OTH 5430 – Exam 2 Study Material: Osteoarthritis (OA) and Rheumatoid Arthritis (RA)
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
107 Terms
Rheumatic diseases are commonly referred to as ______.
"arthritis" = joint and inflammation
more than 100 conditions are classified as rheumatic diseases
What are rheumatic diseases characterized by? What part of the body does it affect?
chronic pain, progressive physical impairment
affects joints, skin, muscles, ligaments, and/or tendons
T or F: Rheumatic diseases are the leading causes of disability.
true
What are the different types of rheumatic diseases?
OA
RA
Lupus
Ankylosing spondylitis
Scleroderma
Gout
Fibromyalgia
T or F: OTs are more likely to see clients with rheumatic diseases as a primary or secondary condition. To recognize problem areas and plan effective intervention strategies, the occupational therapist should know the unique features of each disease, its underlying pathology, and its typical clinical findings; the therapist should also be familiar with commonly prescribed medications and their adverse reactions.
true
Osteoarthritis (OA): Etiology
-most common RD
-affects 33% of working adults in the US
-affects all races and ethnic groups
-blacks and hispanics report twice the prevalence of work limitation and pain vs whites
-risk increases with age!!! (onset later in life)
-number one reason for physician visits for individuals 65 years and older
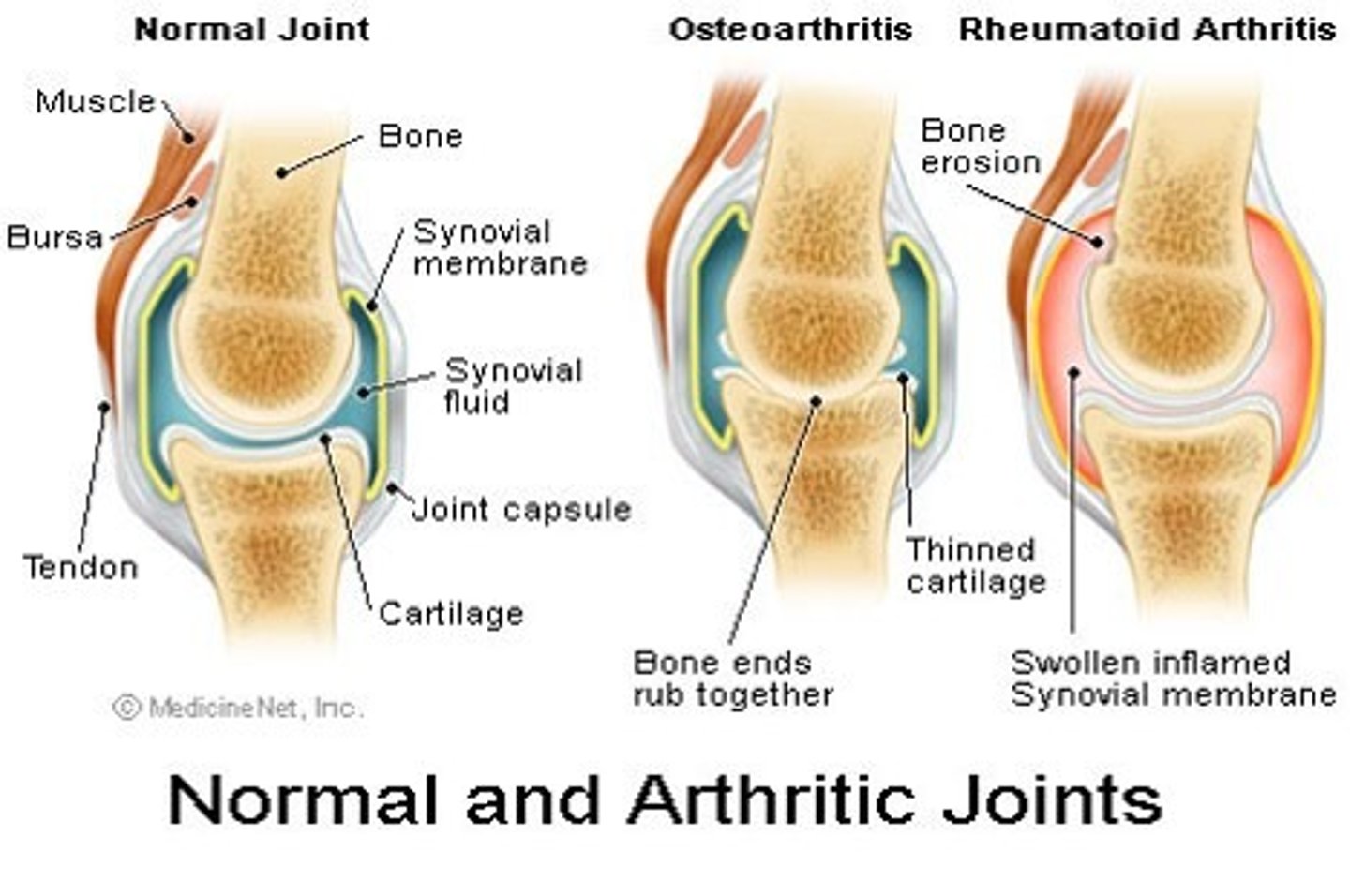
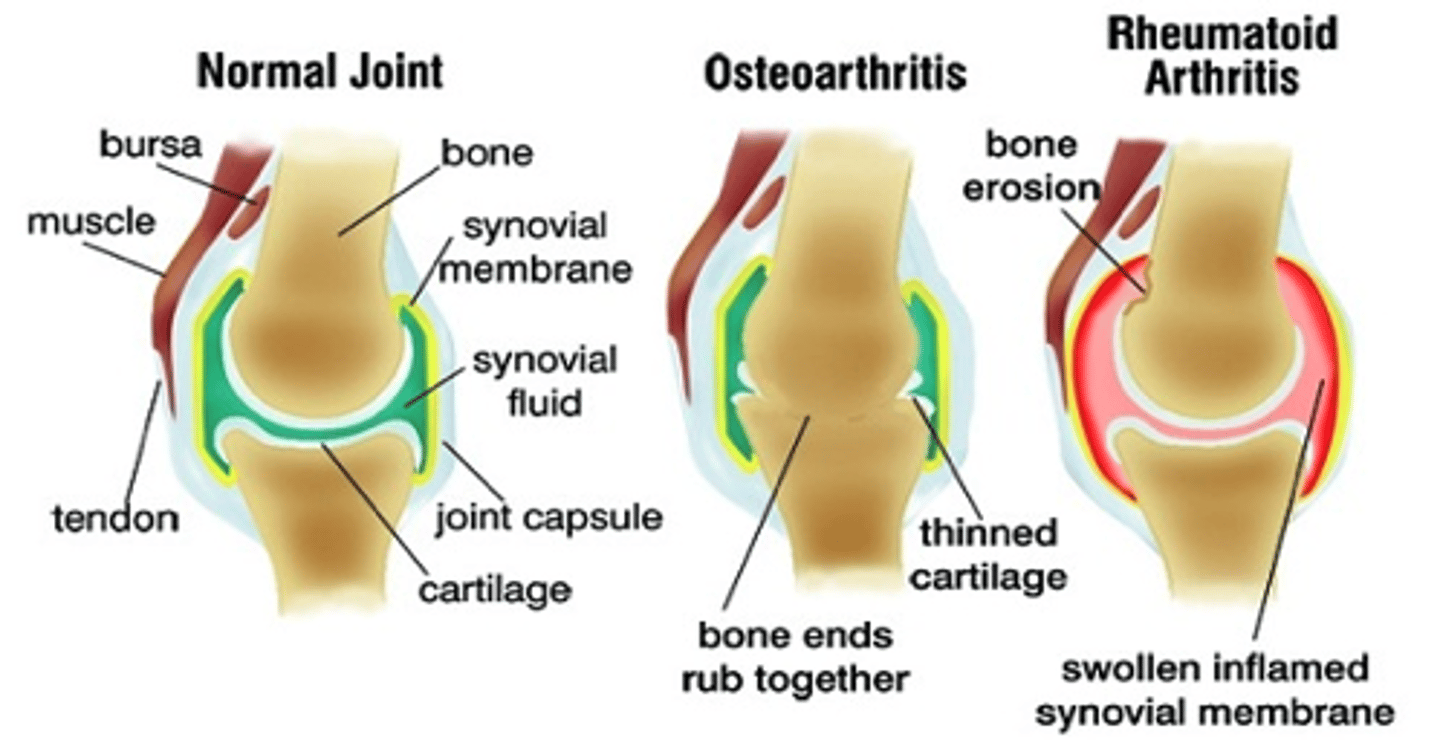
OA vs RA
Osteoarthritis
-individual joints
-non-inflammatory
-21 million
-incidence increases with age
-slow onset
-morning stiffness resolves in 20-30 mins
-NO redness, warmth
-responds to heat
-asymmetrical
Rheumatoid arthritis
-systemic
-inflammatory
-2 million
-40-60 years, females
-sudden onset
-morning stiffness persists for ~1 hr
-redness, warmth
-does not respond to heat
-symmetrical
What is gelling?
Stiffness and limited motion after inactivity
morning stiffness
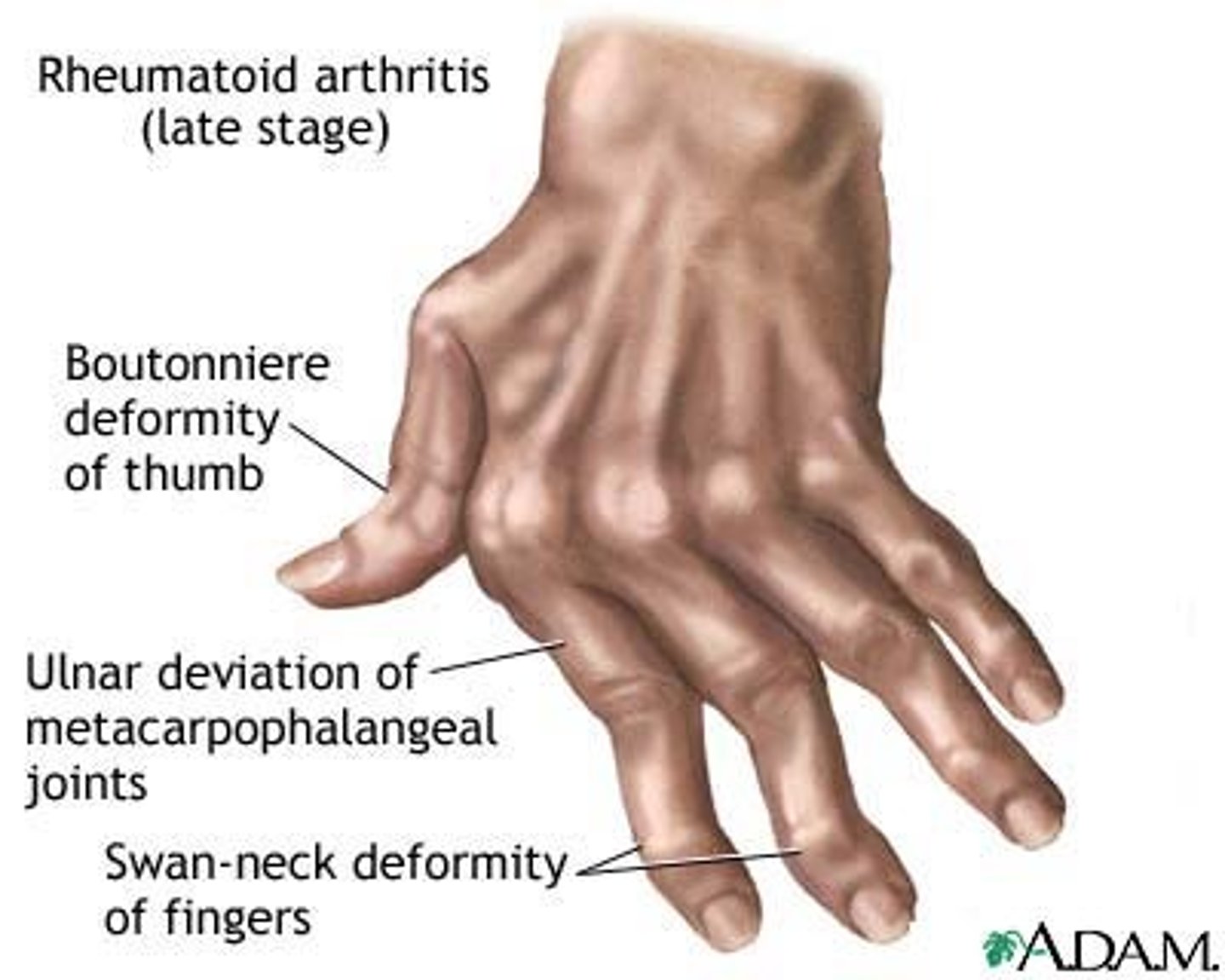
OA vs RA: Joint damage
Osteoarthritis
-bone on bone (bone rubs together)
-thinned cartilage
-fusiform swelling of joints
-heberden's nodes
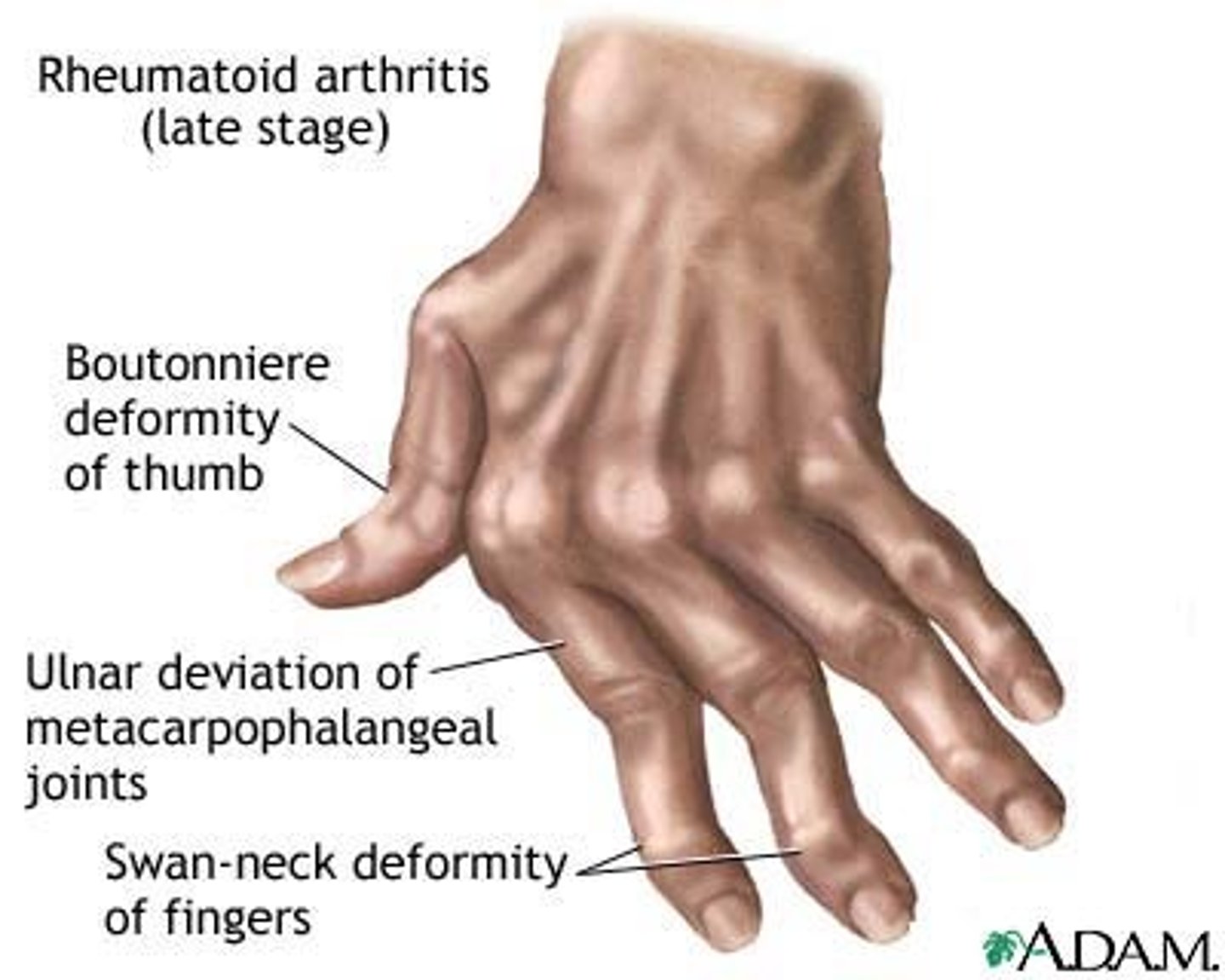
Rheumatoid arthritis
-bone erosion
-swollen inflamed synovial fluid
-ulnar drift of MCPs, boutonniere deformity of thumb, swan neck deformity of fingers
is OA inflammatory or non-inflammatory?
non-inflammatory
is RA inflammatory or non-inflammatory?
inflammatory
What is osteoarthritis?
-most common type of degenerative joint disease (DJD)
-strongly correlated with age (almost everyone over 65 has some cartilage damage)
-also associated with heredity, obesity, anatomical joint abnormality, injury, overuse, and repetitive movements
-non-inflammatory
-breakdown of cartilage in the joints leading to joint pain and stiffness
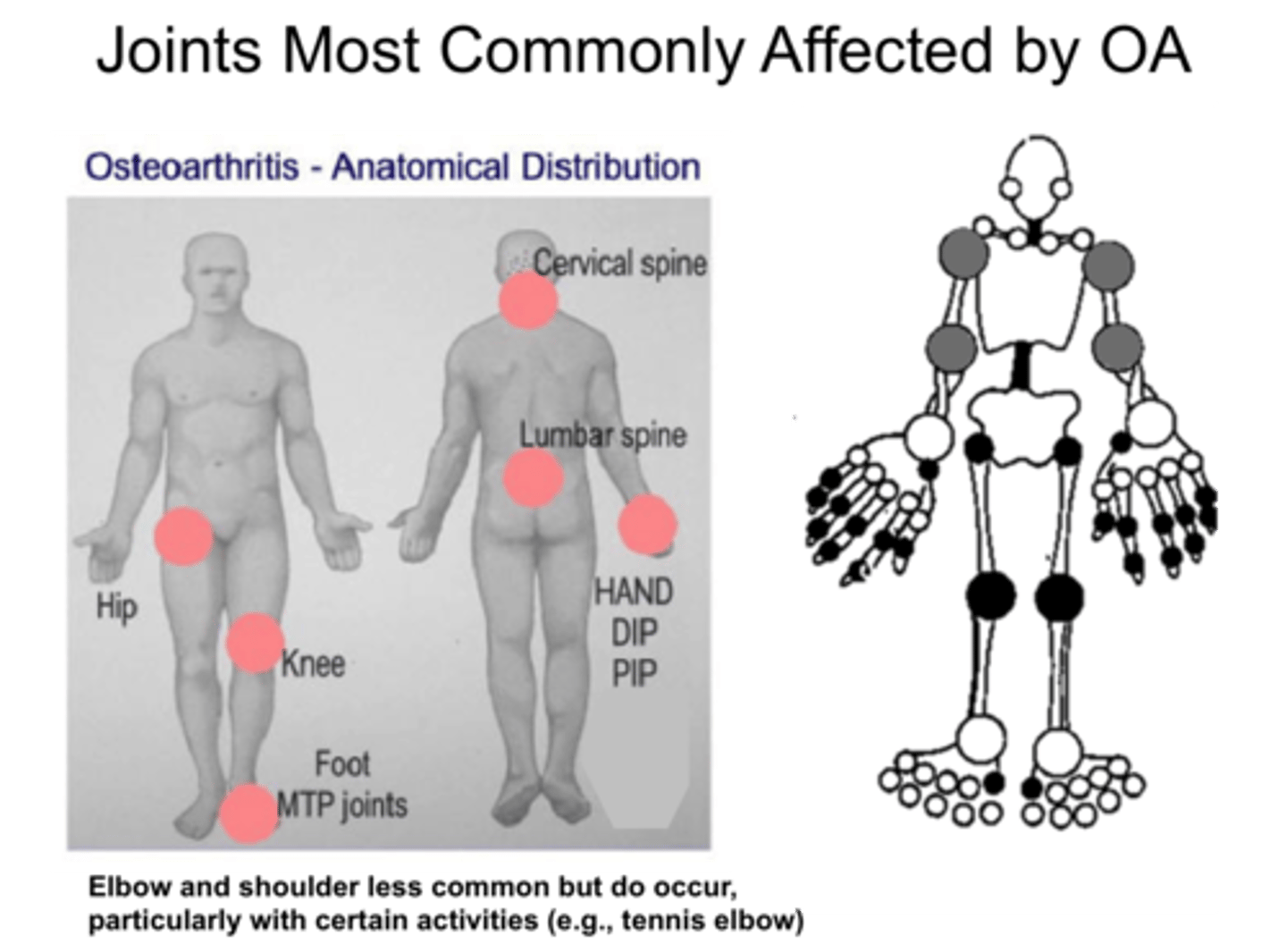
-affects specific joints (hands, hips, knees, spine) and may arise on both sides of the body
-minimal or not present warmth, swelling, and joint redness
-morning stiffness for ~20 mins
-absent systemic symptoms
What are the clinical features of OA?
pain
stiffness
tenderness
limited movement
variable degrees of local inflammation
crepitus
reduced ROM (with crepitus and hard end feel)
OA affects which joints
-hand: DIP, PIP, thumb CMC
-cervical and lumbar spine
-feet: MTP
-knees, hips
Is OA a 2-part process?
yes
1) deterioration of articular cartilage
2) new bone formation
steps
-cartilage softens, loses elasticity
-large sections wear away
(reduced spaces, bone-on-bone contact)
-osteophytes from as ends of bones thicken
-cysts may form, cartilage particles float in joint space
T or F: OA is classified as either primary or secondary
true
What is primary OA?
-no known cause (idiopathic)
-may be localized (involvement of one or two joints) or generalized (diffuse involvement, three or more joints)
more common
What is secondary OA?
-related to an identifiable cause
-due to trauma, anatomic abnormalities, infection, or aseptic necrosis
less common
How is OA diagnosed?
patient history
x-rays
MRI
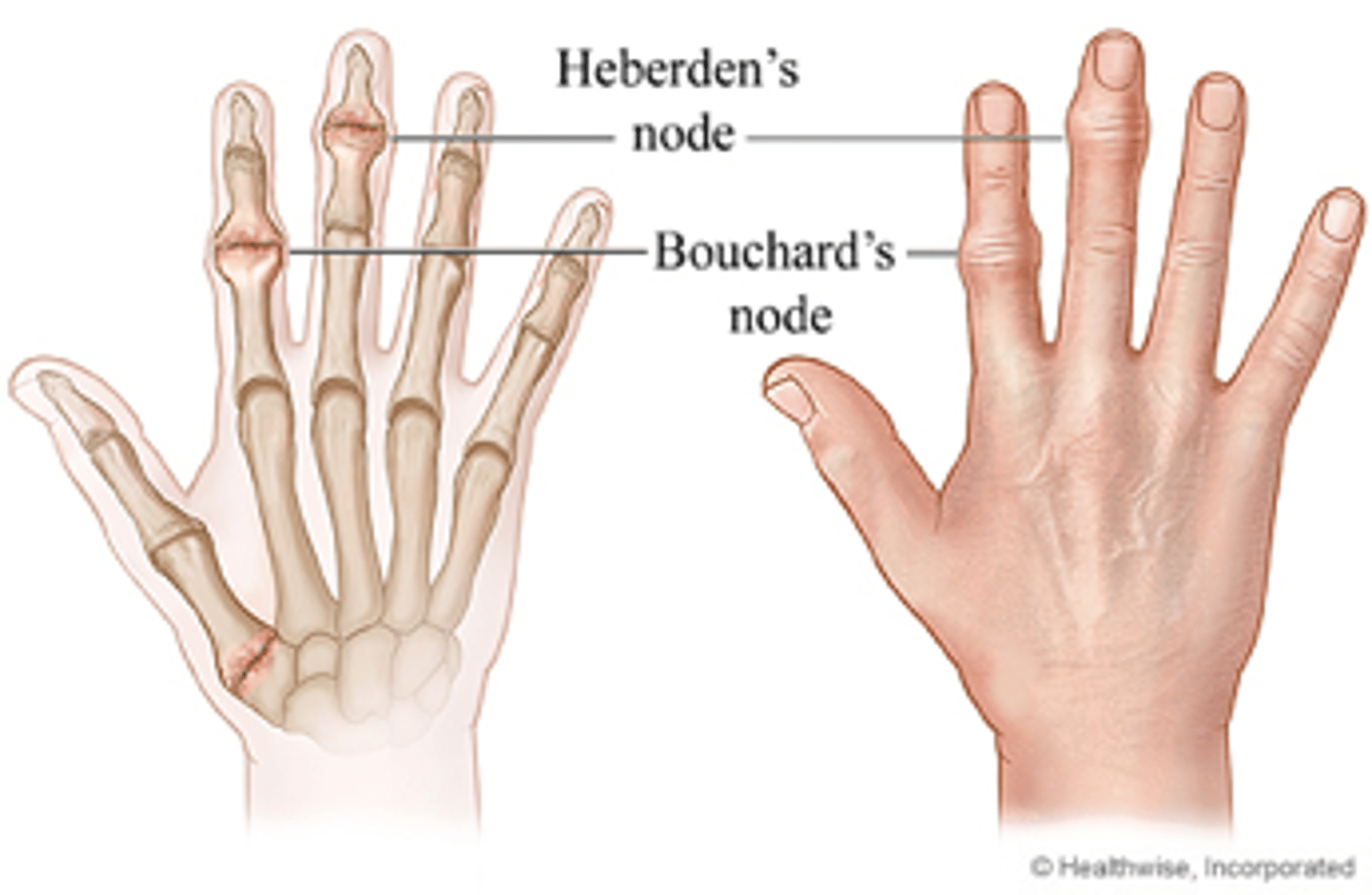
What characteristics are noted in the hands with OA?
heberden's nodes - DIP
bouchard's nodes - PIP
thumb CMC
How is OA medically managed? What are the treatment goals?
treatment goals = relieve symptoms, improve function, limit disability, avoid drug toxicity
medications may target system or local joints
-pain relievers: narcotics, non-narcotics (can affect tx i.e. drowsy, nauseous, constipated)
-anti-inflammatory meds: provide pain relief, decrease local joint inflammation
-risk of GI and kidney complications
-nonpharmacological agents (herbal remedies)
How is OA surgically managed?
arthroscopic joint debridement, grafting, fusion, replacement
How is OA treated?
positioning - splints (static splints for rest and support)
pain management
joint protection techniques
increase function
What is rheumatoid arthritis?
-chronic, systemic inflammatory condition with an onset earlier in life
-develops suddenly or within weeks or months (insidious onset)
-affects many joints: wrists, elbows, shoulders, mainly smaller joints on both sides of the body
-warmth, swelling, and joint redness is common
-morning stiffness lasts longer than OA (longer than 1 hr
-systemic symptoms are present
Rheumatoid arthritis (RA): Etiology
-onset is earlier
-yet-unknown trigger causes an autoimmune inflammatory response in the joint lining of a genetically predisposed host.
-peak incidence occurs between 40 and 60 years of age
-rate of disease two to three times higher in females
T or F: RA manifests itself as synovitis, which is inflammation of the synovial membrane that lines the joint capsule of diarthrodial joints.
true
Is RA symmetrical or asymmetrical?
symmetrical
What are the clinical features of RA?
-symmetric pain and swelling, prolonged morning stiffness (1 hr +), malaise, fatigue, and low-grade fever
-PIP, MCP, and thumb joints, wrist, elbow, ankle, MTP, and temporomandibular joints (jaw); the hips, knees, shoulders, and cervical spine
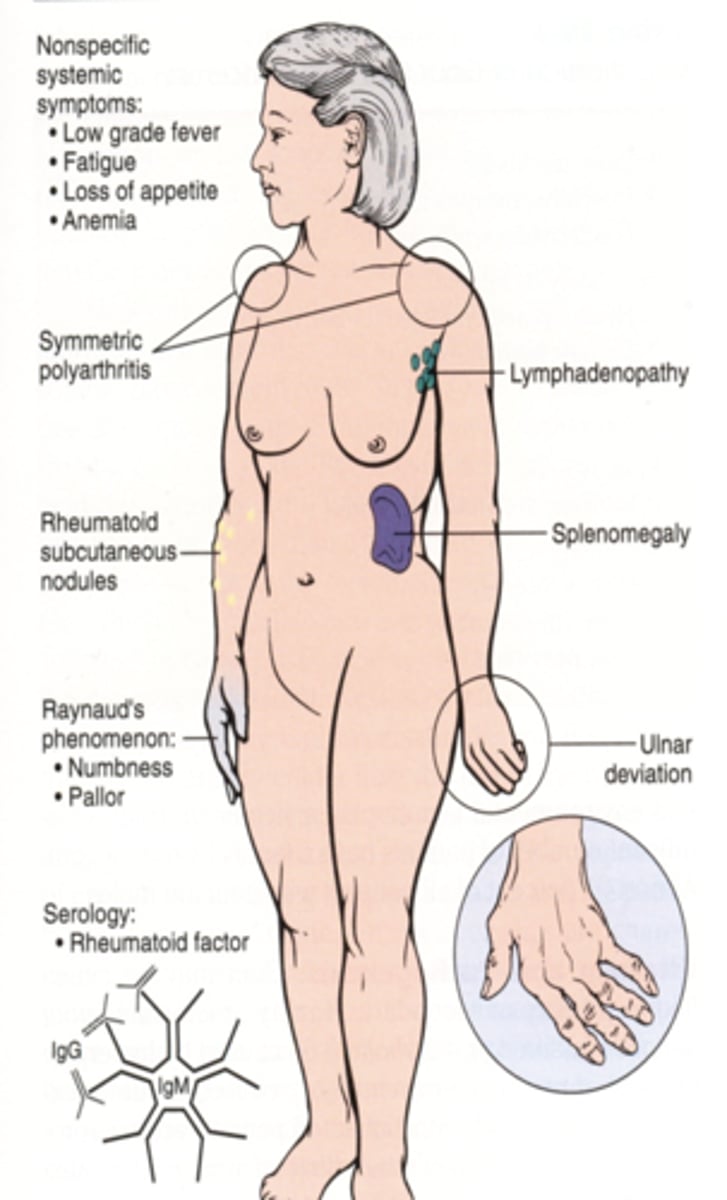
What are the classic external S&S of inflammation (in RA)?
heat
edema
erythema (redness)
pain
___________, a cutaneous manifestation of RA, develop in 25% to 30% of persons with RA during periods of increased disease activity.
rheumatoid nodules
With RA, pain can be acute or chronic. When do these occur?
Acute pain occurs during disease exacerbations, or flare-ups. Chronic pain results from progressive joint damage.
What is the diagnostic criteria for RA?
-morning stiffness greater than 1 hour
-arthritis of 3 or more joint areas
-arthritis of hands
-symmetrical arthritis
-rheumatoid nodules
-RH factor
-x-ray changes
Edema and no deformities noted are indicative of what stage of RA?
RA early stages
Ulnar drift and joint deformities are indicative of what stage of RA?
RA late stages
How many stages are in the inflammatory process of RA?
1) acute stage
2) subacute
3) chronic active
4) chronic inactive
What are the signs and symptoms of the acute stage in RA?
inflammation
red, hot joints
pain and tenderness at rest that increase with movement
weakness, tingling, or numbness
overall stiffness
limited motion
What are the signs and symptoms of the subacute stage in RA?
inflammation subsides
warm, pink joints
decreased pain and stiffness
limited movement and tingling remain
stiffness limited to the AM
What are the signs and symptoms of the chronic active stage in RA?
minimal inflammation
less pain and tenderness
increased activity tolerance
low endurance
stiffness remains
What are the signs and symptoms of the chronic inactive stage in RA?
no inflammation
pain and stiffness – result from disuse
low endurance – result from disuse
overall functioning may be decreased as a result of fear of pain, limited range of motion (ROM), muscle atrophy, and contractures
Which of the following symptoms is characteristic of the acute stage of rheumatoid arthritis (RA)?
A) Crepitus
B) Hard end feel with reduced ROM
C) Red, hot joints
D) Pain that decreases with movement
C) Red, hot joints
Which of the following symptoms is characteristic of the subacute stage of rheumatoid arthritis (RA)?
A) Red, hot joints
B) Severe pain and stiffness throughout the day
C) Warm, pink joints with decreased pain
D) Hard end feel with reduced ROM
C) Warm, pink joints with decreased pain
Which of the following symptoms is characteristic of the chronic active stage of rheumatoid arthritis (RA)?
A) Severe inflammation with red, hot joints
B) Less pain and tenderness with minimal inflammation
C) High endurance with no stiffness
D) Severe pain and limited activity tolerance
B) Less pain and tenderness with minimal inflammation
Which of the following symptoms is characteristic of the chronic inactive stage of rheumatoid arthritis (RA)?
A) High levels of inflammation with red, hot joints
B) Pain and stiffness, limited range of motion (ROM), muscle atrophy, and contractures due to disuse
C) High endurance and full range of motion (ROM)
D) Severe pain and increased muscle strength
B) Pain and stiffness, limited range of motion (ROM), muscle atrophy, and contractures due to disuse
What is the clinical course of RA? From best to worst.
-single episode of acute inflammation (best)
-periodic episodes of exacerbations
-low-grade symptoms
-progressive with exacerbation and remission (deformities continue to develop)
-rapid unrelenting (worst - chronic, extreme pain)
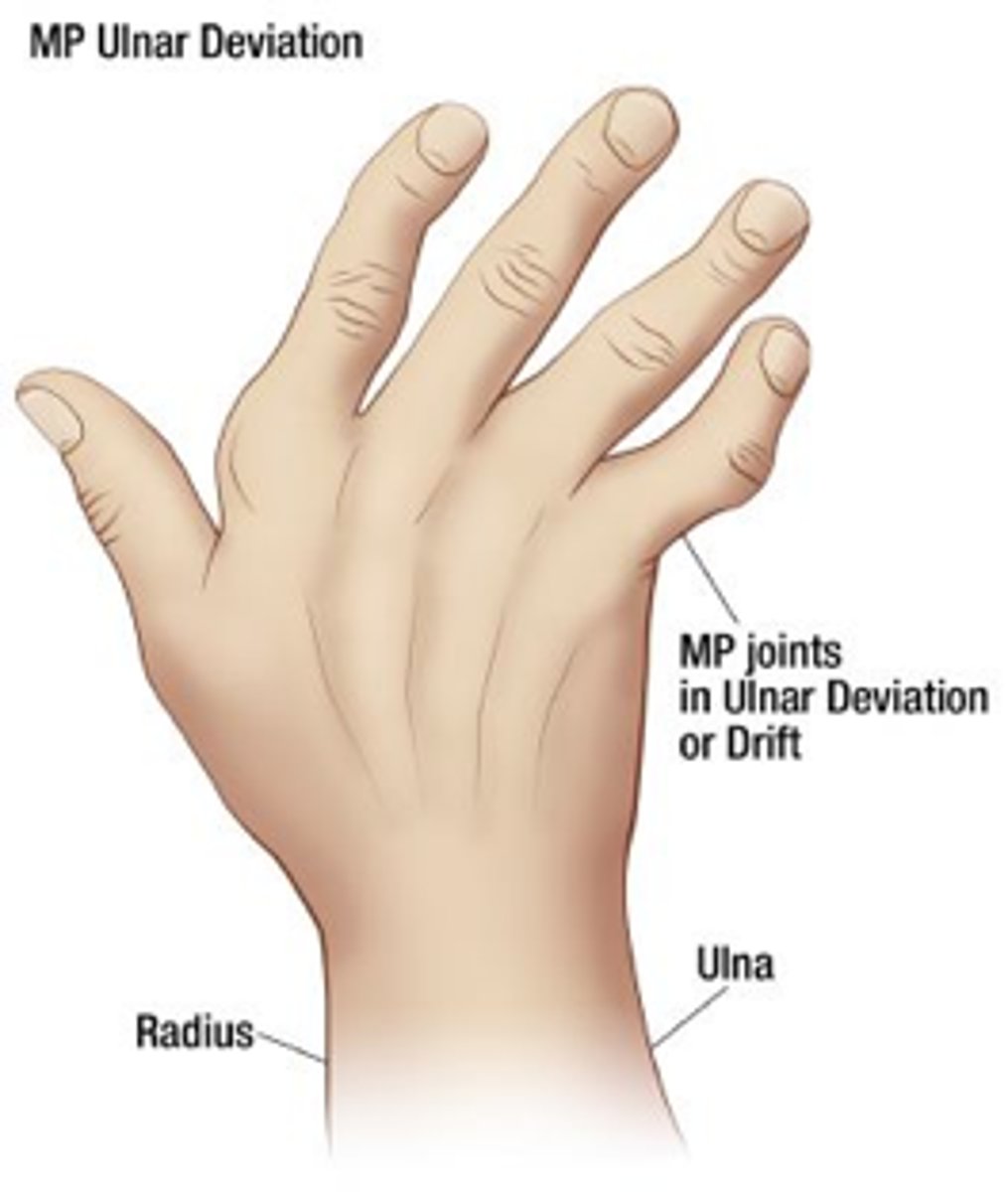
What deformities are associated with RA?
1) swan-neck
2) boutonniere
3) mallet finger
4) ulnar drift
5) thumb
-impaired pinch
-loss of fingertip pick-up
-prominent proximal phalangeal head
What is swan neck deformity?
PIP hyperextension and DIP flexion
dorsal displacement of lateral bands
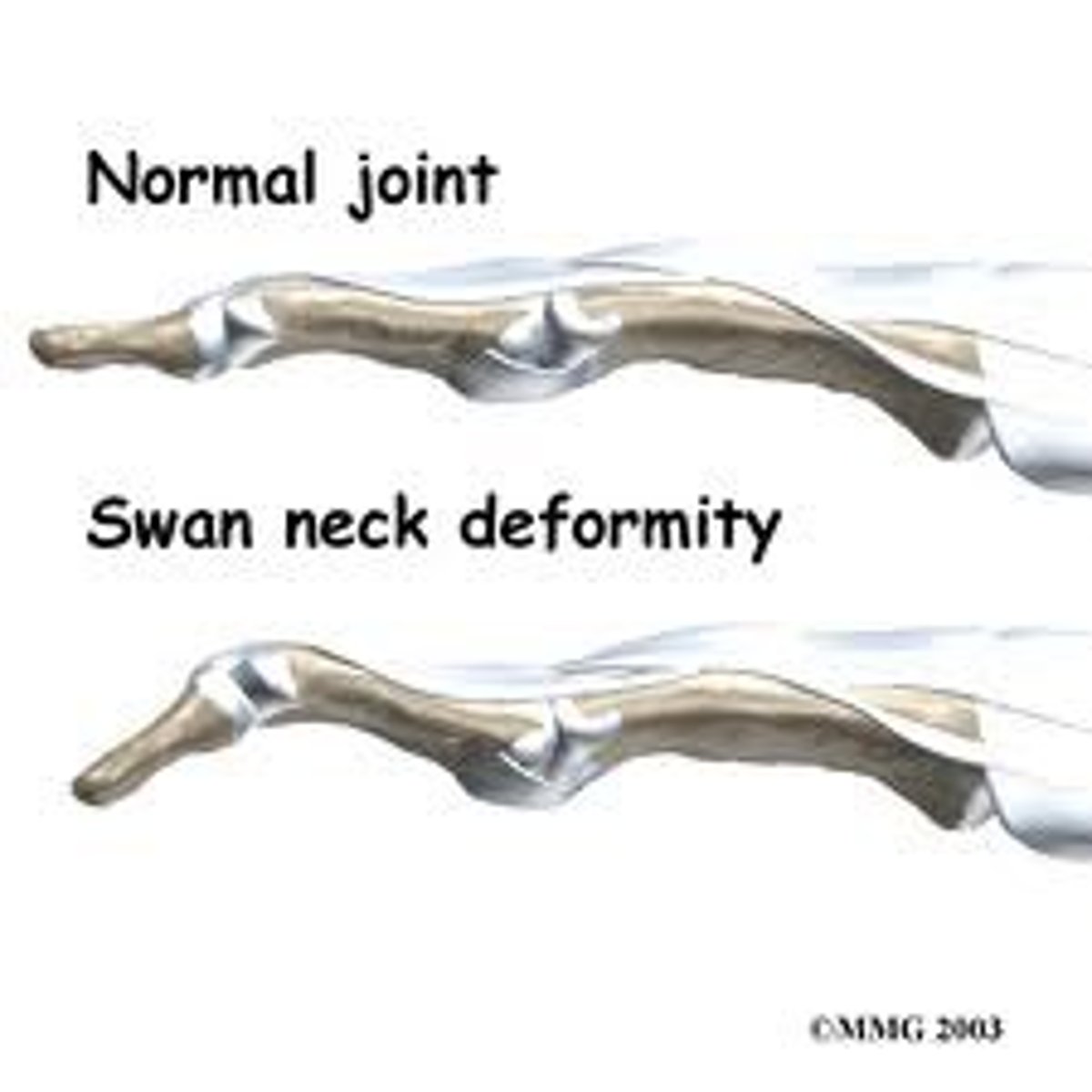
When a person has a __________ deformity, the function of the finger is compromised by an inability to flex the PIP joint, with loss of the ability to make a fist or hold small objects.
swan neck deformity

What is a boutonniere deformity? When does it occur?
PIP flexion and DIP hyperextension
occurs because of synovitis
grasp is preserved
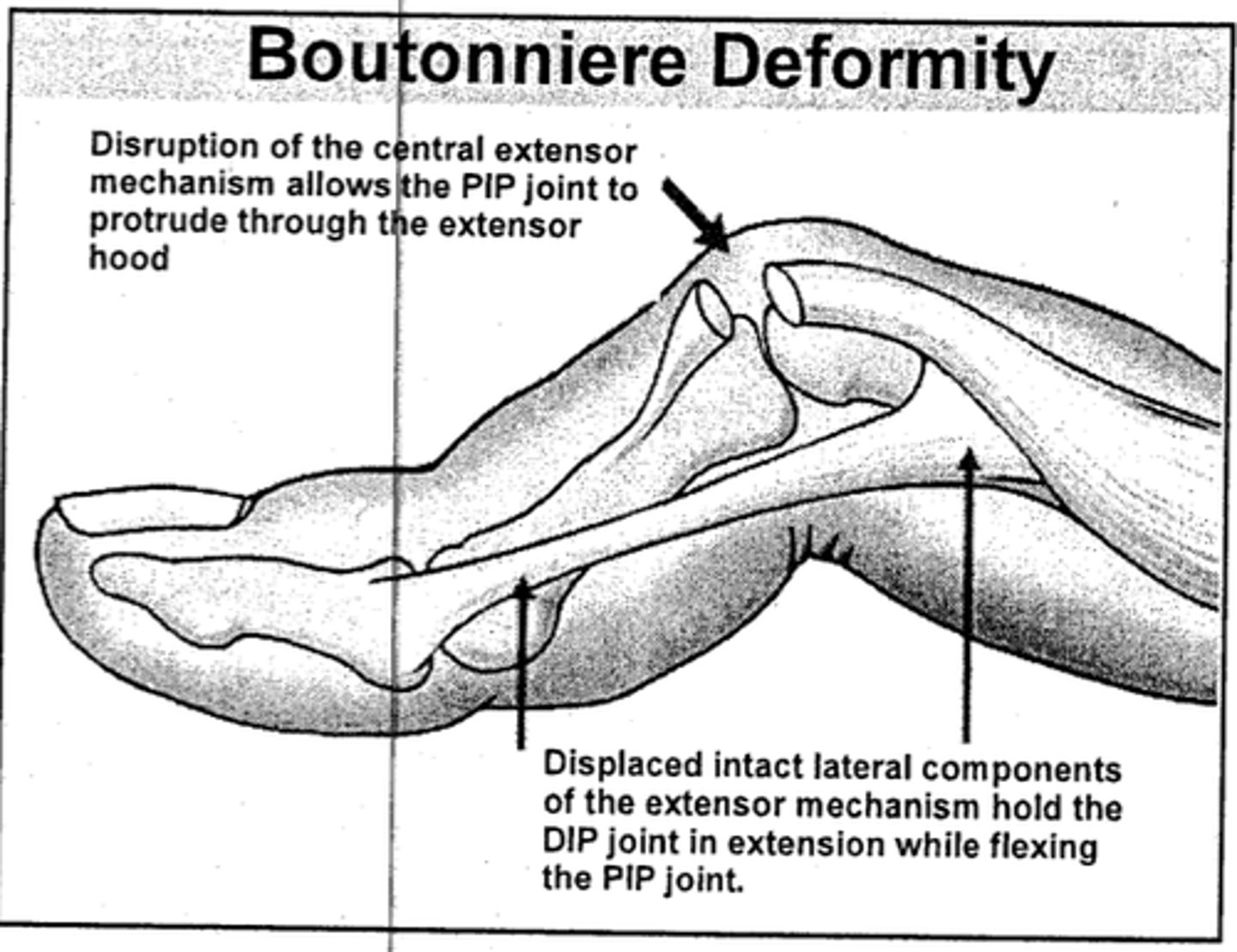
When a person has a _________, the function of the finger is compromised by the inability to straighten the finger and the loss of flexion at the fingertip for pinching.
boutonniere deformity

What is mallet finger? Why does it occur?
DIP flexion (and PIP extension)
occurs bc of rupture of extensor tendon as it crosses the DIP joint
the finger loses the ability to extend the distal phalanx
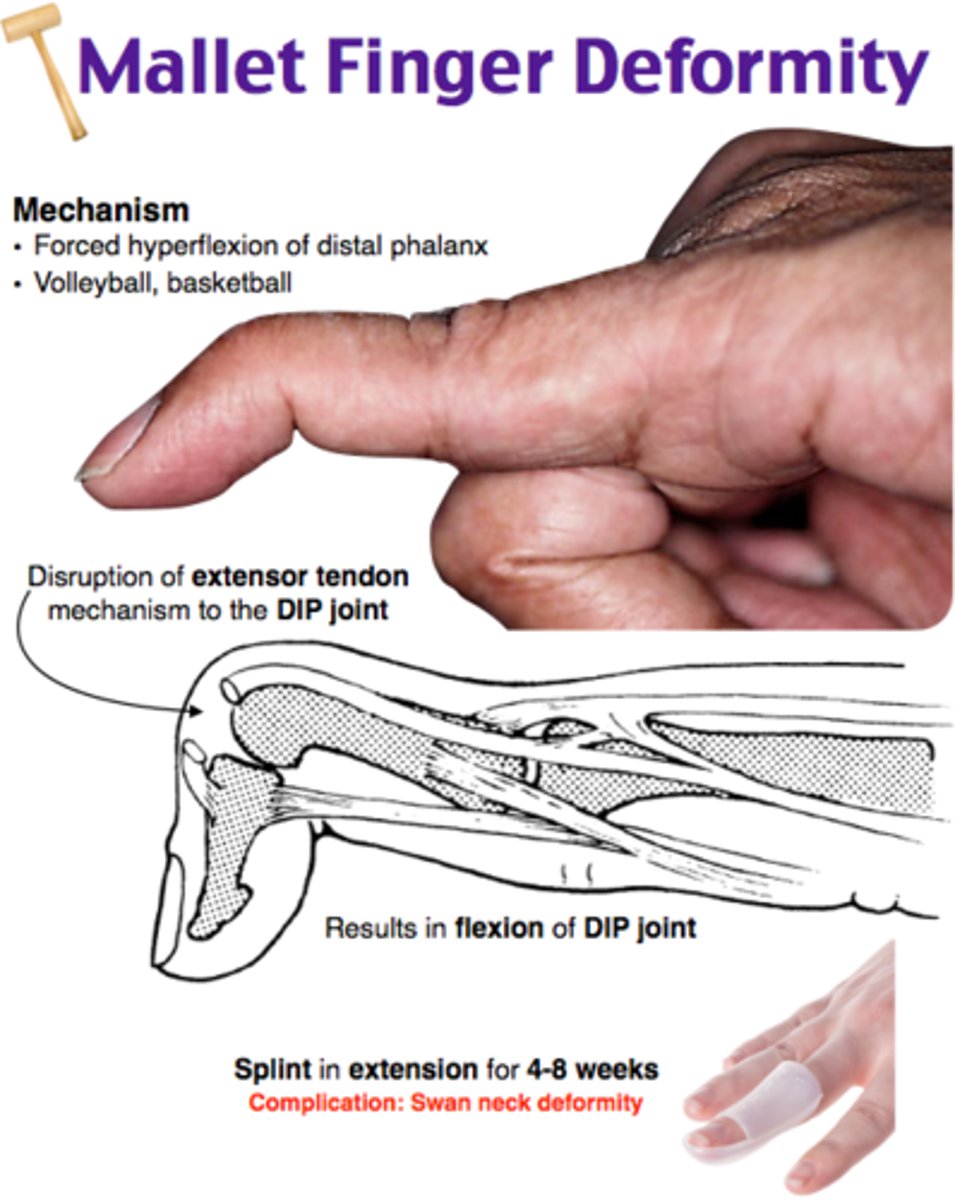
What type of splints can be used for mallet finger and swan neck or hyperextension deformity?
tripod splint

In (1)_______, the most common pattern of deviation is (2)______ deviation of the wrist and (3)______ deviation of the MCP joints. Deviation is caused by ligament weakening or disruption.
1) RA
2) radial deviation of wrist
3) ulnar deviation of MCPs
(1)_____________ are granulomatous and fibrous soft tissue masses that are sometimes painful. They usually occur along weight-bearing surfaces such as the ulna or at the olecranon and can be prognostic of the severity of (2) _______.
1) nodules
2) RA
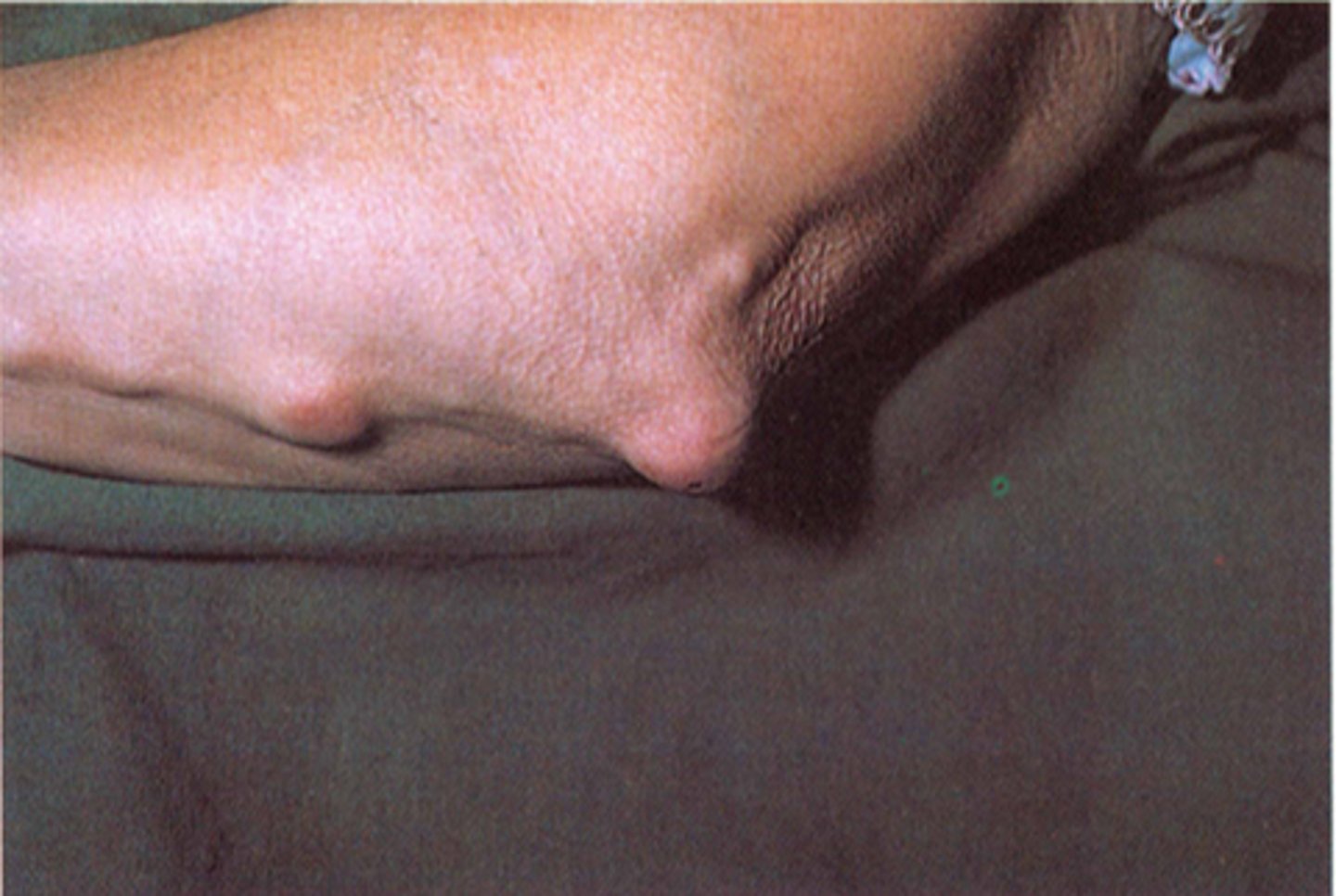
What are nodules? What should we be sure to note when documenting?
granulomatous and fibrous soft tissue masses found on bony prominences exposed to pressure but can occur in other areas
be sure to note:
-location
-size
-sensitivity
-number
-consistency

What two thumb deformities are common in RA?
type I - boutonniere deformity of thumb
type III - swan neck deformity of thumb
Type I - boutonniere deformity of thumb (RA)
CMC not involved
MCP flexion
IP hyperextension
Type III - swan neck deformity of thumb (RA.....and OA)
CMC subluxed, flexed, and adducted
MCP hyperextension
IP flexion

What is subluxation?
-partial dislocation of a joint (volar or dorsal displacement of joints)
-S&S: reduced range of motion, feeling of the joint being "out of place" or "slipping.
dorsal subluxation: the bone moves towards the back side
volar subluxation: the bone moves towards the palm or front side
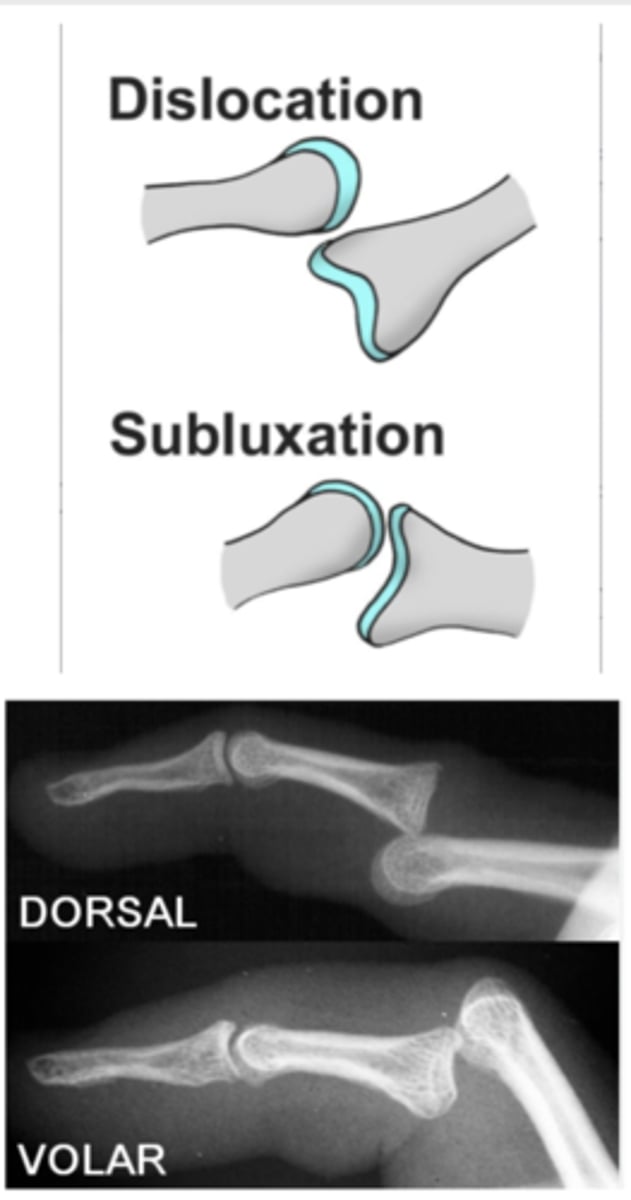
What are the most common sites of subluxation for RA?
most common sites of subluxation are the wrist and MCP joints
(volar subluxation of the MCP joints occurs frequently and is often accompanied by ulnar drift and lateral displacement of the extensor tendons)

What is ankylosis?
abnormal stiffening and immobility of a joint due to the fusion of the bones
fusiform inflammation

Tendon involvements
flexor tenosnyovitis
extensor tenosnyovitis
trigger finger
DeQuervains
Tendon ruptures
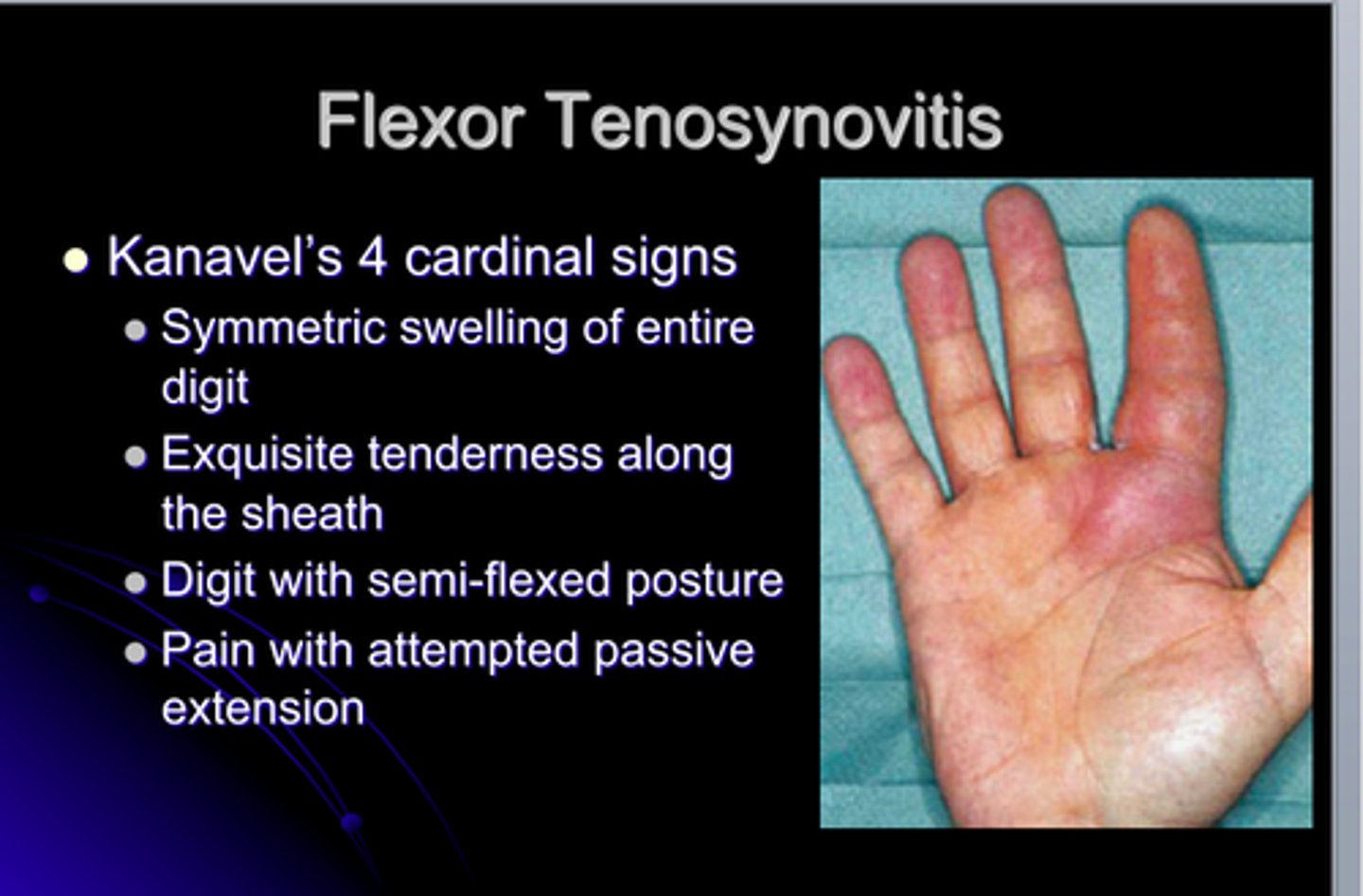
What is flexor tenosynovitis? How do you evaluate?
-inflammation of the tendon and synovial sheath that causes the finger to swell and become painful to move on the volar side
-S&S: heat, swelling, pain or tenderness over the tendon sheath
evaluate
-evaluate the digits between MCP and PIP
-gently pull all digits into hyperextension at MCPs at one time to test simultaneously
-describe location and what motion, if any, increases pain
What is extensor tenosynovitis? How do you evaluate?
inflammation of the tendon and synovial sheath that causes the finger to swell and become painful to move on the dorsal side
evaluate
-place fingers in full flexion (fist), then gently move the wrist into full flexion
-describe location and what motion, if any, increases pain
What is trigger finger?
-caused by a nodule or thickening of the flexor tendons of the finger or thumb as they pass through the digital pulleys
-hinders gliding motion, resulting in catching or "triggering" during flx/ext
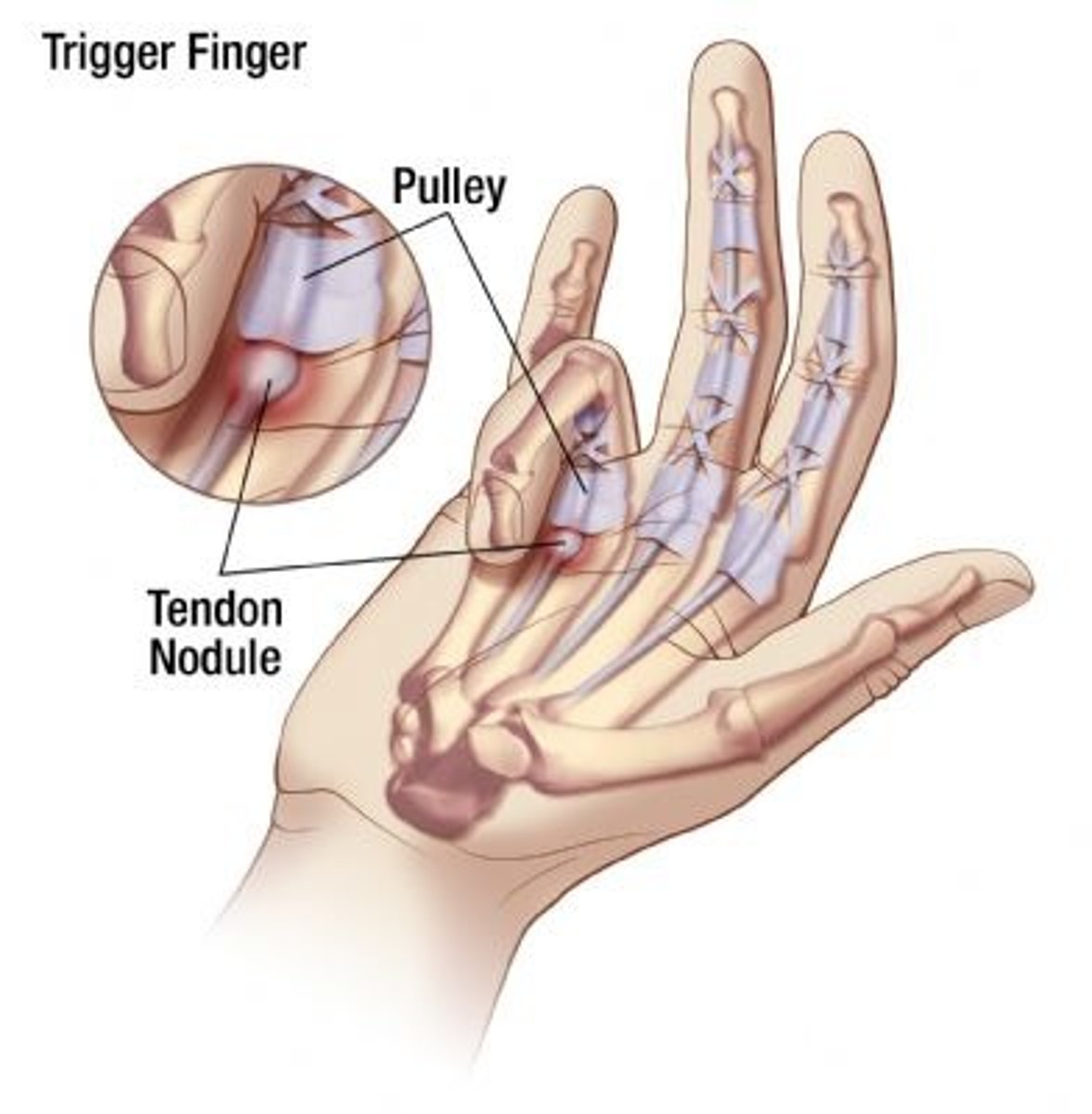
What motions are seen in trigger finger?
can actively flex, but not actively extend
can passively extend
What is DeQuervain's tenosynovitis? How is it tested?
-tenosynovitis involving the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) (("Apple and Peanut butter"))
-tenosynovitis of tendons on radial side
tested through the Finkelstein Test
-patient grasps thumb with fingers and gently deviates wrist ulnarly

What are tendon ruptures?
-most commonly occur with extensor tendons
-result in a loss of active MCP extension with inability to palpate tendon during attempts to extend digit
-rupture can be complete or partial
OT Evaluation of OA and RA involves gathering information on the patient's clinical status including......
1) pain level (throughout day)
2) inflammation or synovitis
3) AROM and PROM
4) strength
5) endurance
6) hand function (grip and pinch)
7) joint deformities
8) joint stiffness and morning stiffness (how long does it last?)
9) crepitus (location, cause, audible and/or palpable)
10) fatigue
12) sensation
12) functional mobility
13) medication
14) joint instability (laxity)
T or F: MMT is contraindicated when a patient with arthritis has inflammation.
true
in the case of an acute or active phase of arthritis, resistance may be harmful to inflamed tissue and joints
joint protection principle!!!
T or F: It is important to understand that strength testing in clients with arthritis differs from normal testing procedures. Resistance is applied at the end range of pain-free motion rather than at the true end of the ROM.
true
when resistance is applied within the pain-free range, inhibition of muscle strength by pain will be avoided.
How is the severity of a mallet finger deformity determined?
determined by DIP flexion with incomplete active extension
mild = partial active extension of DIP
moderate = no active extension of DIP
severe = fixed DIP contracture in flexion
How is the severity of a boutonniere deformity determined?
determined by the loss of active PIP extension
mild = loss of 5-10°
moderate = loss of 11-30°
severe = loss of 31° or more
How is the severity of MCP ulnar drift deformity determined?
determined by degree of ulnar deviation present (without correction)
mild = 0-10°
moderate = 11-30°
severe = 31° or more
How do you evaluate ligamentous instability (laxity) of the PIP / DIP joints?
to evaluate PIP / DIP
-hold joint in neutral (full passive extension)
-stabilize proximal bone while moving the distal bone from side to side
will be noted as:
-mild (5 to 10 degrees in excess of normal)
-moderate (10 to 20 degrees in excess)
-severe (20 or more degrees in excess)
How do you evaluate ligamentous instability (laxity) of the MCP joints?
to evaluate MCP
-hold joint in full passive flexion
-move proximal phalanx
will be noted as:
-mild (5 to 10 degrees in excess of normal)
-moderate (10 to 20 degrees in excess)
-severe (20 or more degrees in excess)
Composite finger flexion to palm
-measures the distance of the finger pulp from the palm when finger joints are flexed simultaneously
-if flexion is near normal, the finger pulp will lie over the distal palmar crease
-if flexion is restricted, the finger pulp will lie over the mid or proximal palm area
-composite finger flexion can be assessed with a ruler that measures the distance from the pulp of the finger to the palm
(tip of index to palmar crease)
-hard end feel - bony blockage
-firm end feel w/ some give - limited by ligament or capsule
How is OA and RA treated?
1) maintain or increase ability to engage in meaningful occupations
2) maintain or increase joint mobility
3) maintain or increase joint strength
4) maximize physical endurance
5) protect against or minimize deformities
6) decrease pain
Pain management includes........
-positioning
-splinting
-thermal modalities
-rest
-pharmacological therapy
-energy conservation
-relaxation techniques
-TENs
-joint protection
-exercise
OA and RA treatment: Rest
-considered an active way of reducing inflammation
-can break the cycle of pain
if have systemic symptoms = whole body rest
if have localized symptoms = splinting, avoiding/modifying task
OA and RA: PAMs - Superficial thermal agents (heat vs cold)
heat can provide
-increased blood flow, pain relief, increased tissue elasticity
-BUT may increase inflammation! (bad)
cold can provide
-reduced inflammation, decreased pain
-BUT may reduce tissue elasticity and increase stiffness
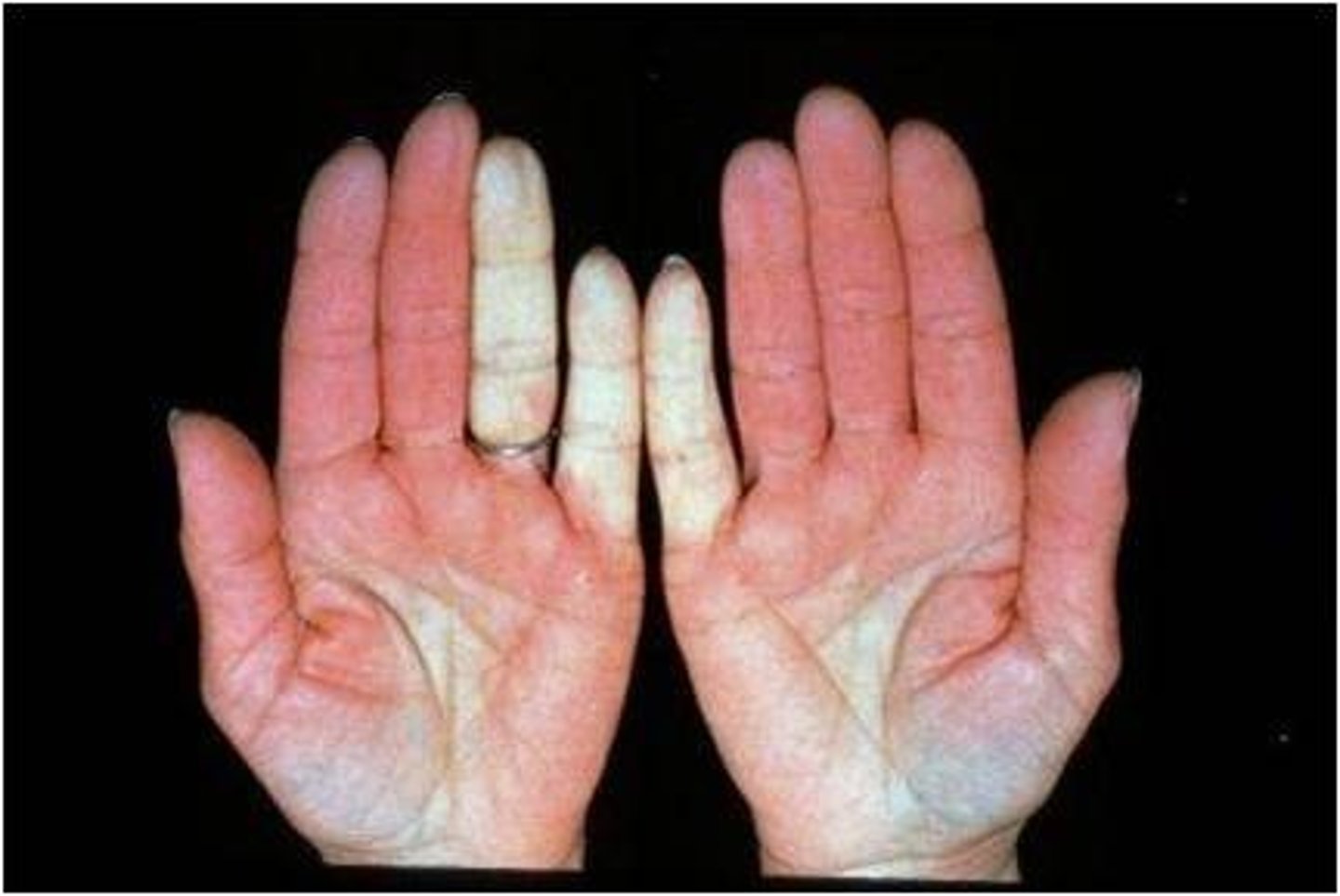
When are the use of cold PAMs contraindicated for RA?
use of cold is contraindicated in clients with Raynaud's phenomenon
-excessively reduced blood flow in response to cold
-skin turns pale, grey, or white
T or F: Clients with RA often have unstable vascular reactions to heat and cold that cause greater than normal heat retention with heat agents or increased coldness and stiffness with cold exposure. Therefore, careful monitoring of client responses to PAMs is crucial.
true
What is the goal of therapeutic exercise for patients with arthritis?
goal = to keep muscles and joints functioning as normally as possible
-exercise programs are individualized
-when pain lasts greater than 1-2 hours post-exercise, then OT should decrease exercise intensity
-avoid undue joint stress, pain, joint swelling
-work within client's comfortable ROM
Therapeutic exercise: Active RA
eliminate stress on inflamed joints (joint protection)
work on AROM (or PROM with stretch at end range)
work on isometric exercises
-resistance if no risk of overstressing joints, and if so, only functional activities like canned foods
Chronic active RA: Treatment objectives
decrease pain and inflammation
Increase ROM
increase strength and endurance
T or F: Rigid splints provide maximal immobilization or stability.
true

T or F: Soft splints allow more freedom of motion.
true

T or F: Semirigid splints combine elements of both.
true
RA Stage I: Early - Splints
Resting splints to decrease acute inflammation, decrease pain, protect joints

RA Stage II: Moderate - Splints
Day splints to provide comfort
Night splints to relieve pain or protect joints against potential deformity
Splints to increase ROM

RA Stage III: Severe and Stage IV: Terminal – Splints
Day splints to improve function (decrease pain, provide stability, limit undesired motion, properly position joints)
Night splints to provide positioning and comfort
Joint protection principles
1) Respect pain
2) Maintain strength and ROM
3) Use joint in most stable anatomical plane
4) Avoid positions of deformity
5) Use strongest joint available
6) Ensure correct patterns of movement
7) Avoid staying in one position for long periods
8) Avoid starting an activity that cannot be stopped
9) Balance rest and activity
10) Reduce force and effort
Joint protection principles: External forces
outside forces placed on joints such as:
-odd-shaped objects
-slippery surfaces
-tight-fit objects (lids, covers)
-small handles
-cold objects
Joint protection principles: Internal forces
internal forces placed on joints such as:
-grasping objects tightly
-poor placement of hand
-poor placement of joints
most joints become stressed in flexion
What movements cause ulnar deviation and should be avoided (or modified)?
holding knives
lifting plates
opening jars
turning a doorknob
pushing in a drawer
wringing out a cloth
Joint protection: Avoid activities involving tight grasp. How can we modify?
use tools with large/rounded handles
use a spike board to stabilize vegetables when cutting them
grasp objects between the palms of both hands instead of using handles (using larger joints over smaller joints)

Joint protection: Avoid sustained positions
maintaining grasp or sustaining a position fatigues muscles easily
-have patient check in with themselves to ensure they don't reach fatigue
STOP sustained activities BEFORE muscles fatigue
Joint protection: Lever arm
increasing the lever arm will decrease the torque
use tongs, reacher, grip wrench

Joint protection: Circumference
increasing the circumference of the tool decreases the force needed
bigger objects easier to manipulate
Joint protection: Diameter
increasing the diameter will decrease the amount of grip required
-preserves the smaller joints
-reduces fatigue from static holding
i.e. thick handles for utensils