Inflammation REVIEW
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
What is inflammation?
Inflammation is an immunologic defense against tissue injury, infection, or allergy
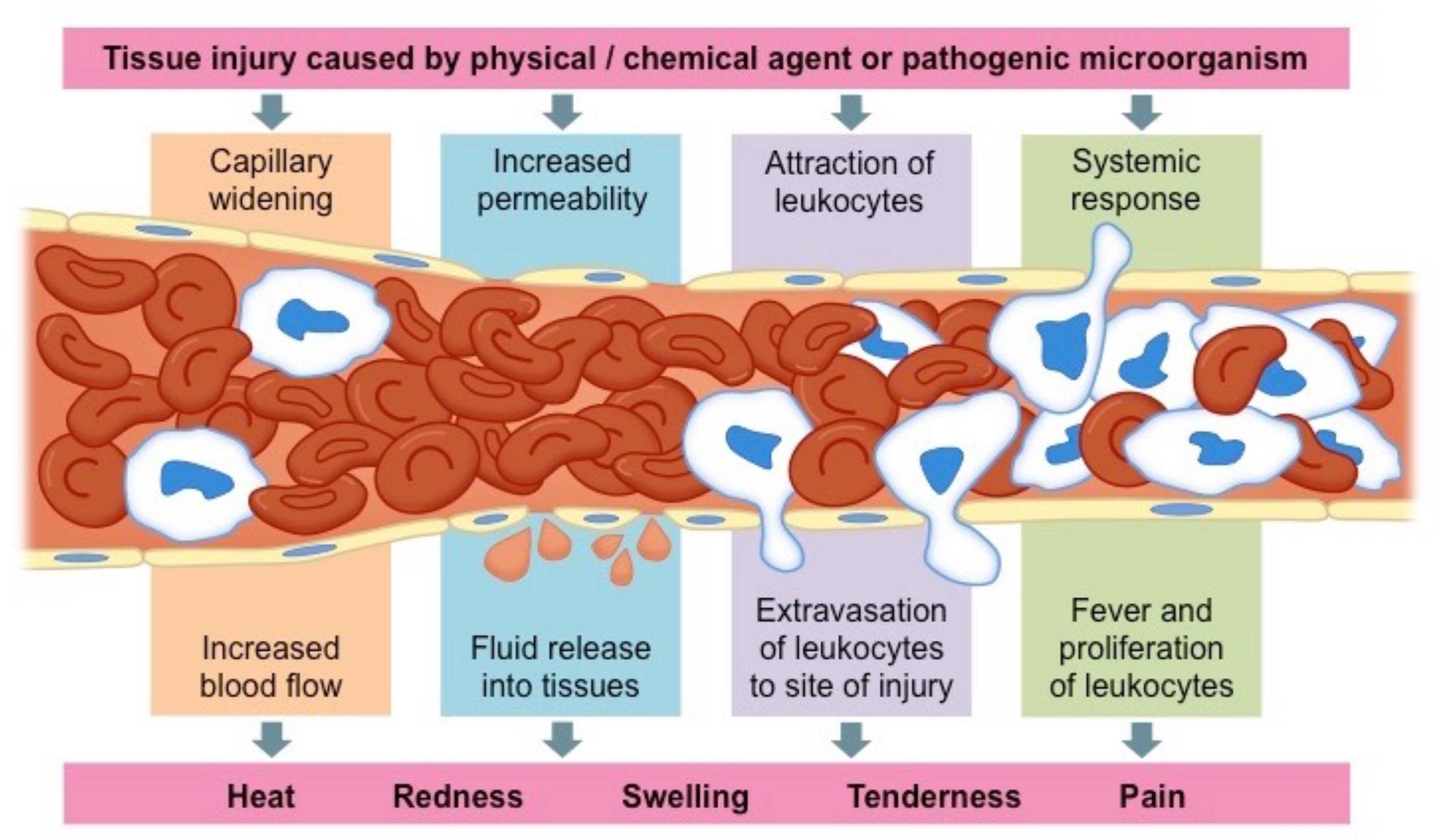
Inflammation: What does it look like?
A localized physical condition in which part of the body becomes reddened, swollen, hot, and often painful, especially as a reaction to injury or infection
Inflammation Pics
Inflammation: Scope
Ranges from no inflammation to active inflammation
May be localized or systemic
Active inflammation may be:
Acute
Chronic
Repair/Restorative
Lymphoid tissues
These are specialized tissues where lymphocytes (a type of white blood cell) are formed and mature. The primary lymphoid tissues include the bone marrow (where B cells mature) and the thymus (where T cells mature). Secondary lymphoid tissues include the lymph nodes, spleen, and mucosa-associated lymphoid tissues (MALT), where immune responses are initiated.
Lymphocytes
These are crucial cells of the immune system that play a significant role in recognizing and responding to pathogens. The main types are B lymphocytes (B cells) and T lymphocytes (T cells). B cells produce antibodies, while T cells can either help other immune cells (helper T cells) or kill infected cells directly (cytotoxic T cells).
Immune response
This is the body’s defense mechanism against pathogens, toxins, or other harmful substances. It can be divided into two phases:
• Innate Immune Response: The body’s immediate, non-specific response that includes physical barriers (skin, mucous membranes), inflammatory response, and phagocytic cells (like neutrophils and macrophages).
• Adaptive Immune Response: A specific response that involves lymphocytes. B cells produce antibodies specific to antigens, and T cells recognize and destroy infected cells.
Types of immunity
• Innate Immunity: Non-specific defense mechanisms that are present from birth and respond quickly to any invader.
• Adaptive Immunity: A specific immune response acquired over time. It has two main types:
Humoral Immunity: Mediated by B cells and antibodies that circulate in bodily fluids to neutralize pathogens.
Cell-Mediated Immunity: Involves T cells targeting and destroying infected or abnormal cells.
Inflammatory response: Function
Restitution of normal, functioning cells after injury
Fibrous repair when restitution of functioning cells is impossible
Acute Inflammatory Response: Steps
Tissue injury and the release of chemical mediators
Vasodilation and increased blood flow
Swelling and retraction of activated endothelial cells
Increased vascular permeability and leakage of small plasma proteins
“Walling off”
Movement of immune response cells to the site of injury
Exudate formation
Movement of glucose and oxygen to the site needing repair
Release of chemical repair factors from activated endothelial cells
Acute Inflammatory Response: Step 1
Tissue injury and the release of chemical mediators
Acute Inflammatory Response: Step 2
Vasodilation and increased blood flow
Acute Inflammatory Response: Step 3
Swelling and retraction of activated endothelial cells
Acute Inflammatory Response: Step 4
Increased vascular permeability and leakage of small plasma proteins
Acute Inflammatory Response: Step 5
“Walling off”
Acute Inflammatory Response: Step 6
Movement of immune response cells to the site of injury
Acute Inflammatory Response: Step 7
Exudate formation
Acute Inflammatory Response: Step 8
Movement of glucose and oxygen to the site needing repair
Acute Inflammatory Response: Step 9
Release of chemical repair factors from activated endothelial cells
Consequences of an Excessive or Ineffective Inflammatory Response
Local tissue damage from compression
Development of chronic inflammation
Systemic pathology:
Atherosclerosis
Chronic renal disease
Neurological disorders
Risk factors: Populations at Greatest Risk
Inflammation can affect all individuals, regardless of age, gender, race, and socioeconomic status. The populations most at risk for a severe or ineffective inflammatory response are the:
Very young
Very old
Uninsured
Blood Test: CBC
A CBC measures overall blood components, focusing on WBCs, which increase with inflammation.
Blood Test: WBC w/ differential
A WBC with differential breaks down WBC types, showing specific increases (e.g., neutrophils for bacterial infection, lymphocytes for viral). These tests help identify and assess inflammation and its potential causes.
Diagnostic Tests: C-reactive protein (CRP)
Measures levels of CRP, a protein that rises with inflammation, often linked to infection or autoimmune diseases.
Diagnostic Tests: Erythrocyte sedimentation rate (ESR)
Measures how quickly RBCs settle at the bottom of a test tube. A faster rate can indicate inflammation in the body.
Diagnostic Tests: Serological tests
To detect specific antibodies or viruses
Diagnostic Tests: Radiographic Tests
X-rays
MRI
CAT
PET scans
Colonoscopy
What should you do to eliminate inflammation?
Provide appropriate nursing and collaborative interventions to eliminate inflammation
Clinical Management: Primary Prevention
Reducing risk for injury and infection
Maintaining good hygiene
Properly using safety equipment
Properly storing and preparing food
Clinical Management: Secondary Prevention
No specific screenings are performed for the general population as it relates to this concept
Collaborative Interventions: Rest, Ice, Compression, Elevation (RICE)
Most helpful after sprain, strain, or minor trauma
Helps minimize swelling
Most beneficial for the first 24 to 48 hours after injury
What is the best method for applying ice? What should the nurse monitor?
Apply ice wrapped in a cloth (never directly on skin) for 15-20 minutes at a time, with 1-hour breaks between applications.
Nurse should monitor for signs of tissue damage (e.g., frostbite, numbness, skin color changes), and assess for pain reduction and swelling.
After applying a compression device, the nurse should monitor for what developments?
Nurse should monitor for impaired circulation, such as changes in skin color (pallor, cyanosis), cold skin, tingling, numbness, increased pain, and swelling distal to the device. Also, check capillary refill and pulse in the area.
How high is “high enough” when elevating an extremity?
"High enough" means elevating the extremity above the level of the heart to promote venous return and reduce swelling. Usually, about 12–18 inches above the heart is recommended.