MICR 2050 Ch. 19: Skin and Eye Diseases
1/130
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
131 Terms
anatomical features/defenses of the skin
- epidermis (keratinized surface)
- chemicals (oils and sweat)
- antimicrobials ( sebum and sweat)
- antimicrobial peptides in epithelial cells
normal biota of skin
Streptococcus, Staphylococcus, Corynebacterium, Propionibacterium, Pseudomonas, Lactobacillus; yeasts such as Candida
What does MRSA stand for?
Methicillin-Resistant Staphylococcus aureus
How is MRSA acquired?
direct contact: touching skin/wounds, bodily fluids
indirect contact: touching contaminated surfaces like hospital beds, gym equipment, toys, etc.
What can help prevent MRSA?
Good hygiene practices
What is the primary treatment for MRSA?
Vancomycin, MRSA is on the serious threat list for antibiotic resistance
MRSA distinguishing symptoms
Skin infections that may look like pimples or boils and can be red, swollen, painful, and full of pus

What causes impetigo?
Staphylococcus aureus and Streptococcus pyogenes (bacterial)
How is impetigo acquired?
direct: touching skin or sores
indirect: sharing contained objects like towels, washcloths, etc.
Impetigo distinguishing symptoms
itchy, oozing skin lesions with honey-like appearing crust that peels off

How is impetigo prevented?
good hygiene, don't touch infected people, antibiotics
What tests are used to confirm the presence of Staphylococcus aureus?
coagulase test: it will coagulate plasma
latex bead agglutination test (binds to IgG antibodies)
What are the virulence factors of Staphylococcus aureus?
exoenzymes: hylaronidase, coagulase, staphylokinase
exotoxins: toxic shock toxin, exfoliative toxin, hemolysin
protein A: IgG binding
What are the virulence factors of Staphylococcus pyogenes?
exoenzymes: hyaluronidase, streptokinase
exotoxins: superantigens, hemolysins
What is a furuncle?
a boil, abscess of a hair follicle

What causes furuncles?
Staphylococcus aureus (bacterial)
How are furuncles acquired?
direct contact with pus/skin, contact with contaminated surfaces
How are furuncles prevented?
good hygiene
What is a carbuncle?
cluster of boils

What causes carbuncles?
Staphylococcus aureus (bacterial)
How are carbuncles acquired?
direct contact with pus/skin, contact with contaminated surfaces
How are carbuncles prevented?
good hygiene
What is Erysipelas?
subcutaneous infection that causes inflammation over a large portion of the body
-skin will be warm to touch

What causes Erysipelas?
Streptococcus pyogenes (bacterial)
How is Erysipelas acquired?
small cuts, breaks in skin
How is Erysipelas prevented?
promptly sanitizing any cuts, scratches, or other wound
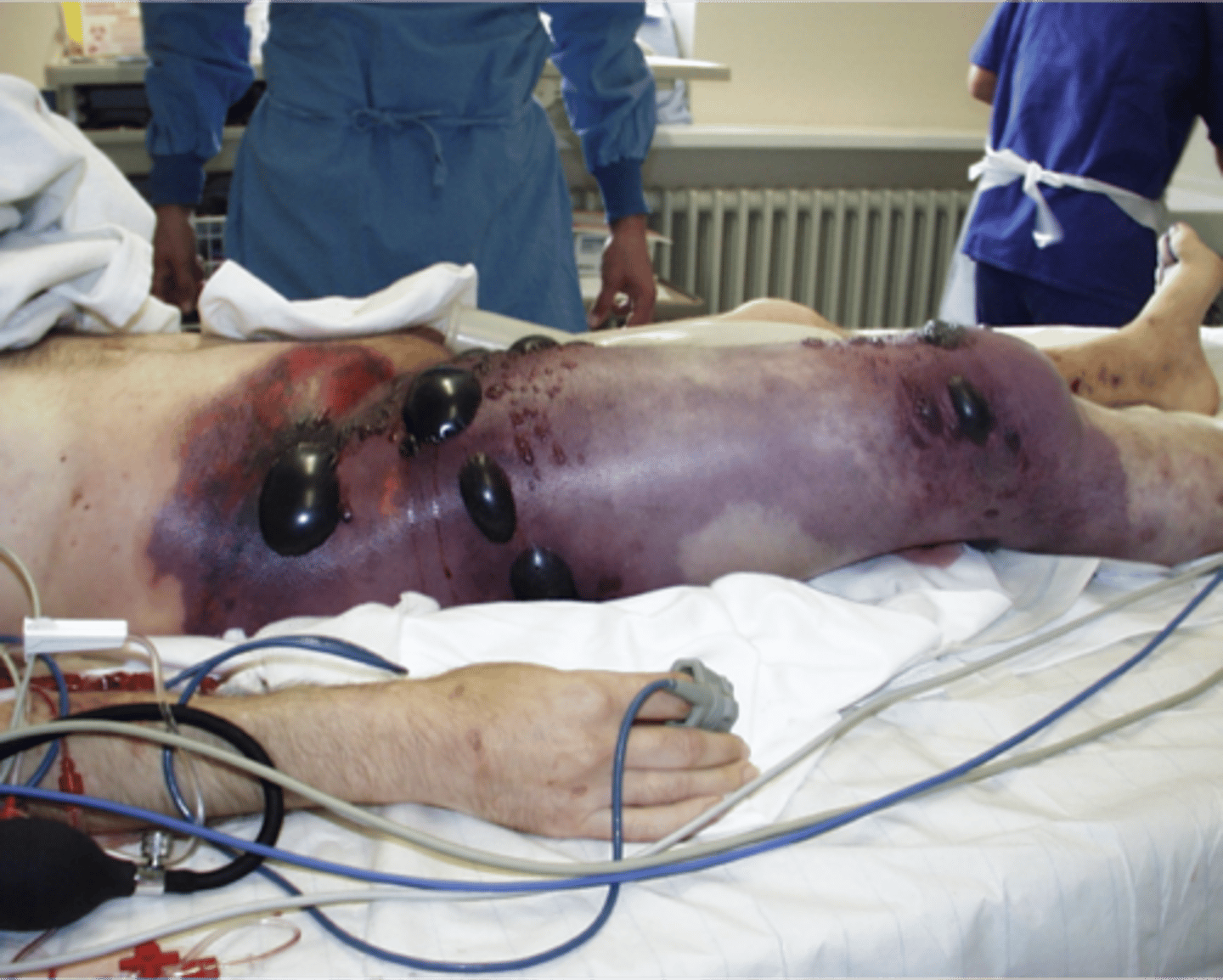
What is necrotizing fasciitis?
spreading infection of connective tissue

What causes necrotizing fasciitis?
Streptococcus pyogenes/Staphylococcus aureus (bacterial)
How is necrotizing fasciitis acquired?
breaks in skin, surgical/traumatic wounds
How is necrotizing fasciitis prevented?
good hygiene, avoid touching patients with bare skin
necrotizing fasciitis distinguishing symptoms
Extensive soft-tissue destruction
What is cellulitis?
acute, spreading infection in the dermis and subcutaneous tissues (lymphangitis often occurs)
What causes cellulitis?
Streptococcus pyogenes/Staphylococcus aureus (bacterial)
How is cellulitis acquired?
breaks in skin
What is Staphylococcal Scalded Skin Syndrome?
syndrome of acute exfoliation of skin , causing top layers of epidermis to slough off

What causes SSSS?
Staphylococcus aureus (bacterial)
How is SSSS acquired?
through direct contact or droplet contact
How is SSSS prevented?
by eliminating carriers in contact with newborns
SSSS distinguishing symptoms
split skin within epidermis that causes sloughing
What is gas gangrene?
infection of tissue that causes necrosis
What causes gas gangrene?
Clostridium perfringens (bacterial)
How is gas gangrene acquired?
through a vehicle (soil), endogenous transfer through the skin, GI tract, etc.
How is gas gangrene prevented?
proper cleaning of wounds
What is Pseudomonas aeruginosa?
opportunist pathogen of burn victims
What is Mycobacterium leprae?
Leprosy= Hansen's disease
Affects cooler (peripheral) body regions
Vesicular and Pustular Rash Diseases
- rash with lesions containing fluid
- chicken pox (varicella/zoster)
- smallpox
- HFMD
What is varicella?
superficial lesions in centripetal distribution, no prodromal fever

What causes varicella?
varicella zoster virus (viral)
How is varicella acquired?
through the respiratory tract
- incubates for 10-20 days, rash resolves in 2-3 weeks
How is varicella prevented?
live- attenuated vaccine
What is zoster?
reactivation of varicella that was latent in spinal ganglia

What causes zoster?
varicella-zoster virus (viral)
How is zoster acquired?
recurring from chickenpox
How is zoster prevented?
Some immunization from varicella as a child
Once to age 50 vaccination is recommended to boost immune system
What is smallpox?
deep rash all over body, fever precedes rash, 50% fatality
- Category A bioterrorism agent

What causes smallpox?
Variola virus
How is smallpox acquired?
through droplet contact or indirect contact
How is smallpox prevented?
live virus vaccine
What is Hand, Foot, Mouth disease?
lesions in mouth with fever, common in children

What causes HFMD?
coxsackie virus (enterovirus)
How is HFMD acquired?
secretions: saliva, sputum, blister fluid, feces
How is HFMD prevented?
hand hygiene
Maculopapular Rash Diseases
measles, rubella, fifth disease, roseola, scarlet fever
What is measles (rubeola)?
Very contagious virus, report cases to CDC, Maculopapular rash on head that spreads to whole body

What causes measles?
Rubeola virus (viral)
How are measles acquired?
droplet contact
How are measles prevented?
live-attenuated vaccine (MMR/MMRV)
What is a complication of measles in young people?
subacute sclerosis panenchephilitis
What is rubella?
Relatively minor rash disease with few complications
- tetrogenic, if acquired congenitally, can cause birth defects

What causes rubella?
Rubella virus (viral)
How is rubella acquired?
respiratory droplets
-postnatal or congenital infection possible
How is rubella prevented?
MMR vaccine
What is a complication of rubella in young people?
dangerous for unborn children, can cause birth defects
What is Fifth Disease?
"slapped face" rash that spreads to limbs and trunk, tends to be confluent rather than distinct bumps
What causes Fifth disease?
Parovirus B19 (viral)
How is Fifth disease acquired?
through droplet contact or direct contact
How is Fifth disease prevented?
Frequent handwashing [no vaccine or medicine yet]
What is Roseola?
high fever that can produce rash, common in young children and babies
What causes Roseola?
human herpes virus 6 (viral)
How is Roseola acquired?
unknown
How is Roseola prevented?
unknown, it is thought that 100% of US population is exposed at some point
Wart and Wart-like Eruption Diseases
warts and molluscum contagiosum
What are warts?
A contagious infection of the epidermal layer of the skin

What causes warts?
HPV (viral)
How are warts acquired?
direct contact, auto inoculation, indirect contact
How are warts prevented?
avoid contact
What is molluscum contagiosum?
smooth, waxy nodules on the face, trunk and limbs
- can be disfiguring to immunocompromised

What causes molluscum contagiosum?
molluscum contagiosum virus (viral)
How is molluscum contagiosum acquired?
direct contact (including sexual), auto inoculation
How is molluscum contagiosum prevented?
avoid contact
Large Pustular Skin Lesions
Leishmaniasis and cutaneous anthrax (lesions greater than a few millimeters)
What is Leishmaniasis?
Protozoan disease carried by sand flies, volcano like edges with central crater
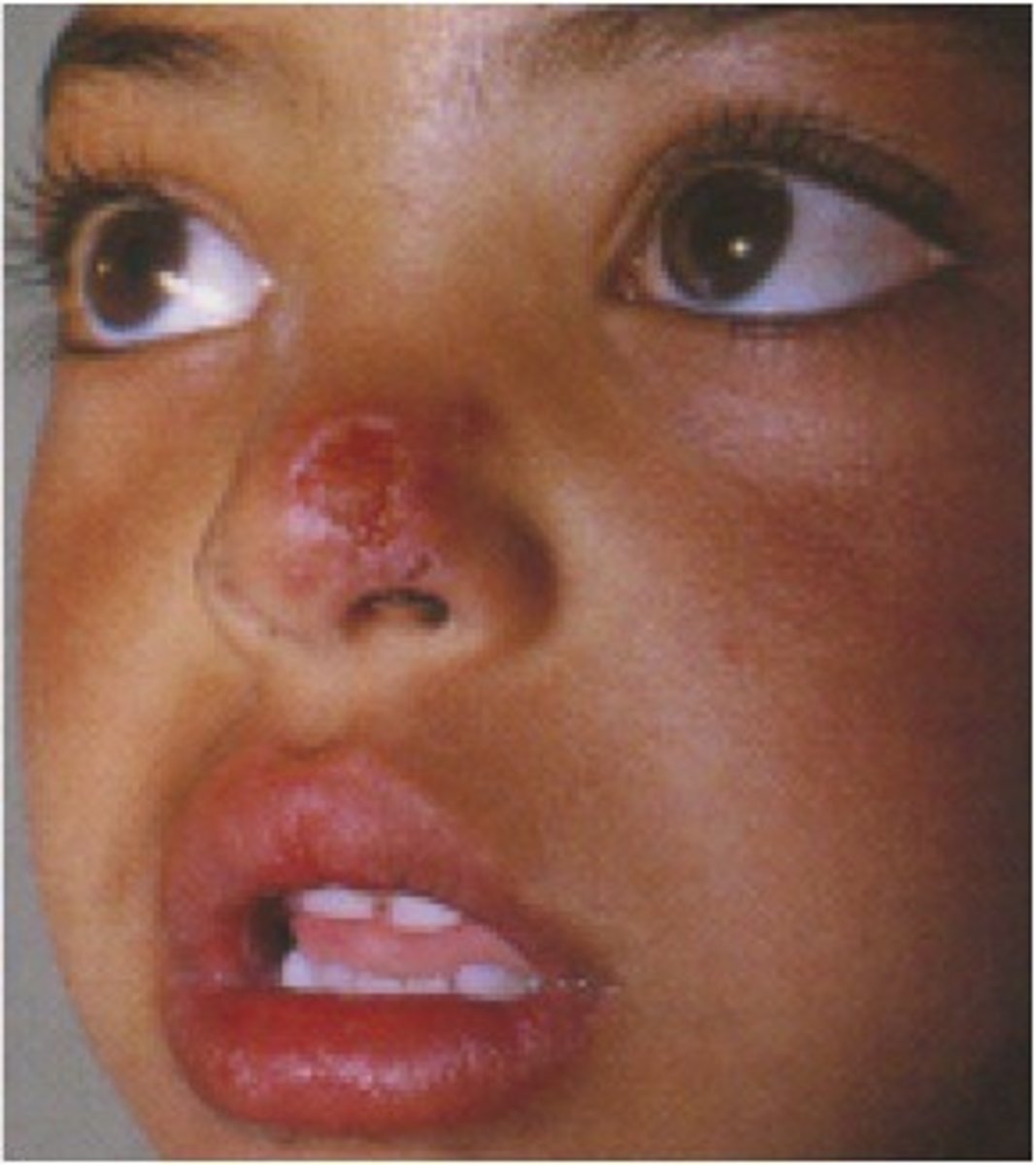
What causes Leishmaniasis?
Leishmania species (protozoan)
How is Leishmaniasis acquired?
sand fly bites
How is Leishmaniasis prevented?
avoid sand fly (vector)
What is Cutaneous Anthrax?
Painless black necrotic lesion
- least dangerous type of anthrax
- papule that grows into necrotic eschar
- category a bioterrorism agent
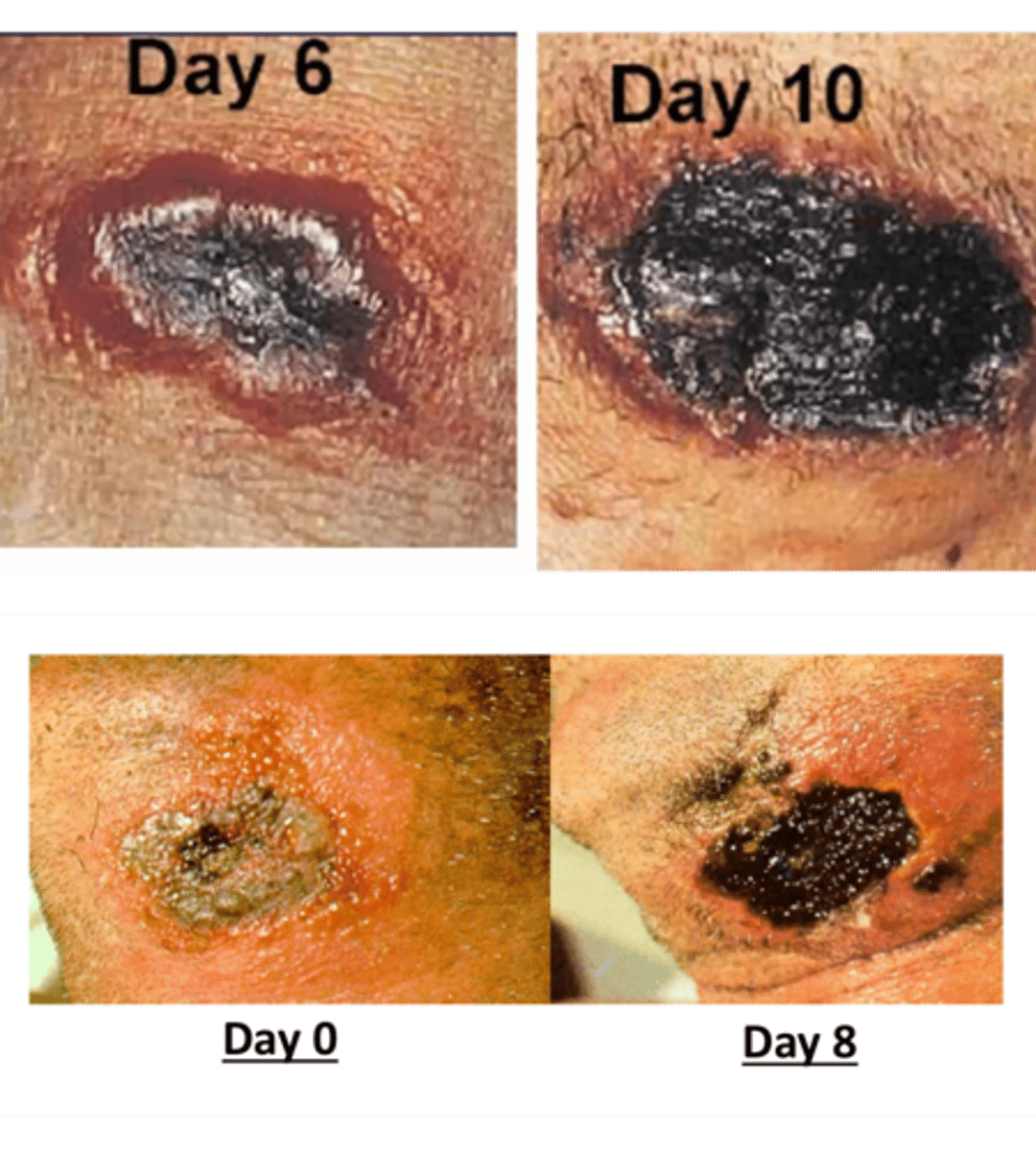
What causes Cutaneous Anthrax?
Bacillus anthracis (bacterial)
How is Cutaneous Anthrax acquired?
Through skin cuts, abrasions, or insect bites contaminated with anthrax spores
How is Cutaneous Anthrax prevented?
vaccine, avoid contact
Fungal Infections
cutaneous (ringworm) and superficial mycoses