GI Lecture 3: Digestion and Absorption
1/100
Earn XP
Description and Tags
Digestion of Carbs, Fat, Proteins in the Small Intestine
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
101 Terms
The major site of digestion and absorption
Small Intestine
Intestinal epithelial cell loss is high, but cell turnover is rapid (replaced 3-6 days) due to stem cells located in
Villus Crypts
Stem cells produce new enterocytes and mucus secreting Goblet Cells
What is the Digestion of Carbs and what are the 3 major sources:
Enzymes return hydrogen and hydroxyl ions from water to polysaccharides separating the monosaccharides from one another
3 Major sources:
1) Sucrose: disaccharide
2) Lactose: disaccharide
3) Starch: polysaccharide
Examples of Starches
-Amylopectin (branched glucose)
-Amylose (unbranched glucose)
-Plants (Potatoes and Grains)
Examples of Glycogen
Animal Tissues (branched glucose) - small amounts
Examples of Disaccharides
-Sucrose (Glucose-Fructose)
-Lactose (Glucose-Galactose)
-Maltose (Glucose-Glucose)
Examples of Monosaccharides
-Glucose
-Fructose
Fiber is not digested by human cells, what linkage is broken down by bacteria
Glucose beta-1,4
Ingested starches, glycogen & disaccharides must be hydrolyzed to monosaccharides in order to be absorbed by enterocytes. Digestion occurs in 2 phases:
-Luminal
-Membrane
Luminal Phase of Digestion
-Begins in the mouth & stomach through the actions of salivary alpha-amylase
-However, digestion mainly occurs in the small intestine via pancreatic alpha-amylase action
Final products of alpha-amylase action are small oligosaccharides and disaccharides
Does alpha-amylase digestion produce any absorbable monosaccharides?
No
-The end-products of alpha-amylase digestion remain undigested because alpha-amylase can only hydrolyze INTERIOR alpha-1,4 linkages
-Most end products possess either terminal alpha-1,4 linkages or branch point alpha-1,6 linkages
Membrane phase of digestion
The products of Luminal Digestion are further hydrolyzed to absorbable Monosaccharides by digestive enzymes located on the mucosal brush border membrane.
Membrane enzymes are mostly what?
Disaccharidases: cleave one or more alpha-amylase digestion product (alpha-Dextrins, Maltotroiose, Maltose) or ingested disaccharides (e.g. Sucrose, Lactose, Trehalose)
Alpha-amylase requires what pH to retain activity
Requires a near neutral pH (optimal 6.7) to retain activity
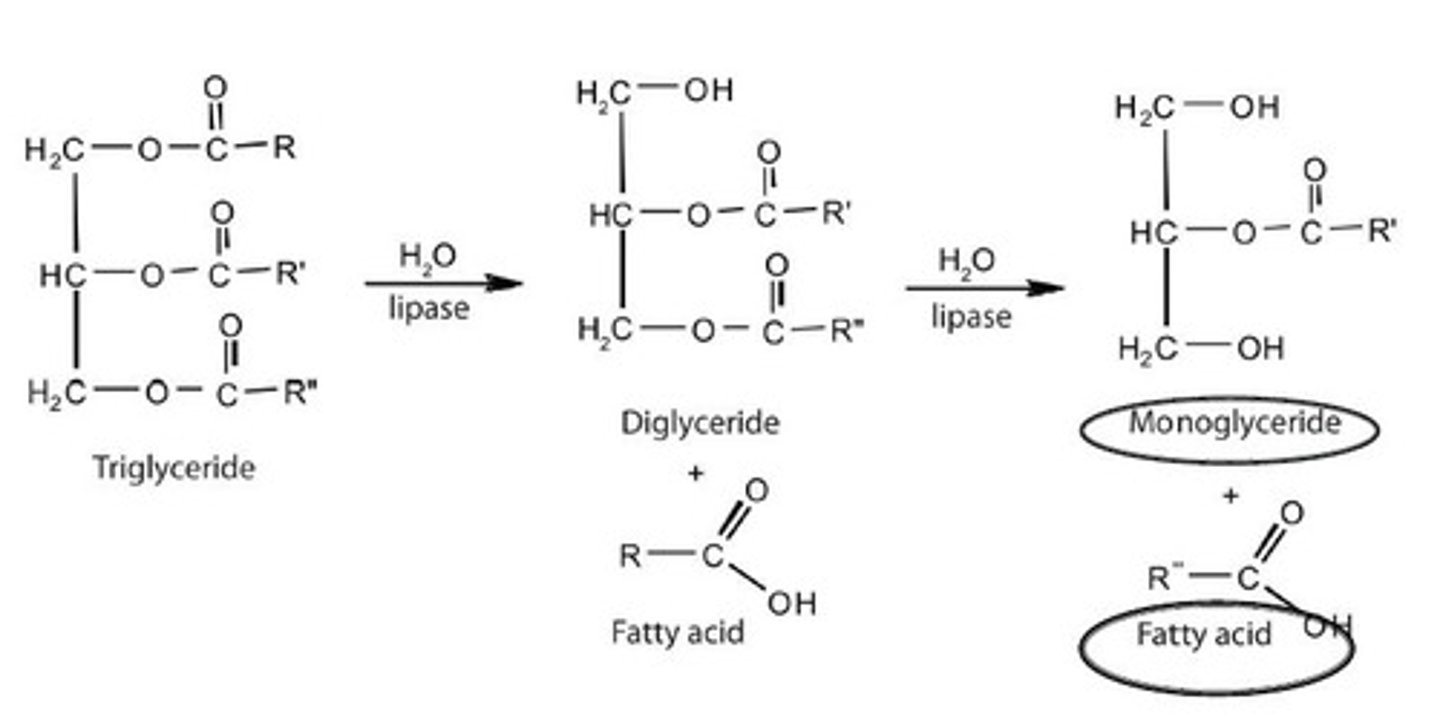
Digestion of Fat (TG)
The fat digesting enzymes return 3 molecules of water to the TG molecule splitting the fatty acid molecule away from the glycerol
Substrate: Fat
Mechanism: Bile and Agitation
End product: ?
Emulsified Fat
Substrate: Emulsified Fat
Mechanism: Pancreatic Lipase
End product: ?
Monoglyceride and Free Fatty Acid
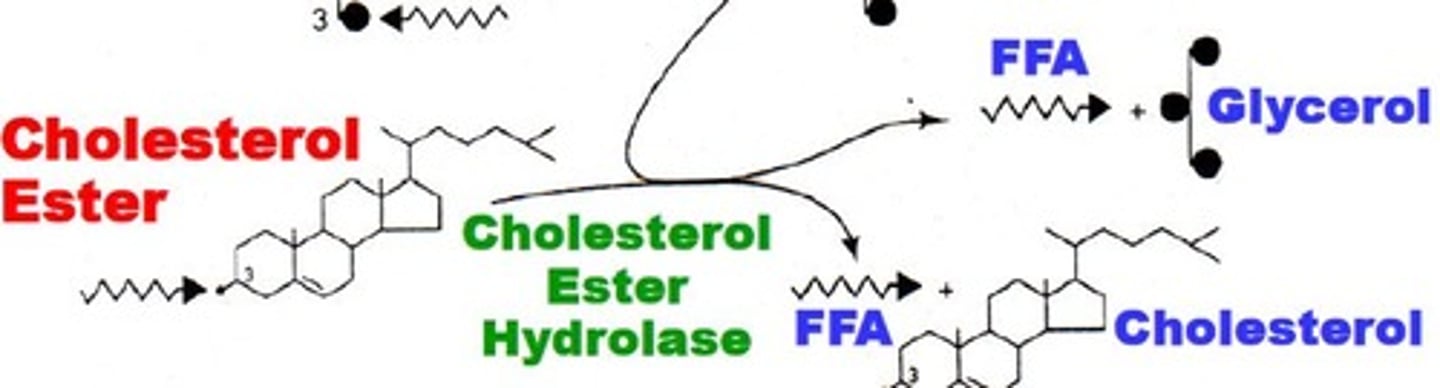
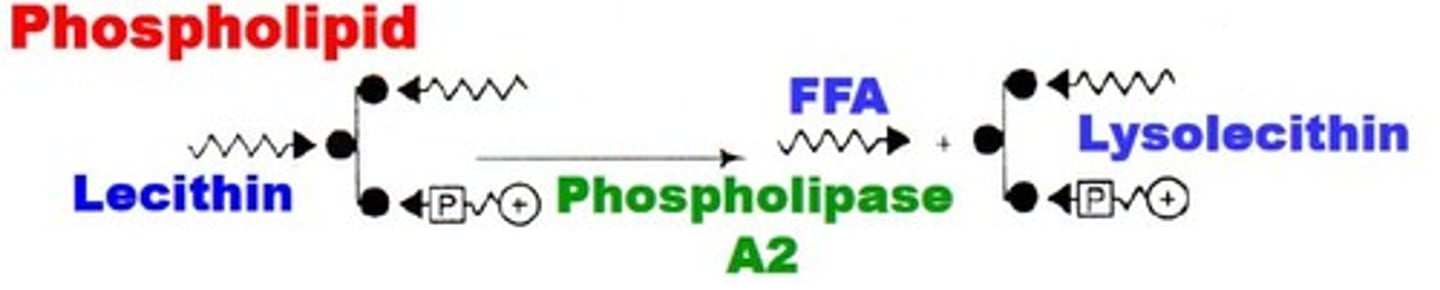
Substrate: Cholesterol esters and Phospholipids
Mechanism: Cholesterol ester hydrolase, Phospholipase A2
End product: ?
Monoglyceride and Free Fatty Acid
Essential Metabolic Functions of the Liver
-Carbohydrate metabolism
-Protein metabolism
-Lipid metabolism
-Drug and Hormone metabolism
-Bile production/secretion
-Digestion/Absorption of Lipid from GI tract
-Bilirubin elimination
-Accumulation = Toxic (Jaundice)
What is the pathway for Bile?
Produced and excreted by Liver → stored and concentrated in the Gallbladder → released into the Duodenum in response to a meal
What are Liver Lobules
-Basic functional units of the liver
-A peripherally located system of blood vessels (portal vein and hepatic artery)
-Secretory Bile Duct branches
-”Plates” of hepatocytes (liver cells)
Ggroups of lobules are organized around a _____
Central Hepatic Venule
What are Sinusoids?
Blood vessels and ducts extend branches between and within the plates of hepatocytes, distributing blood to hepatocytes
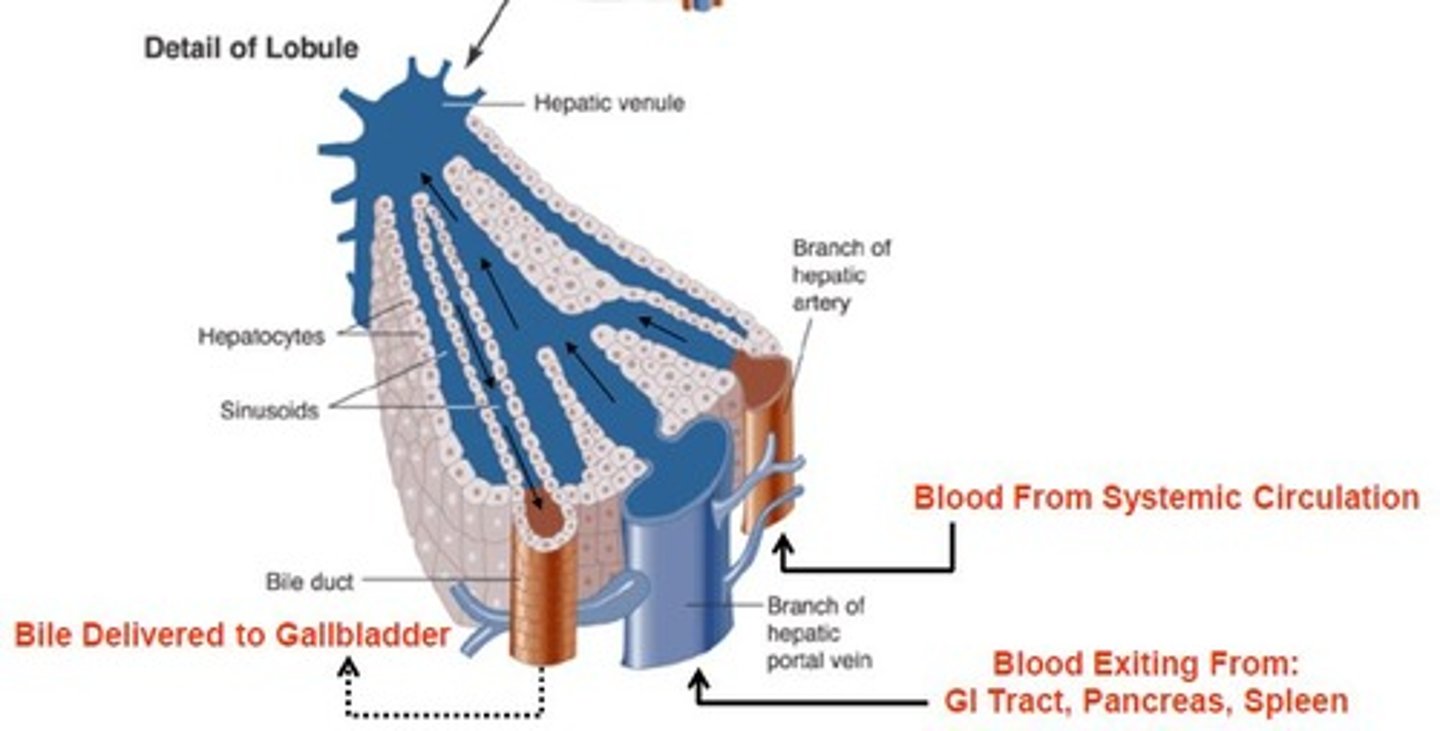
What is the Bile Canaliculi?
Other types of sinusoids located between adjacent rows of hepatocytes, acting as a conduit to deliver bile secreted from hepatocytes
Bile functions: Lipid Digestion
Responsible for fat emulsification (like detergent action), which allows digestion by pancreatic lipase. Dietary fat is INSOLUBLE in the aqueous GI fluids
Bile functions: Lipid Absorption
Solubilizes fat digestion products (e.g. monoglycerides & fatty acids) into Micelles, which is important for fat absorption
Bile function: Waste Elimination
Cholesterol and Bile Pigments (Bilirubin) as well as some drugs and heavy metals are eliminated
Composition of Bile
-Bile salts (conjugated bile acids)
-Phospholipids
-Cholesterol
-Bile Pigments
Combined with an alkaline isotonic fluid secreted from Bile Duct epithelial cells
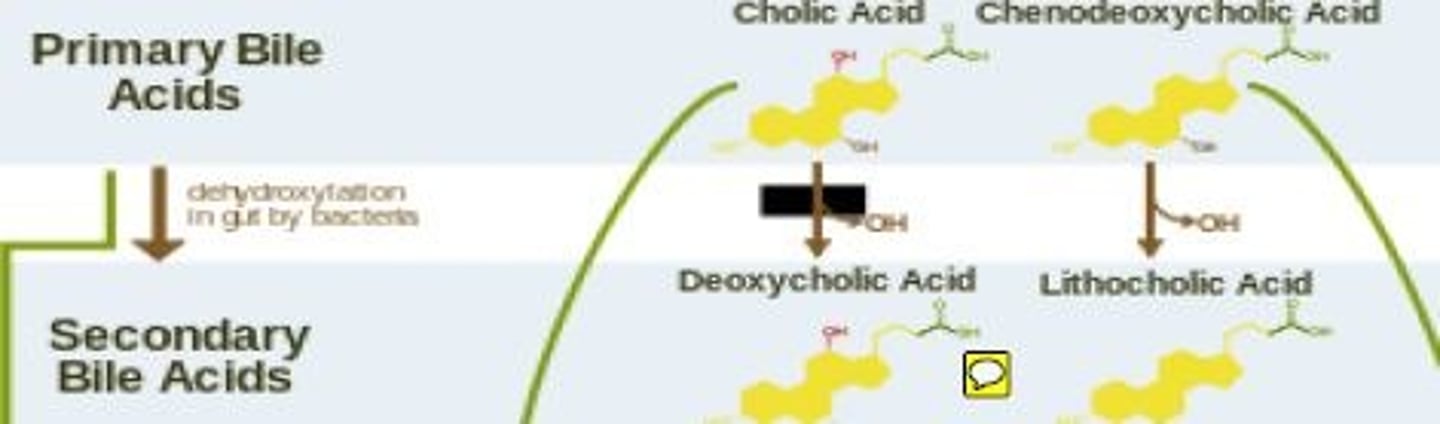
Bile Acid Function in Bile
-50% of the organic component of bile
-Emulsify lipid material in the intestine through Micelle formation
-Primary Bile Acids synthesized in the liver from cholesterol and secreted into the Duodenum
-A fraction of primary bile acids is converted to secondary bile acids by ileal bacteria
Bile Salt function in Bile
-Amino Acid Conjugation and Ionization convert Bile Acids into more water-soluble Bile Salts (actual participants in micelle formation)
-Amphipathic
Role of Phospholipids in Bile
-30-40% of organic bile
-Lecithins (also amphipathic)
-Interact with bile salts to support micelle formation
Role of Cholesterol in Bile
-4% functions to support micelle formation
-Bile is the only route of excretion for cholesterol
-Regulates body stores of cholesterol
Role of Bile Pigments in Bile
-2% do NOT contribute to lipid emulsification or micelle formation
-Secretion of the bile pigment Bilirubin (Hb breakdown)
-Serves as a route for its excretion factors in feces. Main cause of characteristic brown fecal coloration
Bile Secretion
-Produced continuously by liver hepatocytes
-After secretion, addition water, H3CO-, and other electrolytes are secreted by the Bile Duct, regulated by Secretin
Functions of the Gall Bladder
-serves as bile storage site, between meals
-releases bile in response to meal
-CONCENTRATES the fluid by reabsorbing water and electrolytes until release is stimulated
Bile Expulsion: Where does stored bile release?
Released into the Duodenum when the gall bladder is stimulated to contract (in response to a meal)
What are the 2 major stimulants of gall bladder contraction during excretory phase
-Cholinergic Vagal Stimulation (ACh)
-Cholecystokinin (CCK)
Most (95%) bile acids released into the intestine are reabsorbed mainly where and through what processes?
By the ILEUM through passive and active processes
Reabsorbed bile acids are returned to liver via what?
The Portal Blood (Enterohepatic circulation), where they are extracted from the blood by hepatocytes.
A small fraction (5%) of bile acids are lost in where? And how is it replaced?
Lost in Feces. It is replaced through hepatic synthesis of new bile acids
The TOTAL bile acid pool in humans is only _____. However, between _____ of bile acids typically enters the Duodenum
How is this discrepancy compensated for?
2.5 g; 15-30 g/day
This discrepancy is compensated for by the fact that most of the bile acid pool is reabsorbed through the Enterohepatic Recirculation (2-2.5 g) through the billary system between 5-15 x/day
Because of bile acid recirculation, only a small amount of new bile is to be synthesized by hepatocytes to replace amounts lost in the feces: how much is that?
0.75-1.5 g/day
The liver can maximally synthesize how much new bile acids daily?
3-5 g/day
In impairment of bile acid recirculation: complications are related to:
-Excess H2O and electrolyte loss (Osmotic Diarrhea)
-Bile salt excretion and/or impaired fat digestion (Steatorrhea)
In impairment of bile acid recirculation: Clinical manifestations are related to the severity of impaired bile acid circulation. If synthesis of new bile acids by the liver keeps pace with fecal loss, what happens to fat digestion? What are the clinical manifestations?
-Fat digestion remains normal
-Clinical manifestations are primarily H2O and Electrolyte loss, but NO Fat loss in stool (Osmotic Diarrhea)
Mild to Moderate Impairment of bile and acid recirculation (e.g. infection/inflammation)
-Causes excess bile acids to each the colon
-This inhibits colon absorption of electrolytes and H2O due to the osmotic effect of unabsorbed bile acids
Severe Impairment of bile and acid recirculation (e.g. Ileal Resection)
-Outpaces new bile acid synthesis
-Results in impaired digestions of long chain TG
-Results in H2O and Electrolyte Loss AND the Undigested Fat Loss in stool (Steatorrhea)
Treatment for Steatorrhea
-Substituting MEDIUM-chain TGs for LONG-chain TGs in the diet.
-Small TGs do not require micelle formation for absorption
Gallbladder FIlling
Bile is produced continuously by hepatocytes and flows into the gallbladder (via bile ducts)
Sphincter of Oddi
Facilitates by its high tone, bile diversion into the gall bladder between meals by preventing immediate passage into the duodenum
Bile Concentration
-The volume capacity of the human gallbladder is limited to 20-60 mL
-The total volume of bile secreted from hepatocytes may be many time this amount
-Bile that is initially secreted from hepatocytes (Liver) greatly increases in volume due to the addiction of electrolytes (mainly HCO3-) and H2O from bile duct cells
-This discrepancy is accounted for by the gallbladder’s ability to Concentrate Bile 20-Fold
How does the gallbladder concentrate bile
By actively reabsorbing Na+, Cl-, & HCO3-. Water follows passively down the osmotic gradient created by electrolyte movement
The 2 major effects of bile concentration by the gall bladder
1) A large DECREASE in fluid volume (H20 loss)
2) A large INCREASE in the concentration of organic constituents (Bile Salts, Cholesterol, Bilirubin). Effects on electrolyte concentration vary
Critical Micellar Concentration
-Where Micelle formation only occurs when Bile Acids reach a certain concentration
-Only at these high Bile Acid concentrations will bile salts aggregate to form micelles
Why does gallbladder removal sometimes results in impaired dietary fat digestion
Because you can not attain Critical Micellar Concentration to allow for micelle formation
Bile expulsion is a typically initiated within how long after eating a meal?
30 minutes
Bile is primarily expelled from the gallbladder into the duodenum in response to the presence of what in the GI tract?
Fat digestion products (Duodenal Lipids) in the GI tract
Fat Digestion in Oral Cavity: Lingual Lipase
-Is secreted into Saliva and initiates fat digestion
-Due to limited exposure time, actions are non-essential for complete fat digestion
Fat Digestion in Stomach: Gastric Lipase
-Is secreted from the fundus and has similar actions to pancreatic lipase
-Accounts for only 10% of dietary fat (TG) digestion
-Considered non-essential because of the normally excessive secretion of pancreatic lipase
Zollinger-Ellison Syndrome
High gastric acid output condition that can cause pancreatic lipase inactivation
Gastric contribution can be important in this case
Why is indirect action in stomach important for lipid digestion?
The mechanical breakdown and mixing of lipid compounds increases surface area for breakdown by lipase and assists in emulsification of hydrophobic fats
Fat Digestion in Duodenum (90% of enzymatic fat digestion): Pancreatic Lipase
-Digests TG into Fatty acids and 2-MG
-Activity depends on Colipase, which is also secreted from the pancreas
Function of Colipase
-Acts as a lipid-water interface of fat droplets to hydrolyze emulsified TG
Pancreatic Insufficiency
Lipase Deficiency
H+ Hypersecretion
Lipase Inactivation
Triglycerides (TG)
-Major components of dietary fat
-Comprised of 3 Fatty acids esterified to glycerol
Cholesterol Esters
-Consists of cholesterol esterified to a fatty acid
Cholesterol Ester Hydrolase
-Hydrolyzes esters to Cholesterol and FFAs
Completes TG breakdown by hydrolyzing 2-MG to Glycerol & FFA
Phospholipids (e.g. Lecithin)
-Comprised of glycerol esterified to 2 FAs and either choline (phosphatidylcholine) or inositol (phosphatidylinositol)
Phospholipase A2
Releases FFAs to yield lysophospholipids (Lysolecithin)
Relative intestinal bacterial population:
-Duodenum
-Jejunum
-Ileum
-Colon
-Duodenum: few if any
-Jejunum: few if any
-Ileum: few
-Colon: large numbers
Site: Stomach
Enzyme: ?
Substrate: Only initiates Collagen and Proteins
Product: ?
Enzyme: Pepsin
Product: Proteose, peptones, and polypeptides
Site: Upper Small Intestine
Enzyme: ?
Substrate: Act on Protease, Peptones and Polypeptides
Product: ?
Enzyme: Pancreatic Enzymes (trypsin, chymotrypsin, carboxypeptidase, proelastase)
Product: Polypeptides and Amino Acids
Site: Brush Border Enterocytes
Enzyme: ?
Substrate: Polypeptides and Amino Acids
Product: ?
Enzyme: Peptidases
Product: Amino Acids
The GI tract of an individual consuming a typical American diet must process how much protein a day
90-170 gm protein per day
Most protein comes from dietary protein. What percentage constitutes daily adult Caloric Intake?
10-20%
In addition to dietary protein, the GI tract must digest and additional 10-30 gm protein from:
-Gastrointestinal Secretions (Pancreatic, Biliary, and Intestinal)
-Exfoliated Intestinal Cells generated from the constant and rapid mucosal cell turnover of the GI tract
In humans, essentially _____ protein is digested and absorbed by intestinal mucosa
ALL
Typically before it has traversed jejunum
Fecal protein is mostly from
Bacteria and exfoliated epithelial cells from the distal tract
What are the 3 protein digestion sites
1) Luminal digestion
2) Membrane digestion
3) Cytoplasmic digestion
Luminal Digestion
-Dietary Protein digestion beings in the stomach through the actions of Gastric Acid and Pepsin
-Occurs mainly through actions of Pancreatic Peptidases secreted into the small intestine
-End products are predominantly absorbable Free Amino Acids and small Di-/Tri-Peptides, which are transported across the brush border
Membrane Digestion
-Small amounts of Larger Peptides (4-8 amino acids) remain after luminal digestion that are Non-Absorbable and must be further digested
-Brush Border Peptidases are located at apical membrane of enterocytes and serve to further digest Larger Peptides into Free Amino Acids & Di-/Tri-Peptides
Cytoplasmic Digestion
-Very minor amounts of un-absorbable larger peptides remain after membrane digestion. Products are then rapidly absorbed across membrane into enterocyte
-Intracellular Cytoplasmic Peptidases complete the protein digestion process by further hydrolyzing absorbed Di-/Tri-Peptides into Amino Acids
The end products of Cytoplasmic Digestion are mostly what?
-Free Amino Acids (75%), which leave the cell and enter the blood across the basolateral membrane
In luminal digestion, proteolytic enzymes are produced by what cells? What enzyme types are these?
Pancreatic Acinar Cells (Enzymatic Component)
-Endopeptidases (i.e. hydrolyze only Interior peptide bonds)
-Exopeptidases (i.e. remove one amino acid at a time from Exterior C-terminals)
Example of Endopeptidases and their end products
-Gastric Pepsin
-Pancreatic proteases (Trypsin(s), Chymotrypsin, and Elastase(s))
The end-products of endopeptidase digestion are Mostly Small Peptides
Example of Exopeptidases and their end products
-Carboxypeptidase A, Carboxypeptidase B
End-products are Mainly Amino Acids and some incompletely digested peptides
Primary cleavage site for pepsin and chymotrypsin
INTERIOR peptide bonds of aromatic AAs
Primary cleavage site for trypsin’s 1-3
INTERIOR peptide bonds of basic AAs
Primary cleavage site for elastase 1 and 2
INTERIOR peptide bonds of neutral AAs
Primary cleavage site for Carboxypeptidase A
EXTERIOR peptide bonds of aromatic and neutral AAs
Primary cleavage site for Carboxypeptidase B
EXTERIOR peptide bonds of basic AAs
In Luminal Digestion, Pancreatic Proteases are initially secreted
As Inactive Peptidases
How do inactive peptidases become active and where?
They must be enzymatically cleaved within the small intestinal lumen
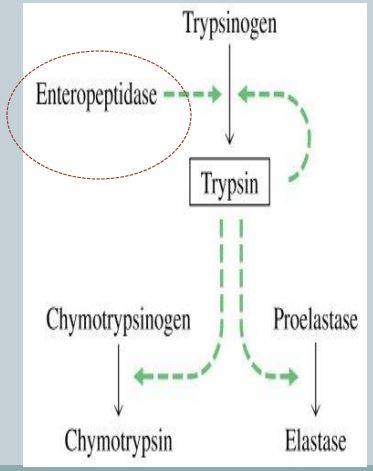
Describe the initial step if the activation cascade
Trypsinogen → Trypsin, catalyzed by Enterokinase (also called enteropeptidase)
The brush border enzyme, Enterokinase, cleaves a hexapeptide from the pancreatic precursor Trypsinogen, forming proteolytically active Trypsin
Why is Trypsin Autocatalytic?
Once a small amount of Trypsin becomes activated, it cleaves its own precursor, which accelerates its own activation
What other pancreatic protease precursors, besides Trypsinogen, does Trypsin cleave?
-It cleaves Chymotrypsinogen → Chymotrypsin (active form)
-It cleaves Proelastase → Elastase (active form)
-It cleaves Procarboxypeptidase A & B → Carboxypeptidase A & B (active form)
How does Pancreatic Inactivation occur?
Occurs through Autodigestion or Cross Digestion
Luminal (Cavital) Digestion is performed by (in big picture terms)
Digestive enzymes secreted into the GI Lumen (mainly by pancreas but also stomach & salivary glands)
Membrane (Contact) Digestion is performed by (in big picture terms)
Digestive enzymes bound to apical Microvilli that comprise the “brush border" of small intestine enterocytes