Dermatology Lecture 2 Immune and Allergic Responses (Sandy)
1/141
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
142 Terms
This is referred to as inflammation of the skin
Dermatitis
This is an IgE-mediated hypersensitivity that requires two separate exposures to antigen. The first exposure causes sensitization. After the second exposure reaction can be minutes or hours.
Type I (Anaphylactic)
What type of hypersensitivity is anaphylaxis, urticaria and angioedema?
Type I
This type of hypersensitivity has IgG or IgM antibodies that react with cell antigens that results in complement activation. Requires 2 separate exposures to antigen. Considered cytotoxic reaction.
Type II Cytotoxic Hypersensitivity
This type of hypersensitivity has IgG or IgM immune complex that activate the complement system.
Type III immune complex hypersensitivity
This type of hypersensitivity activates T cells against cell surface bound to antigens.
Type IV cell mediated (delayed) hypersensitivity
Contact dermatitis and TB skin test are considered what type of hypersensitivity reactions
Type IV
Slight rubbing of the skin results in exfoliation of the outermost layer of skin resulting in erosions. This demonstrates a plane of cleavage at the dermo-epidermal junction.
Nikolsky sign

Pressure on a bulla leads to lateral extension in normal appearing skin
Asboe-Hansen sign (indirect Nikolsky sign)

Measels-like rash, pink macules and thin papules that become confluent
Morbilliform

What is the hallmark skin symptom of an allergic reaction?
Pruritus
"Itch scratch cycle"
Erythematous, at times edematous papules, plaques, scaling, occasionally oozing secondary to scratching, excoriations. These are consider _____ lesions.
Acute lesions
What are examples of chronic lesions?
Lichenification, PIH
Accentuated lower eyelid fold associated with allergic shiners and pale nasal mucosa
Dennie-Morgan folds

Delayed hypersensitivity reactions are type ___
IV
What is the MC hypersensitivity reaction?
Type IV
What are the cells responsible for the type IV hypersensitivity reaction?
T-cells, monocytes and macrophages
Method of testing for contact allergies in which there is a pinprick to the skin with deposition of a small amount of allergen. Results within 15-20 minutes
Scratch testing
What is the benefit of scratch testing for contact dermatitis?
Results within 15-20 minutes
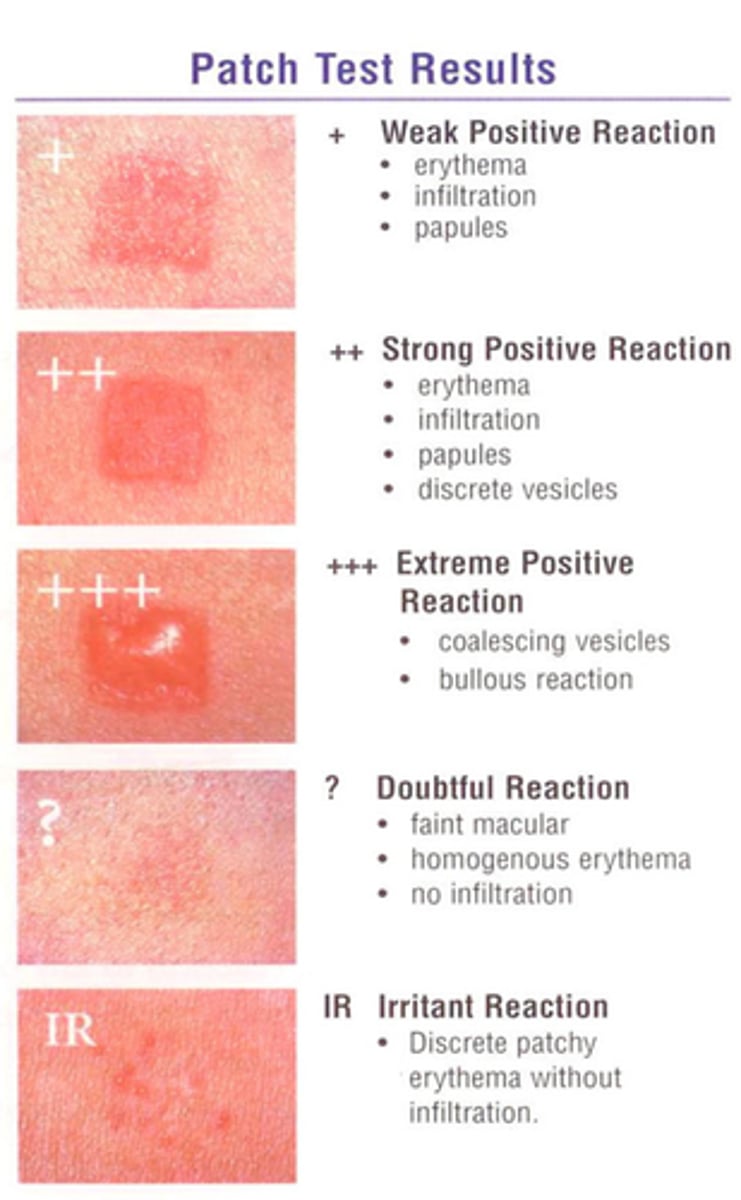
What is the best way to diagnose allergic contact dermatitis?
Patch testing
You have decided to do patch testing for a patient with suspected contact allergy. When should you examine the patient's skin after application?
48 and 72 hours after placement
What is a mild reaction for patch testing?
Erythema
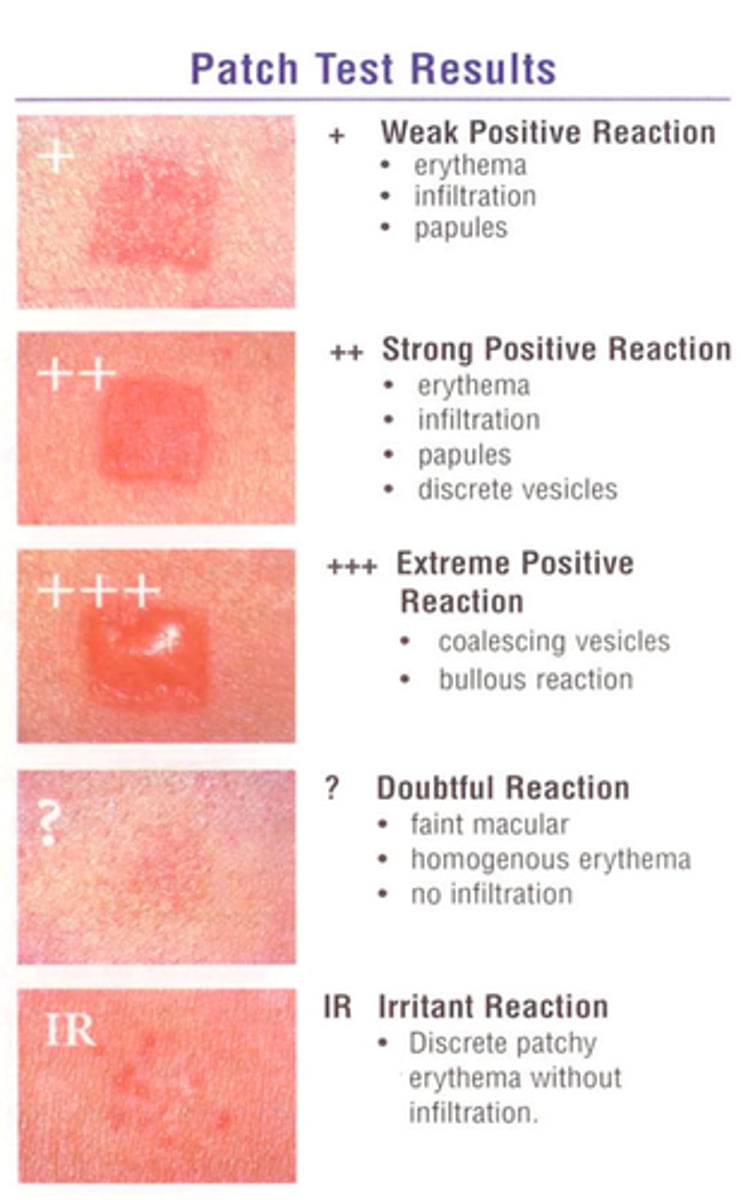
What is considered a moderate reaction for patch testing?
Papules
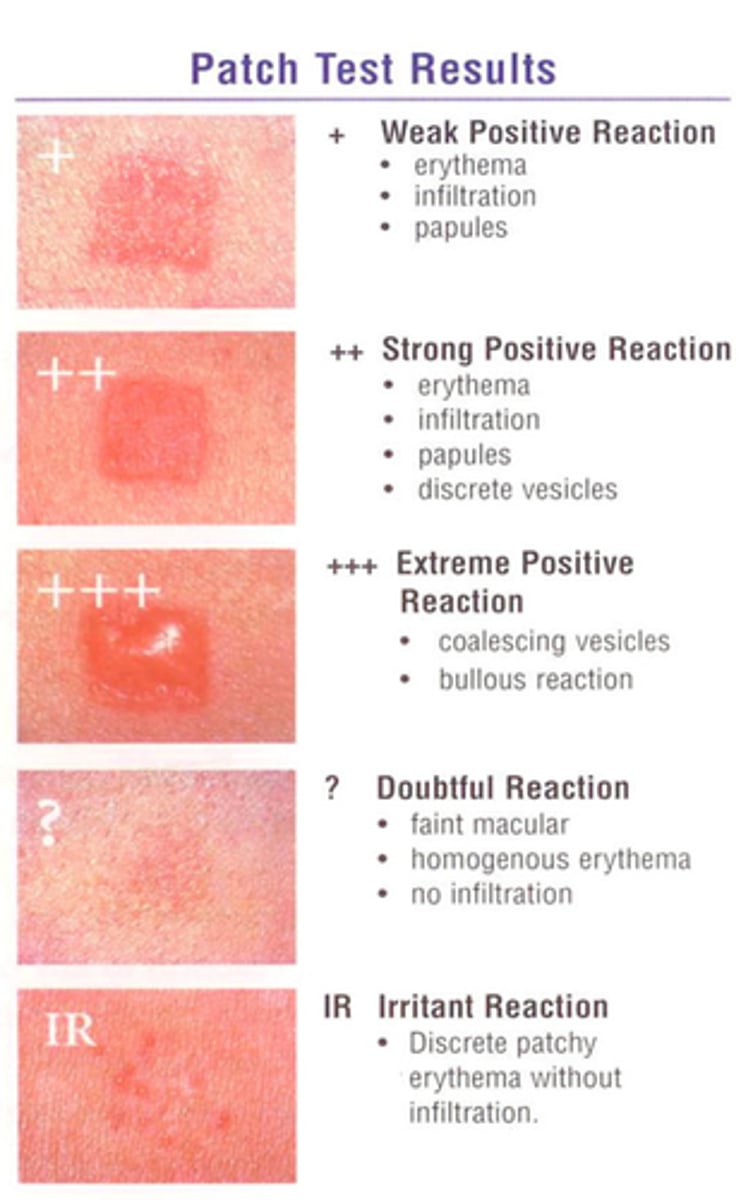
What is considered a severe/extremely positive reaction for patch testing?
Vesicles and bullae
There are 7 classes of medications for dermatitis. Which is the strongest?
Class I is the strongest
Class VII is the weakest
Class I topical corticosteroid used on non-sensitive areas. Good for severe rashes on the body and hands (i.e. poison ivy, severe eczema)
Clobetasol**
Which topical preparation penetrates the skin best?
Ointment
Where should high potency topicals be avoided?
Face and occlusive areas
What is an example of a moderate strength topical corticosteroid (class III-V)?
Triamcinolone (Kenalog)

What is the strength of the following, from strongest to weakest.
Triamcinolone
Clobetasol
Mometasone
1. Clobetasol (strongest)
2. Triamcinolone (middle)
3. Mometasone, desonide, locoid (weakest)
Topical corticosteroid used commonly for children. Used on the face for 3 days and on the body for 7-10 days
Mometasone or desonide (class VII)
To decrease acute inflammation and suppress formation of vesicle you can use?
cold compress
What is the role of lipid rich moisturizers in the treatment of dermatitis? What is their effect?
Help barrier function of the skin by mimicking the lipid layer of normal skin
What is the role of topical coal tars and sal acid preparations in the treatment of dermatitis? What is their effect?
Help to soften the skin and suppress itch
Class of medications indicated if the patient is not responding to oral and topical therapy with severe atopic dermatitis
immunosuppressants
What formulation of topical steroid is best for use on the hands and why?
Ointment because they penetrate the skin better, and the skin of the palms is naturally thicker
What is the recommended regimen for topical use on the body, hands/feet for dermatitis? (frequency, time on vs. time off)
BID, 2 weeks on, 1-2 weeks off, then repeat
A patient with atopic dermatitis on their arms has been given triamcinolone. How many times per day should this be used for? For how many days in a row should they use it? How long should they stop using it before resuming?
BID
2 weeks on
1-2 weeks off
Repeat
What is the recommended regimen for topical use on the face for dermatitis? (frequency, time on vs. time off)
BID 3-5 days on, then 3-5 days off, then repeat
A patient with atopic dermatitis on their face has been given Mometasone. How many times per day should this be used for? For how many days in a row should they use it? How long should they stop using it before resuming?
BID
3-5 days on
3-5 days off
Repeat
However long they are on is how long they should be off for the face
For the face, which class/level of topical steroids is recommended initially? Give some examples of medications in this class
Class V-VII (weak)
Mometasone, Desonide, Locoid
What are two non-steroidal topicals used in the treatment of dermatitis?
Protopic (tarolimus)
Elidel (pimecrolimus)
What is the black box warning for Protopic and Elidel?
Malignancy
What is the benefit of using Protopic and Elidel? What patient population are these topicals particularly useful for?
Non-steroidal, reduced AE
Commonly used in children
What is the issue with phototherapy for dermatitis?
Compliance - patient needs to come back every 2-3 times per week
What type of hypersensitivity reaction are urticaria (hives)?
Type 1
Urticaria is caused by _______ release leads to extravasation of plasma, vasodilation, and edema in the upper portion of dermis (papillary body)
histamine
Transient or evanescent (LESS THAN 24 HOURS) pale to pink-red, edematous papules and plaques. Well defined.
Wheals (Hives) (Urticaria)

Urticaria can be caused by...
Can be associated w/ ____ or ______
Cause: ______
food, medication, insects, parasites, physical, temperature
SLE; Sjogrens
Idiopathic (50%)
What oral medications can be used to tx urticaria?
Topically?
1. Second generation H1 Antihistamines (Certirizine or Fenofexadine)
2. Steroids
Larger edematous area that is deeper involving the dermis and subQ. Ill-defined, skin colored., transient enlargement most commonly occurring on the eyelids, lips, tongue, hands, feet and genitals
Angioedema

What type of angioedema is this ?
• Children
• Face, neck, extremities,trunk
• 7-10 days duration
• Fever, increased body weight from fluid retention
• Increase in leukocytes and eosinophils
• No FH, rare, good prognosis
Angioedema-Urticaria Eosinophilia Syndrome
Hereditary angioedema is an autosomal _____ disorder, may follow _____.
dominant
trauma
What is the treatment of choice for angioedema?
1. Airway protection
2. IV/PO Prednisone
3. Removal of agent
4. EPI if severe
What else can we give if the angioedema is severe?
Epi
Rare extreme reaction to a foreign substance/drug. Often characterized by violaceous patches MC on the leg and can spread to buttocks or trunk. Rash is characterized by Palpable Purpura that can be scattered or discrete.
Allergic cutaneous vasculitis

How long can it take for allergic vasculitis (drug rash) to go away?
6-8 weeks
1. How do you tx allergic vasculitis ?
2. If it is severe, what do we tx with?
1. Removal of offending agent/treat underlying cause
- Supportive care
- possible corticosteroids
2. Severe= PO prednisone
Inflammatory dermatosis of the lower extremity in individuals with chronic venous insufficiency
Stasis dermatitis

In Stasis Dermatitis, there are _______ plaques, scaly and crusted erosions and +/- dermal sclerosis.
_________ is present with old/new hemorrhages and excoriations.
It's MC on the ______ and the ______ . What's the diagnosis ?
Inflammatory
Hyperpigmentation
ankles; lower legs

______ are present in 30% of patients with stasis dermatitis
Ulcers
This is associated with stasis dermatitis where the lower 1/3 of leg has inflammation, pigmentation and induration. There is edema above and below the sclerotic area. Looks like a "Champagne bottle" thats upside down.
Lipodermatosclerosis
What are the risk factors for stasis dermatitis ?
1. Varicose veins
2. superficial phlebitis
3. venous thrombosis
4. pregnancy
A 67 yof present with pruritus, pain, aching, throbbing cramping on ankles and lower legs. Pt states her legs feel heavy but feels better with elevation and ambulating. What is the diagnosis?
Stasis dermatitis

What is the tx for stasis dermatitis?
1. Avoid trauma
2. Compression Stockings
3. Mid-high potency topical steroids BID (clobetasol)
4. Elevation of legs
Patient states legs feel heavy with throbbing pain that gets better with elevation. Immediately youre thinking?
Stasis Dermatitis
Which antibiotic is recommended for ulcerations secondary to stasis dermatitis?
Mupirocin
This is the MC cutaneous drug rash
Erythema multiforme

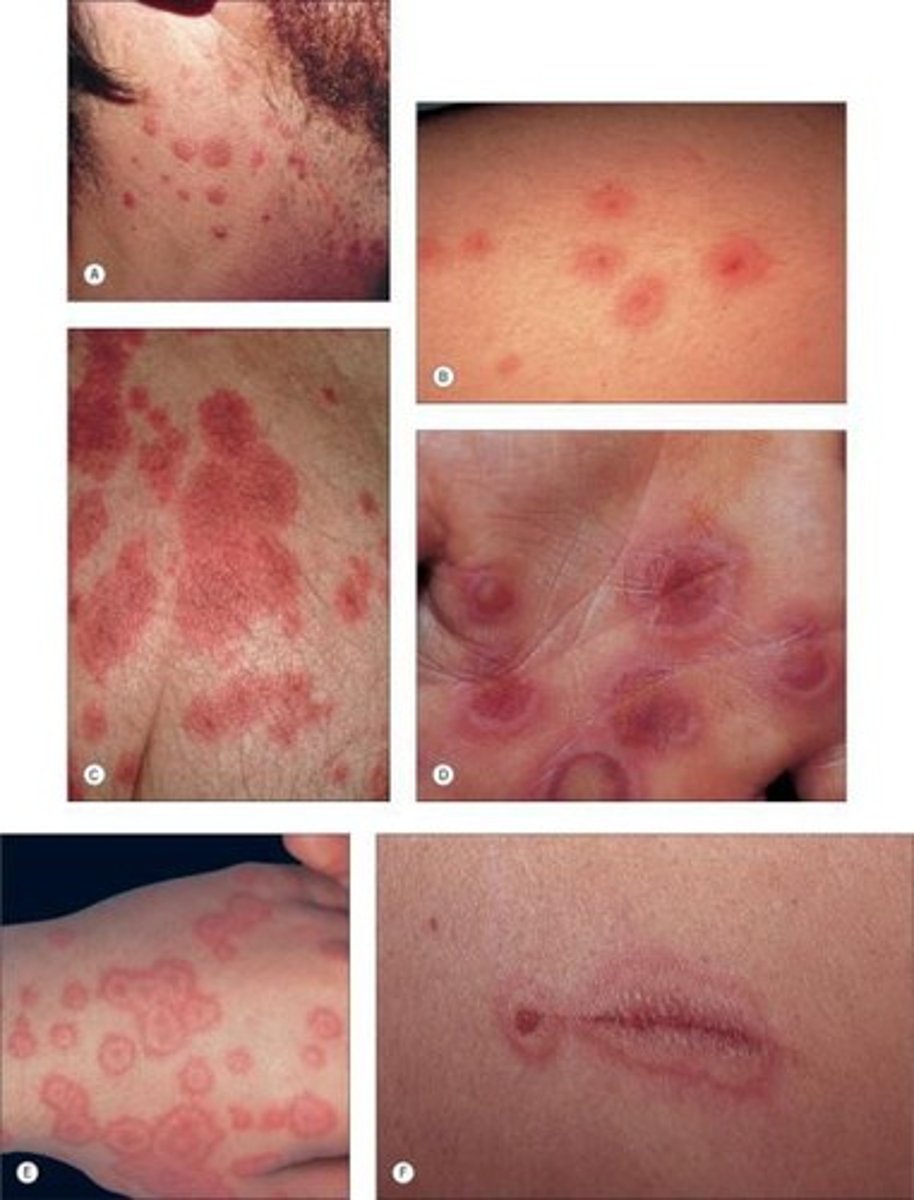
Acute or recurrent cutaneous hypersensitivity IV reaction to antigenic stimuli caused by infection, drugs, or other stimuli. Patient present with dull red, discrete iris or target-like lesions with a negative Nikolsky sign
Erythema multiforme
1. Erythema multiforme is MCC by ?
2. In children ?
1. HSV
2. mycoplasma pneumonia
What drugs can cause Erythema multiforme ?
1. Sulfonamides
2. phenytoin
3. Barbiturates (phenobarbital)
4. penicillin
5. allopurinol
What type of symptoms do pt c/o with Erythema multiforme?
• Pruritus
• Pain (esp mouth lesions)
• Constitutional
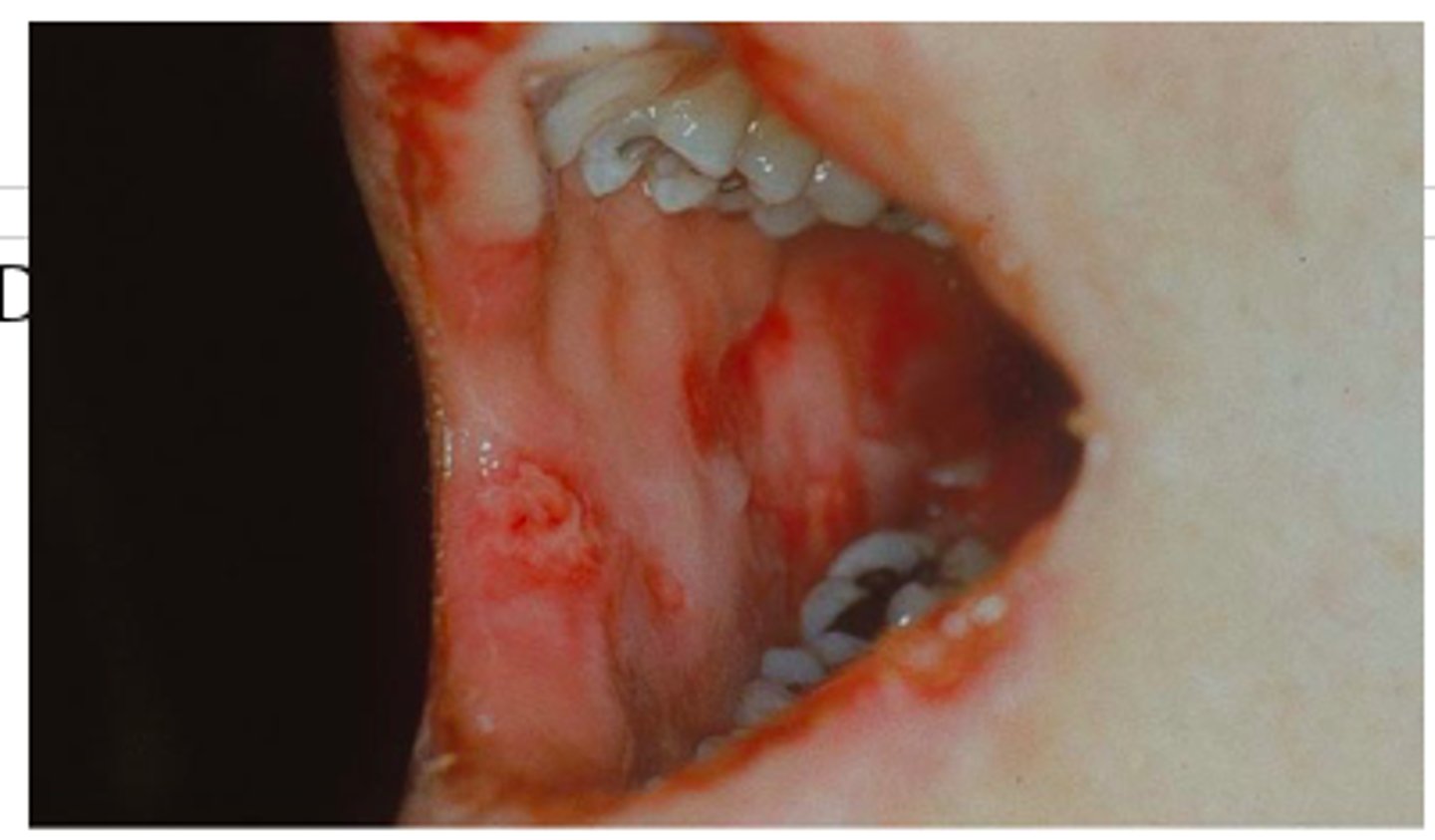
1. What is the tx for symptomatic Erythema multiforme?
2. How do we tx the mouth lesions?
3. If it is severe?
4. if it is caused by mycoplasma or HSV?
1. tx underlying cause
- d/c offending drug
- antihistamines, analgesics, topical steroids, skin care
2. Mouth lesions: mouthwash containing steroids, lidocaine, and diphenhydramine
3. Systemic steroids
3. Abx if mycoplasma and Acyclovir for HSV***
Severe life threatening mucocutaneous hypersensitivity type IV reaction with extensive necrosis and detachment of the epidermis
Stevens-Johnson syndrome/Toxic epidermal necrolysis (SJS/TEN)

SJS & TEN = variants, diff by % of body affected
• SJS: _____ %
• TEN: _____%
• SJS: <10%
• TEN: >30%
Stevens-Johnson syndrome is also known as ____
Erythema multiforme major
What MCC SJS/TEN?
Medications (80%)
What drugs MCC SJS/TENS?
1. Allopurinol
2. sulfa drugs
3. anticonvulsants,
4. lamotrigine
5. NSAIDs, antipsychotics, antibiotics
SJS/TENS occurs _____ weeks after drug exposure
1-3 weeks
What is one of the first symptoms of SJS that occurs 1-3 days before the rash?
Sore throat
-Fever/URI symptoms with skin tenderness then pain, burning sensation, and paresthesia
Morbilliform rash with targetoid with purpuric centers or can be diffuse erythema with no rash
Prodrome rash SJS/TENS
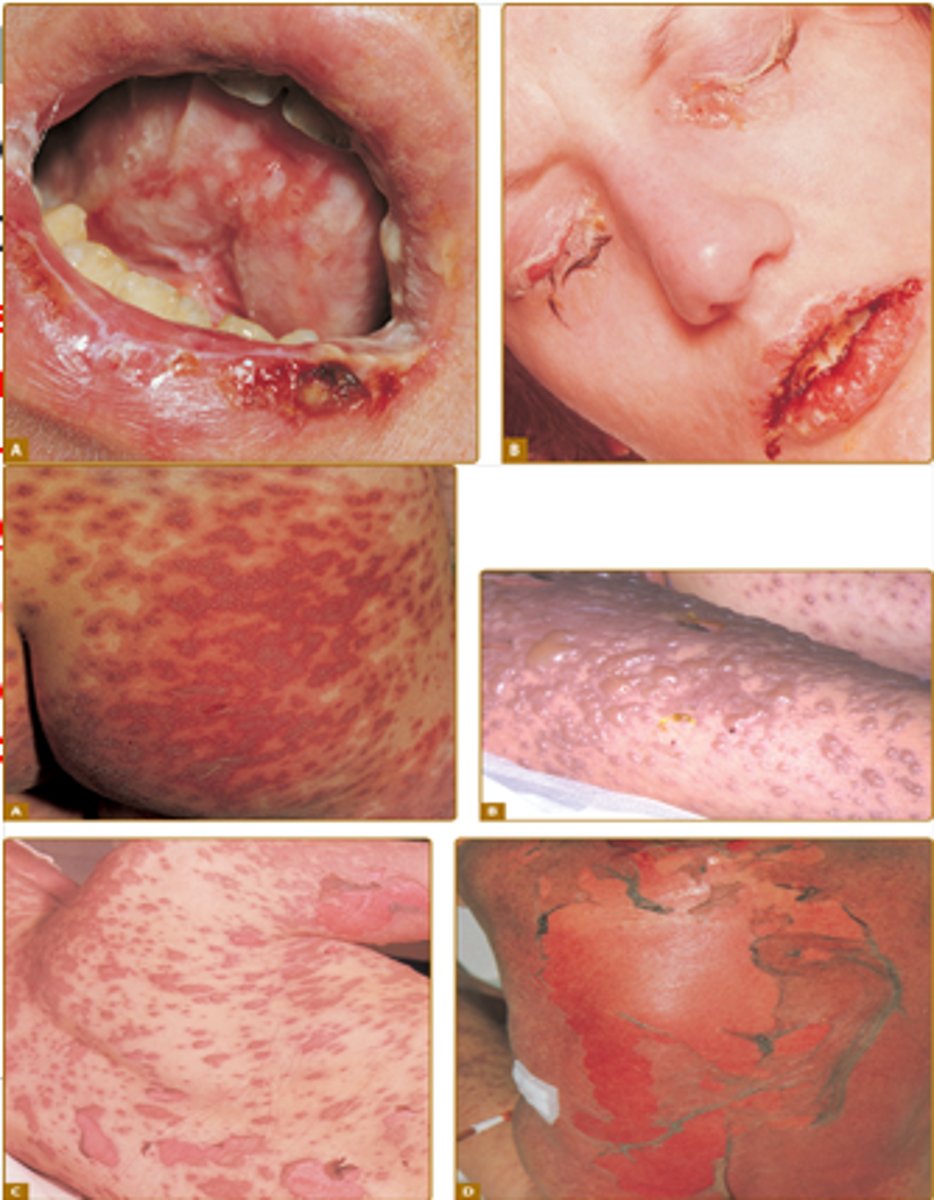
SJS/TENs will have a _______ NIKOLSKY SIGN and ______ bullae & ______ detachment.
POSITIVE
Flaccid
epidermal

At least one _____ membrane is involved in SJS/TEN
mucous
What type of lab abnormalities will a pt with SJS/TEN have?
Anemia, lymphopenia
What are the pt symptoms for SJS/TEN?
• Anxiety
• Pain
• Constitutional
• Sore throat
• Photophobia
How do you tx pt with SJS/TEN?
Tx underlying cause
• Withdrawal of suspected drug
• Admit to ICU or Burn unit
• Supportive therapy: IV fluids, electrolyte replacement, wound care
• Treat any secondary infections
• Medical alert bracelet for recovered patients to avoid medications
• Poor prognosis
What is the MCC of drug reactions?
1. Antibiotics
2. NSAIDS
3. allopurinol
4. thiazide diuretics
5. opiates
6. contrast dye.
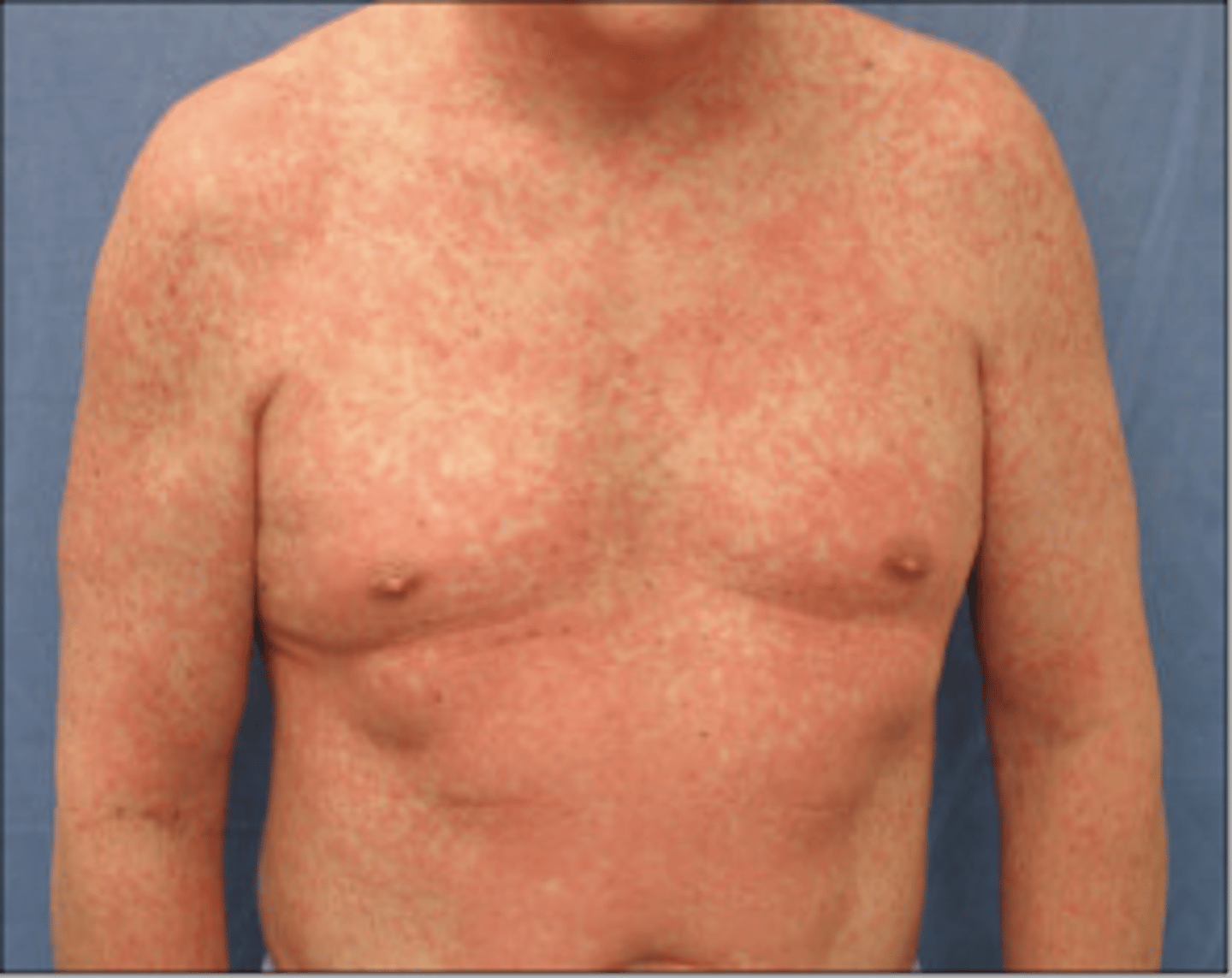
Typically a drug reaction rash begins_______ from onset of offending agent in previously sensitized patient and ______ in naïve patient
2-3 days
5-14
What is the MC skin eruption rash caused by drug reactions?
Exanthematous, morbilliform rashes
What type of hypersensitivity reaction is atopic dermatitis?
Type I hypersensitivity
What is the tx for a patient with a drug reaction?
1. Topical steroids
2 antihistamines
3. PO steroids
True/False
Most drug reactions are self limited after d/c of medicine
True
Do you have a patient d/c BP medication or their new brand of insulin for a skin rash caused by a drug reaction?
NO!!
This is the MC panniculitis hypersensitivity reaction due to many etiologies such as infection, drugs and inflammatory diseases. It causes erythematous indurated nodules that appear flat until palpated. Lesions never ulcerate or scar.
Erythema nodosum
(Panniculitis occurs when there is inflammation of subcutaneous fat (the layer of fat lying underneath the skin). The inflammation causes rounded, tender red bumps (nodules) to form just below the skin surface.)

Where is Erythema Nodosum MC located?
B/L anterior lower legs (shins), Asymmetric
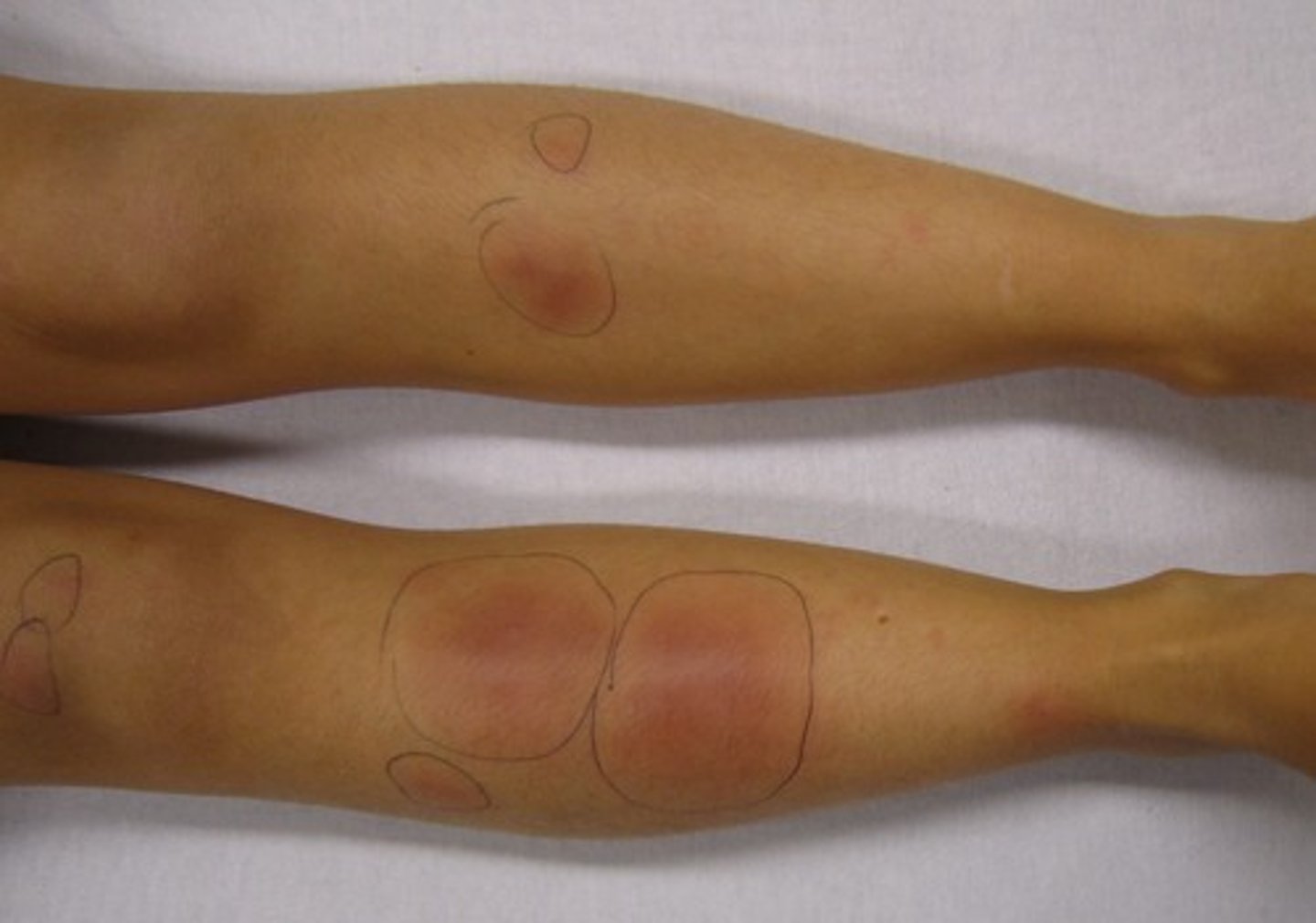
What type of infection can cause Erythema nodosum ?
1. Strep (50%)
2. Coccidiooidmycosis
(HA..weber's coming back to haunt us)
What inflammatory disease can cause Erythema nodosum ?
Sarcoidosis
What labs do you order if you suspect Erythema nodosum ?
How do you confirm dx?
1. ASO titer
2. throat culture
3. ESR
4. chest xray
Confirm= Punch Biopsy
How do you tx Erythema nodosum ?
1. Tx underlying cause
2. Self limiting in 6 weeks
3. NSAIDs (Ibuprofen/ Naproxen)
This is a chronic inflammatory condition with periods of exacerbations and remissions. Usually starts in childhood. Dysfunction of the skin barrier (filaggrin mutation) leading to drying, pruritis and inflammation. Considered a Type I hypersensitivity reaction.
Atopic Dermatitis (Eczema)