human & physio - module 3
1/81
Earn XP
Description and Tags
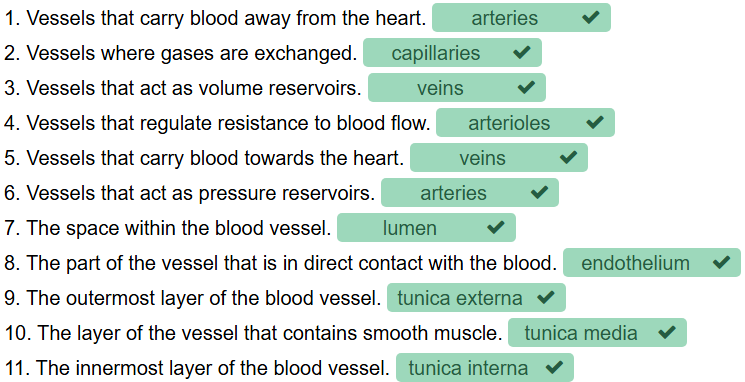
cardiovascular system
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
cardiovascular system
vital transport system that allows for blood to be pumped continuously around the body, transporting substances to and from where they are needed
The cells and tissues of the body require a constant supply of nutrients and oxygen, which are transported to tissues via the cardiovascular system
if the supply of nutrients and oxygen (O2) is insufficient, cells may no longer function effectively and tissue damage may occur
similarly, our cells and tissues are continually producing metabolites and waste products that need to be removed from the body. These waste products are also transported via the cardiovascular system to a part of the body (e.g. kidneys, lungs) where they can be excreted to the external environment
allows for the transport of important substances within the body - examples of this include the transport of hormones from endocrine organs to their target tissues and the transport of circulating immune cells around the body
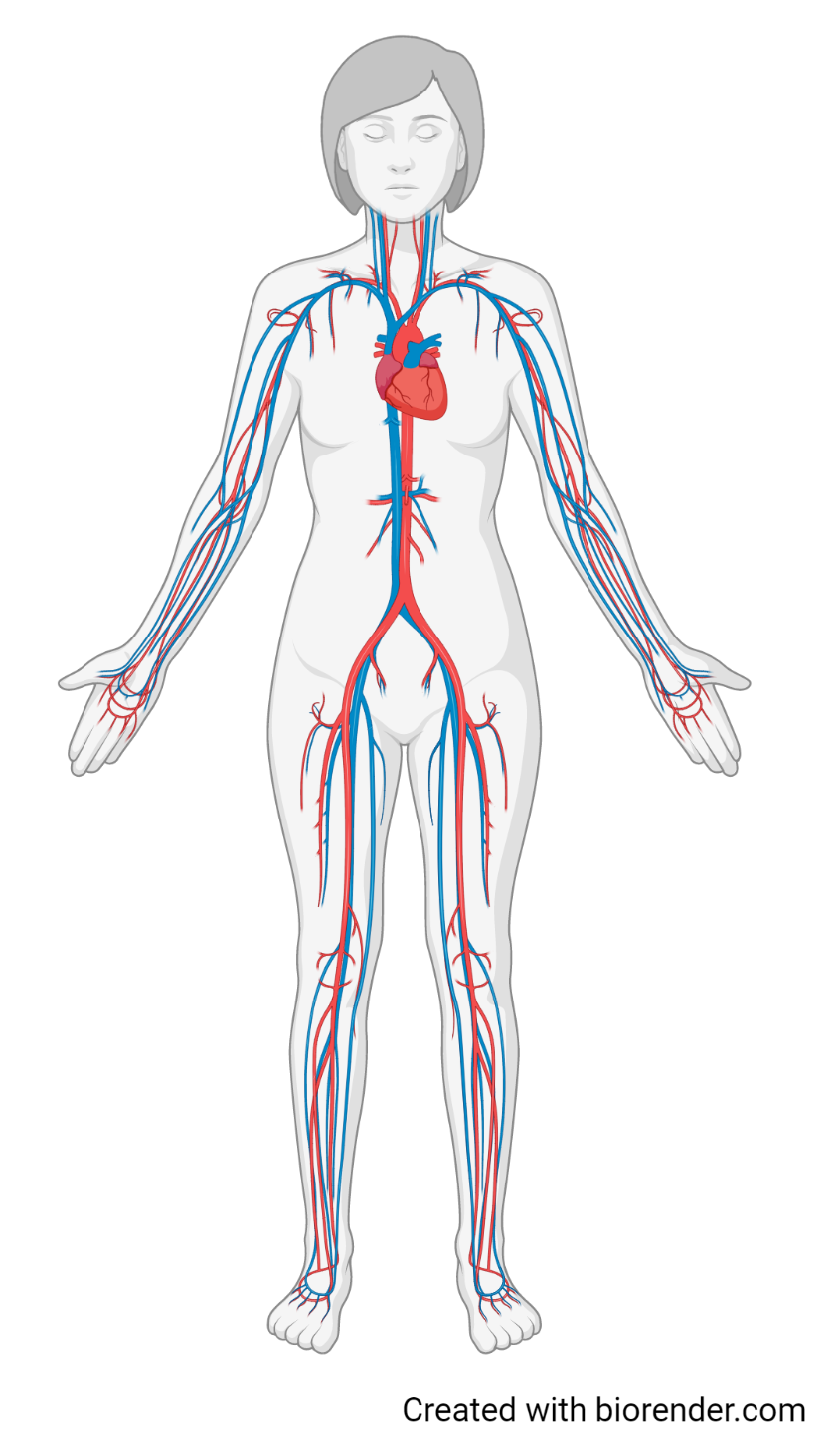
key components of the cardiovascular system
The heart is the pump that provides the driving force to move blood through the cardiovascular system. The two sides of the heart are structurally and functionally distinct and work as two separate pumps acting at the same time
The blood vessels are the tubes that the blood flows through to reach all parts of the body. There are three main types of blood vessels (arteries, veins and capillaries), which have different structures and functions
The blood is the transport medium, which transports substances such as O2, CO2, nutrients, wastes, hormones and blood cells throughout the body
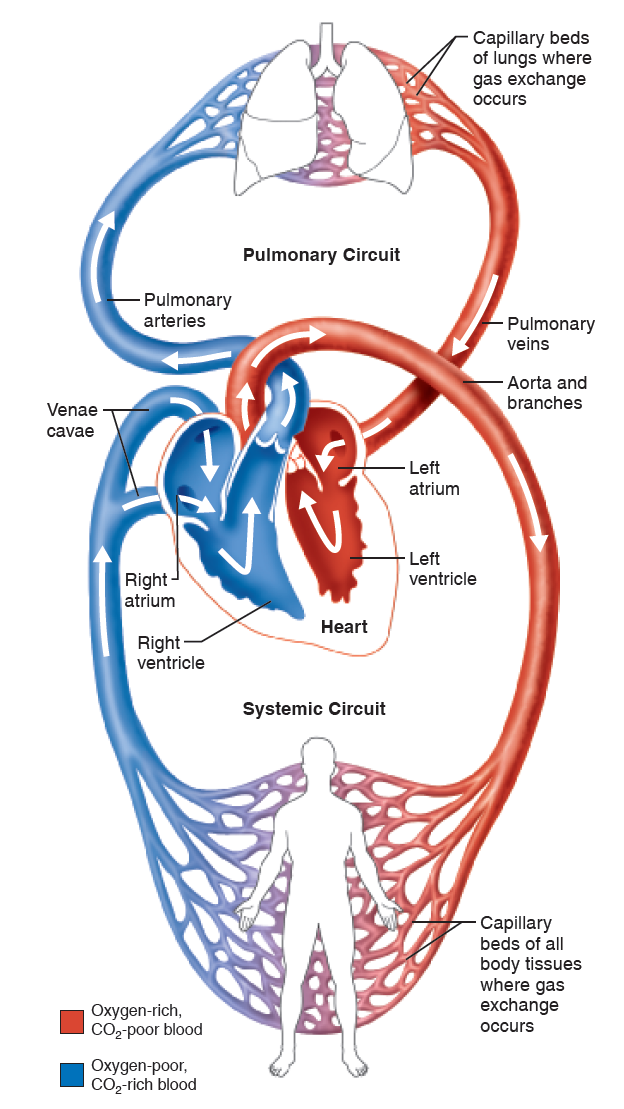
organisation of the cardiovascular system
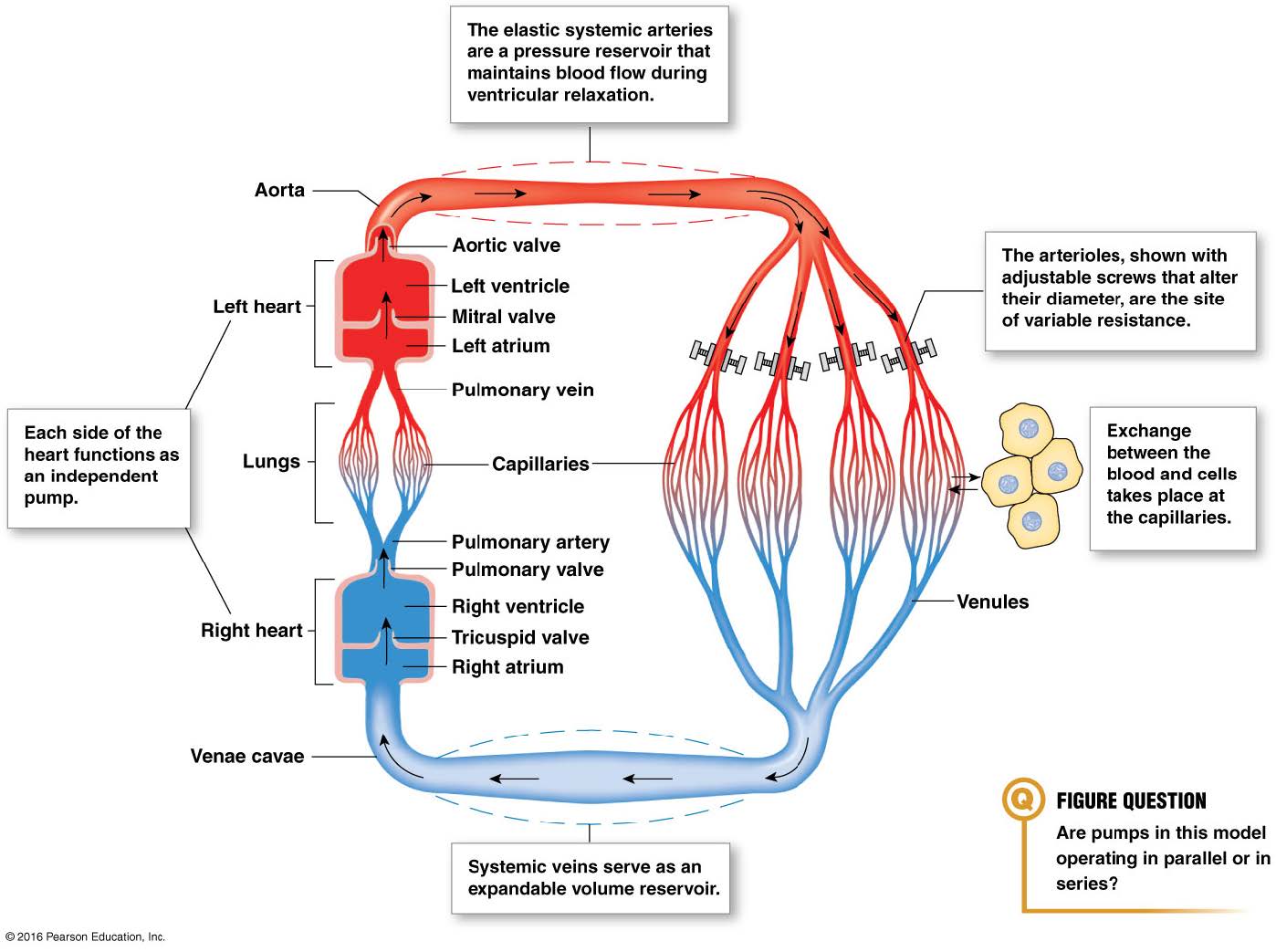
organised so that blood continually circulates the body, allowing for the delivery of nutrients and removal of waste products from cells and tissues. The blood travels through two anatomically distinct circulatory loops (the pulmonary circulation and the systemic circulation) that both start and end at the heart. The heart provides the force that pumps blood into the blood vessels that make up these two circulatory loops
organisation of the cardiovascular system 2
The right side of the heart contains oxygen-poor (or deoxygenated) blood. It pumps blood into the pulmonary circulation. This circuit takes blood to the lungs, where it picks up oxygen (O2) and gets rid of carbon dioxide (CO2). The oxygen-rich (or oxygenated) blood is then returned from the pulmonary circulation to the left side of the heart
The left side of the heart then pumps this oxygenated blood into the systemic circulation. This circuit takes this blood to all the other tissues of the body, delivering oxygen and nutrients. Blood travelling through the systemic circulation also picks up CO2 and other waste products. The blood leaving the systemic circulation is then returned to the right side of the heart
The heart has four chambers, two on each side: The upper chambers on each side are the atria (singular; atrium). The atria are the receiving chambers that receive the blood that is being returned to the heart from the circulation
Right atrium: receives blood returning from the systemic circulation
Left atrium: receives blood returning from the pulmonary circulation
The lower chambers are the ventricles. The ventricles are the pumping chambers that pump blood into the circulation
Right ventricle: pumps blood into the pulmonary circulation
Left ventricle: pumps blood into the systemic circulation
Note: Arteries and veins are NOT defined by the type of blood they contain (i.e. oxygen-rich or oxygen-poor). Instead, these vessels are characterised by which direction they carry blood in. Arteries carry blood away from the heart, whilst veins carry blood towards the heart
What is the primary function of the cardiovascular system?
The primary function of the cardiovascular system is to transport substances around the body. This includes transporting substances to and from sites for external exchange (e.g. the lungs, where O2 enters the body and CO2 exits the body), as well as between organs and tissues of the body.
What are the 3 key components of the cardiovascular system, and what are the functions of these components?
The 3 key components of the cardiovascular system are the heart, the blood vessels, and the blood. The heart is the pump, which generates the force to pump blood through the circulation. The blood vessels are the 'plumbing', or the tubes that the blood flows through. The blood is the transport medium, which travels through the heart and blood vessels, and contains the different cells and substances that are being transported through the body.
What happens to O2 and CO2 as blood passes through the pulmonary circulation? What happens to O2 and CO2 as blood passes through the systemic circulation?
As blood passes through the pulmonary circulation, O2 enters the blood from the lungs, and CO2 leaves the blood and moves to the lungs. As blood passes through the systemic circulation, O2 leaves the blood and is delivered to the working tissues, and CO2 moves from the tissues to the blood.
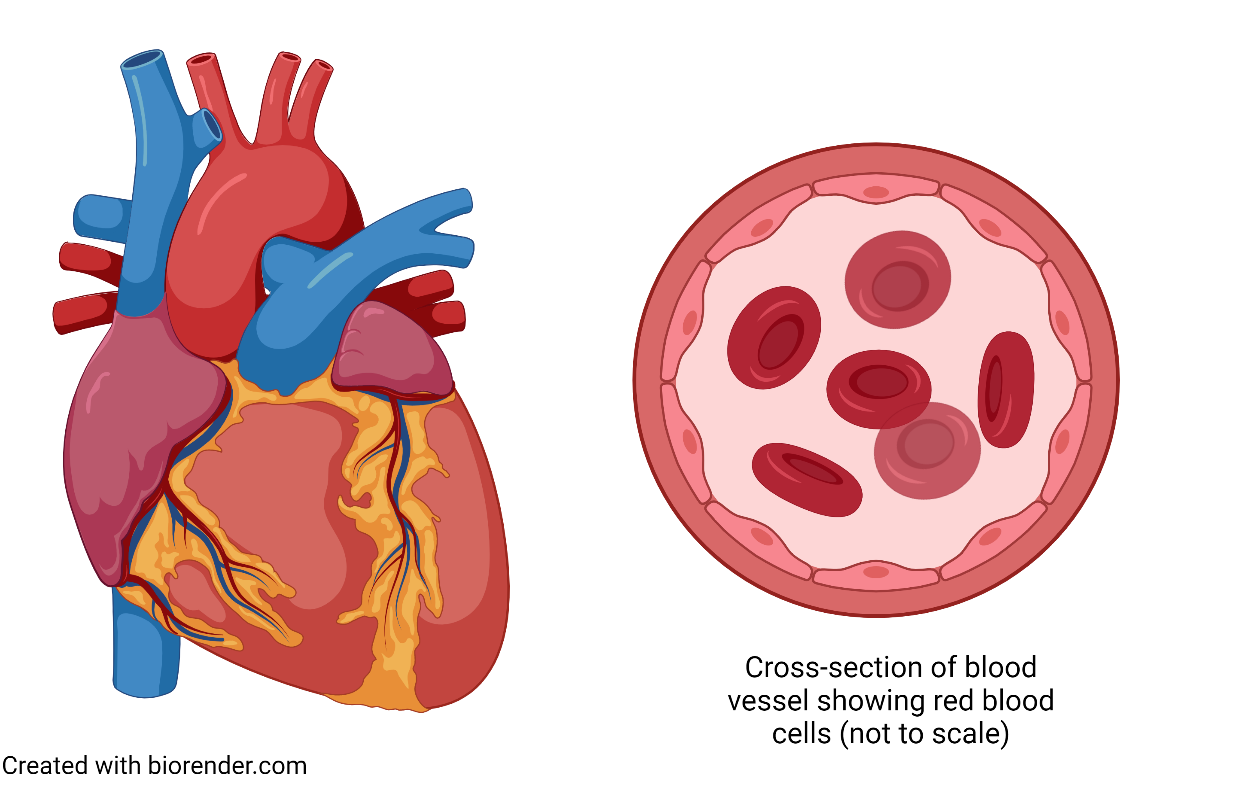
The heart
The pump of the cardiovascular system. It provides the driving force to continually move blood around the body via the circulatory system.
The heart acts as two separate pumps that work at the same time. The right side of the heart pumps blood into the pulmonary circulation, and the oxygenated blood leaving the pulmonary circulation is returned to the left side of the heart
The left side of the heart pumps oxygenated blood into systemic circulation, and the deoxygenated blood leaving the systemic circulation returns to the right side of the heart
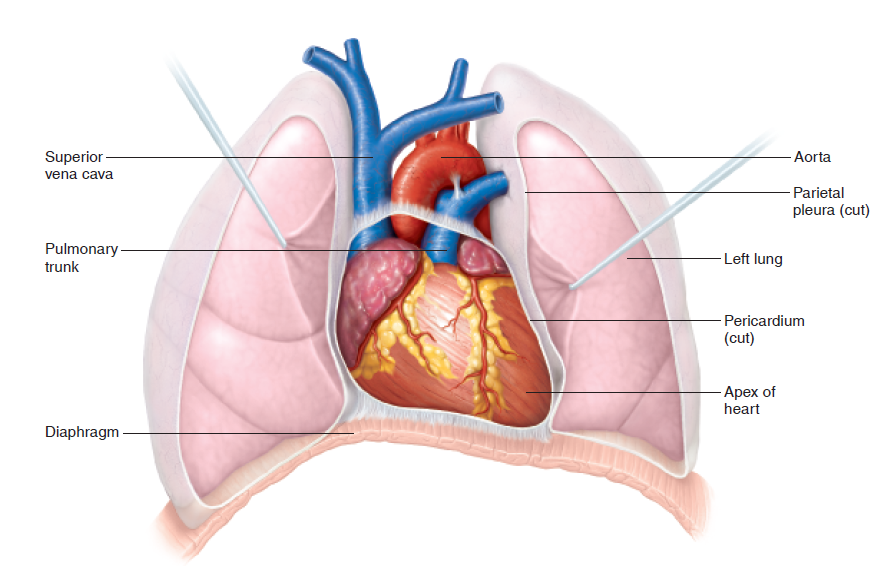
location and size of heart
the heart is approximately the size of your closed fist and in an adult weighs around 250-300 grams
It is located within the thorax, between the lungs and anterior to the vertebral column and posterior to the sternum
About 2/3 of the heart’s mass is on the left side of the midline of the body. The apex (pointed tip) of the heart points downwards and to the left
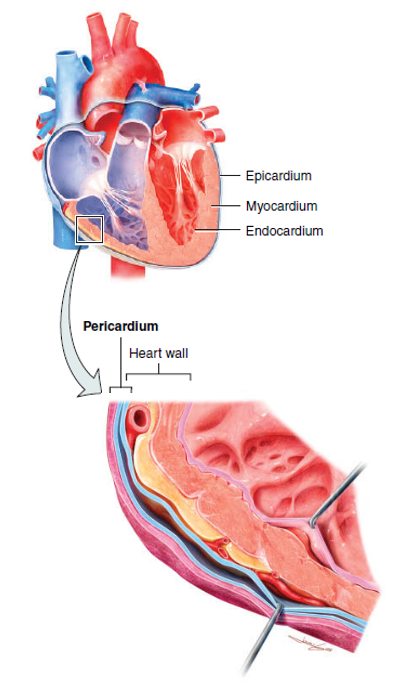
layers of heart
The heart wall is composed of 3 layers: the epicardium, myocardium and endocardium. The epicardium is the external layer and also forms part of the pericardium
The myocardium is primarily cardiac muscle and is the part of the heart that is responsible for cardiac contraction and the pumping action of the heart (middle layer of the heart wall)
The endocardium is the innermost layer of the heart. This thin layer of squamous epithelium and connective tissue provides a smooth layer lining the inside of the heart
The heart is surrounded by a double-walled sac called the pericardium. This structure helps to protect the heart and anchors it to the surrounding structures. The pericardial fluid between the two layers of the pericardium acts as a lubricant, which reduces friction as the heart contracts and relaxes (outermost layer of the heart wall)
Note: Although the heart is filled with blood inside the chambers, this blood does not supply the heart muscle itself with nutrients due to the thickness of the myocardium. Instead, the heart receives its blood supply and nourishment through the coronary circulation. Blockages in the coronary circulation deplete the heart of O2 and nutrients, causing tissue damage and potentially leading to a myocardial infarction (heart attack)
chambers of the heart
There are four chambers in the heart. The atria are the superior (upper) chambers that receive blood back into the heart from the circulation and the ventricles are the inferior (lower) chambers that pump blood from the heart back into circulation
The right and left sides of the heart are separated by a wall called the septum. Blood flow in the heart is one-directional; as blood enters the heart, it flows into the atria before moving into the ventricles and then leaving the heart via the great arteries. This one-way flow of blood is maintained by two sets of valves
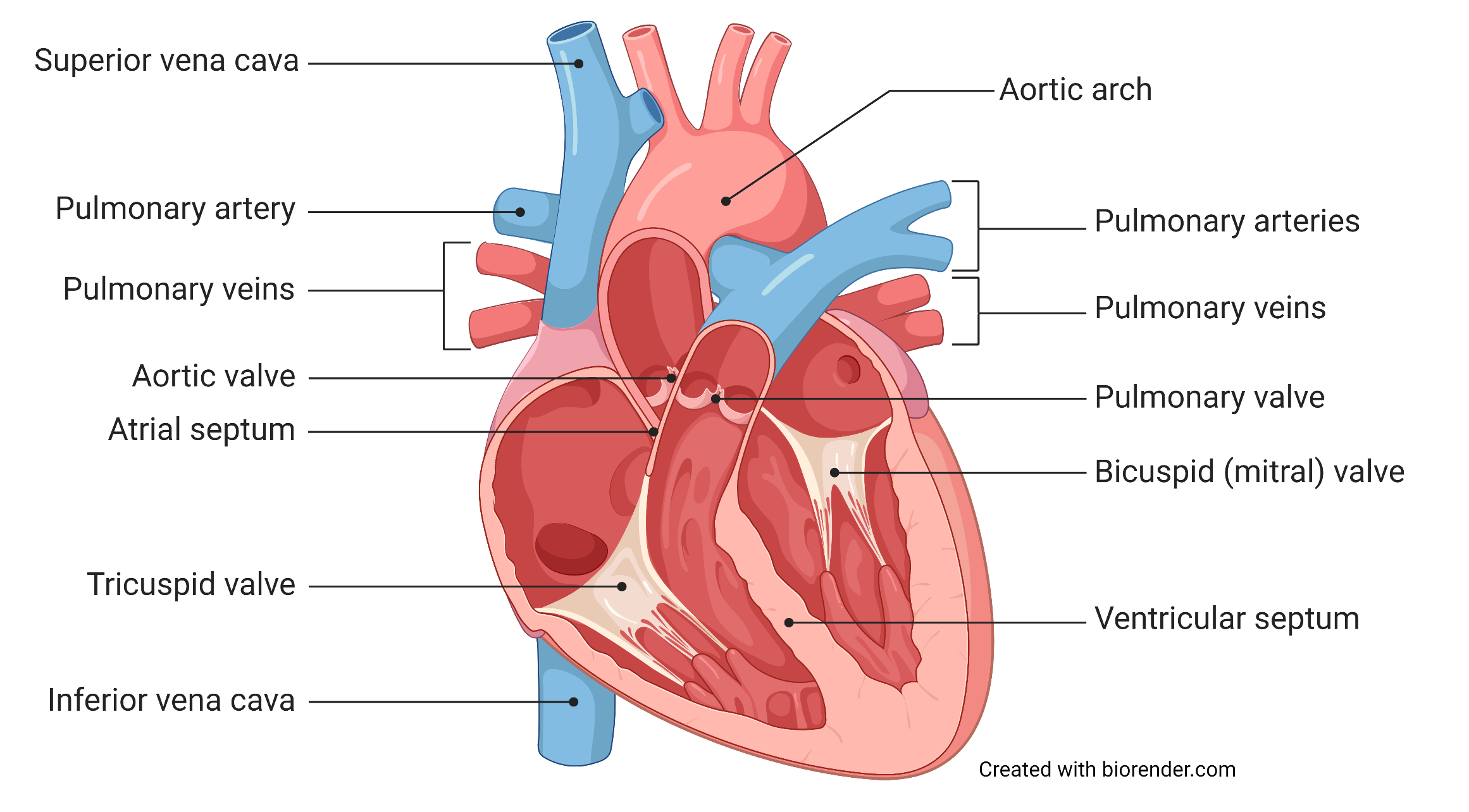
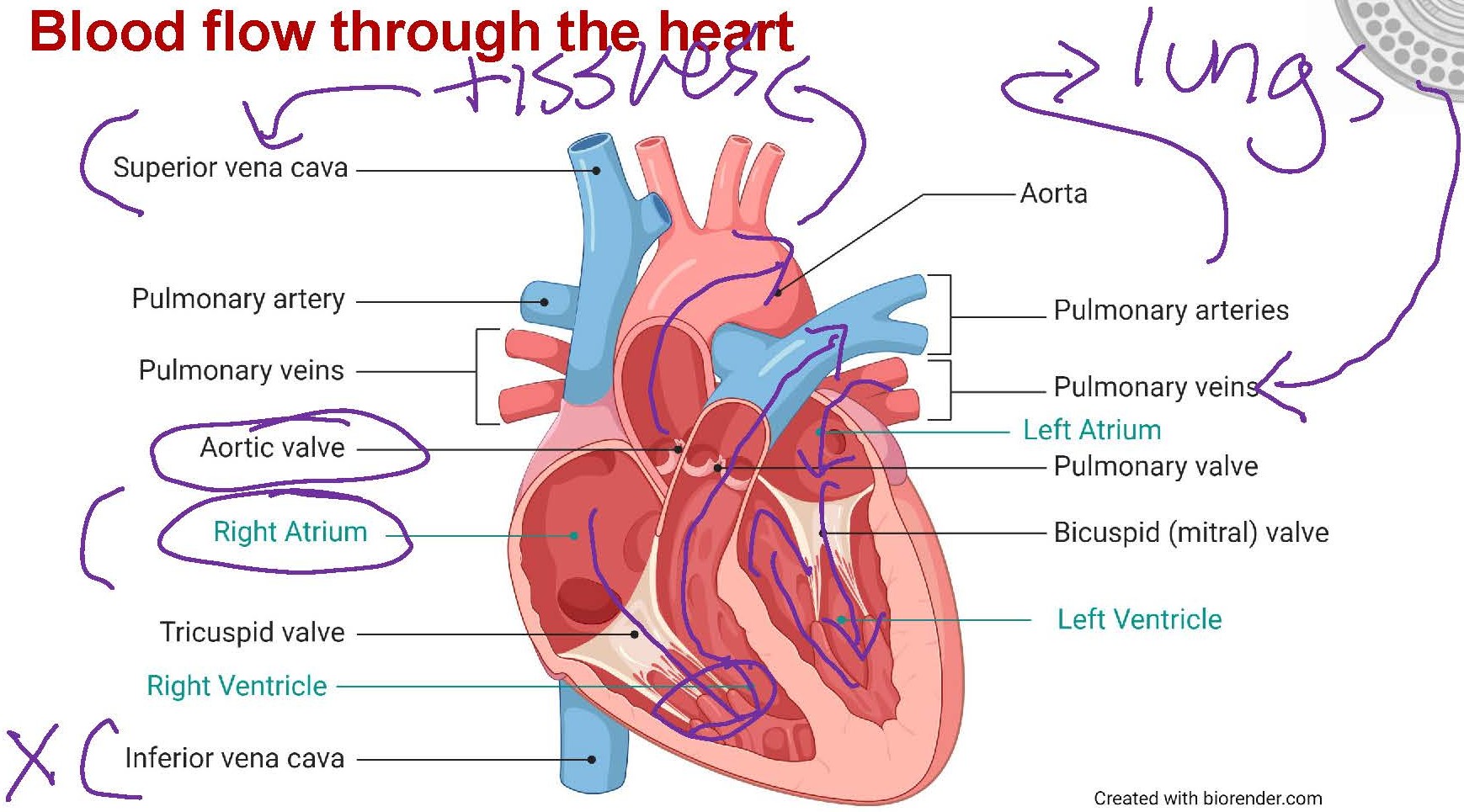
blood flow through the heart
The atria are small chambers with thin walls, as they don’t need to generate much force to push blood to their adjacent ventricle
The right atrium receives the blood from the systemic circulation (via the inferior and superior vena cava) and this blood then passes through the tricuspid valve to the right ventricle.
The left atrium receives blood from the pulmonary circulation (via the pulmonary veins), and this blood then passes through the bicuspid valve to the left ventricle
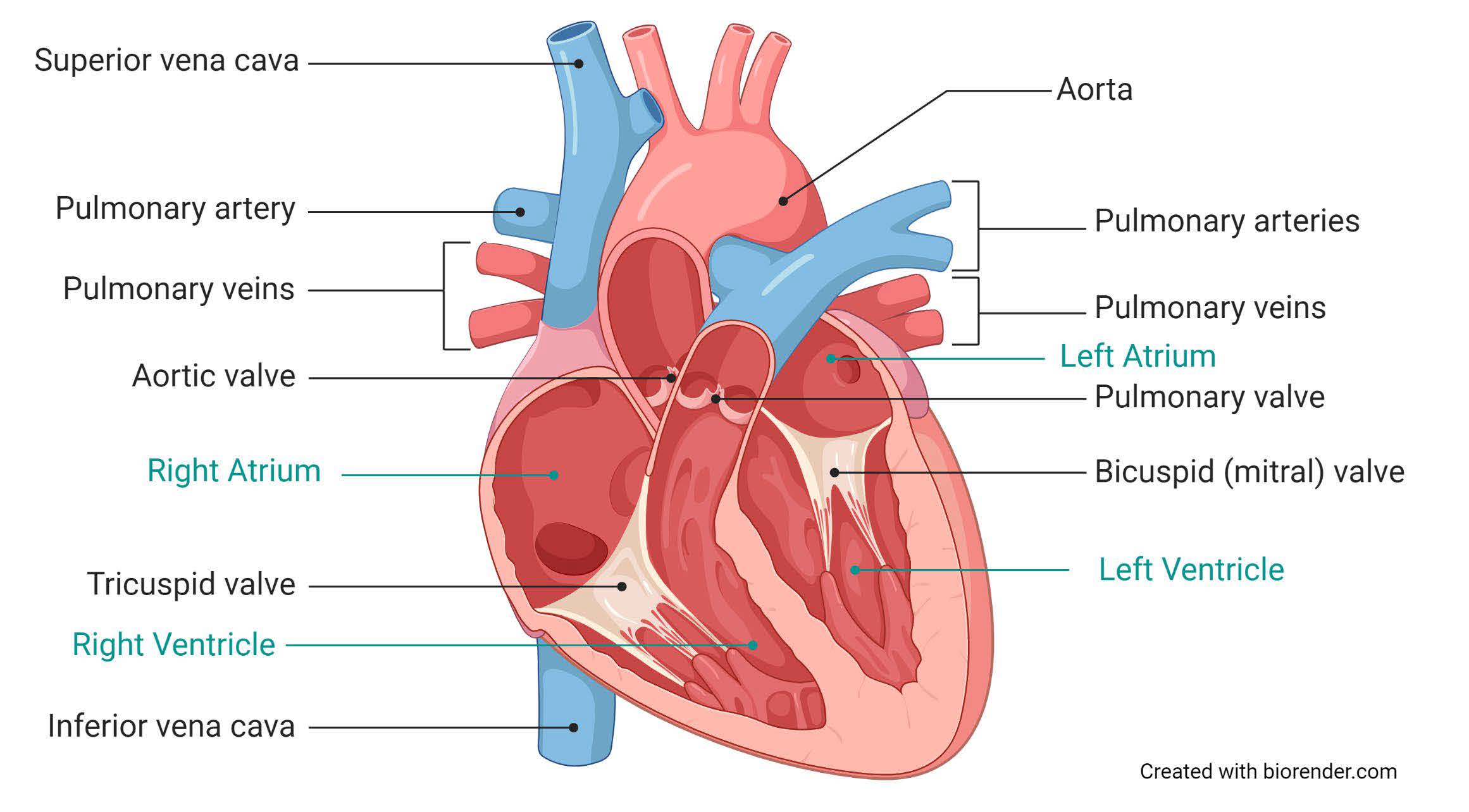
blood flow through the heart 2
The ventricles make up most of the mass and volume of the heart. The ventricles receive blood from the atria and then pump that blood into the circulation
The walls of the ventricles are much thicker than the walls of the atria due to the larger amount of force that the ventricles need to generate to pump blood into the circulation
The right ventricle pumps blood through the pulmonary valve into the pulmonary arteries - this blood then passes through the lungs, where it picks up oxygen and gets rid of carbon dioxide. The left ventricle pumps blood through the aortic valve into the systemic circulation via the aorta, the largest artery in the body. Vessels that branch off from the aorta then carry blood throughout the rest of the body
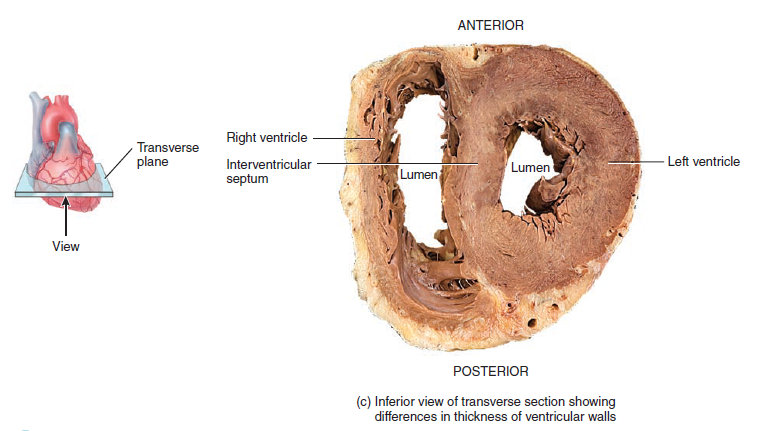
ventricle thickness
The wall of the left ventricle is much thicker than the wall of the right ventricle (image).
This is because the left ventricle has to pump blood into the systemic circulation, which covers a much greater distance than the pulmonary circulation and, therefore, requires more force to be generated by the left ventricle.
Note: Remember that the heart is a muscle, and the larger the muscle, the more force it can generate!
REVIEW - blood flow throughout the heart
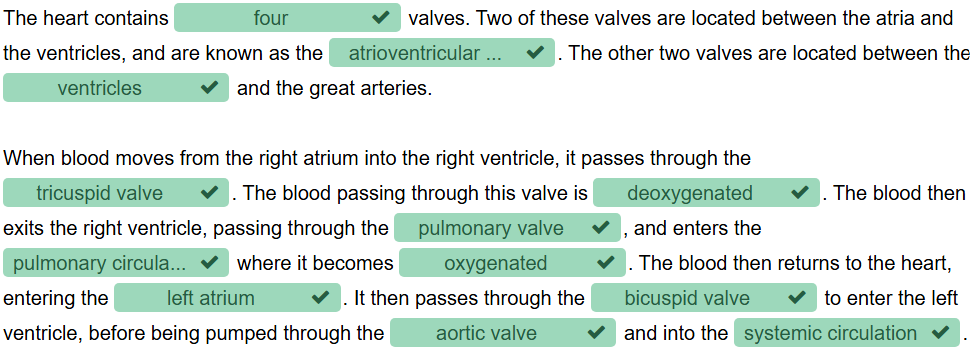
valves
There are two sets of valves that ensure blood flow through the heart in one direction: from the atria to the ventricles and then out of the heart via the great arteries
The valves open to let blood pass through and then close to prevent the backflow of blood. The opening and closing of the valves are caused by changes in pressure as the chambers of the heart contract and relax
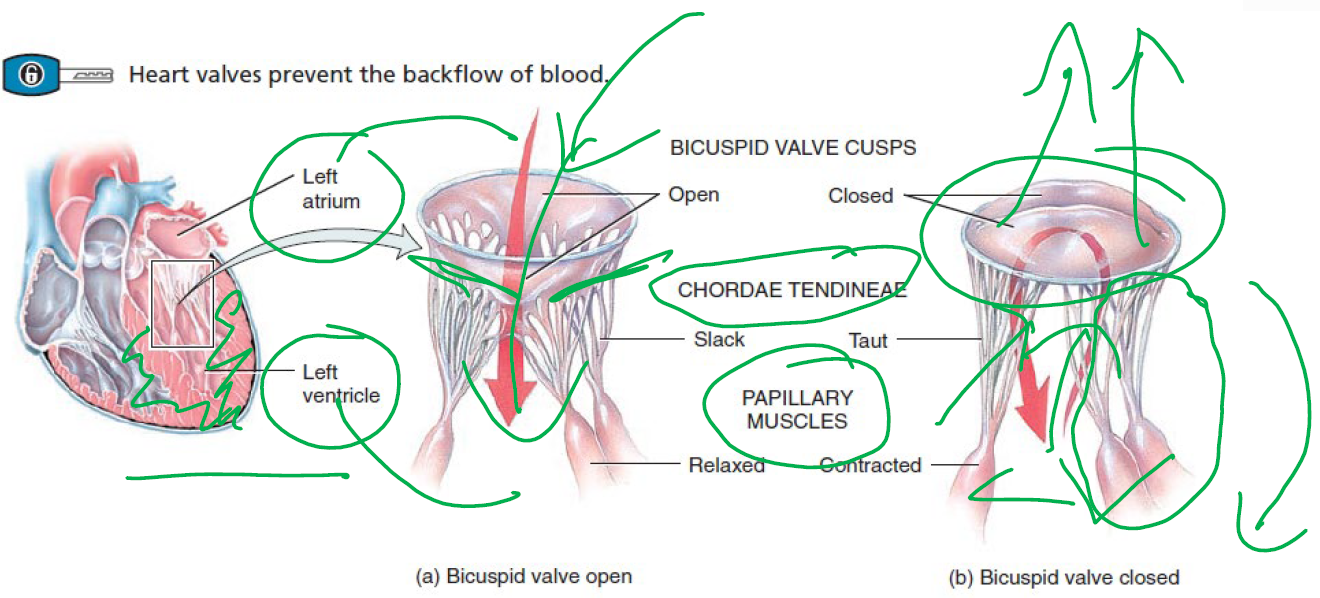
atrioventricular (AV) valves
located between the atria and ventricles. These valves are made up of flexible cusps.
The right AV has three cusps and is called the tricuspid valve. The left AV valve is open, allowing blood to flow from the atria into the ventricles.
When the ventricles contract, the increased pressure in the ventricle pushes the cusps upward, closing the valve and preventing backflow.
The cusps of the AV valve are connected to cords of connective tissue called chordae tendinae. These cords connect the valve to the papillary muscles on the inside of the ventricular wall.
The chordae tendinae and papillary muscles act as supports to prevent the AV valves from everting (opening back into the atria) under high pressure
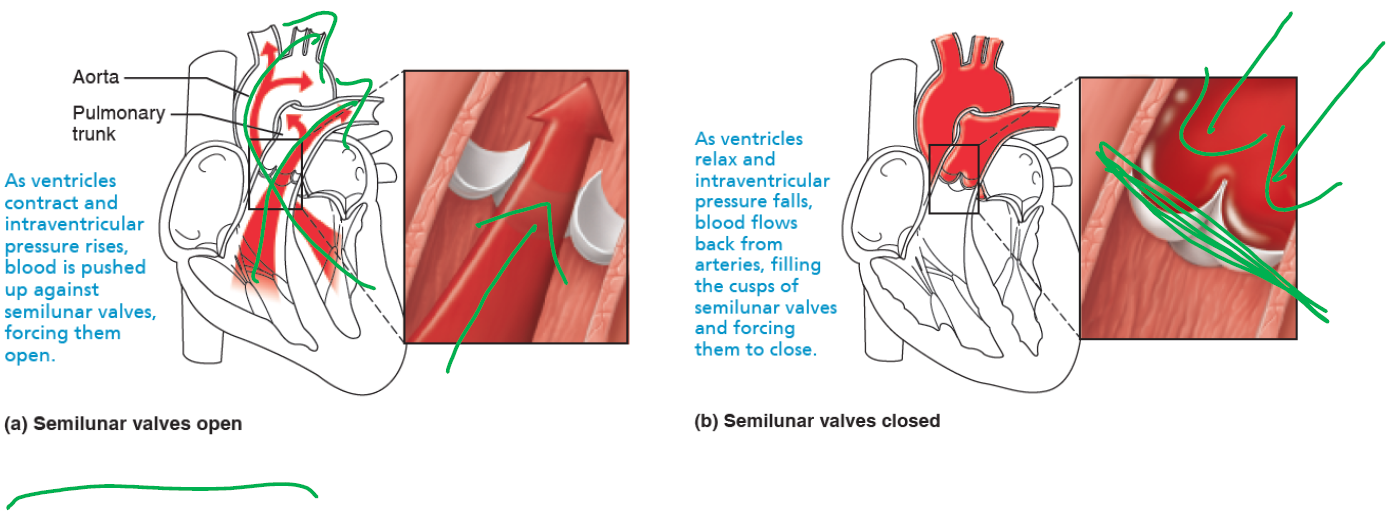
semilunar (SL) valves
Located between the ventricles and the great arteries, the aortic valve is located between the left ventricle and the aorta, and the pulmonary valve is located between the right ventricle and the pulmonary artery
Like the AV valves, the SL valves open and close based on changes in pressure. When the ventricles are contracting and the pressure in the ventricles is higher than the pressure in the arteries, the SL valves will be open
As the ventricles relax and the pressure inside the heart decreases, the pressure in the arteries forces the valves closed, preventing backflow
four valves of the heart
Surrounded by rings of connective tissue that help to support the valves. This connective tissue is part of the fibrous cardiac skeleton, which reinforces and anchors the myocardium
The cardiac skeleton also acts as electrical insulation, which helps to ensure that cardiac contraction is coordinated
REVIEW - valves
cardiac cycle
For the heart to act as a pump, it must alternate between contracting and relaxing. During contraction, blood is forced out of the heart and into circulation, whilst during relaxation, the heart chambers refill with blood
The cardiac cycle is the complete sequence of contraction and relaxation during a single heartbeat. Systole refers to the period of cardiac contraction, whilst diastole refers to the period of cardiac relaxation
The atria and ventricles do not contract and relax at the same time - rather, during the cardiac cycle, there is a carefully controlled sequence of events that are coordinated to make sure that the heart is acting efficiently as a pump
cardiac muscle cells
One of the 3 different types of muscle tissue, an involuntary muscle, meaning that the contraction of this muscle is not consciously controlled
Cardiac muscle is a type of striated (striped) muscle where the muscle cells are branched and interconnected.
Like neurons, these cardiac myocytes (myo = muscle, cyte = cell) are excitable cells that can fire action potentials. It is the electrical activity generated by cardiac myocytes that causes the contraction and relaxation of the heart that makes up the cardiac cycle
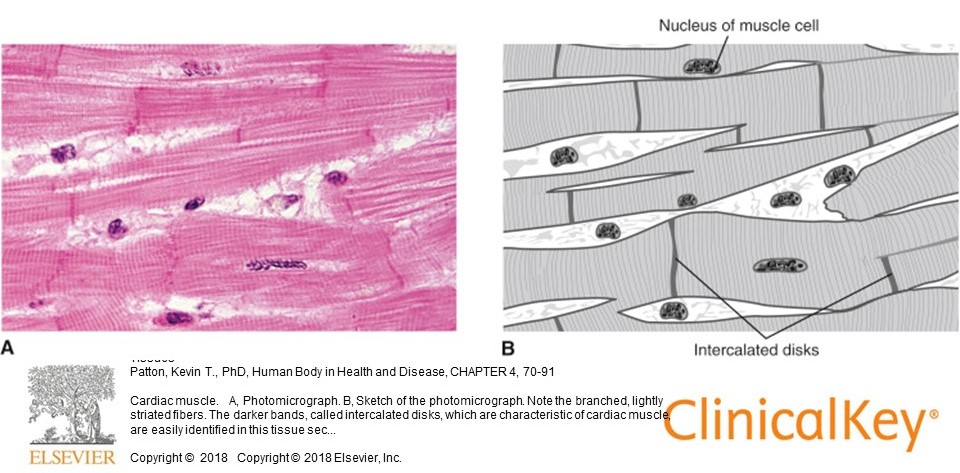
cardiac myocytes
Intercalated discs: The dark bands in the image above are the intercalated discs, where the plasma membrane of two adjacent cardiac muscle cells join together. They contain desmosomes and gap junctions that connect cardiac muscle cells
Desmosomes: Anchoring proteins that link adjacent cardiac muscle cells. They provide a mechanical connection between these cells so that they don’t separate from each other during muscle contraction
Gap junctions: Provide an electrical connection between adjacent myocytes. They form a pore between adjacent cells that allows ions to flow from one cell to another, transmitting the electrical signal throughout the heart. This means that when cardiac muscle cells depolarise, this depolarisation spreads from cell to cell across the heart. This electrical connection is critical for allowing the heart to contract as a unit in a coordinated manner
Mitochondria: Cardiac myocytes have lots of mitochondria, as they rely almost exclusively on aerobic metabolism for energy. This means that the heart cannot operate effectively if deprived of oxygen for any period of time
types of cardiac myocytes
A feature of the heart is that it can generate its electrical activity without relying on input from nerves. This ability to generate electrical energy is what allows the heart to beat spontaneously - if you cut all of the nerves supplying the heart (such as in a heart transplant), the heart will still beat. This unique property of the heart is due to the different types of cardiac myocytes in the heart
The vast majority of cardiac myocytes are contractile myocytes - these are the cells that contract and generate force and are responsible for the pumping action of the heart
However, a small number (~1%) of cardiac myocytes in particular places in the heart are non-contractile, autorhythmic cells. These cells are also known as pacemaker cells, and they can depolarise spontaneously and generate their action potentials. It is these cells that allow the heart to beat on its own
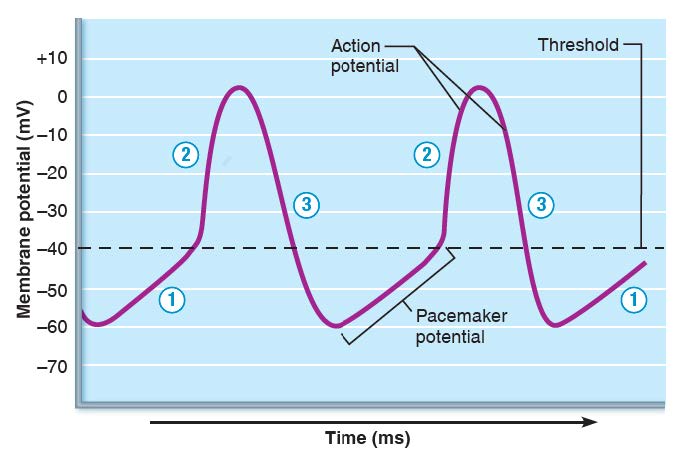
action potentials in pacemakers cells
Pacemaker cells can generate their action potentials because they have an unstable resting membrane potential - when this unstable potential reaches the threshold, an action potential will fire
Pacemaker potential - slow, spontaneous depolarisation due to slow entry at Na+
Depolarisation - at threshold, Ca2+ causes depolarisation and rising phase of action potential
Repolarisation - Ca2+ channels inactivate, repolarisation (falling phase of action potential) is due to opening of K+ channels and exit of K+ from cell
Whilst the pacemaker cells in the heart allow it to contract without requiring a neural signal or input, that doesn’t mean that the heart is completely independent of the NS. The autonomic NS is an important regulator of heart rate
The action potentials and electrical activity generated by pacemaker cells can spread to other adjacent cells via gap junctions. When action potentials are generated in contractile cardiac myocytes, this causes contraction of these muscle cells. The coordinated spread of electrical activity is what ensures the heart contracts in a co-ordinated manner
electrical conduction in the heart
The cardiac cycle consists of both electrical events (depolarisation and repolarisation) and mechanical events (contraction and relaxation) that occur in a coordinated way so that the heart can pump efficiently
Cardiac myocytes are electrically connected by gap junctions, which allows electrical activity to spread from cell to cell
Within the heart, the cardiac conduction system is a network of specialised cells that generate and spread electrical activity through the heart. This coordinated spread of electrical activity through the heart ensures that the atria and ventricles contract (and relax) in the correct order to maintain the proper flow of blood through the heart
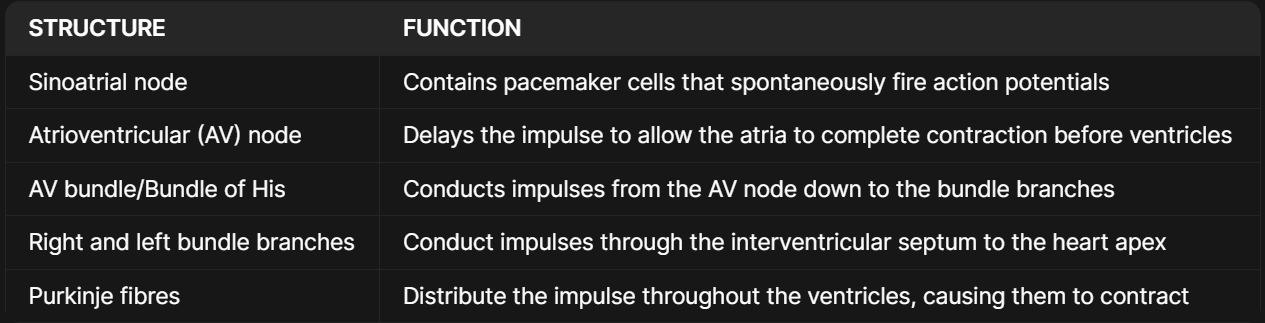
cardiac conduction system
The heart contains a small number of cardiac myocytes that are non-contractile and autorhythmic. These cells are an important component of the cardiac conduction system, which acts to generate and spread electrical activity through the heart in a coordinated manner
In a healthy heart, pacemaker cells in the sinoatrial (SA) node generate the electrical impulses that travel through the heart. The rate at which these autorhythmic pacemaker cells in the SA node depolarise and generate action potentials is what determines the heart rate
If the pacemaker cells depolarise and fire action potentials more frequently, heart rate will increase. If the pacemaker cells depolarise and fire action potentials less frequently, heart rate will decrease
cardiac conduction pathways
Depolarisation begins in the SA node and spreads through the atria
Depolarisation spreads to the AV node via internodal pathways
Depolarisation moves through the septum to the heart apex via the AV bundle (Bundle of His) and bundle branches
Depolarisation spreads from the apex through the ventricles via Purkinje fibres
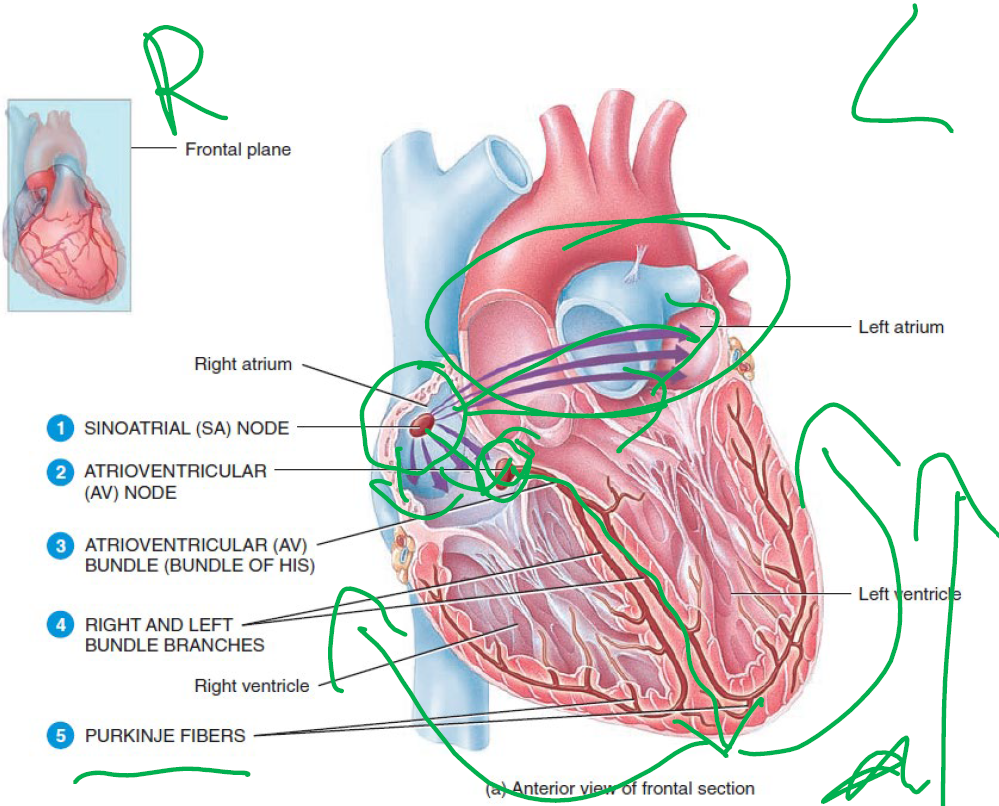
structure and function involved in cardiac conduction pathway
Note: Normally, the pacemaker cells in the SA node determine the heart rate. However, there are also other cells in the cardiac conduction system (e.g. in the AV node or Purkinje fibres) that can also act as pacemakers if the SA node is damaged. These other pacemaker cells have a slower rate of spontaneous depolarisation than the pacemaker cells in the SA node
What structure determines heart rate in a healthy heart? How does it do this?
The sinoatrial (SA) node determines the heart rate in a health heart. This is because the SA node contains autorhythmic pacemaker cells that spontaneously fire action potentials. This electrical activity then spreads through the cardiac conduction system.
What would happen if the SA node is damaged? How would the heart rate compare to a healthy, undamaged heart?
If the SA node was damaged, then other autorhythmic cells found in other parts of the cardiac conduction system would take over (e.g. in the AV node). The heart rate would be slower in this example, as the rate of spontaneous depolarization is slower in these cells than the cells in the SA node. This means it will take longer for these cells to hit threshold to fire an action potential, therefore decreasing the rate of action potential firing.
What would happen if the AV node is damaged, so that electrical signals could not pass through this area? How would cardiac contraction be affected?
If the AV node was damaged and electrical signals could not pass through, the coordination between the atria and ventricles would be lost. The pacemaker cells in the SA node would fire action potentials that would spread through the atria as normal, but these would not continue to the ventricle. Autorhythmic cells in the Purkinje fibres would take over as pacemakers for the ventricles, however these would not be coordinated with the electrical activity in the atria. This means that the atria and ventricles would be contracting independently of each other, and the heart would no longer operate effectively as a pump.
heart repolarisation
The repolarisation of the atria and ventricles is critical because the repolarisation of cardiac myocytes is what causes the relaxation of the muscle
Relaxation is particularly important in the heart, as it is during the relaxation phase (diastole) that the chambers of the heart fill with blood, ready to be pumped out into the circulation with the next contraction
electrocardiogram (ECG)
Uses recording electrodes placed on the body surface to measure the electrical activity of the heart. The ECG does not detect individual action potentials, but rather it represents the overall electrical activity in the heart
The ECG is an important diagnostic tool for clinicians, as many types of cardiac disease or damage can cause disturbances in heart rate or rhythm
An ECG can also be useful in diagnosing other cardiac pathologies (e.g. tissue damage from lack of oxygen or enlargement of the heart)
3 key waves include P wave, QRS complex and T wave
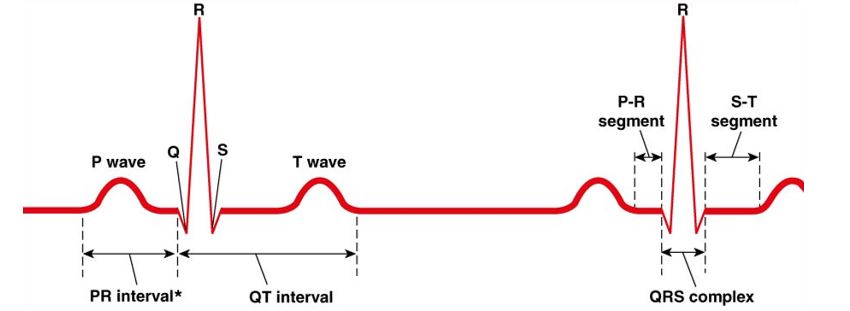
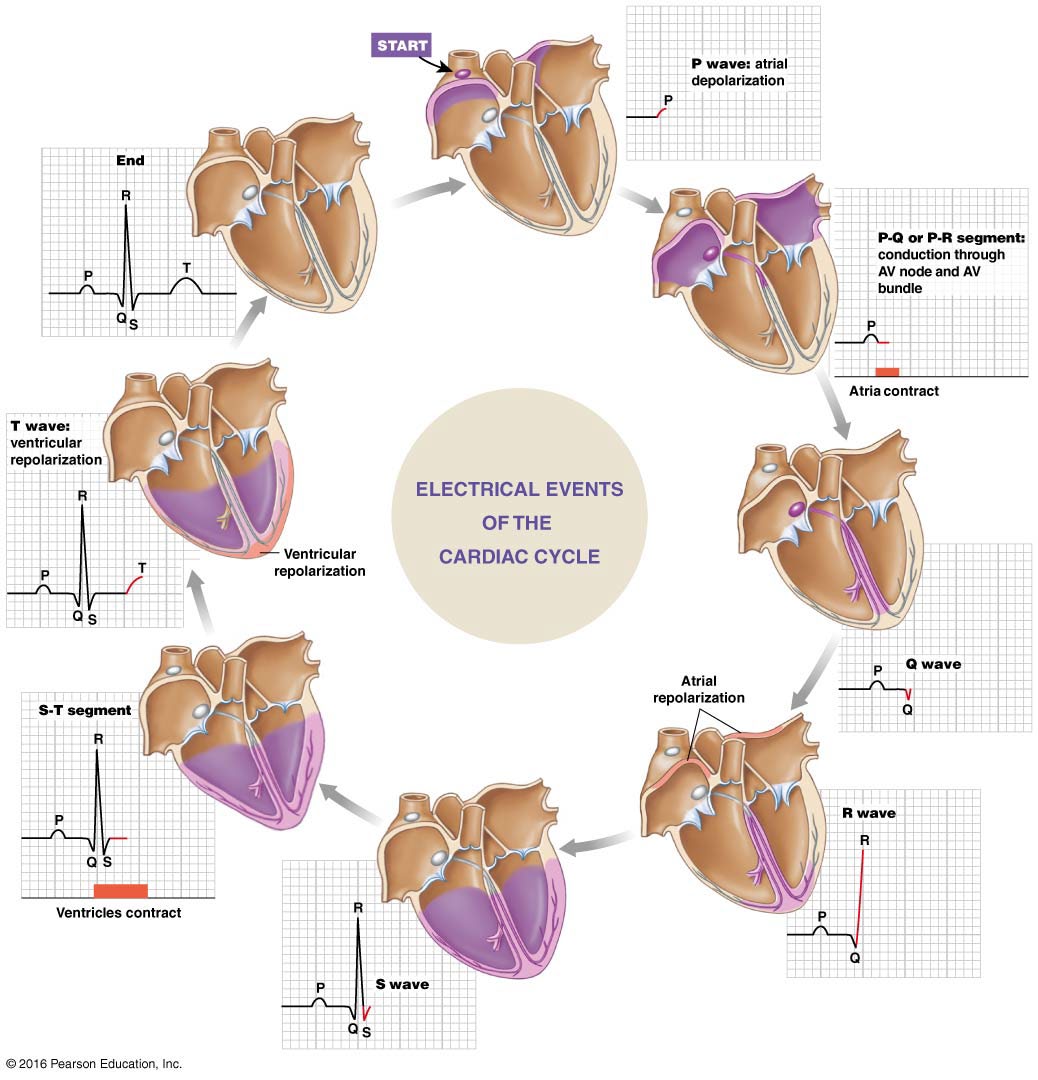
electrical events of the cardiac cycle
P wave: atrial depolarisation
QRS complex: ventricular depolarisation
T wave: ventricular repolarisation
The P wave is smaller than the QRS complex because the atrial muscle mass < ventricular muscle mass
In a normal ECG, atrial repolarisation is masked by the QRS complex
Note: purple colour represents the electrical activity in the image
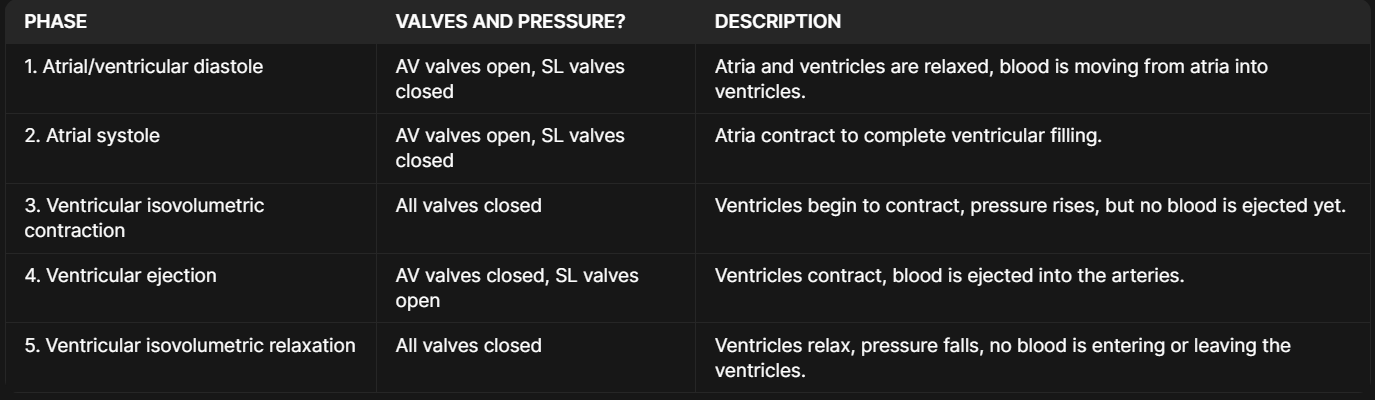
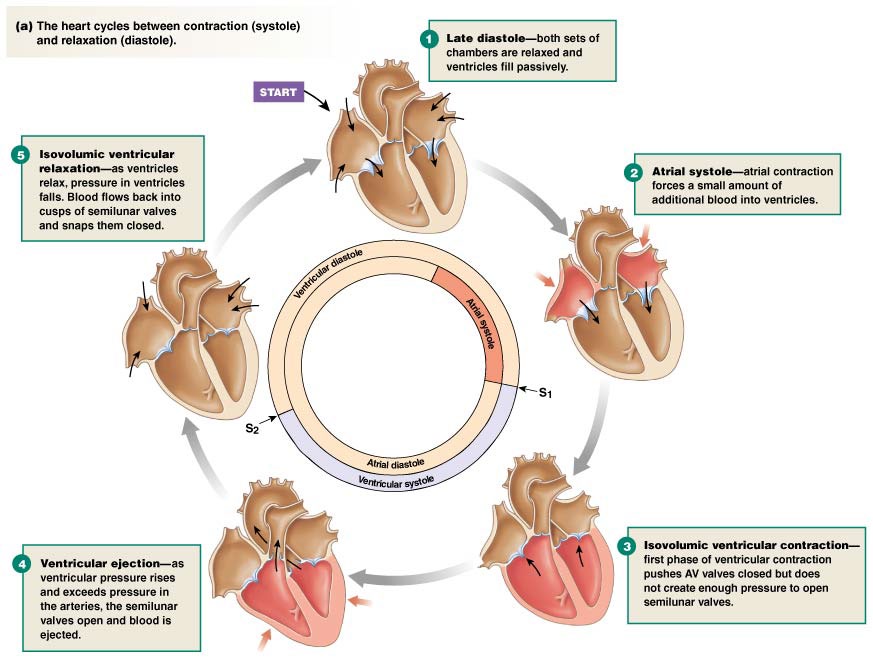
phases of the cardiac cycle
The electrical activity of the heart drives the mechanical activity: depolarisation of cardiac muscle causes contraction and repolarisation of cardiac muscle causes relaxation
The atria and ventricles don’t contract in unison - rather, the regulated spread of electrical activity through the cardiac conduction system causes the atria and ventricles to contract and relax in a coordinated manner
The contraction and relaxation of the different heart chambers causes changes in pressure in the different chambers.
When a chamber contracting (systole), pressure in that chamber increases. When a chamber is relaxing (diastole), pressure in that chamber decreases.
These changes in pressure drive the movement of blood through the heart and circulation, as blood flows from an area of high pressure to an area of lower pressure. These changes in pressure also trigger the opening and closing of the cardiac valves that maintain blood flow in the heart
phase 1&2 of cardiac cycle
When the heart is at rest, both atria and ventricles are relaxed and are passively filling with blood (atrial and ventricular diastole)
Depolarisation of the atria causes atrial contraction (atrial systole). Additional blood is pushed out of the atria and into the ventricles. At this stage, the ventricles are still relaxed
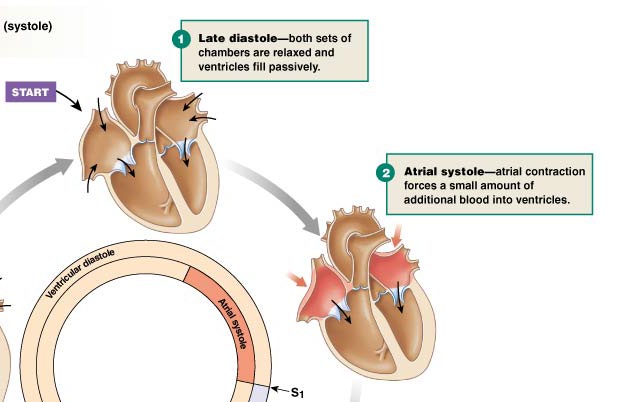
phase 3 of cardiac cycle
As the depolarisation spreads to the ventricles, they begin to contract
This increases the pressure inside the ventricles. When the pressure inside the ventricles is higher than the pressure in the atria, the AV valves will close
At this stage, pressure in the ventricles remains lower than the aorta/pulmonary artery, so the semilunar valves stay closed whilst the ventricles are contracting (isovolumetric contraction)
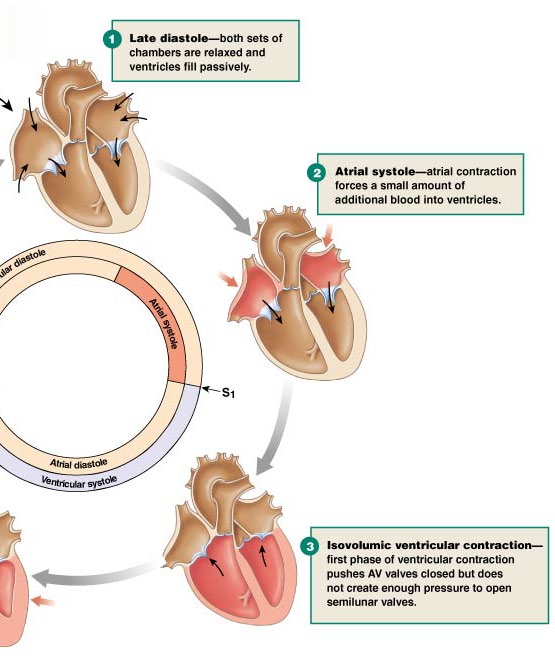
phase 4 of cardiac cycle
As the ventricles continue to contract, the pressure in the ventricles keeps increasing
When the pressure in the ventricles exceeds the pressure in the aorta/pulmonary artery, the semilunar valves will open
Blood will now flow out of the ventricles and into these arteries (ventricular ejection)
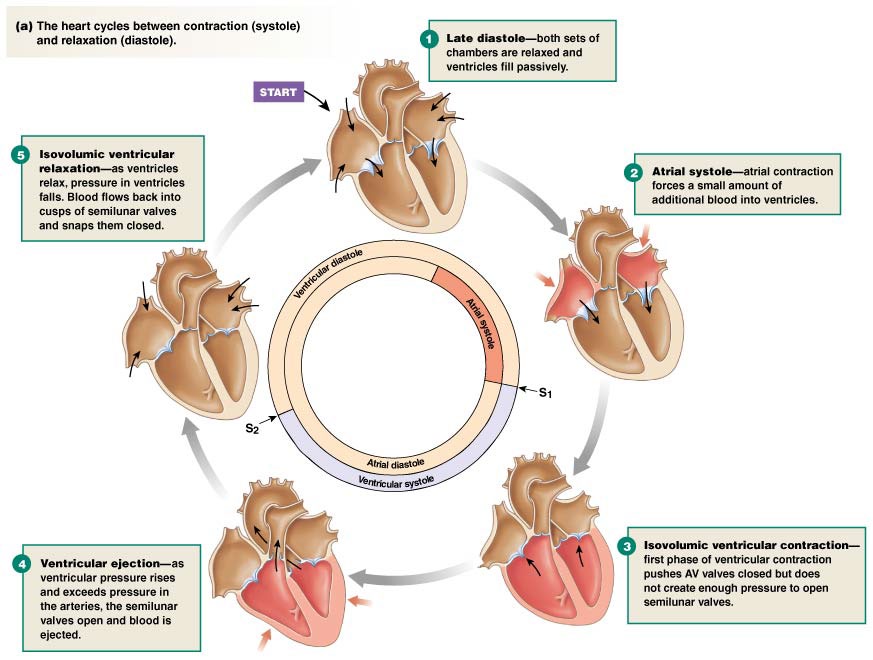
phase 5 of the cardiac cycle
As the ventricles repolarise, they begin to relax. Pressure inside the ventricles decreases
When pressure in the ventricles drops below the pressure in the aorta/pulmonary artery, the SL valves will close. The ventricles continue to relax whilst all valves are closed (isovolumetric relaxation)
When the pressure in the ventricles drops below atrial pressure, the AV valves will open again and ventricular filling begins (atrial and ventricular diastole)
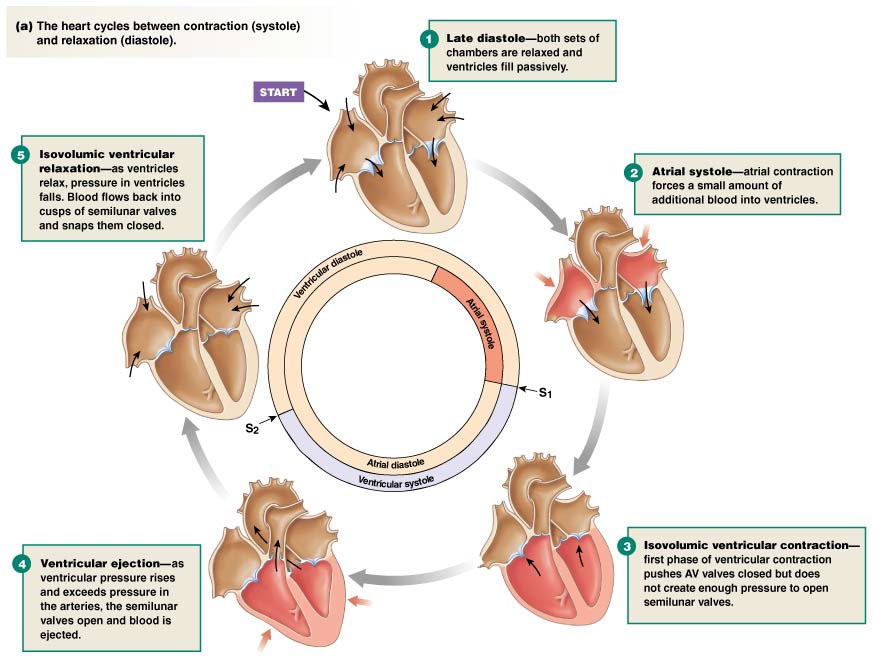
phases of cardiac cycle summary
heart sounds
If you use a stethoscope to listen to the heart (a process known as auscultation), you will usually hear two sounds associated with each heartbeat
These sounds are associated with the closure of the different valves in the heart. The first sound (‘lubb’) is usually louder and longer and is associated with the closure of the AV valves. The second sound (‘dup’) is usually softer and shorter and is associated with the closure of the SL valves
S1: closure of AV valves & S2: closure of SL valves (see image)
cardiac output
The amount of blood that is pumped out of the heart each minute. In a typical healthy adult at rest, the cardiac output is ~ 5 L/min
The typical adult blood volume is also about 5 L, so this means that your entire blood volume passes through your circulation each minute
Cardiac output is variable and can increase according to body demands (e.g. during exercise)
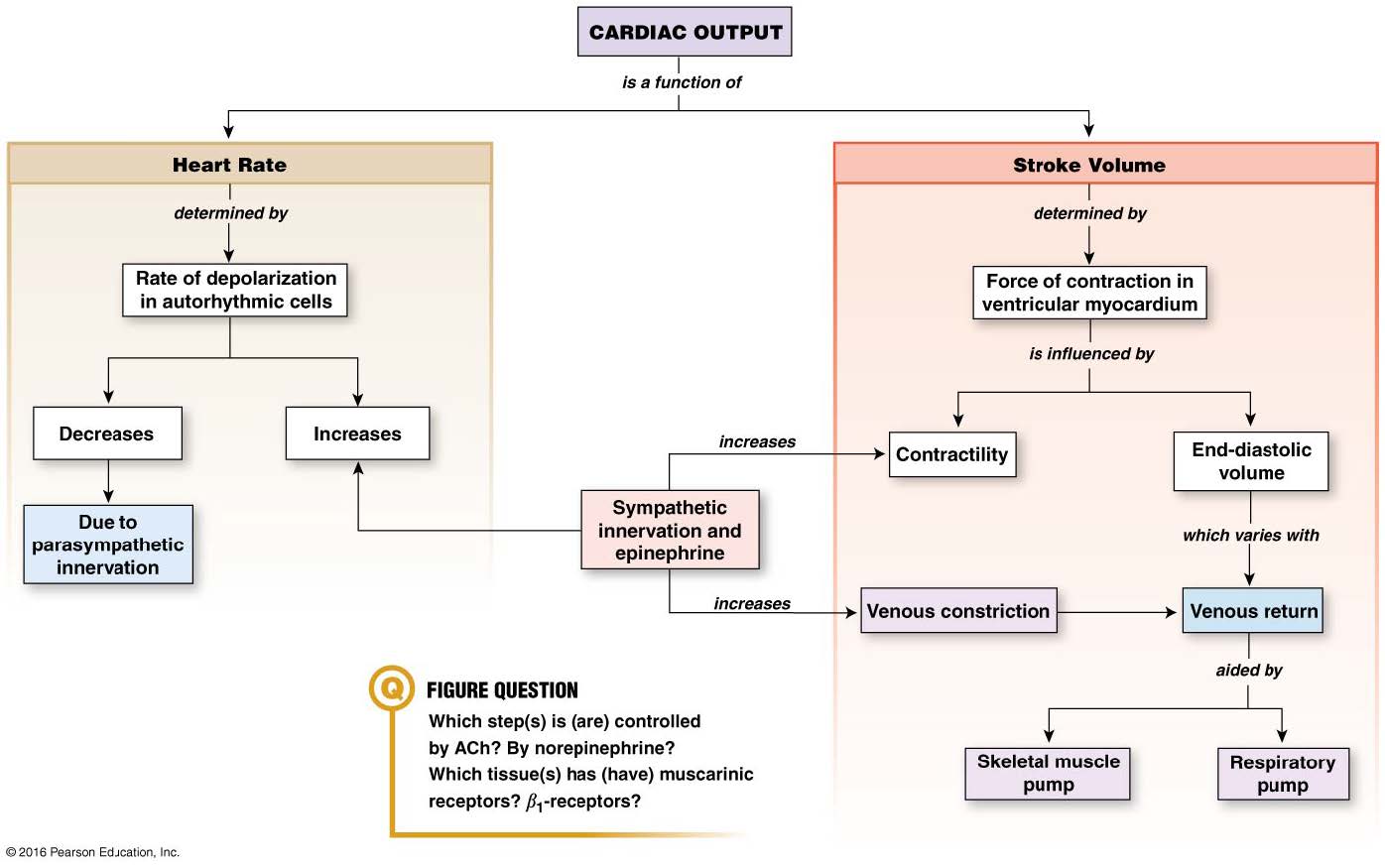
determinants of cardiac output
Cardiac output (CO) is defined as the amount of blood that is pumped out of each ventricle per minute. Two factors determine cardiac output: the heart rate (HR) and the stroke volume (SV)
The heart rate is a measure of how often the heart contracts and is measured in beats per minute (bpm). The stroke volume is the volume of blood that is pumped out of the ventricle in a single contraction (beat)
The cardiac output is the product of heart rate and stroke volume, so we can calculate cardiac output by multiplying these factors together (CO = HR x SV)
effect of heart rate on cardiac output
Autorhythmic (pacemaker) cells in the SA node of the heart spontaneously fire action potentials, and it is these action potentials that lead to cardiac contraction
The rate at which the SA node fires action potentials, therefore, determines our heart rate. If the SA node is firing more frequently, then the heart rate will increase. Similarly, if the SA node fires less frequently, the heart rate will decrease
Heart rates will vary throughout the day with different types of activity - for example, increases in heart rate during exercise and decreases in heart rate during sleep
However, persistent changes in heart rate can be a sign of cardiovascular disease. Tachycardia is an abnormally fast resting heart rate, whilst bradycardia is an abnormally slow resting heart rate
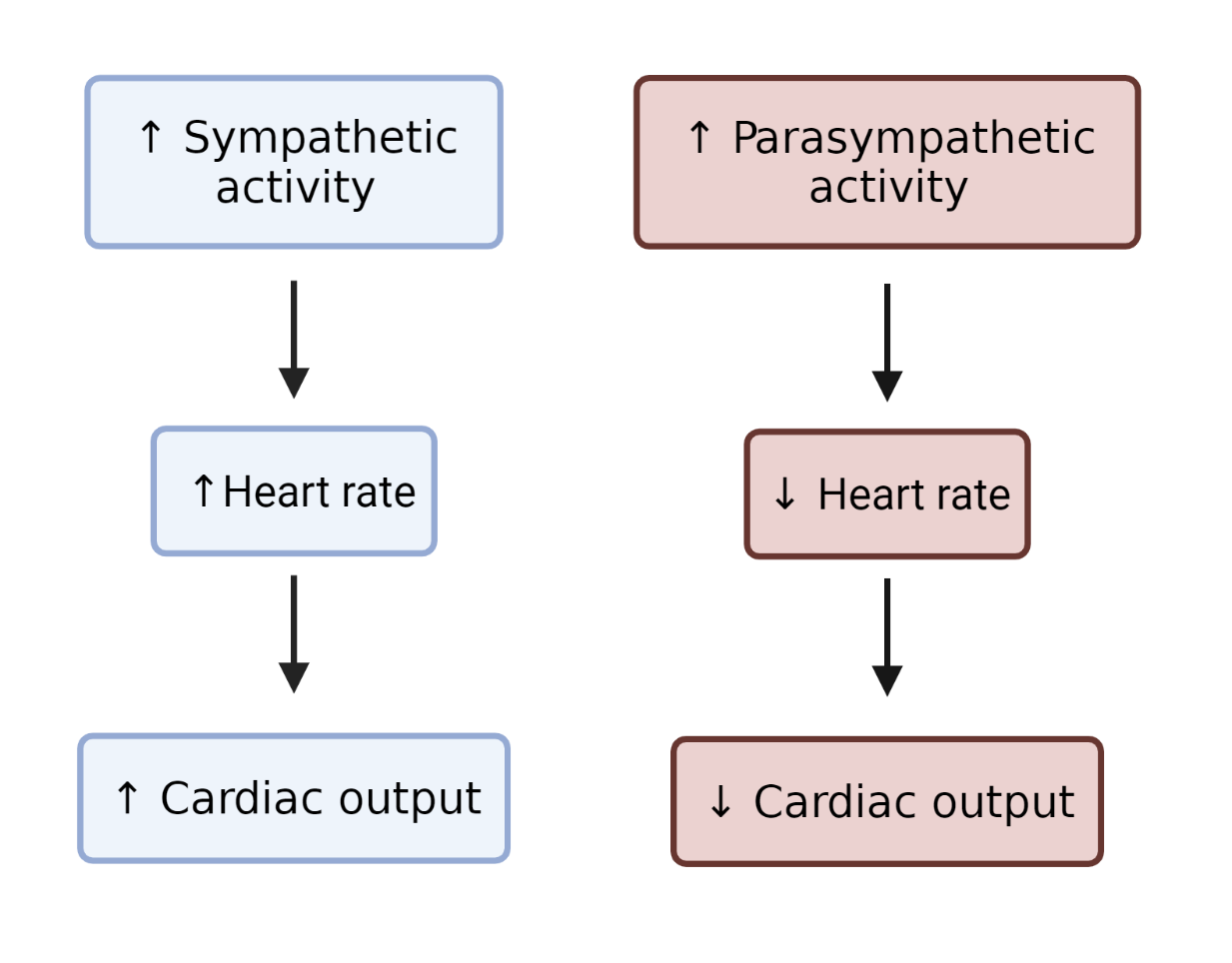
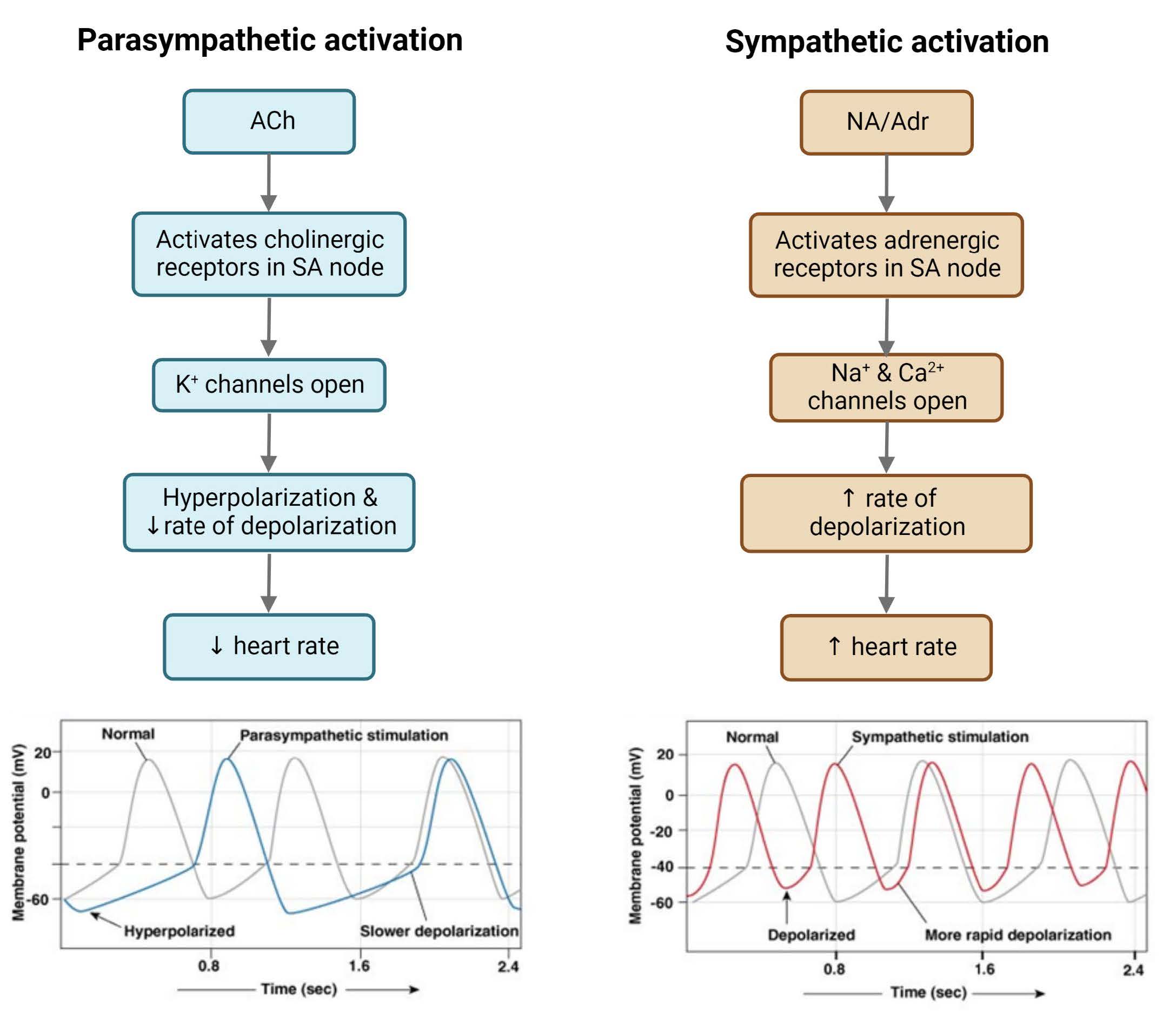
ANS as a regulator of heart rate
The SA node of the heart is innervated by both parasympathetic and sympathetic nerves, so both branches of the autonomic NS can influence heart rate
Activation of the sympathetic NS causes the SA node to fire more rapidly, which increases the heart rate.
In contrast, activation of the parasympathetic NS causes the SA node to fire less rapidly, which decreases heart rate
This means that the autonomic NS can also alter cardiac output. If the sympathetic NS is activated, the heart rate will increase, causing an increase in cardiac output. If the parasympathetic NS is activated, the heart rate will decrease, causing a decrease in cardiac output
The ANS regulates heart rate by changing the rate of spontaneous depolarisation in the pacemaker cells. It does this by altering the opening and closing of different ion channels and, therefore, altering ion permeability
autonomic control of heart rate
Several factors can affect heart rate, including circulating hormones. For example, adrenaline (which is released into the circulation from the adernal medulla during sympathetic NS activation) and thyroxine (a thyroid gland hormone) are examples of hormones that increase heart rate
Changes in plasma ion levels can also affect heart rate, and imbalances in plasma electrolytes can lead to the risk of serious damage to the heart. In particular, changes in blood K+ or Ca2+ can be potentially life-threatening due to effects on electrical activity and risk of arrhythmias
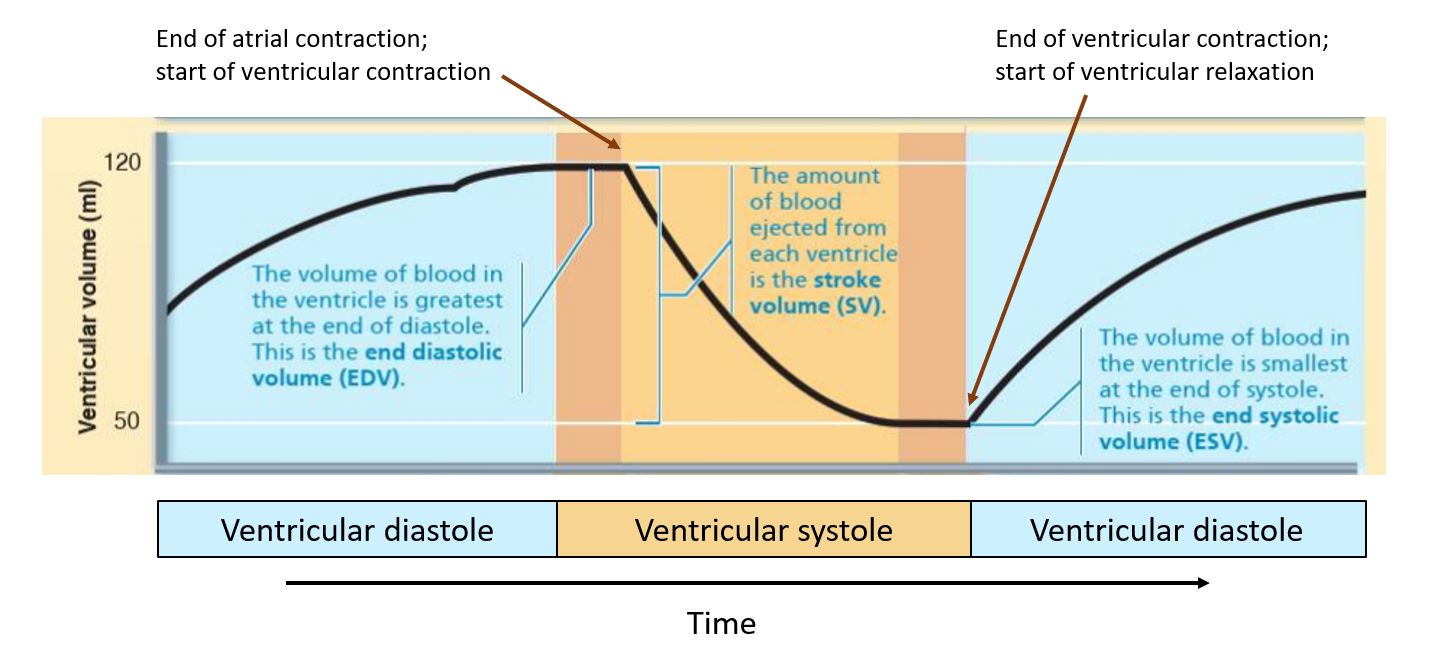
effect of stroke volume on cardiac output
The stroke volume is the amount of blood that is pumped out of the ventricle in a single contraction (beat) of the heart. Stroke volume is the difference between the end diastolic volume (EDV) and the end systolic volume (ESV)
End diastolic volume: volume of blood in the ventricle at the end of diastole (i.e. how much blood has collected in the ventricle before it begins to contract)
End systolic volume: volume of blood that is left in the ventricle at the end of systole (i.e. how much blood remains in the ventricle after it has contracted)
A key factor that determines ESV is the contractility of the heart, which describes the ability of the heart to generate force
The main factor that determines EDV is the venous return (VR), or the amount of blood being returned to the heart - a larger venous return means a larger EDV
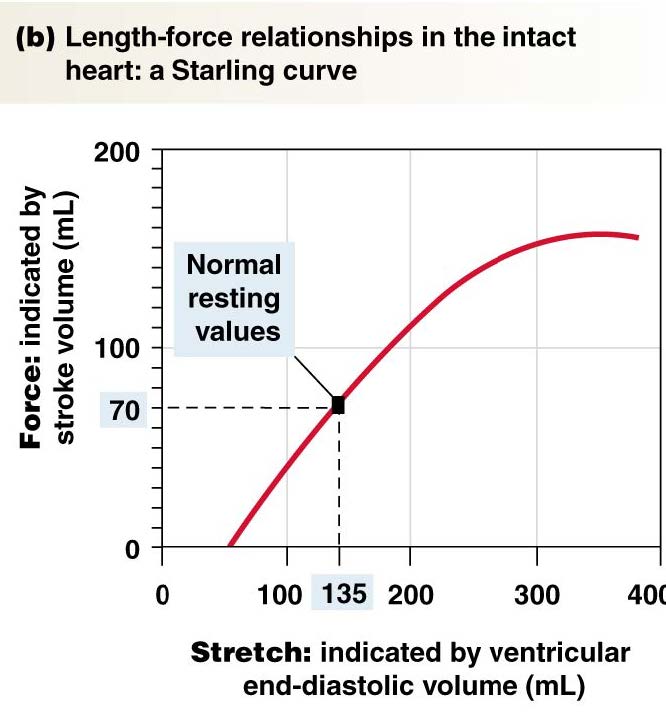
EDV, VR and stroke volume: Frank-Starling Law of the Heart
The end diastolic volume (EDV) is one of the most important determinants of stroke volume. This is because cardiac muscle displays a length-tension relationship: how much stretch is on the muscle before it begins to contract affects the amount of force the contracting muscle can generate (more stretch = greater force generated during contraction)
The amount of stretch on the muscle before it begins to contract is determined by the amount of blood returning to the heart (the venous return), as a more significant venous return will cause more distension or stretch of the ventricular wall
The relationship between EDV and stroke volume is essential, as it is a mechanism that allows the heart to increase its force of contraction when more blood is returned to the heart. This is known as the Frank-Starling law of the heart
Frank-Starling Law: Increases in EDV lead to an increase in SV
The more blood that is returned to the heart, the greater the stretch on this ventricular wall. This increases the force of contraction so that the heart can eject more blood
factors affecting venous return/end diastolic volume
Affected by both the venous pressure and the duration of ventricular diastole. Increases in venous pressure will increase venous return
3 physiological mechanisms help to maintain venous pressure and venous return:
Skeletal muscle pump: Many deep veins in the body are surrounded by skeletal muscle. As the skeletal muscles adjacent to these veins contract and relax, they act as a pump that squeezes the veins, propelling blood back towards the heart. The action of the skeletal muscle pump is actively dependent - standing still for long periods can cause blood to pool in the feet and legs, causing swelling and even fainting as the lack of skeletal muscle activity reduces venous return
Respiratory pump: Breathing in increases abdominal pressure, which squeezes adjacent veins and propels back blood to the heart
Sympathetic constriction of veins: Veins are innervated by the SNS. Activation of the SNS causes constriction (narrowing) of the veins, propelling blood back to the heart
Decreases in the duration of ventricular diastole will decrease venous return. Diastole is when the ventricles are relaxing, and blood is being returned to the heart and filling the ventricles. If this filling time is reduced to the heart before the next contraction. Extremely high heart rates can, therefore, lead to a decrease in venous return due to this reduction in filling time

What is end diastolic volume? How does an increase in end diastolic volume affect cardiac output?
End diastolic volume is the volume of blood in the ventricle at the end of diastole, immediately before the ventricles begin to contract. Increases in EDV cause the heart to contract with more force, increasing stroke volume to increase cardiac output.
Hayley has severe tachycardia that is causing her heart to beat extremely fast. How might that affect her end diastolic volume?
An extremely fast heart rate will mean that the time the heart spends in diastole (relaxing and filling between contractions) is reduced. If the time spent in diastole is very short, there may not be enough time for ventricles to fill adequately before the next contraction. This will decrease end diastolic volume.
How do exercises such as running and cycling increase venous return?
Exercises such as running and cycling use the large muscle groups in the legs. The contraction and relaxation of these muscles helps to promote venous return via the skeletal muscle pump, whereby the external compression (and relaxation) of the veins by the adjacent skeletal muscle helps to propel blood back to the heart. Exercise also stimulates the sympathetic nervous system, which increases venous return by causing vasoconstriction of systemic veins.
factors affecting end systolic volume/cardiac contractility
The end-systolic volume (ESV) is the volume remaining in the ventricle at the end of the contraction. The main factor that determines ESV is the contractility of the heart
Cardiac contractility is the amount of force that can be generated by the heart at a given muscle length (which is determined by the EDV). Muscle (including cardiac muscle) contains contractile proteins, and it is the activation of contractile proteins that allows the muscle to generate force and shorten
The main regulator of these contractile proteins is Ca2+ - if more Ca2+ ions enter the cytoplasm of the cell, more contractile proteins are activated, and more force is generated. Cardiac contractility is therefore increased when more Ca2+ ions enter the cytoplasm and interact with the contractile proteins
There are many different types of chemicals (e.g. hormones, medications) that can influence cardiac contracility. Substances that increase cardiac contractility are called positive inotropes and include hormones such as adrenaline. Substances that decrease cardiac contractility are called negative inotropes
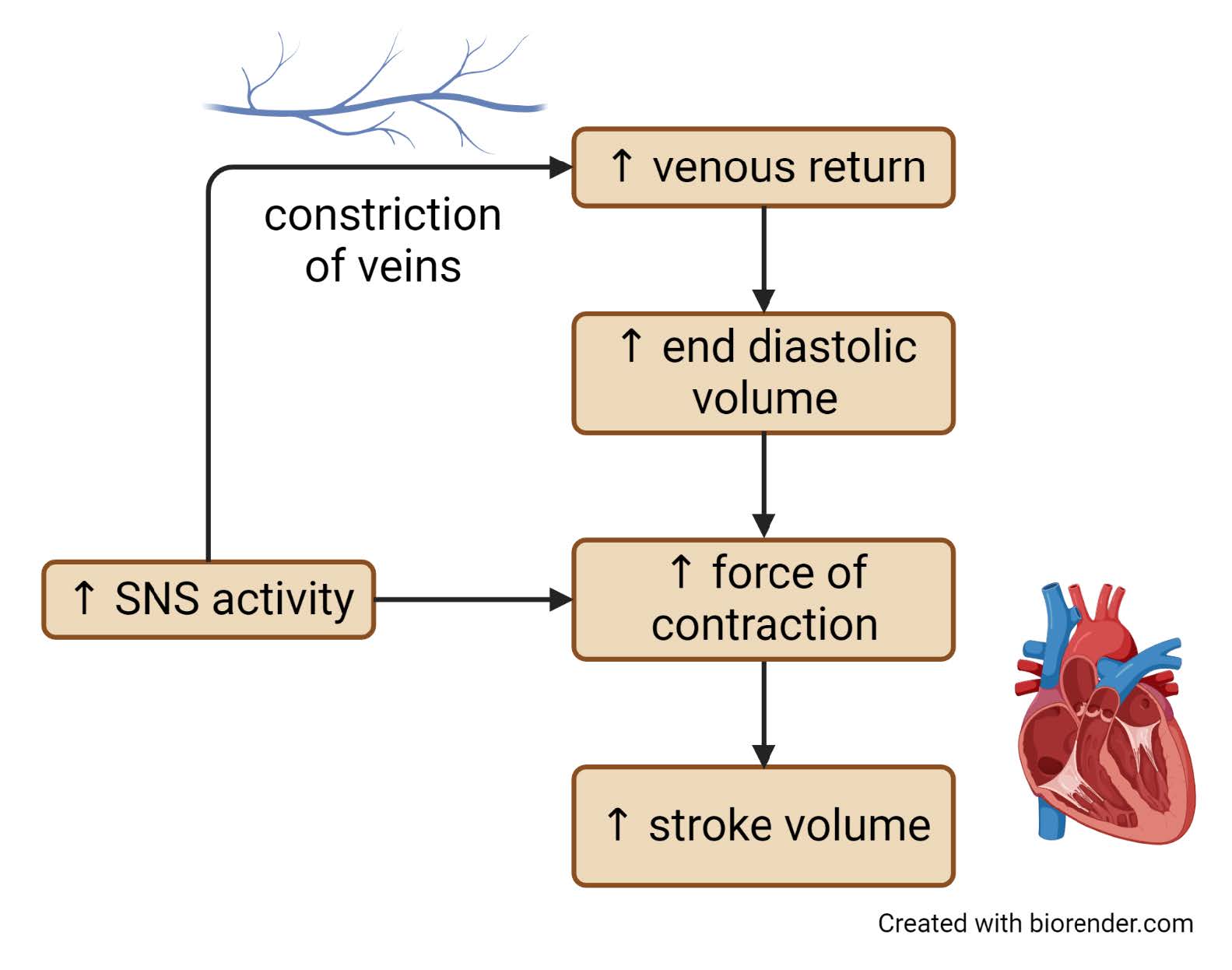
parasympathetic vs sympathetic NS regulation of heart rate
Whilst the sympathetic NS is a key regulator of both heart rate AND stroke volume, the parasympathetic NS regulates heart rate but has very little effect on stroke volume
This is due to the innervation of the heart by the autonomic NS. The SNS innervates both the SA node and ventricular wall, so the neurotransmitters released with SNS activation can affect both heart rate (through actions on the SA node) and stoke volume (through actions on the ventricular wall)
In contrast, the parasympathetic NS innervates the SA node but not the ventricles, so the transmitters released with parasympathetic NS activation will affect the heart rate (through actions on the SA node) but not the ventricles
factors determining cardiac output
blood vessels
There are 5 main types of blood vessels: arteries, arterioles, capillaries, venules and veins
When the heart contracts, blood is pushed from the ventricles into the arteries. Arteries are large, muscular vessels that carry blood away from the heart. These arteries branch off to produce small arteries and finally the arterioles
The arterioles carry blood into the tissues and organs of the body, feeding blood into the branched capillaries. It is in these capillaries that the exchange of substances between blood and tissues occurs
Blood drains out of the capillaries into small veins called venules. These venules then merge to form progressively larger and larger veins. It is these veins that then return blood to the heart
Blood vessels overview - functional roles
Arteries act as pressure reservoirs
Arterioles provide variable resistance
Exchange takes place in the capillaries
Veins act as volume reservoirs
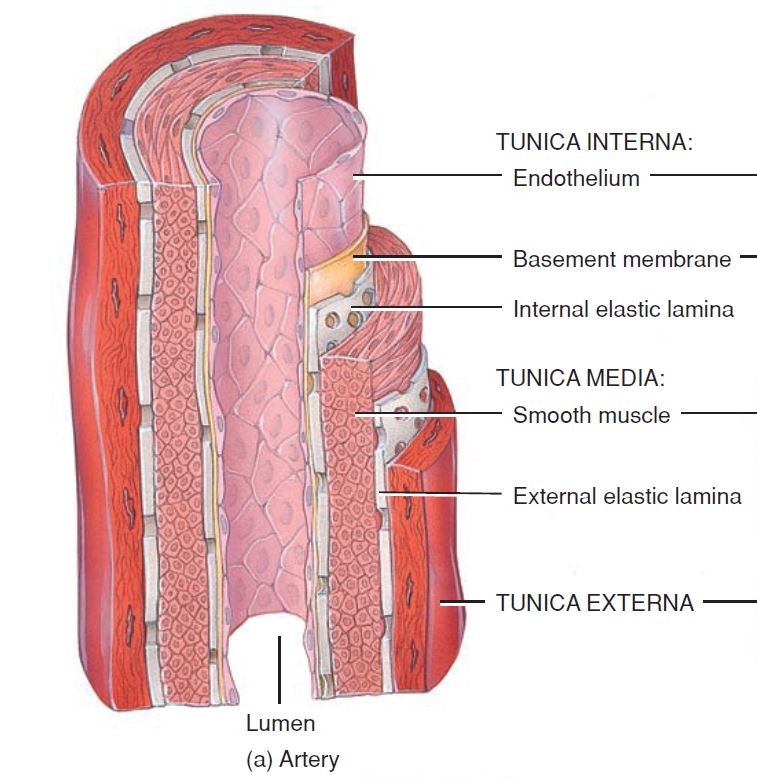
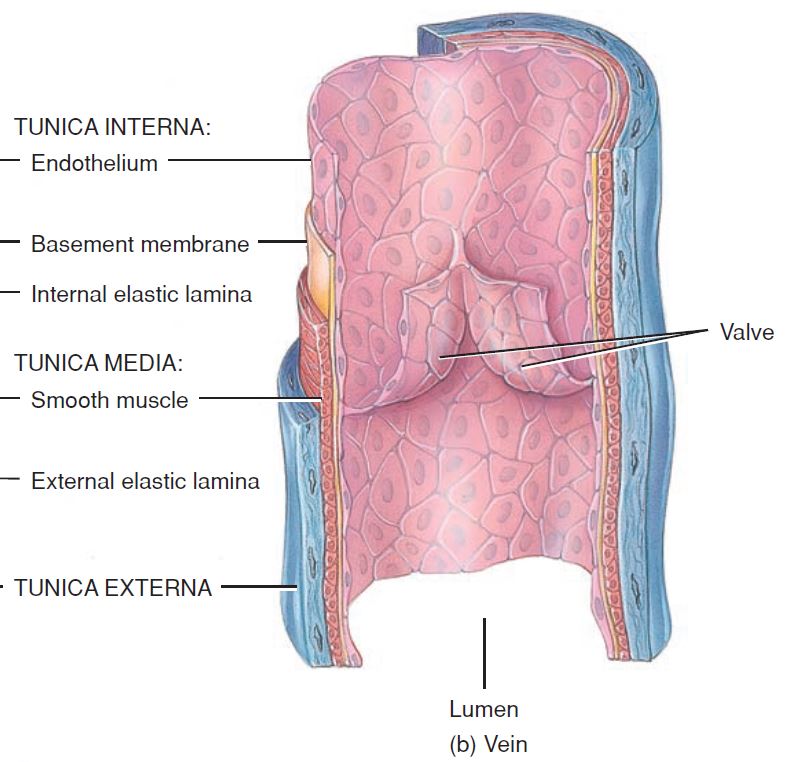
layers in an artery - blood vessel layers
The walls of most blood vessels are made up of 3 layers (or tunics). The space within the blood vessel (which the blood travels through) is called the vessel lumen
The tunica interna (also called the tunica intima) is the innermost layer of the blood vessel and is in direct contact with the blood that is flowing through the vessel lumen
The innermost part of the tunica interna is the endothelium, which is a layer of simple squamous epithelium that lines the inside of all blood vessels
The endothelium plays an active role in blood vessel function, as it can synthesise and release chemical substances that regulate functions such as the constriction and dilation of blood vessels and the initiation of blood clotting. The endothelium is supported by a basement membrane and connective tissue
layers in a vein - blood vessel layers
The tunica media is the middle layer of the vessel wall. It contains elastic fibres and smooth muscle cells arranged circularly around the vessel (in the same way that a ring encircles your finger)
The smooth muscle in this layer is what allows blood vessels to change their diameter in response to the NS or chemicals/hormones in the blood
When the smooth muscle in the vessel wall contracts, this decreases the vessel diameter. This narrowing of the vessel is called vasoconstriction
When the smooth muscle in the vessel wall relaxes, this increases the vessel diameter. This widening of the vessel is called vasodilation
These changes in vessel diameter are what allow the body to regulate and change the amount of blood flow to different organs and tissues, depending on demand
Arteries and arterioles have more smooth muscle and a thicker tunica media than veins
The outer layer of the blood vessel wall is the tunica externa or tunica adventitia, which contains elastic fibres and connective tissues that help to protect and support the vessel
REVIEW - blood vessels
Arteries
contains all 3 layers (tunica interna, tunica media and tunica externa) that can be found in blood vessels.
Relative to their vessel size, arteries have the largest amount of smooth muscle in their walls of any other blood vessels types
Like with other vessel types, the structure and composition of the artery wall are important for the function of that artery type
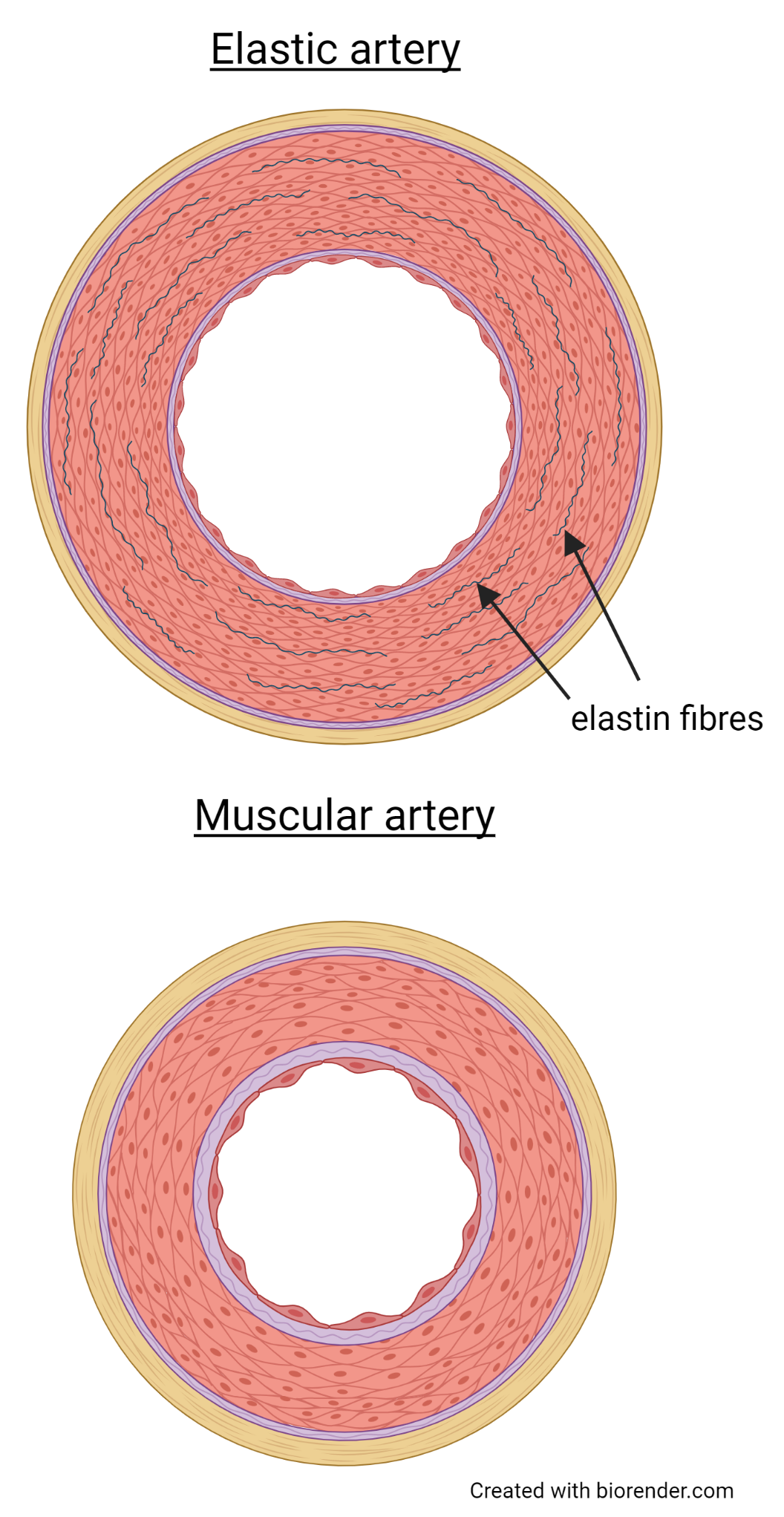
elastic artery
Large, thick-walled arteries that are located closest to the heart. Their thick walls help them to withstand the high pressures generated by the contraction of the heart
Elastic arteries contain a large amount of a protein called elastin in their vessel wall, and it is the presence of this elastin that makes these arteries very elastic
This elasticity allows these arteries to act as pressure reservoirs. They expand during ventricular contraction, and then recoil during ventricular relaxation
The elastic recoil of the arterial wall maintains arterial pressure during ventricular relaxation, which helps to maintain a relatively constant flow of blood into the circulatory system
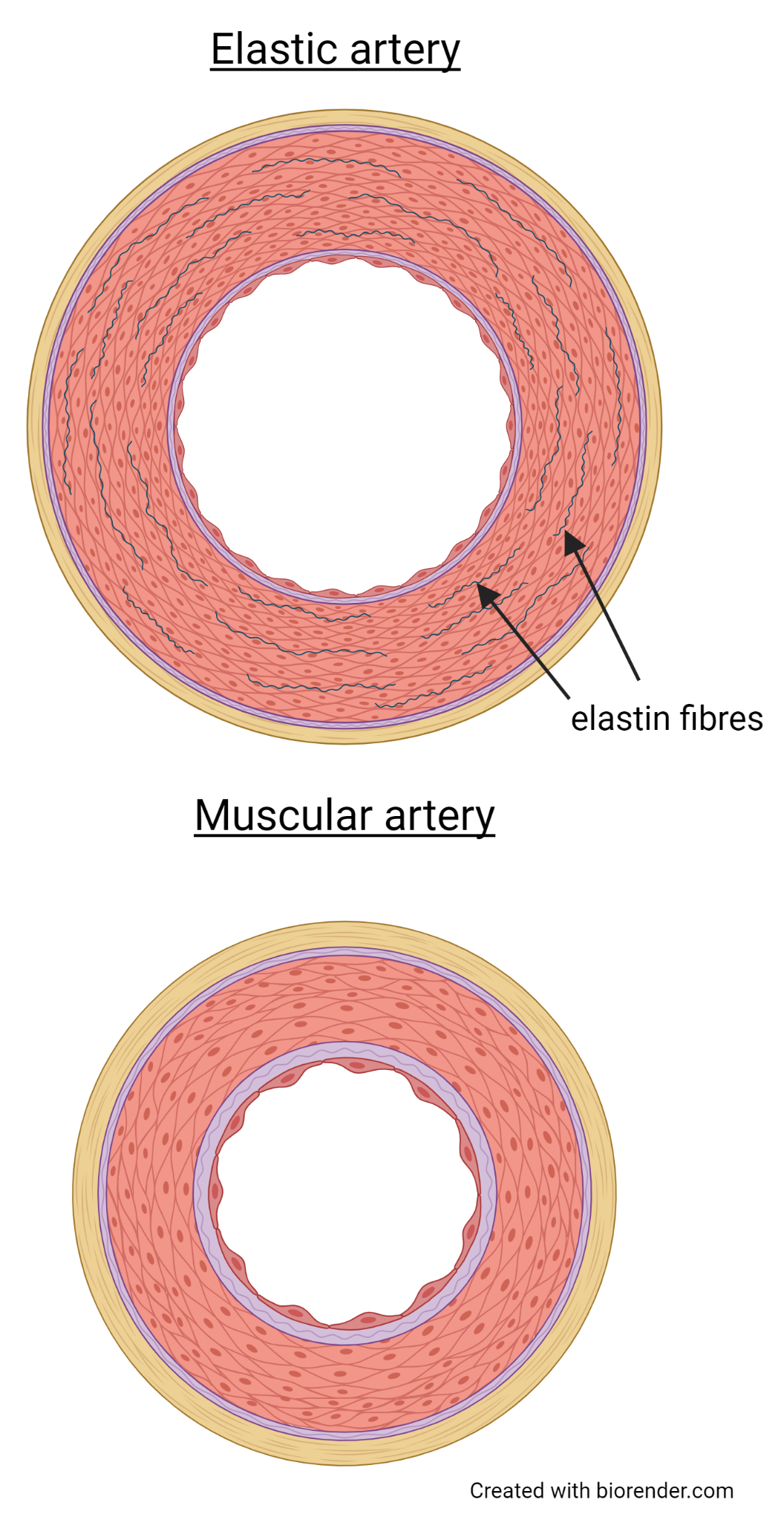
muscular arteries
Located distal to the elastic arteries. These muscular arteries distribute blood to the organs in the body
They have a thick muscular tunica media but less elastin than the elastic arteries
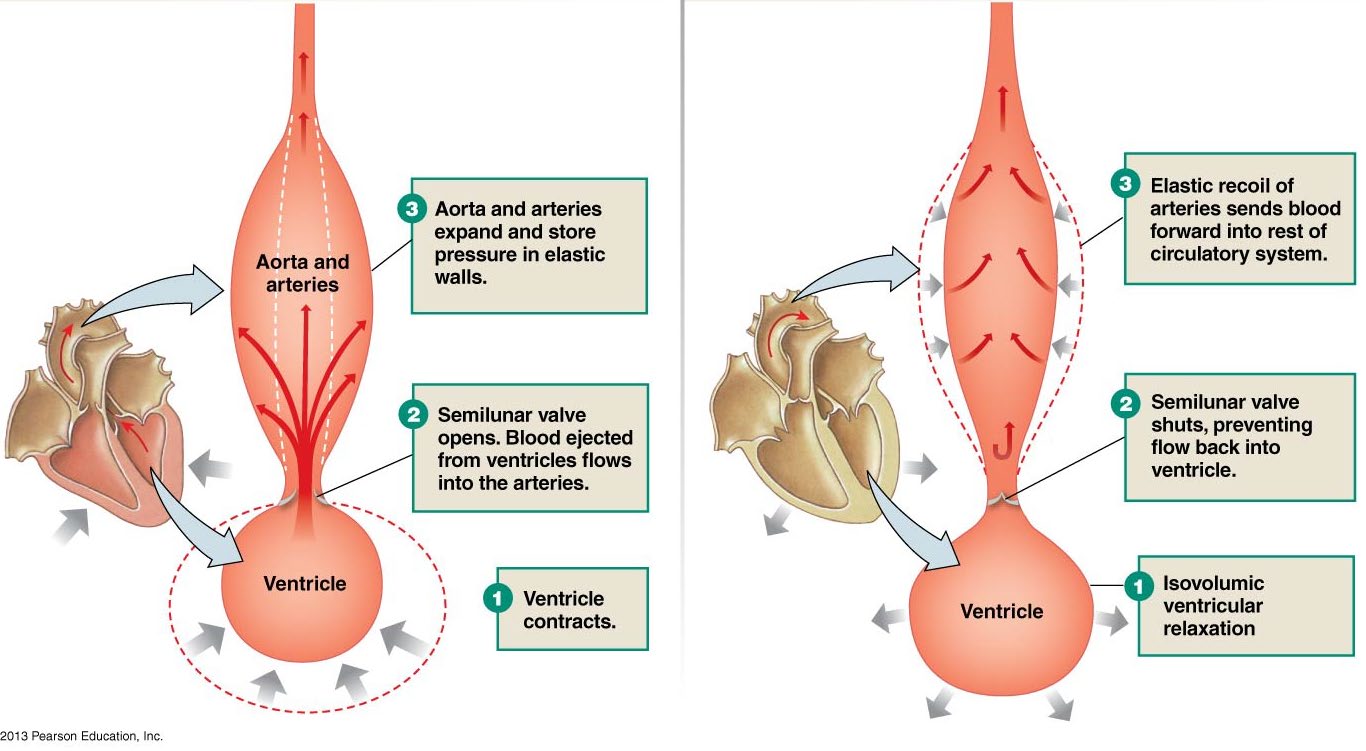
arteries act as pressure reservoirs
During ventricular contraction, blood enters and expands the arteries
As the ventricle relaxes, the elastic recoil of the arterial wall maintains pressure
Maintaining pressure in the arteries means that blood continues to flow through the circulation even as the ventricles are relaxing
Ventricular contraction on the left and ventricular relaxation on the right are shown in the image
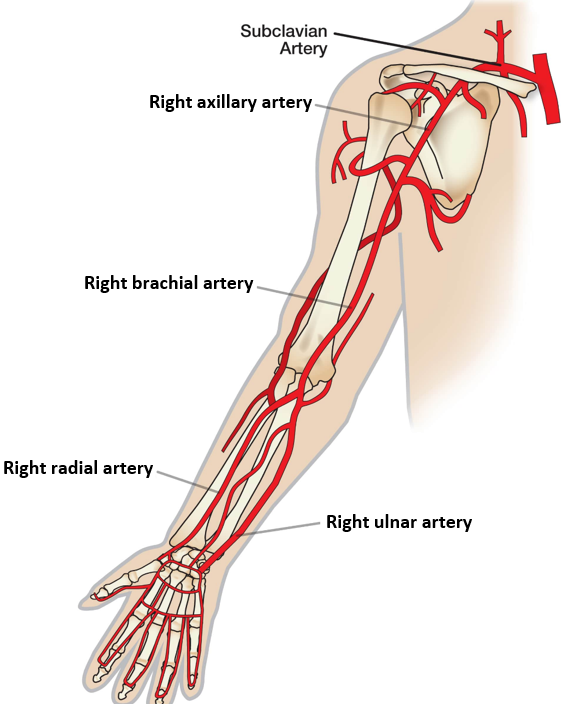
major arteries superior to the heart
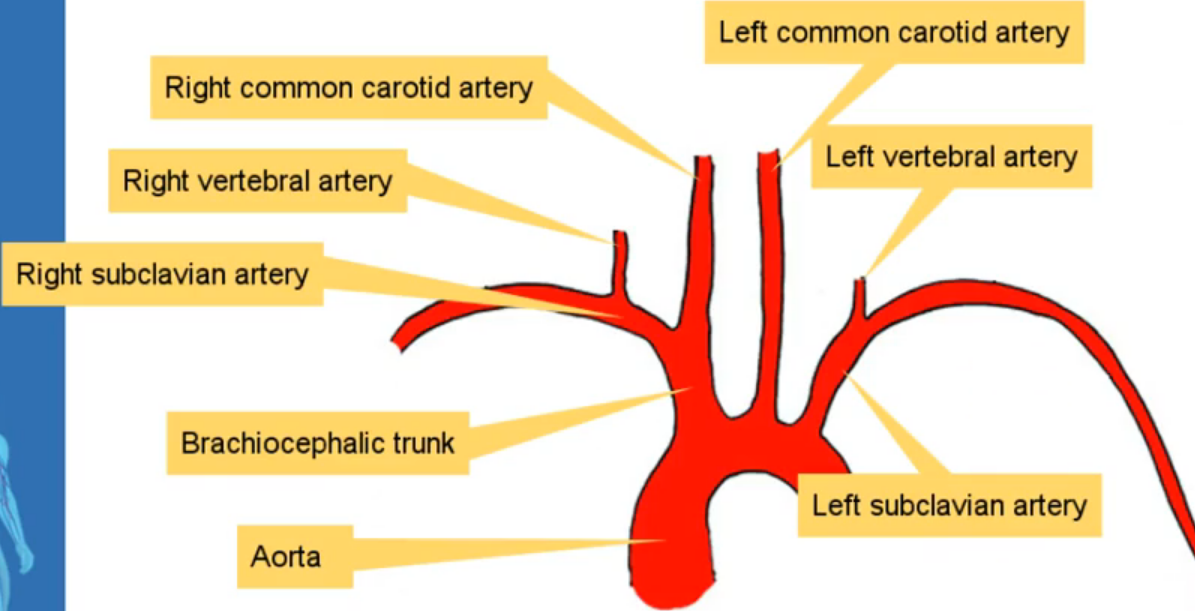
major arteries in the arm
arterioles
The arterioles are the smallest arteries in the body, and are responsible for regulating the flow of blood into the different tissues and organs of the body
The arteriole wall contains smooth muscle, and the contraction and relaxation of this smooth muscle will change the diameter of the arterioles, and therefore the amount of blood that can flow through those arterioles into a particular tissue
The arterioles are therefore critically important for changing how blood is distributed to different organs depending on changes in demand
Distribution of cardiac output
Cardiac output is not distributed equally to all tissues - some organs will receive more than others, and this can change depending on circumstances
Control of blood flow to individual organs can be altered by the NS and by local control mechanisms. This enables the body to alter local blood flow to meet metabolic demand
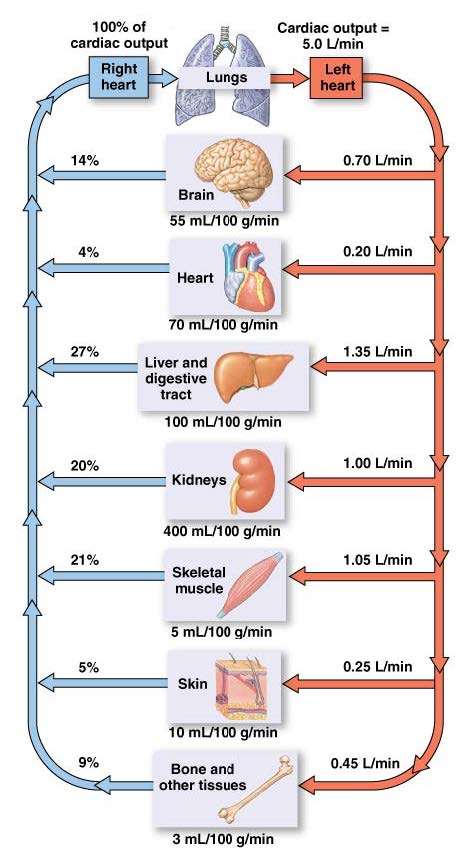
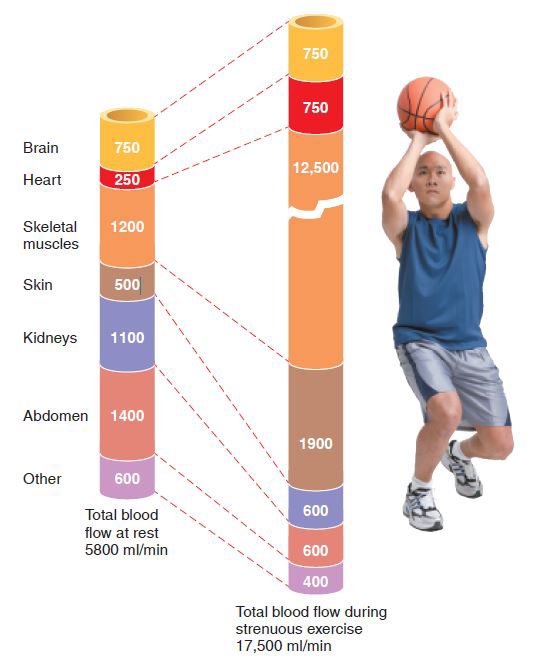
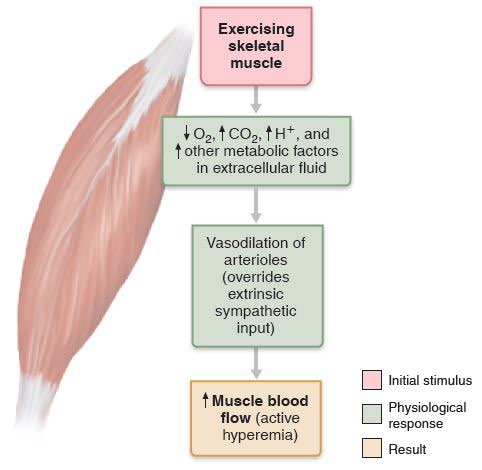
Distribution of cardiac output: exercise
During exercise, cardiac output is increased. The distribution of cardiac output to different organs is also altered during exercise
This ensures sufficient blood supply to the organs that need it
blood pressure
Blood pressure is the amount of force that blood exerts on the vessel wall and is measured in millimeters of mercury (mmHg)
In the circulatory system, blood pressure is highest in the arteries near the heart and lowest in the veins. It is these differences in blood pressure that cause blood to move or flow through the circulation
Blood will flow from an area of high pressure to an area of low pressure, following the pressure gradient
blood flow
Blood flow is the volume of blood that is flowing through a region each min, and is usually expressed in mL/min.
Arterioles play a role in regulating how much blood flows through different organs and tissues at any one time. They do this by altering the resistance to blood flow
resistance
The force that opposes blood flow. The higher the resistance in a blood vessel, the lower the blood flow through that vessel, and vice versa
Resistance in blood vessels is determined by vessel length, blood viscosity and vessel diameter
Vessel diameter is inversely proportional to resistance. This means that when the smooth muscle in the arteriole wall contracts, it causes vasoconstriction that reduces arteriole diameter and increases resistance to blood flow
However, when the smooth muscle in the arteriole wall relaxes, it causes vasodilation that increases arteriole diameter and decreases resistance to blood flow
The overall resistance to blood flow in the circulation will be determined by the resistance in many different blood vessels - peripheral resistance is used to describe the overall resistance to blood flow in the systemic circulation
local regulation in blood flow
Changes in arteriole diameter are one of the main mechanisms that regulate local blood flow or blood flow to different tissues and organs
This local regulation of blood flow is important for making sure that the amount of blood flowing to a particular tissue (or organ) matches the needs of that tissue at the time
For example, immediately after eating a meal, you need lots of blood flowing through the capillaries surrounding your gastrointestinal tract so that you can absorb the nutrients in the food you have just eaten
In contrast, when you are exercising, you need less blood flowing through your gastrointestinal tract, so the arterioles that supply these capillary beds will constrict to reduce blood flow through this area
This allows more blood to be re-directed to other areas of the body, such as the exercising skeletal muscles
Many factors can influence arteriole diameter, but two of the most important are the autonomic NS (primarily the sympathetic NS) and local mediators (e.g. that are produced by metabolically active tissue)
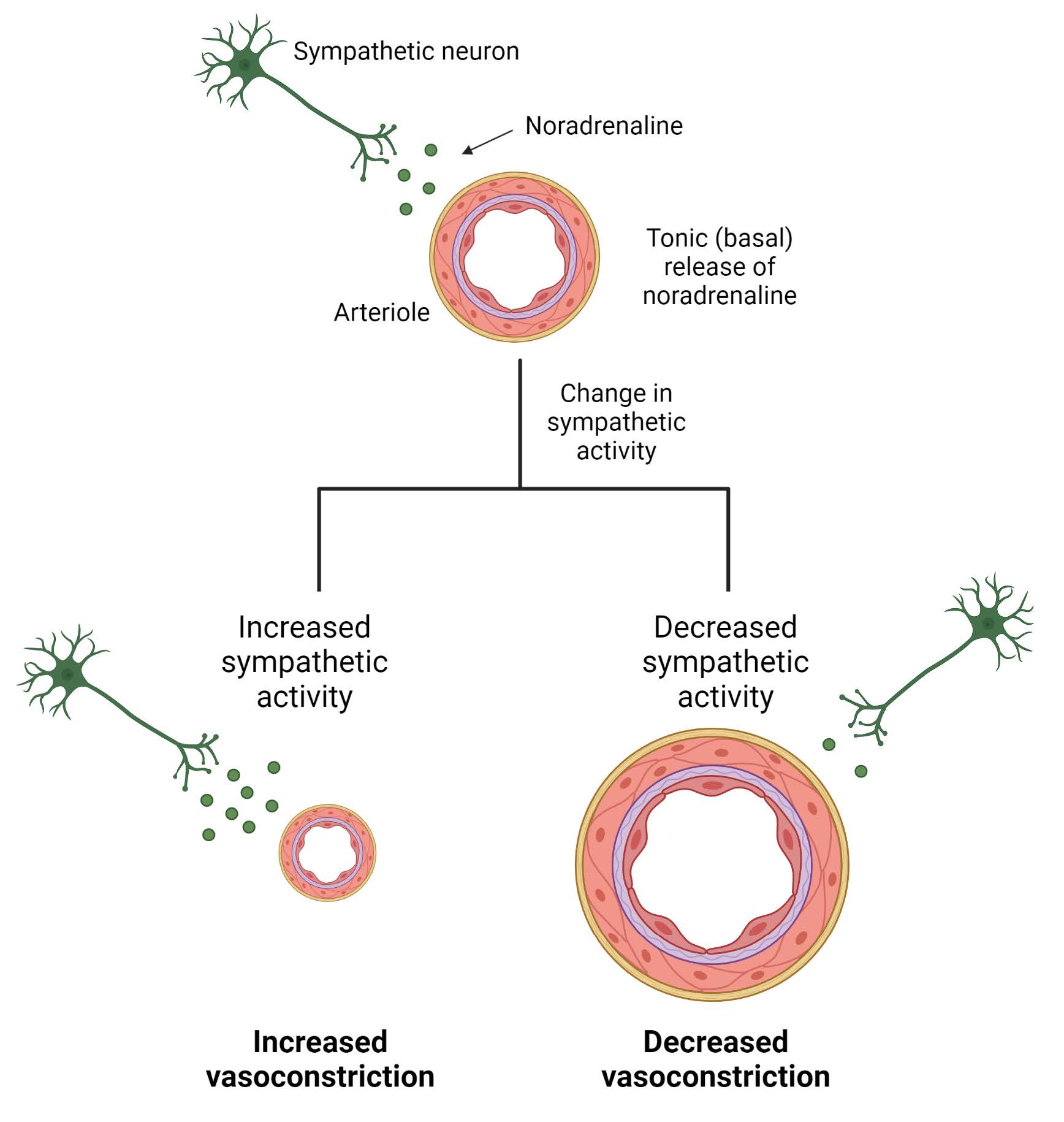
local regulation of blood flow - ANS
Most arterioles have sympathetic innervation. Activity of the SNS releases noradrenaline and causes vasoconstriction
Many arterioles have basal tone (partial contraction) that can be regulated by changes in NS activity, circulating mediators, etc
local regulation of blood flow - local mediators
Blood flow to tissues can also be regulated by locally produced mediators that alter arteriole diameter
Production of these mediators is often linked to metabolic activity of the tissue
Circulating hormones can also alter arteriole tone and local blood flow
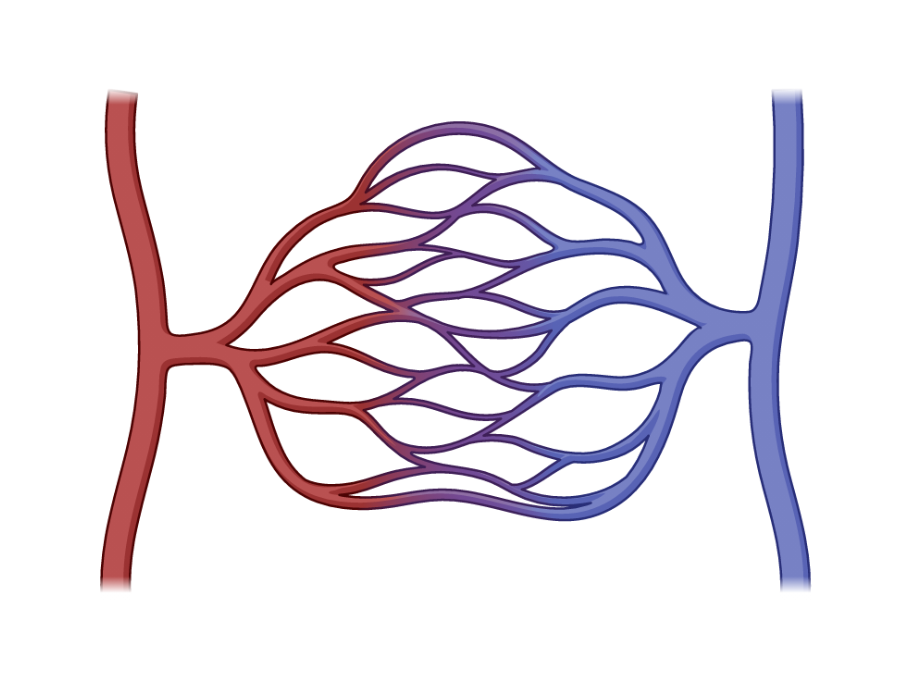
Capillaries
The smallest blood vessels in the body. Capillaries form branched networks known as capillary beds. As blood flows through the capillary bed, materials such as gases, nutrients, metabolites and waste products are exchanged between the blood and tissues
The capillary wall is made up of just a single squamous cell layer (the endothelium) together with a basement membrane, which makes the wall of capillaries very thin
As the wall is very thin, it means that exchanged materials don’t have far to travel between the blood and tissues, helping to make this an efficient process. This exchange process is also aided by gaps between endothelial cells that help to make the capillary permeable
Blood enters capillary beds from the arterioles and flows out of the capillary beds into the venules. The amount of blood that enters the capillary bed is regulated by the upstream arterioles
If the arterioles are dilated, then more blood will flow through the capillary bed, which allows the exchange of materials to occur. If the arteriole is constricted, then blood won’t flow through that capillary bed
location of capillaries
The number of capillaries found in different tissues (the capillary density) varies depending on the metabolic demand of a particular tissue
Tissues with high metabolic demand (e.g. brain, muscles, liver) will require more O2 and nutrients to function and therefore have more capillaries
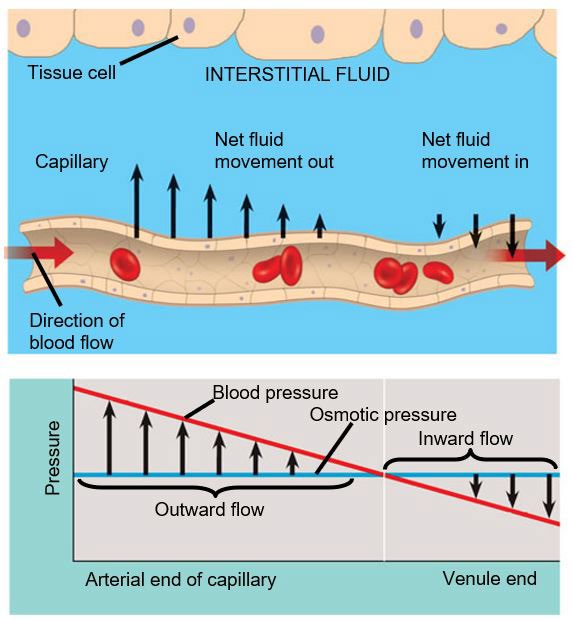
Fluid movement across the capillary wall
In addition to the movement of nutrients, metabolites and waste products, large amounts of fluid also move across the capillary wall in a process known as bulk flow
At the arterial end, fluid that is forced out of the capillary bed and into the interstitial fluid that lies in the space between vessels and tissues
Most of the fluid that is forced out of the capillaries at the arterial end then re-enters the capillary bed at the venous end
The movement of fluid across the capillary wall is driven by different pressures, in particular, capillary blood pressure and osmotic pressure
capillary exchange
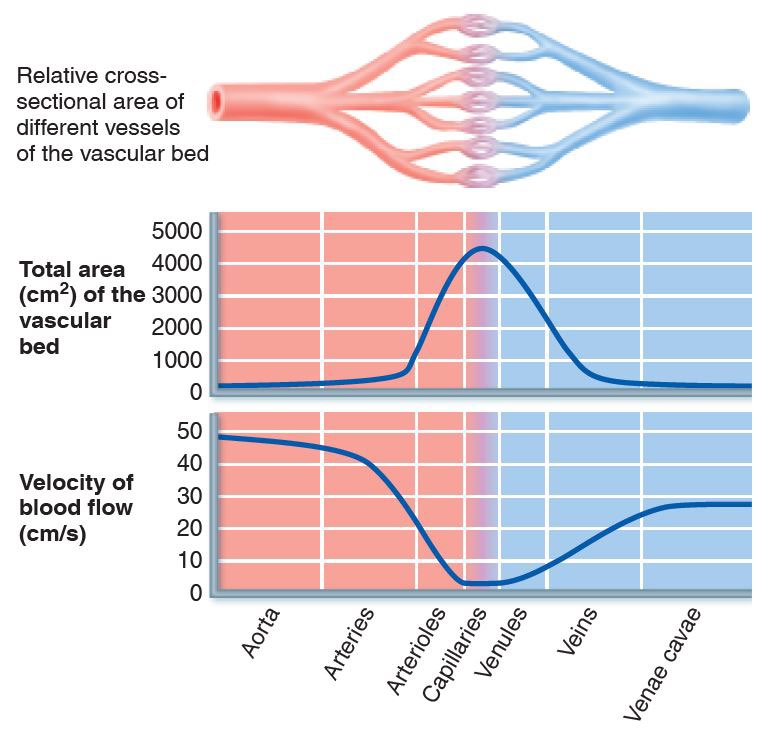
The velocity of blood flow through a vascular bed depends on its total cross-sectional area (CSA). High CSA = low velocity
Whilst the diameter of individual capillaries is very small, the large number of capillaries means that the total CSA is high and the velocity of blood flow through the capillaries is low
This slow velocity is important as it allows time for substance exchange to occur
Capillary bulk flow
Bulk flow is driven by hydrostatic and osmotic pressure gradients
Hydrostatic pressure is the pressure generated by blood within the vessel. Colloid osmotic pressure is the osmotic pressure generated by plasma proteins
Arterial end of capillary: hydrostatic pressure » osmotic pressure, driving fluid out of the capillary
As blood flows through the capillary bed, the hydrostatic pressure decreases whilst osmotic pressure remains relatively constant
Venous end of capillary, hydrostatic pressure « osmotic pressure, driving fluid back into the capillary
REVIEW- capillary bulk flow