all of NURS116
1/1299
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
1300 Terms
Pharmacology
"study of medicines"
- 'pharmacon'= medicine/drug
- 'logos'= to study
purpose of Pharmacology
- cure
- relieve symptoms
- improve quality of life
Pharmacology (before 20th century)
used nature sourced remedies('medicine/treatment'). the 'active' ingredients were the thing that remedied ppl. ex:
- bark of Willow tree= aspirin(this is the 'active' ingredient in the tree)
bark of Willow tree
it's active ingredient:
- aspirin (treats pain & fever)

molds
it's active ingredient:
- penicillin (antibiotic. used to treat BACTERIAL infection)
Digitalis plant
it's active ingredient:
- digoxin (improves strength & efficiency of heart)

bark of Pacific Yew tree
it's active ingredient:
- taxol (drug used to treat cancer)

Pharmacology (after 20th century)
started synthetic('imitating') manufacturing of the 'active ingredients' in nature
- this allowed the drugs to be more precise, consistent, and controlled
Symptomology
bunch of symptoms that's shown on an individual.
- ex. fever: when someone has fever, we want to find & cure the UNDERLYING cause, not cure JUST the symptom('fever') itself
Pharmacotherapeutics
utilization of medicines('drugs') to heal or manage suffering of patient. to do so, we must know:
- what the drug does to our body
- compatibility of diff drugs ("can these 2 meds be taken at same time?")
how many prescription drugs/ year
500 000
- approx. 10/person
Pharmacotherapeutics (3 categories)
- Drug/ medication
- Biologic
- Natura; health product
Drug/ Medication
1/3 category of Pharmacotherapeutics
- a chemical agent
* a drug that's considered 'medically therapeutic' is referred to as= "medication"
Biologic (type of medication)
1/3 category of Pharmacotherapeutics
- naturally produced in animal cells
- CANT be taken orally! 'this' is usually injected
- ex. antibodies(ex. immunoglobulin), RBCs(blood donation), hormones(ex. insulin)
Natural Health Product (NHP)(type of medication)
1/3 category of Pharmacotherapeutics
- naturally occurring. used as adjunct('supplement'): therefore ppl usually don't consider 'these' as "meds"
- ex. vitamins, minerals(ex. Calcium), dietary supplements(ex. protein)
Canadian Pharmaceutical Association
publishes "compendium of pharmaceuticals & specialties"(CPS): compilation of drug info & all adverse('side effects') effects of the drug
- 'this' collaborates w Health Canada
Health Canada
regulates & is responsible for helping Canadians maintain and improve their health
how a new Pharmacotherapeutic('a drug used to treat/ help ppl') gets approved
1. research
2. laboratory (aka. preclinical trials): testing on non-humans
3. Clinical Trials Application to 'health canada' (CTA): 3 phases
4. New Drug Submission (NDS) to 'health canada'
5. if approved, NOC(notice of compliance) & DIN(drug ID) is assigned
6. drug monitored, ongoing by MHDP (marketed health product directorate) for adverse('side effect') reports
7. each province decides whether to add new drug or not & how drug cost is covered(insurance or no)
*NHP(natural health products) approval is NOT this stringent('strict/ precise'). doesn't go through all these steps
Clinical Trials Application to health canada (CTA)
clinical trials. 3 phases:
- phase 1: ~100 healthy volunteers
- phase 2: ~300
- phase 3: ~3000
*if serious adverse effect('side effect') on a volunteer, drug is cancelled!
*only 10% of new drugs going through 'approval process' make it to phase 3
New Drug Submission (NDS) to health canada
step after the clinical trials
- 80 new submission per year (only 10% is approved!)
SAP(special access program)
by Health Canada
- allows for not yet approved drugs to be used in special circumstances
Placebo
a substance that's 'said' to have an effect but in reality, it doesn't acc treat anything('no therapeutic value')
Declaration of Helsinki (2000)
states that Placebo can only be used in clinical trials when there's no proven effective treatment for the condition being studied
- if there's an anti-placebo(an acc effective treatment) that exists, u CANT USE PLACEBO (bc participants should receive best available treatment)
Pharmacotherapeutics (3 types of drug names)
3 types:
- Generic name
- Brand/ trade name
- Chemical name
Generic name
1/3 type of drug name
- a drug w/o a proprietary affiliation('ownership by a company')
- ONE 'this' per drug. same name throughout the world
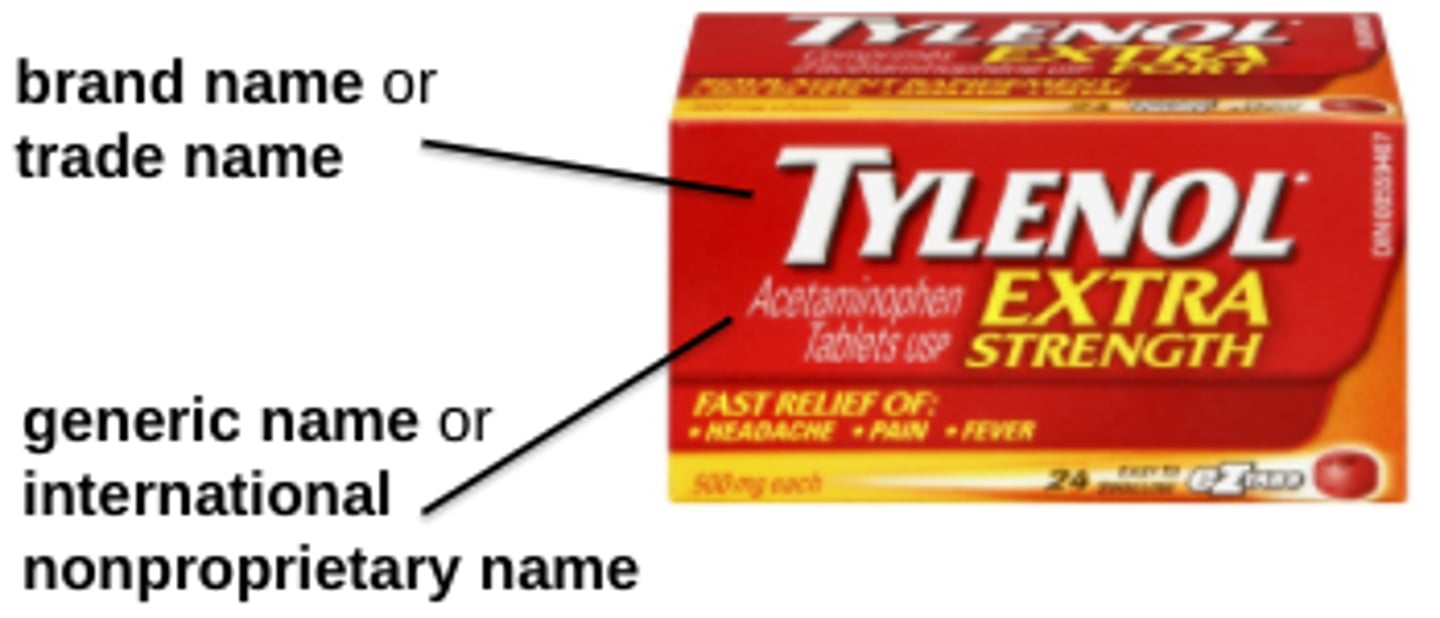
Brand/ Trade name
1/3 type of drug name
- named by the Manufacturing company (ex. advil)
- there's MANY 'this' per ONE generic drug name
- the manufacturing company of a drug first to market applies for 'patent protection': allows 20 years of selling the drug w no competitions
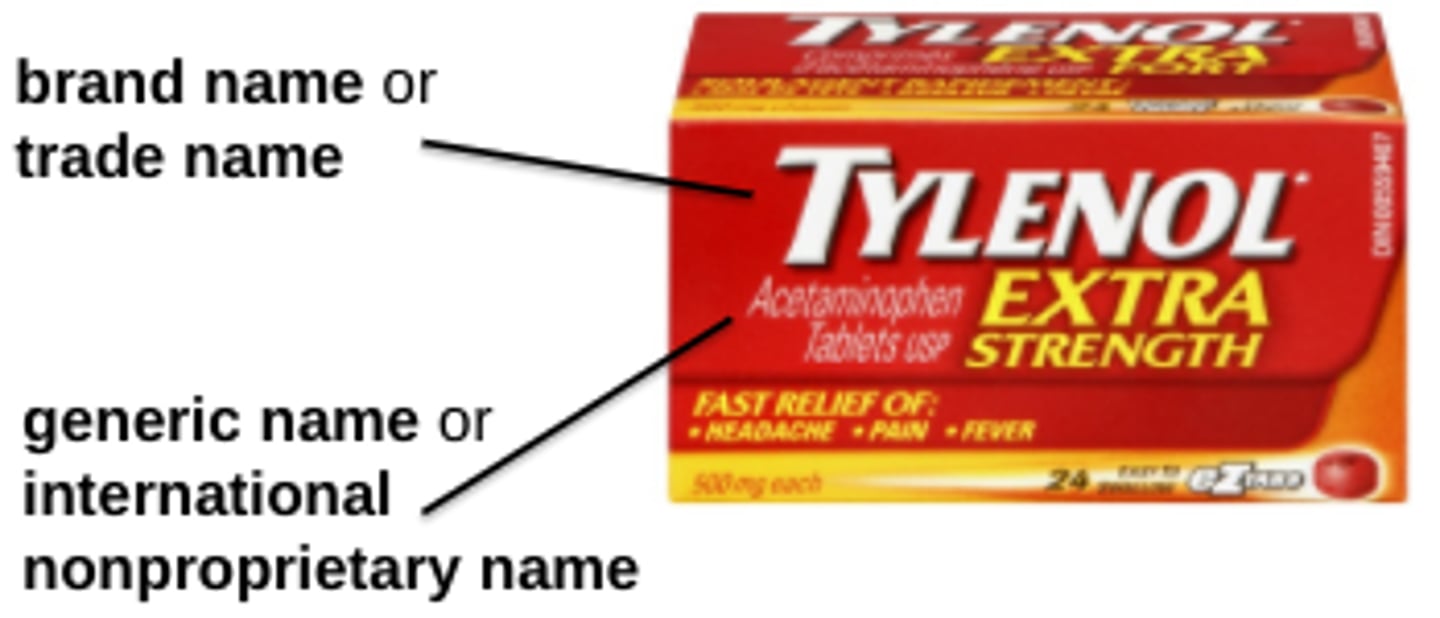
Chemical name
1/3 type of drug name
- the 'chemical composition' is the drug name
- name is assigned by IUPAC
- ex. Potassium Chloride
Generic vs Brand/Trade drugs
g: cheaper. cost is mostly covered by insurance
b/t: more expensive. mostly not covered by insurance
*when prescribing, they may substitute generic name if trade name is not available (and vise versa)
Bioequivalence
amount of drug in our body's circulation
- even if there's different non-active ingredients in Generic vs Brand drugs, the drug's effectiveness is not rlly affected
Prototype drug
usually the o.g drugs of that kind (1st one's to the market)
- 'these' aren't used that much anymore, but r the role models for future brand drugs
- also r role models to predict actions, adverse effects('side effects') of other drugs withing the same drug class
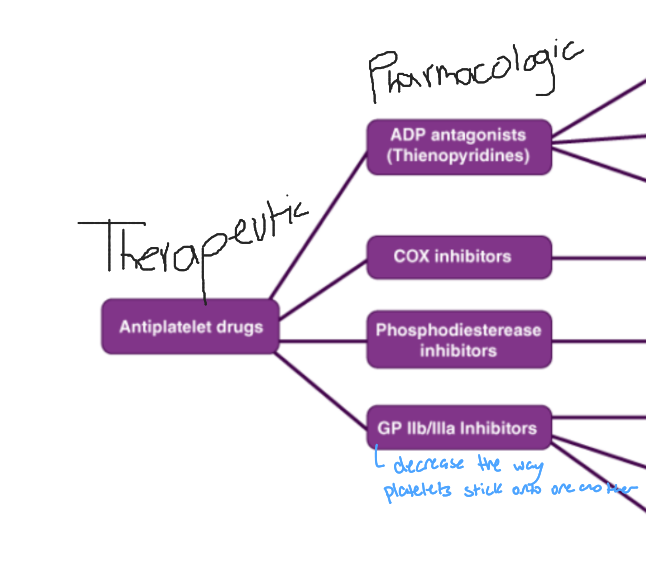
2 types of naming Drug Classes
- Therapeutic drug class nomenclature: less specific
- Pharmacological drug class nomenclature: more specific
Therapeutic drug class nomenclature
1/2 types of naming Drug Classes
- the name of this drug class states a treatment/therapy of a particular disease or disorder
- less specific ('this' can be further broken down by Pharmacological action)
- ex. antihypertensive (decreasing B.P)
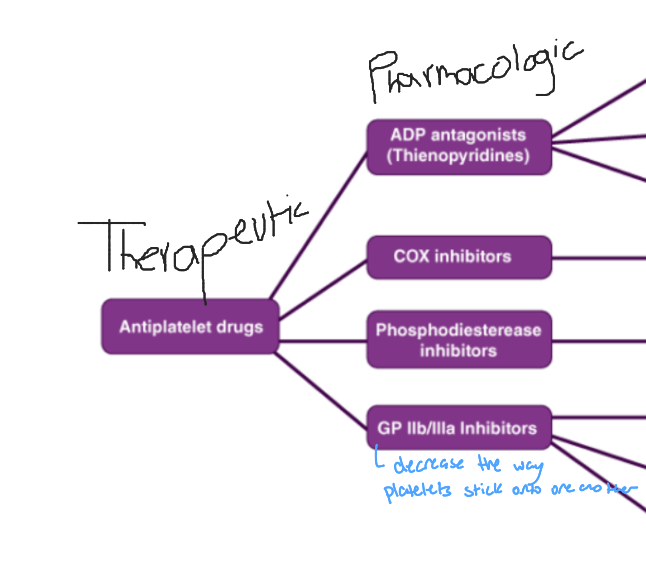
Pharmacological drug class nomenclature
1/2 types of naming Drug Classes
- the name describes the molecular/ receptor activity ('mechanism of action': how it works)
- more specific (mult of 'these' can be grouped into 1 therapeutic drug class)
- ex. calcium channel blocker (blocks Ca channels)
In Hospital settings all drugs are..
All drugs are PRESCIRBED for rigour('being rlly thorough/ accurate')
Schedule System (for drugs sold in Canada)
diff types:
- Schedule I: most restricted
- Schedule II
- Schedule III
- Unscheduled: least restricted
Schedule I
1/4 Schedule Sys for drugs in Canada
- drugs r only available w PRECRIPTION & provided w pharmacist
- All prescription drugs
- Controlled drugs(potential for addiction/ abuse) & Narcotic drugs r found in 'this' schedule
- Prescription is granted to specific healthcare professionals (depends on what meds)
- ex. Cannabis
Schedule II
1/4 Schedule Sys for drugs in Canada
- drug is available only from a pharmacist (u DONT need prescription)
- drug must be in an area w NO public access(bc these drugs can be addictive) (only pharmacists can get to it)
- ex. very strong iron pill
Schedule III
1/4 Schedule Sys for drugs in Canada
- drugs r available by open access in pharmacy/ pharmacy area (Over The Counter drugs= no prescription needed)
- drug can't be access by ppl if pharmacy's closed (bc pharmacist MUST BE PRESENT)
Unscheduled
1/4 Schedule Sys for drugs in Canada
- drug can be sold in any store w/o professional supervision (NO pharmacist needed)
- ex. any meds u can buy at a gas station
5 Essential steps of Nursing Process
1. Assessment (u do this throughout the WHOLE process. not just one step)
2. Diagnosis
3. Planning
4. Implementation (giving ppl meds)
5. Evaluation (assessing drug action & side effects)
Assessment (in Nursing Process)
1st step of Nursing Process (but u still do 'this' throughout the WHOLE process. not just one step)
- u do 'this' to find out what's wrong w someone
Implementation (in Nursing Process)
4th step of Nursing Process (aka. 'Intervention')
- 'this' step includes use of Pharmacotherapeutics(giving ppl med to treat/ manage the problem) (enhances or suppresses person's normal physiology)
- ALWAYS include Patient Education: teaching patient abt the new med
Evaluation (in Nursing Process)
5th(last) step of Nursing Process
- includes ASSESSMENT of drug action & drug side effects
- ex. tries giving 200mg. if it doesn't work, give 400mg next time.
one of patient assessment: Subjective data
we ask abt patient's Pharmacotherapy:
- Health history: we ask patient -> r u taking any Meds? Supplements? Vitamins?
- Chief (presenting) concern: we ask -> have u tried taking any meds for this concern?
- Personal & Social History: we ask -> do u do any recreational drug use(ex. alcohol, smoking)?
Drug administration
"giving of drug" via ex. orally, rectal, topical
- 'this' is diligent!(w care & thoroughly)
Drug administration (how to do it diligently)
nurses do so by:
- understanding pharmacotherapeutic goal (__ med to reduce swelling)
- specific monitoring: ex. drug blood serum/plasma/blood lvls. checking for blood glucose lvl
- monitoring for adverse effects('side effects')
- patient medication teaching: explaining drug treatment to the patient (but patient can refuse treatment)
Patient medication teaching
nurses ALWAYS explains the drug treatment to the patient
- after being educated, patient can refuse the drug treatment
6 Rights of Medication Administration
nurse asks herself 6 questions before administering any meds:
1. Right Patient
2. Right Drug
3. Right Dosage
4. Right Route
5. Right Time
6. Right Documentation
Right Patient
1/6 rights of medication administration
- "have I verified patient's identity w at least 2 identifiers?(ex. name, date of birth)"
Right Drug
1/6 rights of medication administration
- "did i check the med label against the prescription & patient's medication record?"
Right Dosage
1/6 rights of medication administration
- "did i confirm the correct dosage and measured it accurately?"
Right Route
1/6 rights of medication administration
- "am i administering the med by the correct route?(ex. oral, intramuscular)"
Right Time
1/6 rights of medication administration
- "am i giving the med at the correct time as prescribed?"
Right Documentation
1/6 rights of medication administration
- "did i document the med administration accurately in patient's record?"
drug Formulation
the way drug ingredients r prepared to be administered('given to patient'): has a specific form(ex. solid, liquid, injectable)
- just bc it's a liquid med, it DOESNT mean u can always inject it
drug Route of Administration
'the ways the drugs can be taken into body' (ex. oral, topical)
- 'this' is specified by drug Formulation
drug Route of Administration (depends on..)
depends on:
- medical situation: ex. emergency
- drug kinetics: do we want med to spread systemic or localized?
- drug formation availability: ex. same med but liquid vers might be out of stock and there's only tablet vers
- clinical setting
types of Routes of Administration
- Oral (PO)
- Sublingual (SL)
- Intranasal (insufflation)
- Inhalation + via Endotracheal(ET) tube
- Topical
- Transdermal
- Rectal
- Intravenous (IV)
- Intramuscular (IM)
- Subcutaneous
- Implanted ports(?)
Oral (PO) administration
1/11 Route of Administration
- med taken by MOUTH
- aka. Enteral (bc drug passes through GI tract)
- ex. liquid, tablet/pills, powder
- most COMMON
- most CHALLENGING in regards to drug Kinetics: dependent on acidic env, peristalsis, drug entering portal circulation (liver) first
- SYSTEMIC EFFECT
Enteric coated Tablet/Pill
this means the drug will make it to SMALL INTESTINE before it starts dissolving
- WONT dissolve in stomach
drug Kinetic in Oral drugs
'this' is most challenging for PO drugs bc:
- drug is dependent on ACIDIC env('stomach'): ex. aspirin needs that low pH to dissolve. but if patient took Tums= pill won't work properly
- dependent on PERSITALSIS: if patient has bad peristalsis= constipated= drug stays in GI tract longer= drug will be absorbed more (vise versa for ppl w diarrhea)
- drug enters '1st pass metabolism' (portal circulation (liver)): it reduces the amount of active drug reaching the bloodstream
Enteral feed
feeding a patient by a tube into GI tract
Nasojejunal Tube (NJ tube)
- tube begins @nose
- tube extends till @jejunum
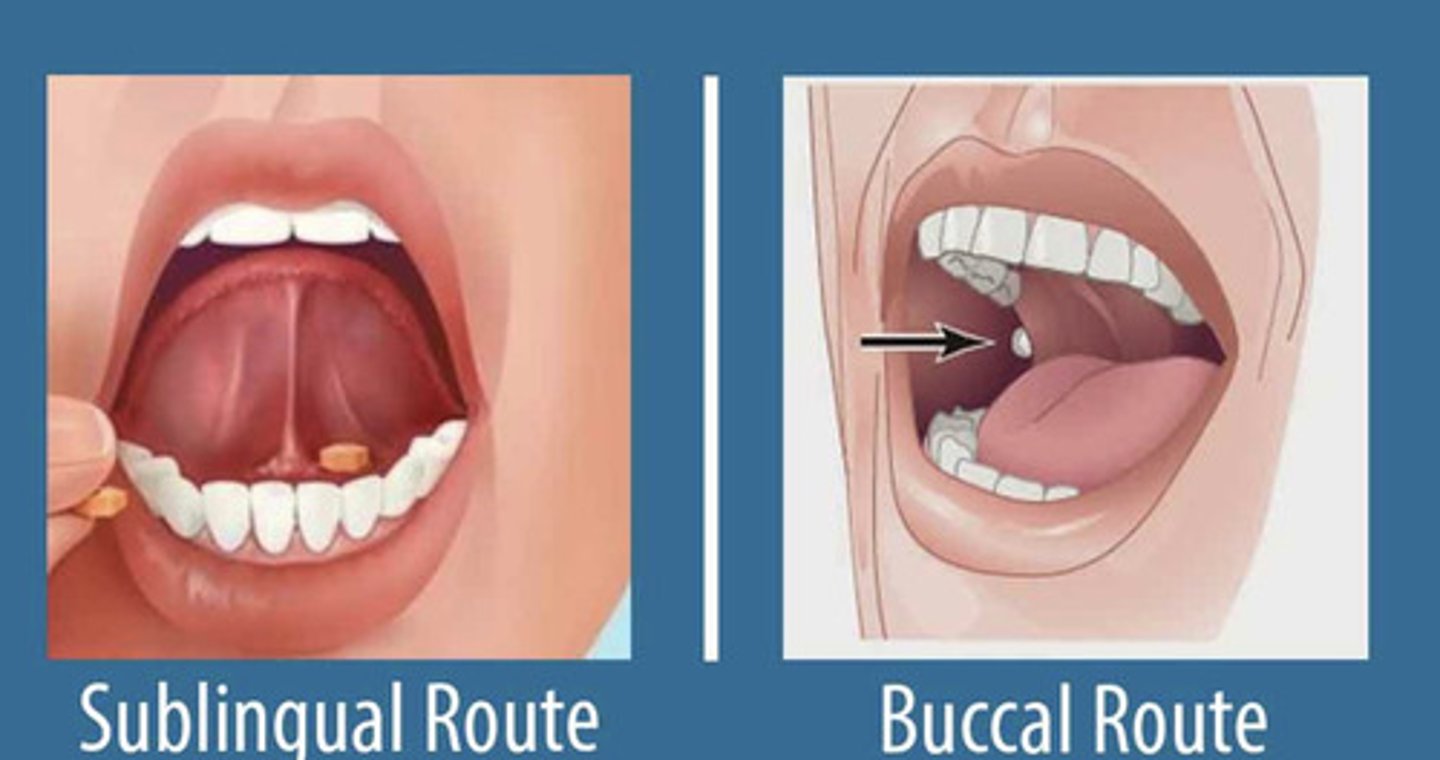
Sublingual (SL) administration
1/11 Route of Administration
- med taken UNDER the TONGUE
- drug is absorbed into capillary -> into bloodstream
- BYPASSES GI tract & 1st pass metabolism(liver)
- acts FASTER than PO(oral)
*oral mucosa may be damaged if u take too much 'this' method

Buccal absorption
placing pill into ur cheek pocket
- cheek is more muscular= thicker wall than under tongue= pill must be able to get absorbed better
Intranasal (insufflation) administration
1/11 Route of Administration
- meds taken into NASAL CAVITY
- 'this' allow drugs to travel through cap., cranial nerve(ex. olfactory & trigeminal), and BBB
- can be LOCALIZED or SYSTEMIC effect (depends on the drug's formation + molecular characteristics)
Intranasal (insufflation): localized & systemic ways
intranasal administration can have:
- LOCAL (nasal mucosa) effect: ex. Rhinocort spray. ~30% mf med ends up systemic tho
- SYSTEMIC effect: ex. Flu vaccine(sprayed into nose)
- high CNS effect: ex. cocaine (lipophilic. small. travels along Cranial Nerve and reaches CNS)
Inhalation administration
1/11 Route of Administration
- meds inhaled into LUNGS
- lungs= super vascular= drugs in pulmonary cap has a RAPID effect
- can be LOCALIZED or SYSTEMIC effect(depends on drug's molecular characteristics)
Inhalation: localized & systemic ways
Inhalation administration can have:
- LOCAL effect: ex. asthma drugs. a % still ends up in systemic circulation tho
- SYSTEMIC effect: ex. general anesthesia drugs (we want it to spread sys. so it reaches brain. we use Endotracheal tube for it)
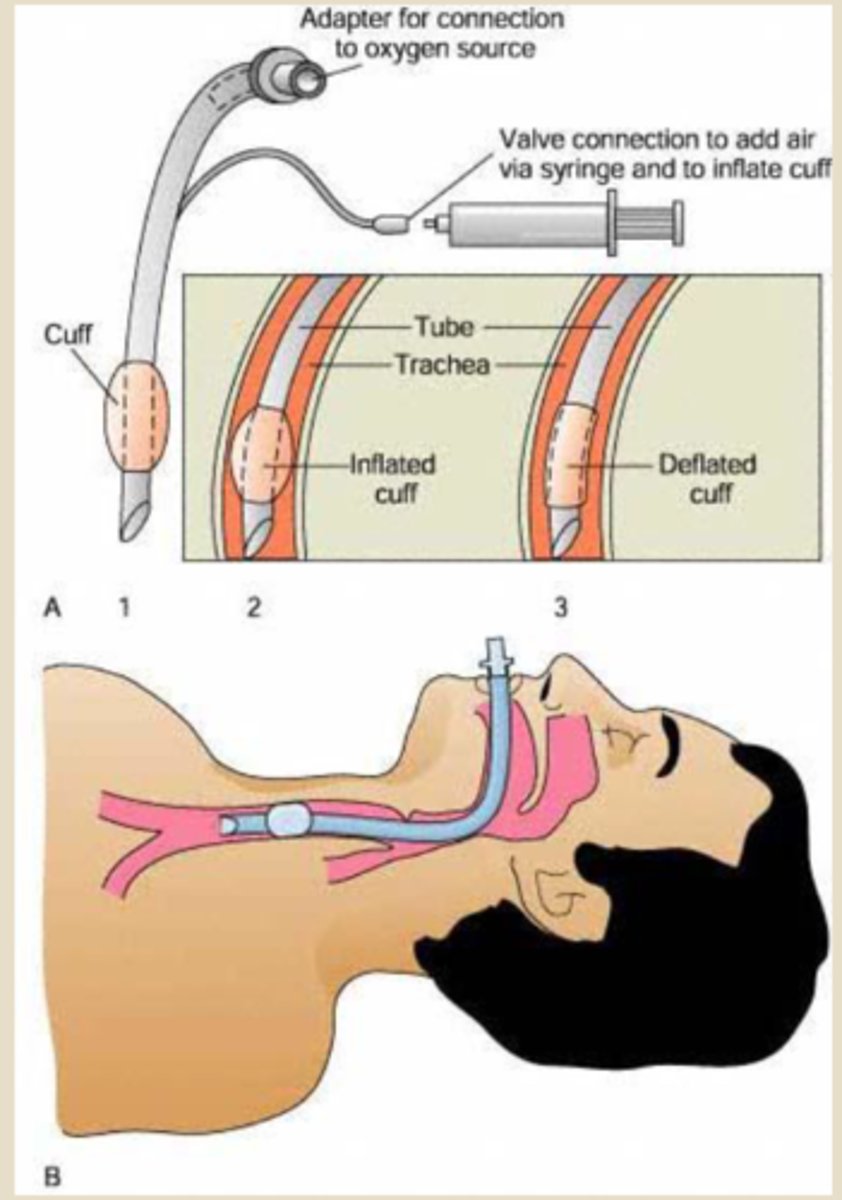
Endotracheal (ET) tube
we usually use 'these' for ER & ICU situations. the tube goes into Trachea
- bigger tube: gives O2. airbags can attach
- smaller tube: can administer drugs (ex. epinephrine) here. only few drugs can be administered this way
Topical administration
1/11 Route of Administration
- applied directly to a SURFACE (ex. skin/eye creams, ointments)
- LOCAL effect
- many molecules of 'these' drugs r too large(>500daltons) to penetrate all skin layers= minimal systemic presence
Tropical administration (caution!!)
the systemic presence can be contraindicated('harmful')
- ex. Retinoid creams (wrinkle treatment): local effect. has low systemic effect BUT we advise against using it during pregnancy bc it can be contraindicated!
Transdermal administration
1/11 Route of Administration
- med that's applied as a 'PATCH'
- dermal cap absorption: drug molecule must be small enough to penetrate skin layers
- SYSTEMIC effect
- longer acting: SLOW & steady release & absorption
- ex. nitroglycerine, nicotine, morphine patch, hormone treatment
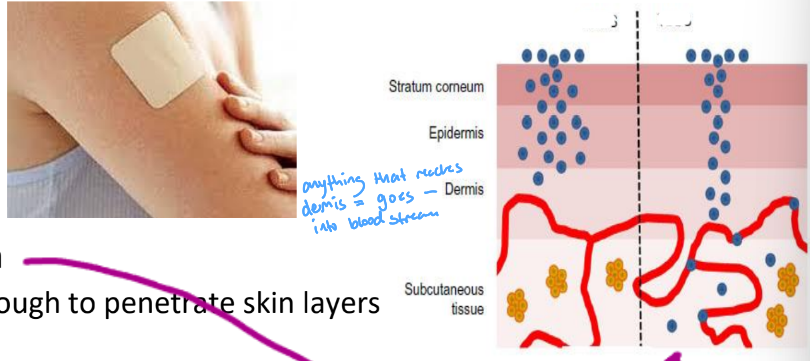
Dalton
expresses molecule size of drug
- <500 Dalton: topical cream is absorbed more into body= increased systemic circulation
- >500 Dalton: less topical cream is absorbed into body
Rectal adminstration
1/11 Route of Administration
- med is inserted into RECTUM
- LOCAL or SYSTEMIC effect
- 50-75% of 'these' bypasses 1st pass metabolism(liver)
- systemic effect is unreliable= bc there's many factors affecting it
Rectal: localized & systemic ways
Rectal administration can have:
- LOCAL effect: ex. glycerin suppository (given when constipated. has a bit that goes to systemic circulation)
- SYSTEMIC effect: ex. morphine suppository (given when u want whole body's pain gone)
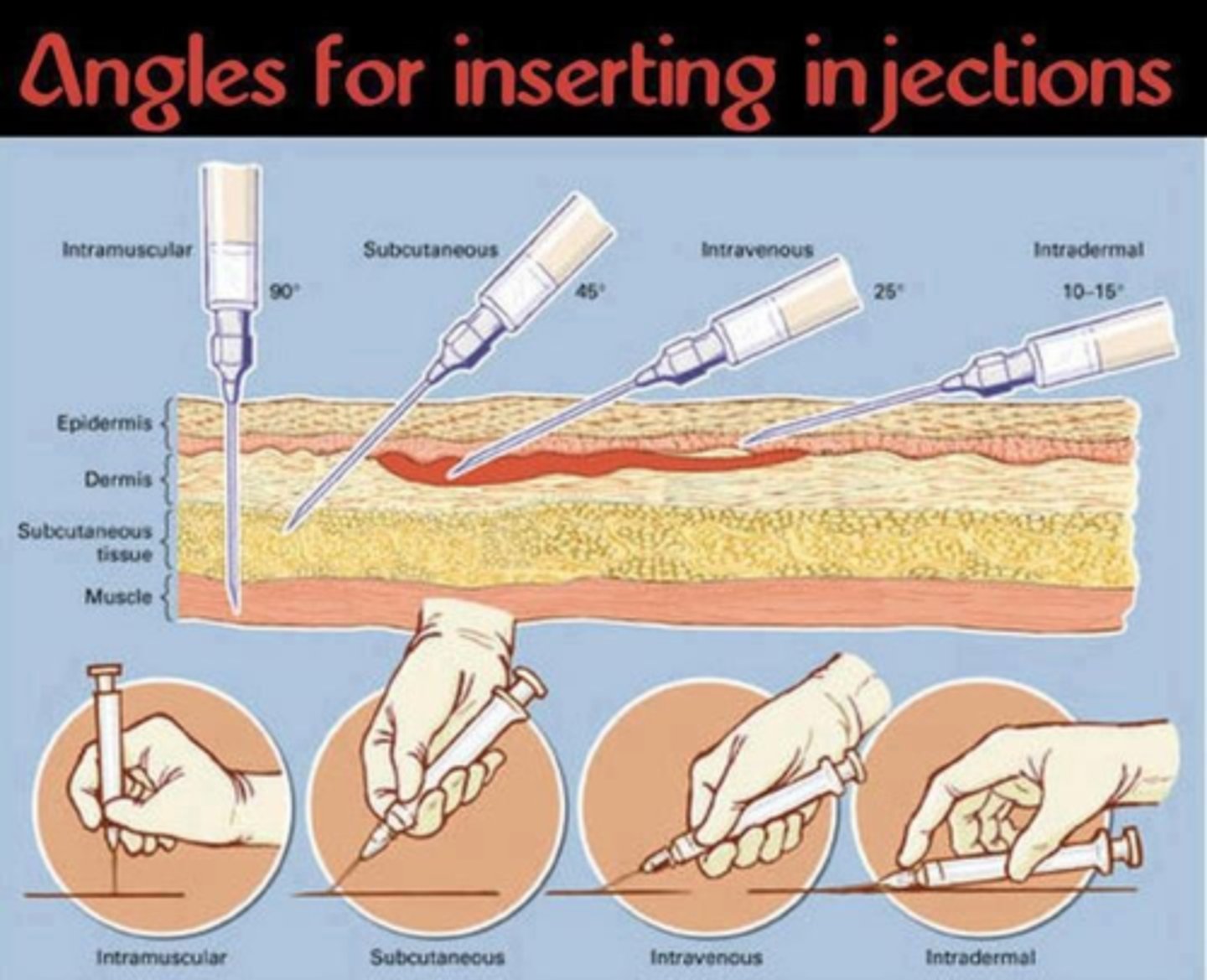
Parenteral administration routes
these administration all require an INJECTION
- ex. Intravenous (IV), Intramuscular (IM), Subcutaneous (SC), Implanted ports
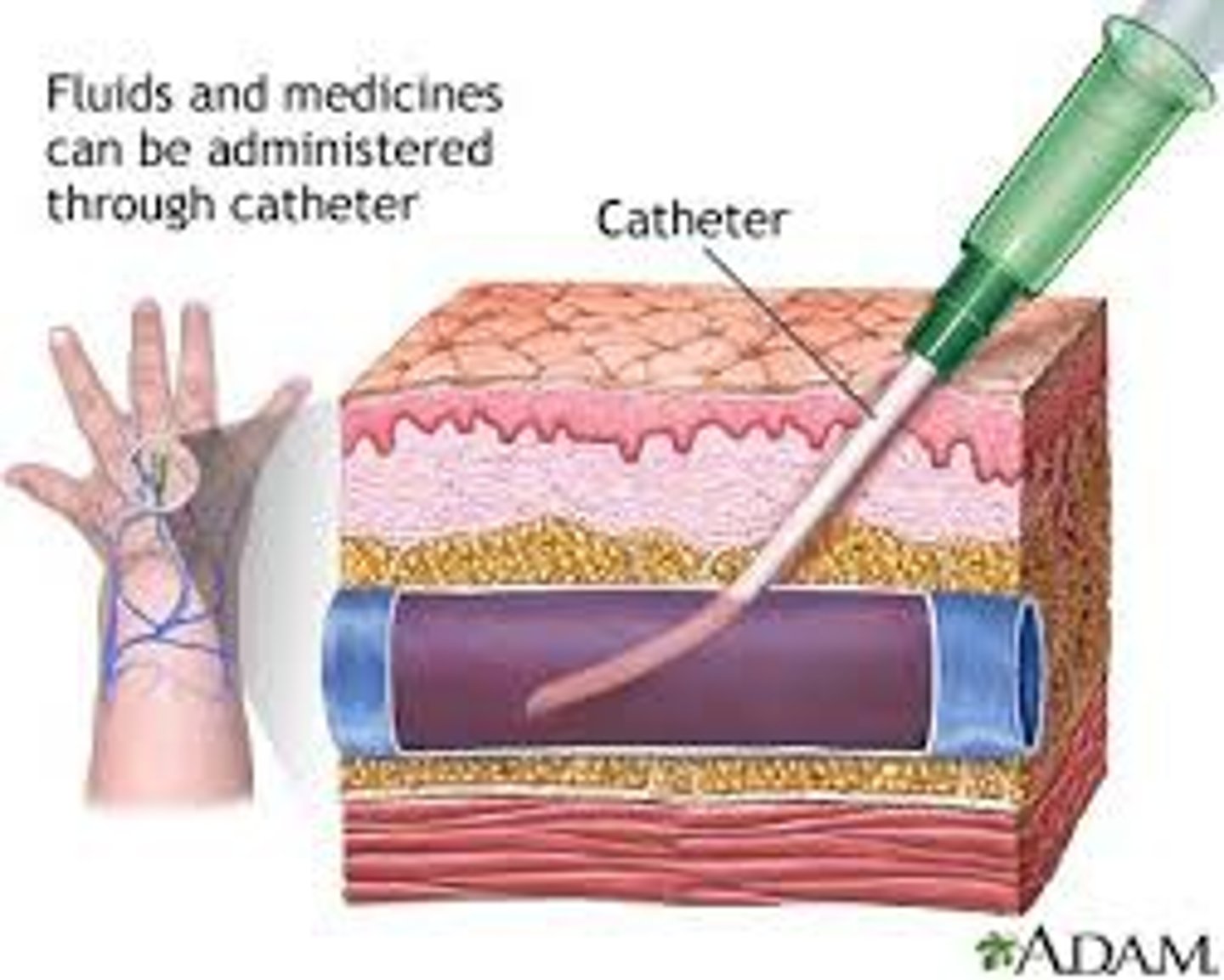
Intravenous (IV) administration
1/11 Route of Administration
- needle-catheter into a VEIN
- IMMEDIATE absorption= fast onset of action
- amount of dose given = amount of dose circulating to receptors
- SYSTEMIC effect
- common in hospital settings
- 'expensive': bs u need professional to inject IV's
- INFECTION risk (esp immunocompromised ppl)
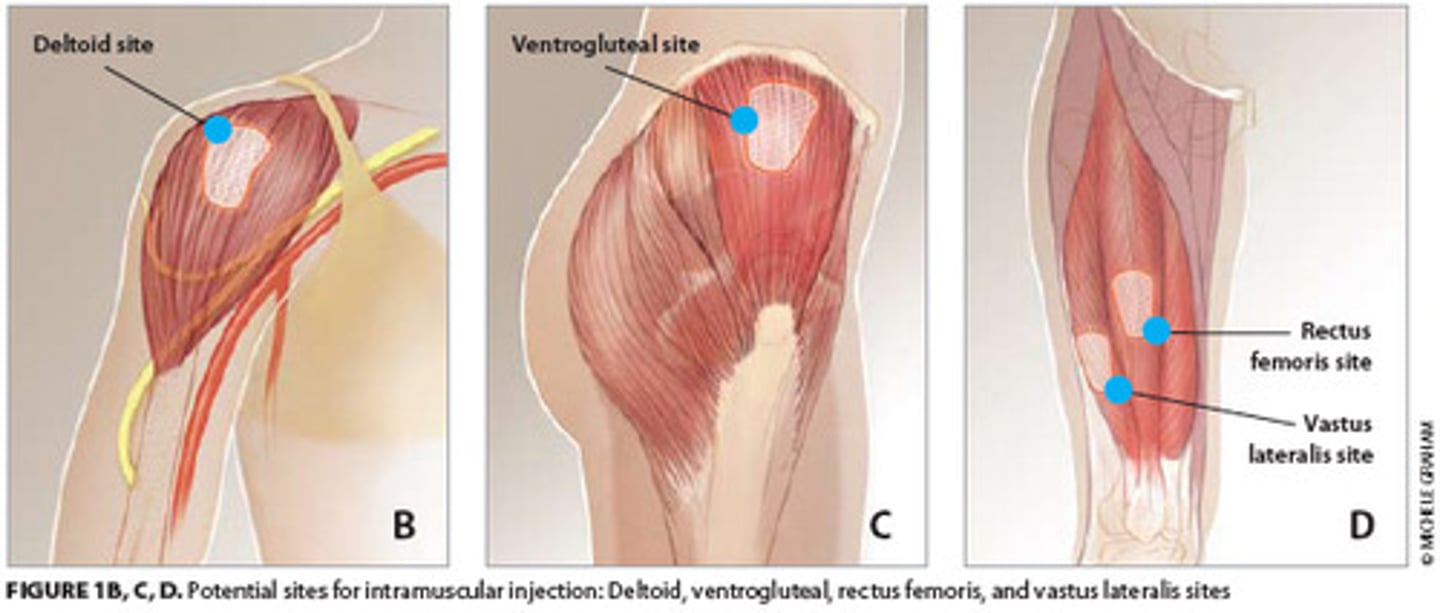
Intramuscular (IM) administration
1/11 Route of Administration
- needle injection into MUSCLE TISSUE
- can have aqueous(faster effect) or depot(slower effect. sustained release) preparation
- absorbed into cap bed -> goes into bloodstream
- SYSTEMIC effect
- painful
- ex. flu & covid vaccines, Epipens
Intramuscular (IM) injection sites
inject at:
- Deltoid site
- Ventrogluteal site
- Rectus femoris site
- Vastus lateralis site
*Dorsolateral (NOT recommended)
Bioavailability
'how much of drug acc reaches SYSTEMIC CIRCULATION?'
- IV route has 100% 'this'
- Oral route doesn't have 100% of 'this'
Extensively 1st pass Metabolized drugs
"large portion of these drugs r metabolized in the liver= causes rlly low bioavailability. only a lil bit of drug is available to make acc therapeutic affect"
Extensively 1st pass Metabolized drugs (examples)
include:
- Morphine
- Meperidine (brand name: Demerol)
- Diazepam (brand name: Valium)
- Midazolam
- Lidocaine (NOT given orally!(PO))
- Propranolol
- ETOH (alcohol)
- Nitroglycerine (NOT given orally(PO))
- THC (an active compound in cannabis)
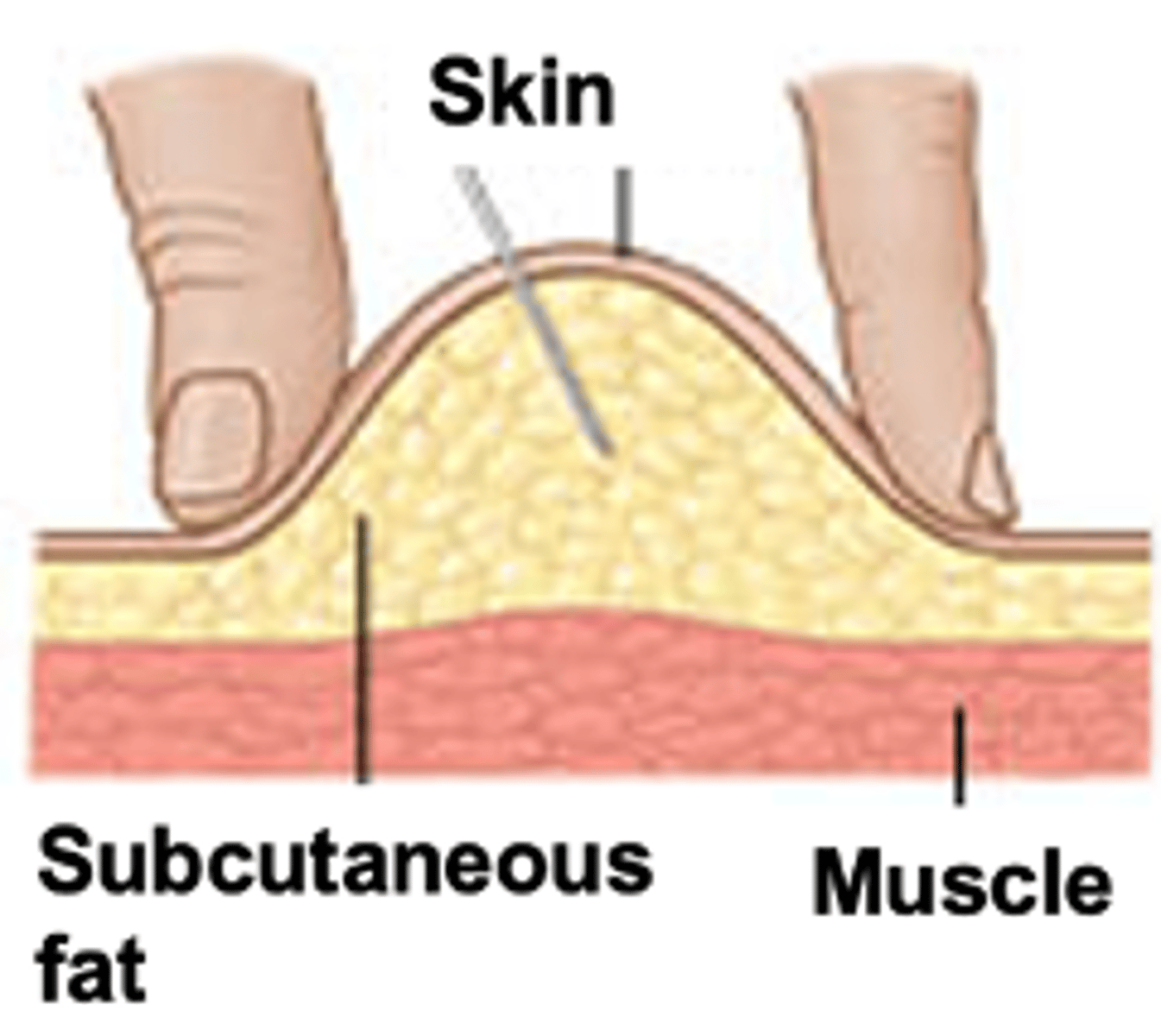
Subcutaneous (SC) administration
1/11 Route of Administration
- injects into ADIPOSE tissue of hypodermis('subcutaneous')
- absorbs into capillary bed -> systemic circulation
- can have fast or slow onset (depends on drug prep)
- ex. insulin
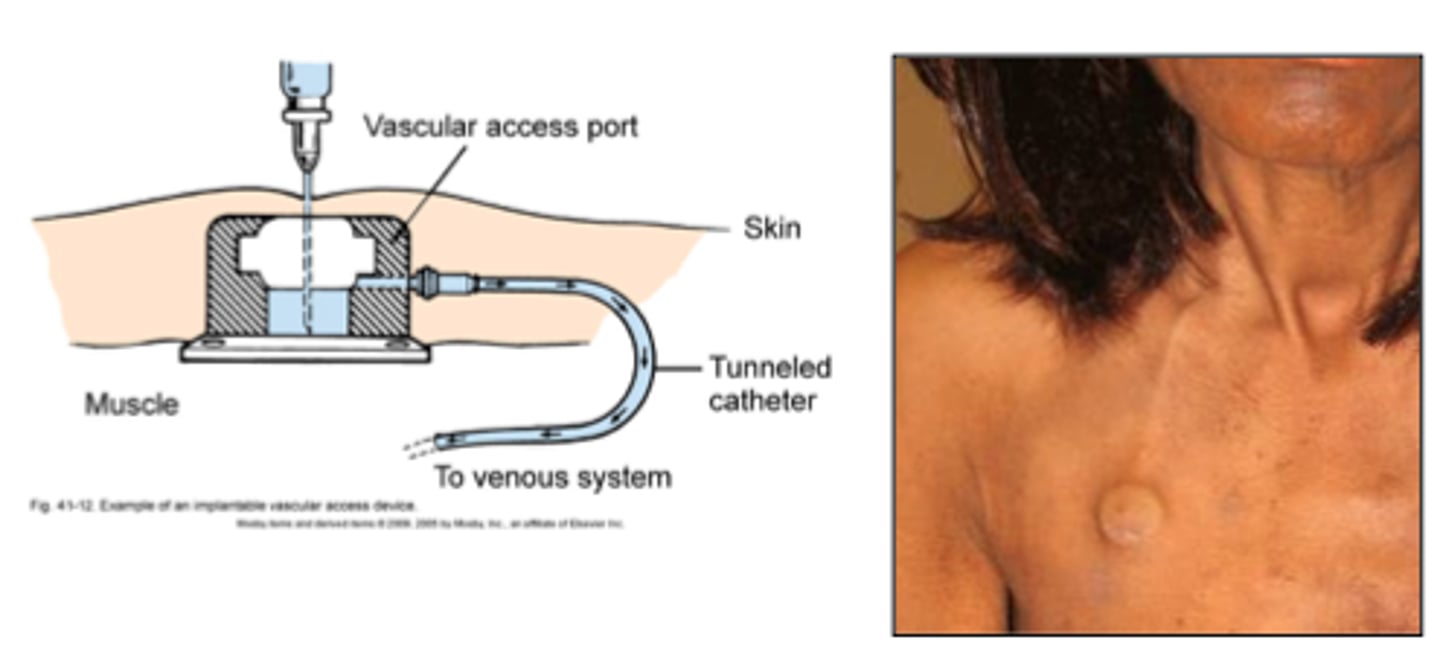
Implanted ports
1/11 Route of Administration
- used for long term injection
- drug usually injects into subclavian vein
- must maintain patency('keeping hole open & clear'): uses flushing w solution (so hole isn't blocked by blood clot or debris)
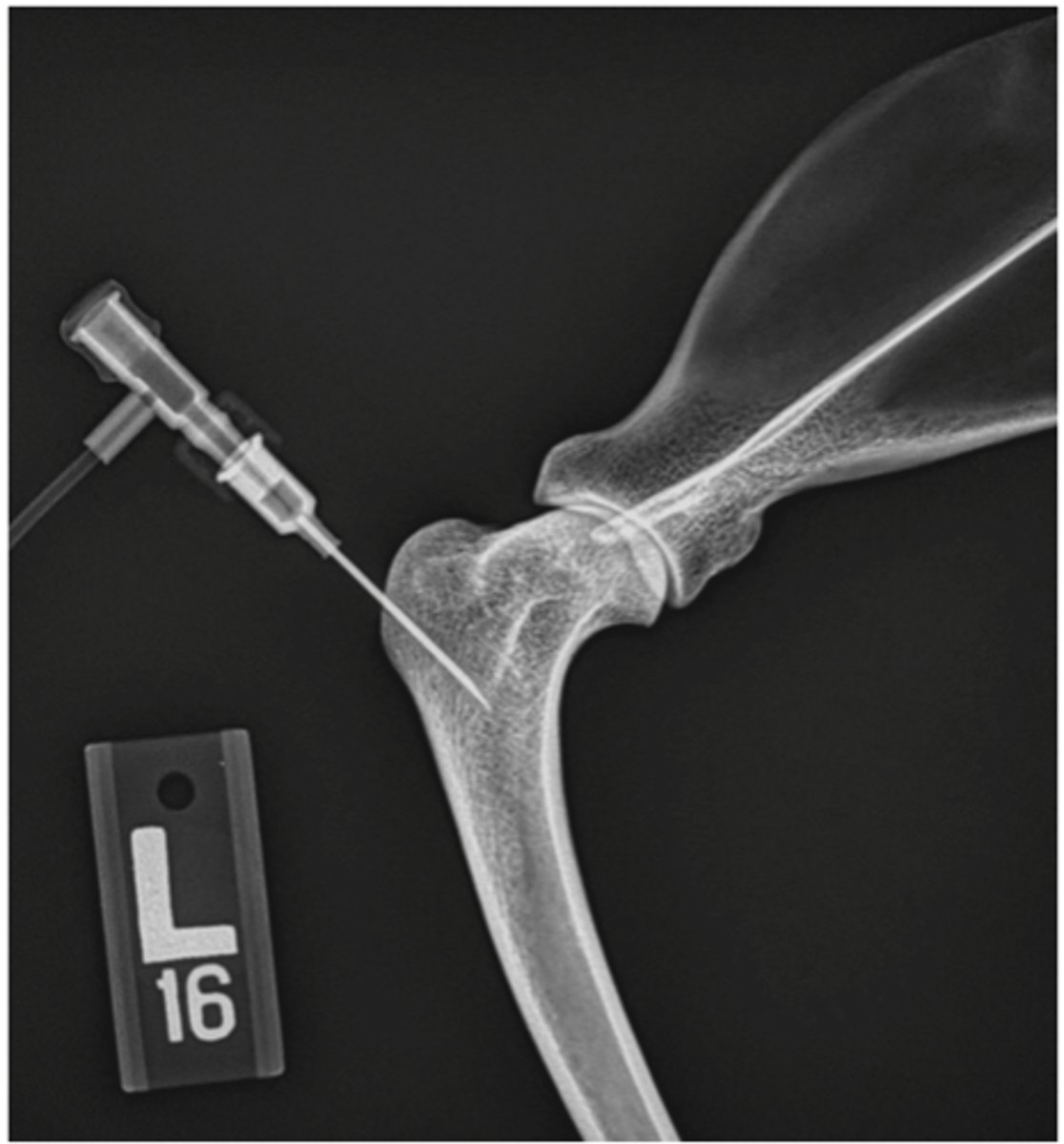
Intraosseous administration
1/11 Route of Administration
- used in EMERGENCY situations (ex. hemorrhagic shock: low B.P= vein collapsed= can't inject IV= must inject med through 'this' way)
- uses drill-like needle to inject into bone (proximal end of tibia)
ac
before meals
ad lib
as desired/directed
bid
twice per day
cap
capsule
/d
per day
gtt
drop
hs
hour of sleep/ bedtime
no
number
pc
after meals; after eating
PO
by mouth; orally
PRN or prn
when needed/ necessary
q
every
qd
every day
qh
every hour