Quiz 9: Biomedical Sciences
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
What are the three main tissues that regulate Ca and P balance in the body?
GI tract (absorption), kidney (reabsorption/excretion), and bone (storage and release)
Which hormones regulate Ca and P homeostasis?
parathyroid hormone (PTH), calcitriol (active vitamin D), and FGF23 (mostly for P)
Calcitonin exists but has minimal physiologic relevance.
What is the overall goal of Ca/P homeostasis?
maintain tight serum levels through balanced intake, storage, and excretion
Which hormones are physiologically most important for calcium regulation?
PTH and calcitriol
Calcitonin is not physiologically essential
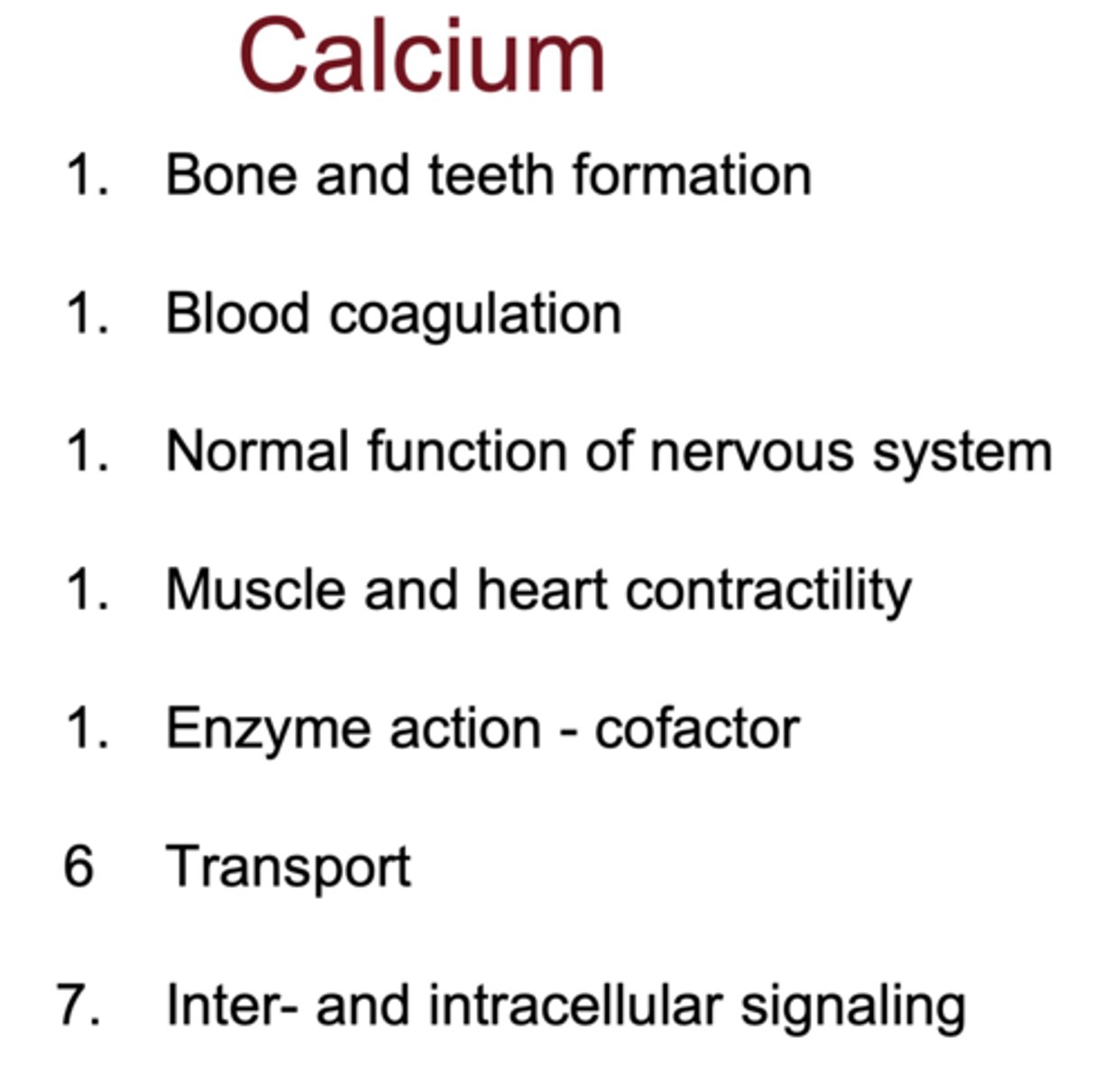
What are the major functions of calcium in the body?
- bone/teeth formation
- muscle and cardiac contractility
- neurotransmission
- blood coagulation
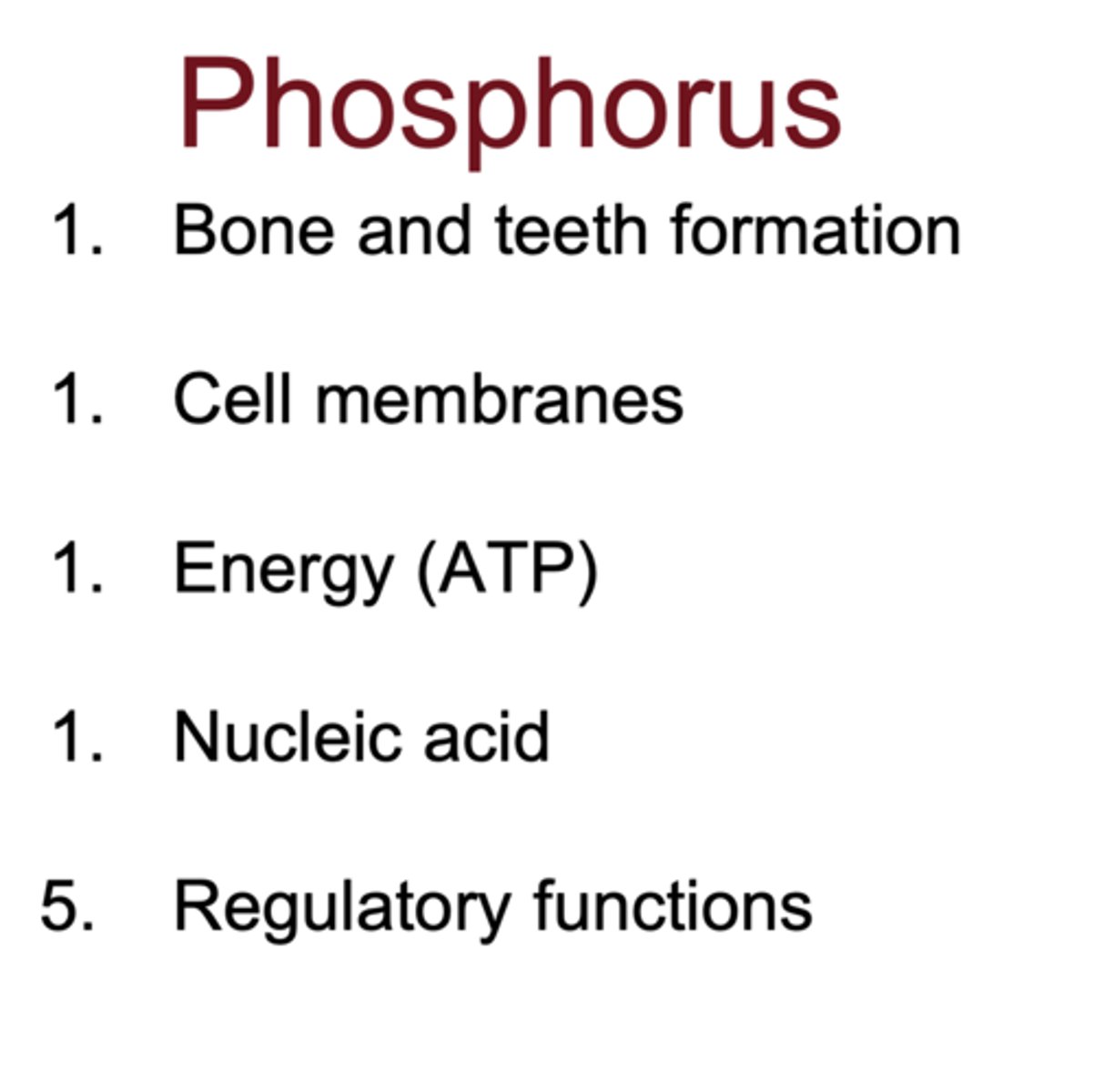
What are the major functions of phosphorus in the body?
- bone/teeth formation
- ATP production (energy)
- nucleic acids
- cell membrane structure (phospholipids)
- regulatory functions
Why are small serum calcium changes clinically significant?
it affects critical systems like neuronal excitability, cardiac rhythm, muscle contraction. Even slight imbalance causes dysfunction
What disease is caused by vitamin D deficiency in children leading to bone softening?
rickets
What are symptoms of hyperparathyroidism?
kidney stones, bone loss (osteoporosis), and muscle weakness
What disorders involve excessive bone resorption?
osteoporosis, Paget's disease, and hyperparathyroidism
What symptoms occur in hypoparathyroidism?
tetany, heart block, neuromuscular excitability
What is the key for balance in whole-body calcium turnover?
dietary intake must equal urinary and fecal losses, with bone as major storage
What organ filters the most calcium daily, and what percent is reabsorbed?
the kidney; over 98% of filtered calcium is reabsorbed
Why is renal excretion of calcium important despite low amounts?
even small changes in urinary calcium significantly affect serum Ca balance
Which 3 tissues does PTH target?
bone (increase resorption), kidney (increase reabsorption), GI tract indirectly via calcitriol
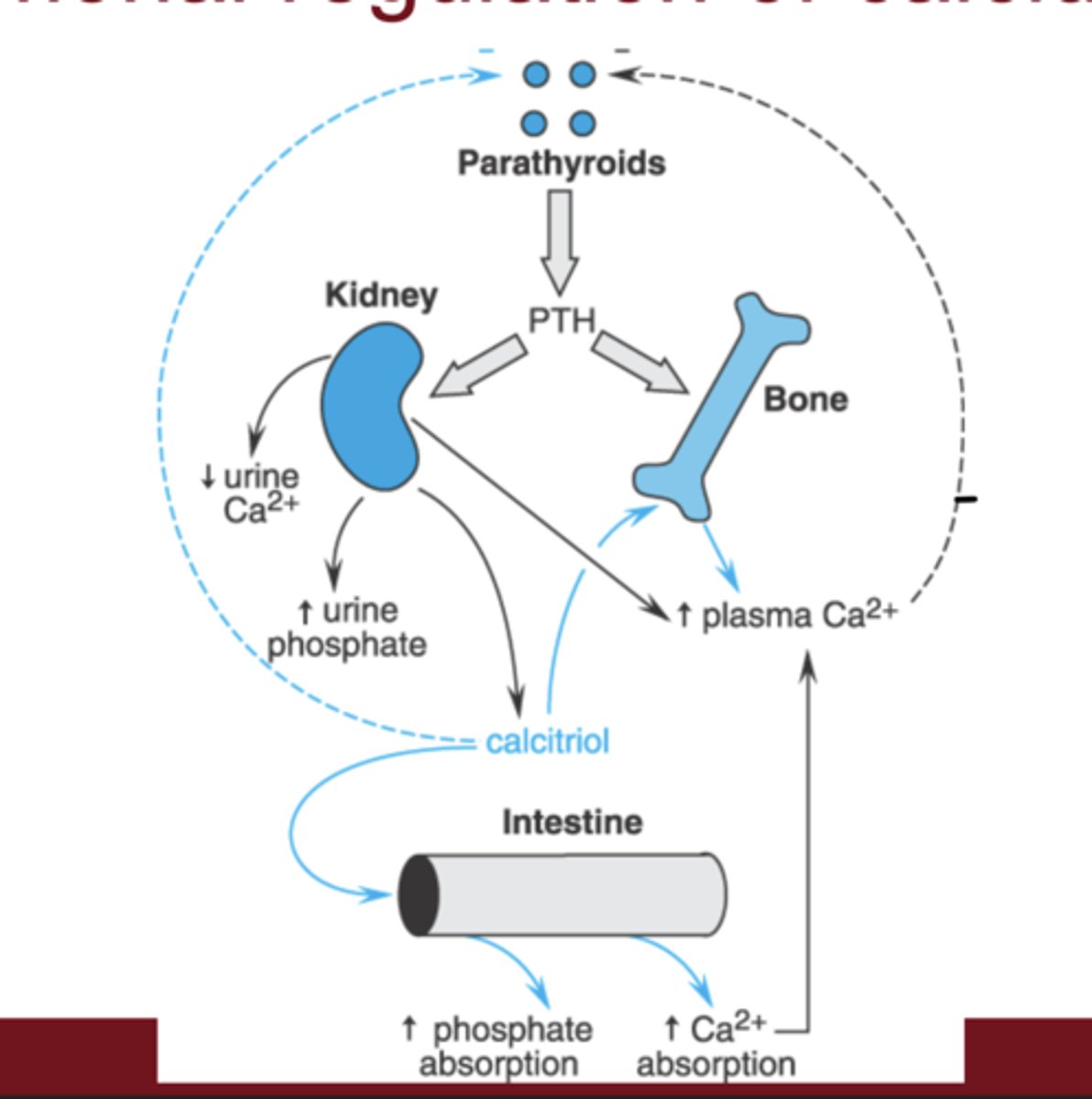
How does calcitriol indirectly influence calcium?
it increases calcium absorption from the GI tract
How does PTH affect phosphate levels?
it decreases phosphate by inhibiting reabsorption in the kidney
What determines bone density?
balance between osteoclast-mediated resorption and osteoblast-mediated bone formation
Which cell type releases calcium from bone?
osteoclasts
Which cell type builds new bone and sequesters calcium?
osteoblasts
What are the three key proteins required to absorb calcium through intestinal cells?
TRPV channels, Calbindin, and PMCA (plasma membrane calcium ATPase)
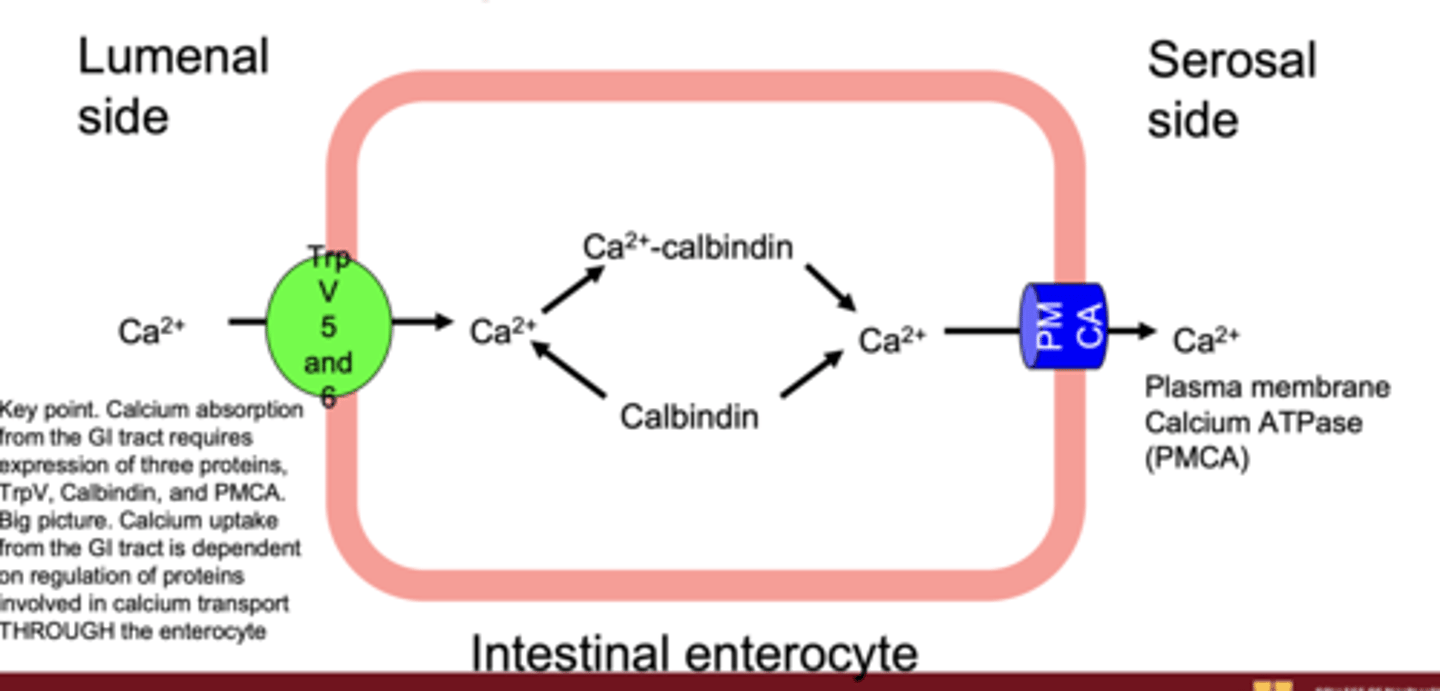
What is the role of calbindin in enterocytes?
binds calcium and shuttles it across the cell to prevent toxicity and allow transport to blood
What is the big-picture concept behind intestinal Ca absorption?
hormone-regulated expression of transport proteins moves calcium THROUGH the enterocyte into blood
Which three proteins are required for renal calcium reabsorption in the distal tubule?
TRPV channels (5 and 6), Calbindin, and PMCA (plasma membrane calcium ATPase)
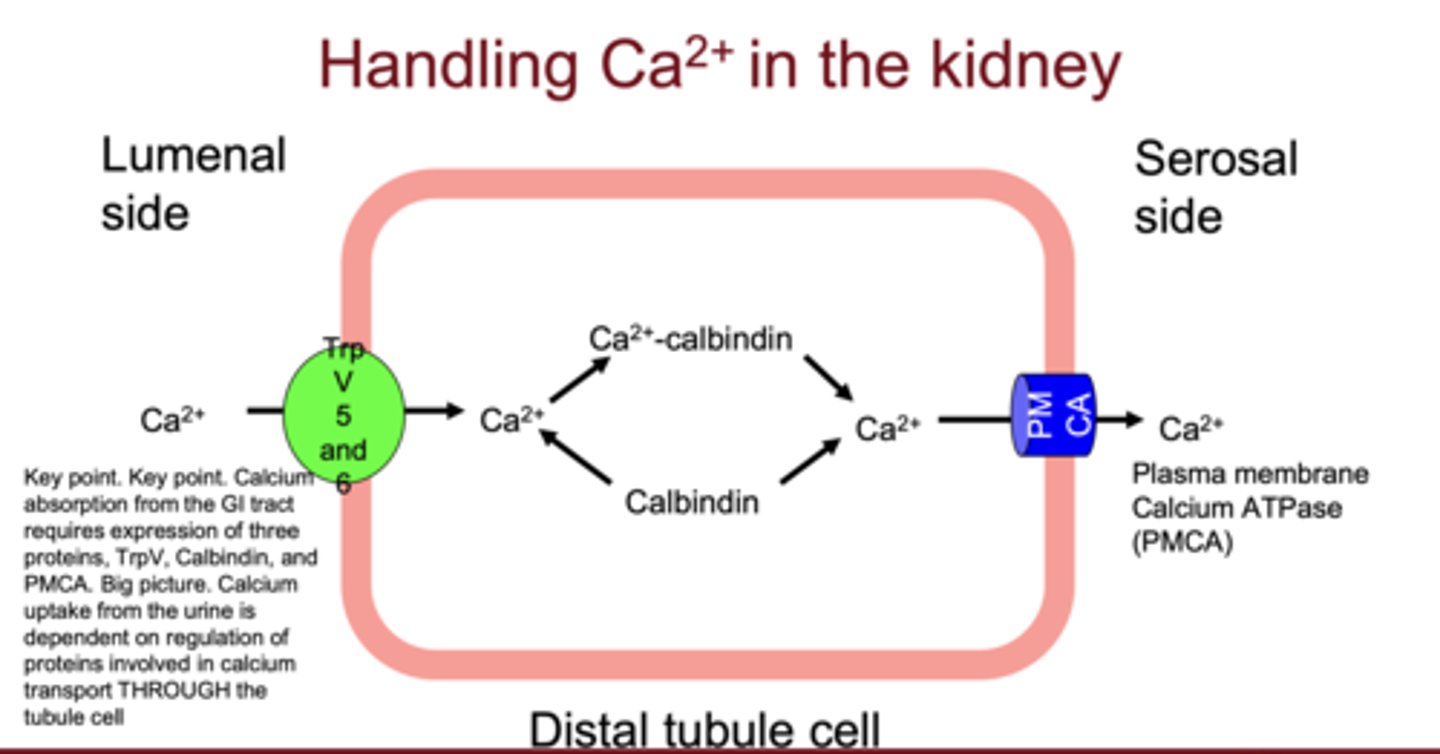
What hormone stimulates renal expression of TRPV5/6, Calbindin, and PMCA?
Parathyroid hormone (PTH)
Where does hormonally regulated calcium reabsorption mainly occur in the kidney?
distal convoluted tubule
Where is the parathyroid gland located?
posterior to the thyroid gland in the neck
Is PTH a peptide, steroid, or amine hormone?
PTH is a peptide hormone
What is the effect of PTH on bone?
increases bone resorption, activates osteoclasts, and releases Ca²⁺ and phosphate into blood
What is the effect of PTH on calcium in the kidney?
increases calcium reabsorption by upregulating TRPV, Calbindin, and PMCA
How does PTH affect phosphate in the kidney?
inhibits phosphate reabsorption (promotes phosphate excretion)
What enzyme does PTH stimulate in the kidney?
1-alpha-hydroxylase (converts vitamin D to calcitriol)
What is the strongest stimulus for PTH secretion?
decreased serum ionized calcium
What two signals decrease PTH secretion?
increased serum calcium and high calcitriol levels
How does calcitriol decrease PTH production?
directly suppresses PTH gene transcription in the parathyroid gland
How does PTH secretion respond to small changes in ionized calcium?
PTH release changes drastically in response to even small calcium fluctuations, demonstrating tight regulation
What type of feedback regulates PTH release by calcium?
negative feedback (higher calcium suppresses PTH)irect negative feedback — decreases PTH gene transcription
How does ionized calcium inhibit PTH secretion at the cellular level?
calcium binds to Ca-sensing receptors on parathyroid cells → inhibits PTH gene transcription and secretion from granules
What happens when Ca-sensing receptors are unactivated (low Ca²⁺)?
PTH secretion increases
What happens when PTH binds to distal tubular cells?
it stimulates expression of TRPV channels, Calbindin, and PMCA for Ca²⁺ reabsorption
Why is renal calcium reabsorption vital to PTH function?
prevents excessive calcium loss in urine and defends plasma Ca²⁺ levels
What is the first rapid response to reduced plasma calcium?
rapid release of calcium from the labile pool in bone (independent and PTH-stimulated)
What is the slow response to low serum calcium?
PTH stimulates osteoclasts to resorb bone and produce calcitriol → increasing GI absorption of calcium
How does PTH prevent calcium-phosphate precipitation?
inhibits phosphate reabsorption → lowers serum phosphate → prevents Ca-P complex formation
Which processes are rapid in PTH response?
bone labile Ca release, renal Ca reabsorption, and phosphate excretion
Which processes are slow in PTH response?
osteoclastic bone resorption and calcitriol-mediated GI absorption
Why is calcitriol activation slow?
it requires kidney conversion via 1-alpha-hydroxylase and acts through gene expression changes
Where is most phosphorus stored in the body, and in what form does it circulate in blood?
~85% in bone; circulates as phosphate (HPO₄²⁻ / H₂PO₄⁻)
What are the three main hormones regulating phosphorus homeostasis?
PTH, FGF23, and calcitriol
What are the two major hormone target organs for phosphorus regulation?
kidney (elimination) and GI tract (absorption)
- bone is minor
What is the primary mechanism for regulating serum phosphorus?
renal phosphate excretion (proximal tubule)
How does PTH affect phosphate in the kidney?
inhibits phosphate reabsorption by degrading Type IIa transporters on urine side
How does FGF23 regulate phosphate?
decreases calcitriol synthesis and inhibits both uptake and efflux of phosphate in kidney
What stimulus causes bone to release FGF23?
high serum or dietary phosphate
How do PTH and FGF23 interact in phosphate regulation?
both inhibit phosphate reabsorption in kidney, but have opposite effects on calcitriol
Which hormones stimulate 1α-hydroxylase?
PTH, estrogen, low Ca²⁺/P
Which hormones inhibit 1α-hydroxylase?
FGF23 and calcitriol (self)
What is the precursor of vitamin D, and what activates it?
cholesterol; activated by UV light in skin → Vitamin D₃ → liver (25-OH) → kidney (calcitriol)
How does calcitriol affect the parathyroid gland?
direct negative feedback → decreases PTH gene transcription
How do PTH, calcitriol, and FGF23 coordinate?
PTH: ↑ Ca, ↓ phosphate
Calcitriol: ↑ Ca & phosphate (GI)
FGF23: ↓ phosphate & ↓ calcitriol
**Together maintain Ca/P balance
How does chronic kidney disease (CKD) affect Ca/P homeostasis?
reduces calcitriol production and phosphate excretion → ↑ PTH (secondary hyperparathyroidism)