11. Diseases of the lips. Mouth diseases. Gingivitis. Tartar. Neoplasia of the soft and hard tissue in mouth. Cleft palate. Oronasal fistula. Surgical diseases of the nose.
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
69 Terms
What are examples of diseases of the lips?
Lip fold dermatitis
Eosinophilic granuloma complex
Feline eosinophilic granuloma complex
What is lip fold dermatitis?
Chronic skin inflammation of drooping upper lips and lower lip folds.
Accumulation of moisture in the lip folds, leading to irritation, inflammation, and a good environment for bacterial growth. Worsens with bad oral hygiene
Conservative: Clipping hair, cleaning folds with mild skin cleansers/chlorhexidine, keeping the area dry
Surgical correction of droopy lips.
In which animals can eosinophilic granuloma complexes be found?
Dogs, horses (rare)
Cats (common)
A type IV hypersensitivity reaction
Which breed of dog is predisposed to eosinophilic granuloma complex?
Siberian Husky

What are the clinical signs of eosinophilic granuloma complex regarding lips?
Dental prophylaxis, fluids, nutritional support, antibiotics (amoxicillin), and corticosteroids (prednisone: 0.5-1 mg/kg PO for 7 days, taper off).
What are examples of mouth diseases?
Stomatitis
Gingivitis
Periodontitis
Feline odontoclastic resorptive lesions
Trauma and periodontal disease/gingivitis (Ulcers where the lip touches tartar (upper lip next to P4 or canines)
Heavy metal poisoning
Oral neoplasia
Chemical injury – strong acid or alkali
Metabolic – renal failure, DM, hypothyroidism
Idiopathic – eosinophilic granuloma complex
Infectious – Herpes, Calici, Candida, spirochaetes
Auto-immune – SLE, pemphigus, idiopathic vasculitis, toxic epidermal necrosis
Immune-deficiency – FeLV, FIV
What are causes of gingivitis?
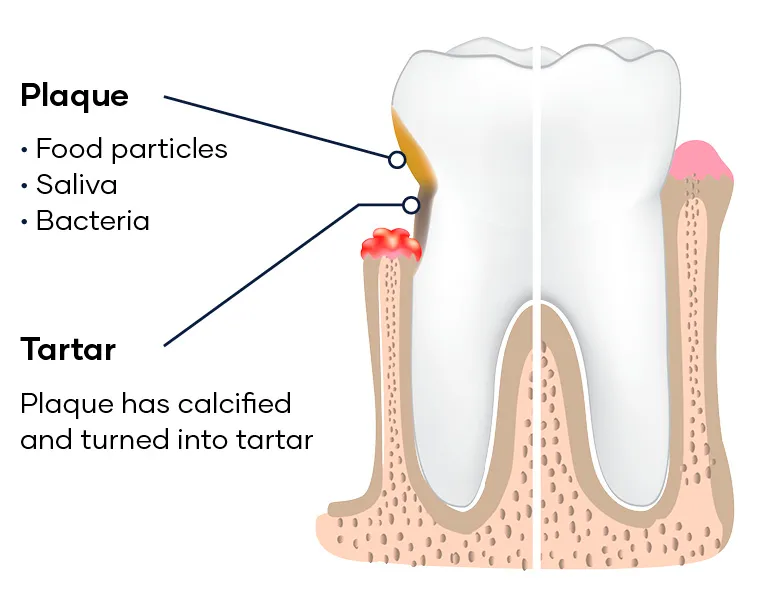
Plaque: microorganisms form in a matrix of salivary glycoproteins and extracellular polysaccharides, adhere to tooth covering
Complicated by bacteria: Actinomyces, Streptococcus, Porphyromonas gingivalis, Fusobacterium, Prevotella
Tartar: mineralised plaque >2 weeks in duration
Forms in layers, separated by organic cuticle, mineralised plaque forms from saliva and sulcular fluid
Stage 0: Normal
Stage 1: Mild gingivitis (reversible)
Stage 2: Moderate gingivitis (reversible)
Stage 3: Periodontitis (irreversible)
Stage 4: Severe periodontitis (irreversible).
Mild plaque and inflammation of the gingival margin.
Moderate sub-gingival plaque and supra-gingival calculus, moderate gingivitis.
Increasing plaque and calculus (including sub-gingival), established gingivitis, pocket formation, and radiographic changes.
Severe gingival inflammation, deep pocket formation, bone loss, and tooth mobility.
Bacteria grow and adhere to teeth → plaque progresses under the gingiva → loss of connective tissue → deep pockets. Plaque then mineralises into tartar → swelling, bleeding, pus formation, bone loss, gingival recession, root exposure, and loose teeth.
Red gingival margins, periodontal pockets, pain on gum palpation, halitosis, reluctance to eat hard food, gingival recession, black calcified material on teeth, root mobility, root exposure, and purulent discharge.
Clinical signs, X-rays of roots, and probing for pockets (deep pockets are > 3mm).
What are complications of periodontitis if not treated?
Deep periodontal pockets → anaerobic environment for virulent strains → pneumonia, endocarditis, micro-abscessation in liver or kidneys
Resorption of dentine from inside out, loss of cementum and dentine, penetration of the pulp cavity, resorption up to the crown, and replacement of resorbed tissue with bone-like tissue.
Squamous cell carcinoma
Melanoma
Fibrosarcoma
Reticulo-endothelial cell tumours
Rhabdomyosarcoma
Leiomyoma (often infiltrative and ulcerative).
Complete surgical excision, potentially including tongue resection.
Tongue resection is a bloody procedure, can be controlled by electro-cautery or temporary occlusion of carotid arteries
What are some complications of oral neoplasia?
Primary (harelip – affecting the upper lip and maxilla)
Secondary (affecting the hard or soft palate or both).
What is the most common cause of cleft palate in cats?
Traumatic after falling from great heights.
Vary depending on severity.
In young animals: starvation, poor growth, milk drainage from nostrils, coughing, gagging, sneezing while eating, respiratory tract infections (aspiration pneumonia), and nasal cavity infections.
Primary cleft palate is obvious at birth.
Secondary cleft palate requires examination of the oral cavity.

Euthanasia (in severe cases)
Removal of affected parents from breeding
Pre-operative care (feeding tube, antibiotics)
Conservative management (orogastric tube feeding, palate guard)
Surgical correction (after 12 weeks of age, potentially requiring multiple surgeries as animal grows).
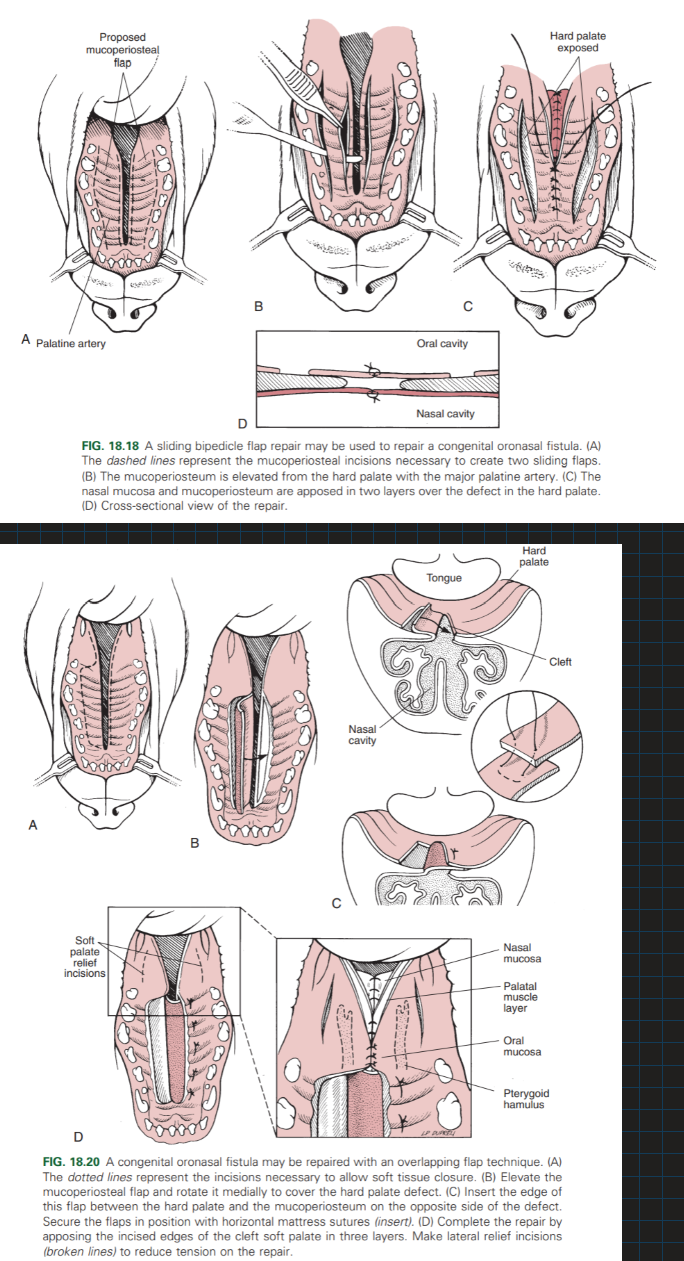
What are some surgical techniques for cleft palate repair?
Separate the oral and nasal cavities by reconstructing the nasal floor – Suture together airtight.
Close opening with an overlapping flap technique or Sliding bipedicle flap repair.
Soft palate: suture together or use overlapping flap technique
What is the post-operative care after surgical repair of cleft palate?
Adequate nutrition - gastric tube, soft food.
Do NOT feed dry food for at least 6 weeks post-op
An abnormal communication between the nasal and oral cavities caused by trauma or disease (e.g., canine tooth extraction, periodontal disease).
Chronic rhinitis, sneezing, chronic unilateral serous or mucopurulent nasal discharge, drainage of water/feed from nostrils, cough, aspiration pneumonia.
Conservative management (antibiotics for rhinitis, tube feeding)
Surgical correction (simple suturing for small fistulas, flap techniques for larger ones).
What is the flap technique for operating on an acquired oronasal fisula?
Create a flap from surrounding tissue to cover the fistula. Mucosal, single/double layer, hard palate, soft palate flaps
Nasal tumors: Removal of neoplastic growths from nasal structures (e.g., squamous cell carcinoma). - Rhinotomy
Nasal foreign bodies: Surgical removal of lodged foreign materials (e.g., grass awns). - Rhinotomy/endoscope
Chronic rhinitis/sinusitis: Inflammation of the nasal passages - Sinusotomy
Nasal fractures: Surgical correction of traumatic nasal fractures. Open reduction internal fixation (ORIF) or closed reduction
What is the main problem caused by soft palate surgery?
Swelling
How often should dogs be checked for dental care?
Small dogs: every 6 months
What can cause acquired cleft palate?
Trauma in cats after falling
What can untreated oronasal fistulas cause?
Aspiration pneumona, panophthalmitis (severe, purulent inflammation of all layers and structures of the eye)