein, ↓ glucose
•Viral meningitis: no changes in protein & glucose
•
•Normal protein in CSF: 15-60mg/dL
•Normal glucose in CSF: 50-80 mg/100 mL
Which of the following best describes B waves?
A. Plateau-shaped waves considered significant because of the reduced cerebral perfusion pressure (CPP) associated with ICP
B. Sawtooth-shaped waves associated with permanent cell damage from ischemia
C. Sawtooth-shaped waves that are normal in any patient but are amplified in states of low intracranial compliance
D. Small, rhythmic waves related to normal fluctuations in respiration and arterial pressure
C. Sawtooth-shaped waves that are normal in any patient but are amplified in states of low intracranial compliance
A waves: Baseline of 20 or more, increased to 30-69, for 2-20min.
Cause: vasodilation, ↑ CBF, ↓ venous outflow, fluctuations in PaCO2, ↓ CSF absorption
Prolonged increased ICP associated with plateau waves may result in transient & permanent cell damage from ischemia
B waves: Sawtooth appearance, 5-70, q 30sec-2min.
Normal physiologic phenomenon but amplified in low cranial compliance.
Cause: fluctuations of cerebral blood volume.
C waves: q 4-8min, normal fluctuations in respiration & systemic arterial pressure.