INTRAOP PT.2 (my copy)
1/59
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
Topical Application
Anesthetic agent applied directly into the mucosal membrane to a serous surface or into an open wound.
may be applied such as the skin, inside the mouth or throat, in the nose, or in the eyes.
Local Infiltration Anesthesia/ Local Anesthesia (LA)
Injected into the tissue around the incisional area
Field Block
Anesthetic agent is introduced around the operative field through a series of injections
Peripheral Nerve Block (PNB)
Administered directly into or around one nerve or group of nerves into the involved area that control sensation and movement to a specific part of the body.
Intravenous Block (Bier block)
often used for arm, wrist and hand procedure
is a type of regional anesthesia where a local anesthetic is injected into a vein, causing temporary numbness and loss of sensation in the distal part of the limb.
an occlusion tourniquet is applied to the extremity to prevent infiltration and absorption of the injected IV agents beyond the involved extremity
Caudal Anesthesia/Caudal Block
Is produced by injection of the local anesthetic into the caudal or sacral canal or anesthesia in the perineum
Spinal Anesthesia/Sub-arachnoid Block (SAB)
Anesthetic agent is introduced into the cerebrospinal fluid (CSF) in the subarachnoid space
Epidural Anesthesia
Administered into the epidural space.
It involves injecting a local anesthetic into the epidural space around the spinal cord, providing pain relief for surgeries or labor.
Sometimes a small tube or catheter is inserted into the epidural space, which allows the anesthesiologist to administer more medications as needed.
often used when long term pain relief is needed
Continuous Lumbar Epidural Anesthesia (CLEA)
Combined Spinal Epidural Anesthesia (CSEA)
Continuous Thoracic Epidural Anesthesia (CTEA)
Types of Epidural Anesthesia
Continuous Lumbar Epidural Anesthesia (CLEA)
continuous injection of an anesthesia solution into the sacral and lumbar plexuses within the epidural space to relieve the pain of childbirth
also used in general surgery to block the pain pathways below the navel.
Combined Spinal Epidural Anesthesia (CSEA)
a regional anesthetic technique, which combines the benefits of both spinal anesthesia and epidural anesthesia.
The indwelling epidural catheter gives the ability to provide long lasting analgesia and to epidural and to titrate the does given to the desired effect.
Continuous Thoracic Epidural Anesthesia (CTEA)
Thoracic epidural analgesia remains a critical tool for anesthesiologist to use in acute pain.
Is particularly effective for reducing pain after thoracic and abdominal surgery, and rib fractures
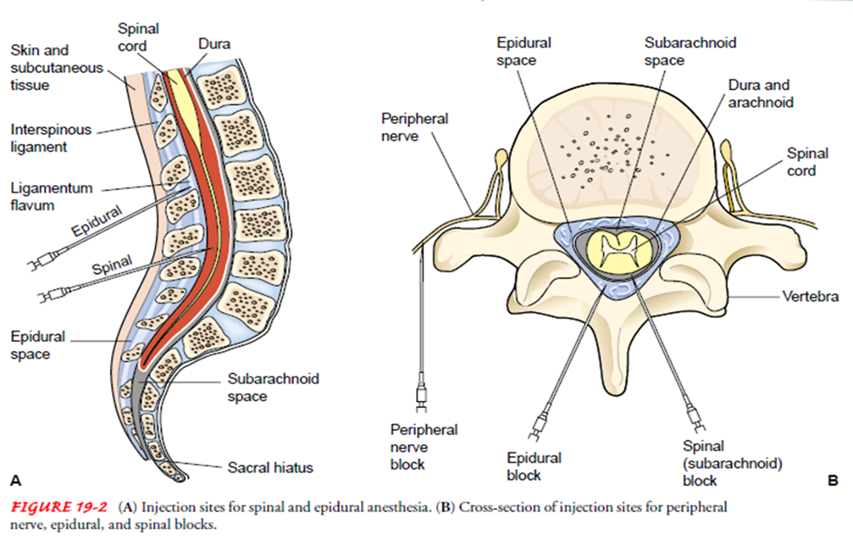
Injection Sites
ANAPHYLACTIC SHOCK
Danger caused by idiosyncrasy of the anesthetic.
HEMORRHAGE
It may cause shock, cardiac arrhythmia, or even death
EMBOLI
air embolism may result from accidental introduction of air into the circulatory system.
CONVULSIONS
danger caused by carbon dioxide retention, air embolism, over dosage of regional drugs.
CARDIAC ARREST
A sudden cessation of cardiac function.
CIRCULATORY DEPRESSION OR SHOCK
danger caused by hemorrhage, fast moving of the unconscious patient, rough handling of tissues, or severe fright.
CORONARY THROMBOSIS
danger from severe hypoxia.
CARDIOVASCULAR OCCLUSION
danger from sudden drop of blood pressure
CEREBRAL HEMORRHAGE
caused by sudden increased in blood pressure.
CEREBRAL EDEMA
from cerebral hypoxia. As prevention, move anesthetized patient gently & slowly to allow the circulation to adjust to position to change
BRONCHOSPASM & LARYNGOSPASMS
are caused by certain allergic conditions.
ASPIRATION
may occur during abolition of throat reflexes when the patient is unconscious.
Draping
Purpose is to create and maintain an adequate sterile field during operation.
Counting
Method of accounting for items placed on the sterile table for use during the surgical procedure
Baseline count
during set-up for the surgical procedure
As scrub nurse touches each item, he/she and the circulator count each item ALOUD until finished.
Circulator then documents count for each type of item
Counting should not be interrupted
If the scrub/circulator is PERMANENTLY relieved by another person during surgery, the incoming person should verify all counts.
1st closing count
done before the surgeon starts the closure of a body cavity or a deep large incision
Field count – surgical field
Table count – Mayo stand and instrument table
Floor count – materials recovered from the floor
2nd closing count
done during skin closure
Circulator totals the field, table and floor counts
If final count = total in the tally sheet, circulator informs the surgeon that counts are correct
Incorrect count
The surgeon is informed immediately
The entire count is repeated
Circulator – searches the trash receptacle, under the furniture, floor, laundry hamper and throughout the room
Scrub – searches the drapes and items in the OR table and Mayo stand
Surgeon – surgical field and wound
Circulator – inform OR supervisor to check count and assist with search
Circulator – completes an Incident Report (IR)
X-ray
If all measures exhausted in incorrect count:
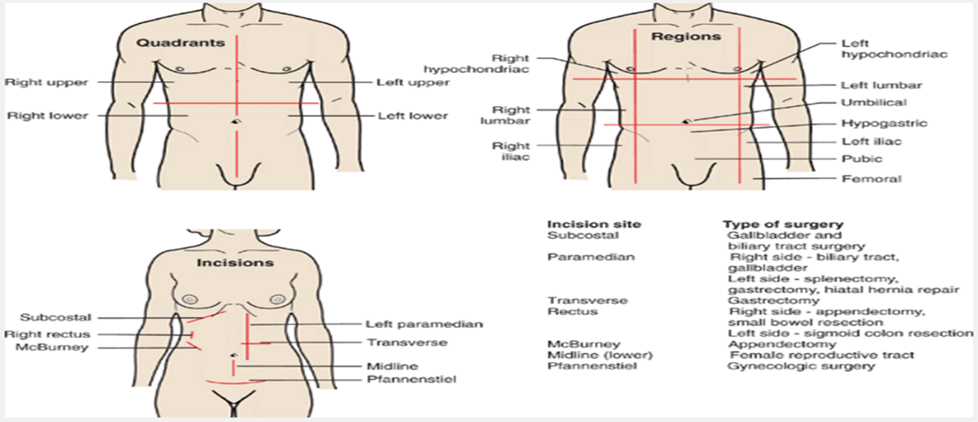
Butterfly incision – for craniotomy
Limbal incision – for eye surgeries
Halstead / Elliptical incision – for breast surgeries
Abdominal incision – for abdominal surgeries
McBurneys incision – for appendectomy
Pfannenstiel – for CS
Lumbotomy or transverse incision – for kidney surgeries
Common Surgical Incision (BLHAMPL)
Type of surgery (anatomical location)
Maximum exposure
Ease and speed of entering (for emergency surgery)
Possibility of extending the incision
Maximal post operative wound strength
Minimal post operative discomfort
Cosmetic effect
The choice of the incision is made by the surgeon with the following considerations:
Skin – interrupted stitch, cutting needle is used
Subcutaneous (yellow) - not always sutured, round needle
Fascia (white) – interrupted stitch, cutting needle
Muscle (red) – interrupted stitch
Peritoneum (white) – continuous stitch, round needle viscera
****Uterus (dark violet) – continuous stitch, round needle is used
Five Main Layers of Abdominal Cavity (SSFMPU)
Suture
Any material used to sew, stitch or hold tissue together until healing occurs.
Ligature/”tie”
A material that is tied around a blood vessel or any hollow organ to occlude its lumen
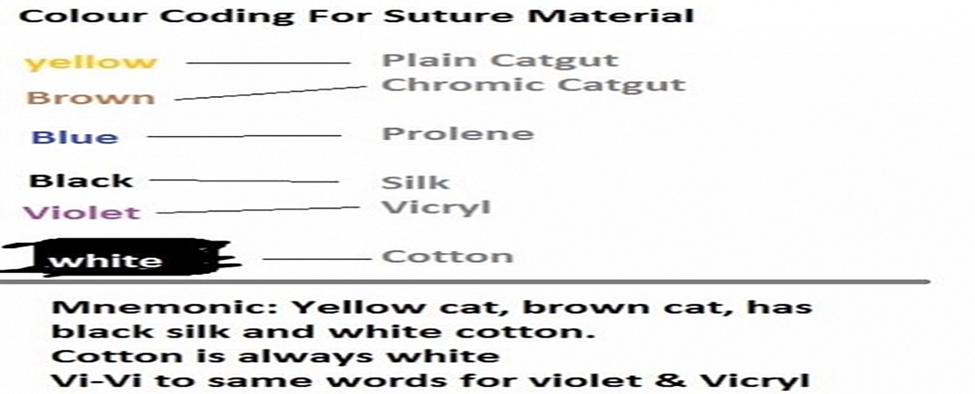
Color Coding for Suture Material
Absorbable suture
digested by body enzymes during the wound healing process
e.g. surgical gut (catgut) collagen and synthetic
Non-absorbable suture
made from various materials that are not affected by the digesting enzymes
remains encapsulated when buried in tissues and is removed post-operatively when used as skin sutures
e.g. Surgical silk, Surgical cotton, Dacron, Nylon, Polythylene, Stainless steel
Types of Suture
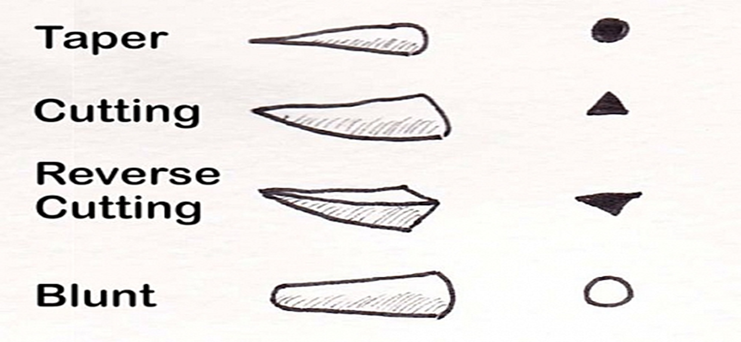
Needle types edges in surgical sutures
1.0 to 7.0
Just as in Canula, the higher the number on surgical sutures, the smaller the size.
The sizes range from sizes _________ but in chromic suture, it is larger than 1.0
Triangular, Round
Cutting needles- cross-section is _____, it is very sharp and/traumatic and is used for skin
Non-traumatic needle- cross section is _____, used for subcutaneous tissue and bowel
Non-absorbable sutures
these take about 7-10 days to come back for removal
10 to 14
Lower limb takes ___ days.
7 to 10
Abdomen takes ___ days to absorb sutures
5 to 7
Chest wall and upper limb takes ___ days to absorb sutures
3 to 5
Sutures used on the Head and neck can be removed after __ days
Hypoventilations & Hypoxemia
Nausea/Vomiting
Oral trauma (broken teeth, oropharyngeal, or laryngeal trauma)
Hypotension
Cardiac Dysrhythmia
Hypothermia
Headache
Peripheral Nerve Damage
Malignant Hyperthermia
Intraoperative Complications
Malignant Hyperthermia
A rare reaction to anesthetic inhalants (notably sevoflurane, enflurane, isoflurane, and desflurane) and muscle relaxant, succinylcholine
Caused by abnormal and excessive intracellular accumulations of calcium with resulting hypermetabolism, increased muscle contractions, and elevated body temperature
IV dantrolene sodium (Dantrium)
Malignant Hyperthermia treatment consists of discontinuing the anesthetic inhalant, administration of ______, and applying cooling techniques (e.g. cooling blanket, iced saline lavage)
Classify the client’s physical status for anesthesia
mild disturbances like mild cardiac disease, mild diabetis mellitus
moribund with little chance of survival like rupture aortic aneurysm
Assess the client’s record for appropriate documentation:
current signed consent form
Specifically ask the client about any known allergies.
Verify client identification & that the correct surgery is scheduled.
Assess for special surgical considerations and precautions
locations where an electric grounding plate can be safely placed on the client
avoiding areas where metal or a prosthesis is present
shielding with a lead apron if radiation is involved if the client is pregnant
Assess the client’s risk for accidental hypothermia or malignant hyperthermia during anesthesia administration and surgery
Assessment (SDASSH)
Risk for fluid volume deficit or excess
Risk for hypothermia or hyperthermia
Risk for infection
Risk for altered tissue perfusion cardiac, respiratory and peripheral
Risk for injury
Nursing Diagnosis
The major goals for the client during the intra-operative period may include maintenance of fluid balance, maintenance of normothermia, prevention of infection, adequate tissue perfusion and absence of injury
Planning
Promote measures that maintain adequate fluid and electrolyte balance
Promote measures that maintain the client’s normal temperature of 36.6°C to 37.5°C
Promote measures that decrease risk of infection
Promote measures that ensure adequate tissue perfusion in the client during surgery.
Ensure the client’s safety in the OR
Perform other actions as appropriate.
Implementation
Grounding pad
Act in the role of client advocate, providing privacy & protection from harm.
Follow established procedures & protocols.
Document all OR care.
Help coordinate health team activities.
Promote ethical behaviors (eg, respect, confidentially).
Monitor blood, fluid, & other drainage output.
Maintain a quiet, relaxing atmosphere. Remember, the client can hear
Apply ______.
Ensure the client’s safety in the OR
Set room temperature & humidity to prevent hypothermia
Remove any potential contaminants
Curtail unnecessary room traffic.
Keep room noise & talk at a minimum.
Recheck electrical equipment for proper operation.
Make sure that necessary equipment & supplies are available.
Ensure that instruments, sutures, & dressings are ready.
Count & record sutures, needles, & instruments, & sponges.
Make sure that staff call the client by name & provide individualized attention.
Assist in transferring the client to the OR table.
Cover the client with a warm blanket, & attach the safety strap
Remain at the client’s side during anesthesia induction.
Verify proper client positioning to protect nerves, circulation, respiration, & skin integrity.
Always pad pressure areas.
Ensure that newly requested items are quickly supplied to the anesthesia or scrub team by the circulating nurse.
Maintaining adequate tissue perfusion
Assess the client’s vital signs continuously.
Asses the client’s respiratory status, & assist with mechanical ventilation.
Assess the client’s cardiovascular status.
Assess the client’s peripheral vascular status.
Temperature
ensure that OR temperature is between 20°C & 25°C
warm all intravenous and irrigating solutions
monitor the client’s _____ continuously
remove all wet gowns and drapes promptly & replace with dry to prevent heat
Urometer and electrolyte values
monitor intake & output accurately; use a ______ if needed
assess the client for dehydration to include skin turgor & mucous membranes
assess the client for circulatory overload to include breath sounds, peripheral edema and jugular vein distention
monitor pertinent _________
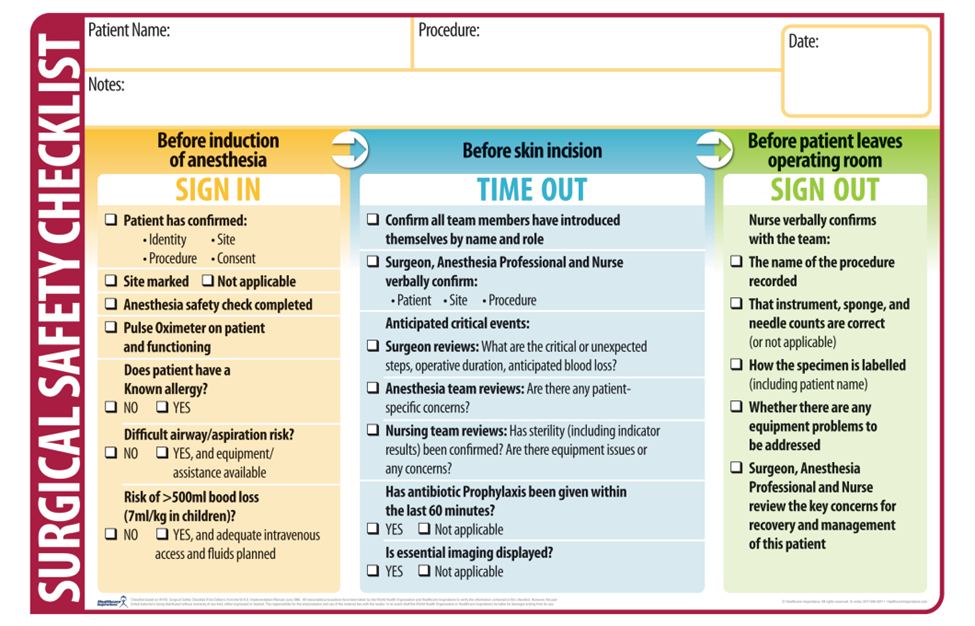
“an immediate pause by the entire surgical team to confirm the correct patient, procedure, and site,” was introduced in 2003, when The Joint Commission’s Board of Commissioners approved the original Universal Protocol for Preventing Wrong Site, Wrong Procedure, and Wrong Person Surgery for all accredited hospitals, ambulatory care centers, and office-based surgery facilities.
represents the last part of the Universal Protocol and is performed in the operating room, immediately before the procedure is initiated.
The "time out" represents the final recapitulation and reassurance of accurate patient identity, surgical site, and planned procedure
have active involvement of the entire surgical team. This means there is 100% oral or visible agreement (nod or gesture) following the time out statement.