NUR4090 Critical care Exam 1 notes
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
Factors that can interfere with pulse oximetry readings
Nail polish
Carbon monoxide (can cause false high reading)
Vasopressor
Shivering
Patient pulls it off
Assessment of the pulmonary system
Assessment of the lung field (auscultation)
Anterior
Posterior [preferred]
Work of breathing (visual inspection)
Rate and rhythm [tachypnea]
Accessory musculature
Level of consciousness
RASS score, make sure level of sedation matches score
Patients requiring artificial ventilation
*common medications used for rest/agitation and decreased WOB (work of breathing)
Intravenous Medications that are common in the ICU for sedation/pain artificial ventilation in place
Propofol (Diprivan)
Precedex (Dexmedetomidine)
Benzo’s
Valium (diazepam)
Ativan (Lorazapam)
midazolam (versed)
Paralytics
Norcurin, Pavulon, Nimbex
Propofol (Diprivan)
sedation and amnesic
Patient needs to be on a vent
Commonly used for sedation (fast acting)
May cause hypotension and bradycardia
If BP goes up pause/stop and monitor
When stabilized, notify provider
Oversedation (can stick around)
Metabolized in the liver, high fat emolument intravenous tubing changed every 12 hours
High likelihood of infection
Precedex (Dexmedetomidine)
Preferred by providers
Works very well with alcoholics
Reverses faster
Decreased chance of delirium
Bradycardia and hypotension
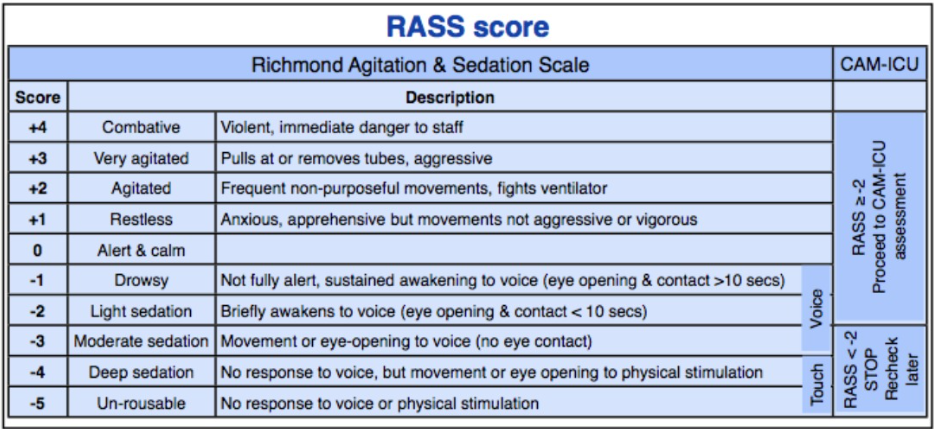
RASS Score - Richmond Agitation Sedation Scale
A 10 point scale used to assess a patient’s level of agitation and sedation
Positive score (+1 to +4): indicates increasing aggression
+4 combative: overly violent and danger to staff
+3 very agitated: pulls at tubes or is aggressive towards staff
+2 agitated: frequent non-purposful movements, may fight the ventilator
+1 restless: anxious and apprehensive but not aggressive
Zero score: patient is alert and calm
Negative score (-1 to -5): indicates increasing sedation
-1 drowsy: not fully alert but can maintain eye contact for over 10 seconds when addressed
-2 light sedation: briefly awakens with eye contact for less than 10 seconds when addressed
-3 moderate sedation: movement or eye opening to voice but without eye contact
-4 deep sedation: no response to voice but there is movement or eye opening to physical stimuli
-5 unarousable: no response to any verbal or physical stimulation
If provider ordered -2 and it is not enough/goes away quick, contact provider for different order or additional meds
Your order must match the sedation score
Benzo’s
Valium (diazepam)
Alcohol detoxification
Hypotension oversedation
Romazicon (Flumazenil)
Ativan (Lorazapam)
Fat pink needle (18g) bc very thick
Seizure control
Hypotension, respiratory depression
Midazolam (Versed)
Short acting
Hypotension, respiratory depression
Reversal agent for benzos: romazicon
Reversal agent for opioids: narcan, may need narcan drip
Know the half life of medications, narcan may be out of system before opioids are therefore may need narcan drip
Paralytics
Norcuron, Pavulon, Nimbex (more)
The client MUST BE ON A VENTILATOR
MUST BE on continuous IV sedation
Initiated before and continued after until paralytic is cleared
Monitored with Train of Four
Provider ordered level of response follow your hospital policy
Usually two or one out of four. Document every hour
Anatomy of the Lungs
Warmth, air and oxygen exchange
Upper respiratory tract: filters impurities and warms the air
Lower respiratory tract: lungs, 3 lobes on the right, 2 lobes on the left. Right lung is more likely to be intubated by mistake (straight path)
Straight path
Pleura: Visceral: vital (closest to lung); parietal lines pleural cavity
Respiration and Ventilation
What is the difference?
Respiration is the whole process of gas exchange between the atmosphere and the blood including the cellular exchange of O2 and CO2
Ventilation is the movement of air in and out of the lungs. Inspiration is active, expiration is passive
Too much sedation can cause issues (diaphragm issues)
Blunt chest trauma
More common, more difficult to treat, vague symptoms so may not seek treatment immediately
Sternal/rib fracture: most of the time we address pain only, there is not much we can do
Flail chest: 3 or more continuous ribs having 2 or more fractures causing a floating space
Opposite movement can be fatal
Need binder
Encourage deep breathing
Gentle chest PT
Pulmonary contusion: chest PT, antibiotics
Penetrating chest trauma
Gunshot/stab wound
Pneumothorax
Need chest tube
Only 2 reasons to clamp
Turn off to remove
When container is full/needs to be changed
No stripping to move clots down (can damage tools)
Tension pneumothorax, tracheal deviation to undamaged side
Dangerous bc it can compress the heart
Cardiac tamponade
Layer around heart punctured and starts filling with fluid
Beck’s triad: JVD, muffled heart sounds, hypotension
Need to decompress, take a needle to pull out fluid
Subcutaneous emphysema
Tracheostomy
Life threatening Injuries
Hypoxemia: low O2
Hypovolemia: low blood volume
Cardiac failure
Chest trauma: Assessment
Time is critical
Mechanism of injury
How serious the injury is (baseball vs car accident)
Responsiveness
Specific injuries
Estimated blood loss
Recent alcohol use
Pre-hospital treatment
Anything they did in the field
Diagnostics
Chest Trauma: Management
Airway
Chest tube:
continuous bubbling means leak or other issue, intermittent bubbling is normal
Keep on floor, below heart level
Keep tubes away from side rails
Record drainage
No stripping
Never clamp, especially when suction
Only clamp when changing receptacle or pulling out
Turn off suction first then clamp
Need for O2
Reestablish fluid volume
Reestablish negative pressure
Drainage of intrapleural fluid/blood
Pulmonary embolism
Obstruction of the pulmonary artery or one of its branches by a thrombus
Originates in the venous system
DVT
DVT + PE = VTE
Associated with:
Trauma
Surgery
Pregnancy
Heart failure
Age (>50)
Hypercoagulable states
Prolonged immobility
Atrial fibrillation
Birth control pills
Clotting disorder
PE: Pathophysiology
Can be a complete blockage of the pulmonary vasculature or a partial blockage
A DEAD space issue ventilation continues
Right heart strain
Varying degrees of hemodynamic instability depending on the size
PE: Clinical manifestations
Size dependent
Dyspnea, tachypnea (most common side effect)
Chest pain
Cough, hemoptysis (secondary to cell death)
Anxiety, apprehension
Fever, tachycardia, diaphoresis
PE: tests
Diagnostic tests: a spiral CAT scan with contrast dye
Contrast dye can cause an allergic reaction
Other test:
VQ (ventilation perfusion) scan is not as precise but may be considered when patients have an allergy to contrast dye or are pregnant. It requires a chemical tracer, which carries a slight chance of a minor reaction and passes quickly without intervention
Radioactive compounds inhaled into airspaces of lungs, in a normal lung this will distribute evenly to all regions
Radioactive compound injected into vein. Travels to lung tissues in blood vessels
“Mismatch” of inhaled and injected compounds on the lung scan images = pulmonary embolus
CXR, EKG, pulmonary angiogram, D-Dimer
Arterial blood gas/pulse oximetry
PE: Medical treatment and nursing care
TPA (clot buster)/heparin therapy
coordinate blood draws to minimize bleeding
Heparin antidote: protimine sulfate
Prevent new clots from forming
Anticoagulant therapy
Thrombolytics
Ambulation, let exercises in bed
Make sure they don’t dangle their feet, have feet planted on floor (blood return)
Using the pulse oximetry for monitoring
Prevent bleeding after TPA therapy
Prevention: assessment, ambulation, SCD (sickle cell), adopt a healthy lifestyle, quit smoking, oral anticoagulants
Anti X antibody [ASSAY]: new more accurate than PTT
PE: Prevention (DVT/VTE)
AVOID VENOUS STASIS
Activity/leg exercise
Early mobilization
Anti embolic stockings
Sequential compression devices
Anticoagulant therapy
Medication interactions
Leafy greens, need to be consistent especially if on coumadin
Greenfield filter
Helps catch clots and prevent it from traveling to brain or lungs
Prevents pulmonary embolism or stroke
Acute respiratory failure
Sudden and life threatening
Decline in gas exchange
Failure to provide oxygenation
pH < 7.35
PaO2 < 60mmHg (hypoxemia)
PaCO2 > 50mmHg (hypercapnia)
Lung failure vs Pump failure
Lung failure: gas exchange failure manifested by hypoxaemia (low O2 in blood)
Pump failure: ventilatory failure manifested by hypercapnia (high CO2 in blood)
ARF: Assessment
Early: restlessness, fatigue, headache, dyspnea, tachycardia, hypertension, hypoxemia
Progression: confusion, lethargy, tachycardia, tachypnea, central cyanosis, diaphoresis, respiratory arrest
ARF: Management/Treatment
Correct underlying causes
Restore gas exchange in the lungs
Intubation/mechanical ventilation
ABG
Will be taken everyday
SaO2
VS
ICU care
ARF: Nursing Management
Assist with intubation
Watch pulse Ox to notify provider at around 92-90
Have suction (yankour) ready if need to clear patients oropharyngeal area
Respiratory therapist should have capnography tester on the end of the bag valve mask and give a couple of amboos, if they see color change that means there is CO2 which is a pretty good indicator of placement
3 point check: listen to right lung, left lung and stomach while ambooing
CXR for confirmation, recommend feeding tube before
Maintain mechanical ventilation
Assess respiratory status:
LOC, ABG, VS, respiratory system
Care of the vented patients
The ventilator bundle
HOB 30-45 degrees
Sedation vacation
GI prophylaxis
DVT prophylaxis Heparin [SC]
Oral care, chlorhexidine
High pressure alarm: secretion or biting tube
Low pressure alarm: not weaning well, circuit error
Communication and education (for family and patients)
Chronic respiratory failure
Deterioration in the gas exchange function
Hypoxemia and hypercapnia develops gradually and is harmful
Persisted for a long period of time after an episode of acute respiratory failure
Absence of acute symptoms
COPD and neuromuscular disease
Arterial Blood Gas
Normal pH: 7.35-7.45
Normal PCO2: 35-45
Normal PAO2: 80-100
COPD patients may be extubated under 80 (around 70s)
Normal Bicarbonate: 22-26
The lungs work much faster than the kidney
Oxygenation is not part of the blood gas pH analysis but is just as important
Metabolic acid base abnormalities
Metabolic Alkalosis
Causes: vomiting, excessive antacid use, contraction alkalosis
Metabolic Acidosis
Causes: any condition that causes a reduction in bicarbonate or in which the body’s metabolic processes outpace bicarbonate production
Kidney disease, DKA, Sepsis, lactic acidosis, aspirin overdose
Respiratory acid base abnormalities
Respiratory Alkalosis
Causes: hyperventilation
Respiratory Acidosis
Causes: respiratory failure, hypoventilation syndrome
Acute respiratory distress syndrome (ARDS)
Severe form of acute lung injury
Severe inflammatory process
Associated with lung trauma
PaFIO2 ratio test: ABG oxygen level/oxygen given by ventilator (convert % to decimal)
300-500: normal
<300: acute lung injury, mild ARDS
<200: moderate ARDS
<100: severe ARDS
Sudden and progressive pulmonary edema
Bilateral infiltrates on chest x-ray
Can look like CHF
Do BNP (brain natriuretic peptide) blood test, if positive then its CHF, if zero its ARDS
Hypoxemia unresponsive to oxygen
Regardless of the amount of PEEP
Bronchial trauma
Reduced lung compliance
Death from non pulmonary multisystem organ failure, with sepsis
Spectrum of disease
pulmonary edema —> acute lung injury —> ARDS
severity is based on the damage of the alveolar membrane which leads to pulmonary fibrosis, vascular destruction, and MODS (multi organ dysfunction syndrome)
Stages of ARDS
The acute exudative phase (about 1 week)
Injury
Pretentious flooding nullifies surfactant
Decreased gas exchange
Proliferative phase (Up to 3 weeks)
Resolution of phase one/may recover or move to next phase
Normal lung tissue changes into fibrotic tissue
Ventilator dependent/death is common
Usually resulting in sepsis, overwhelming infection, and MODS
Factors Commonly associated with the Development of ARDS
40% mortality rate
Direct lung injury
Pneumonia
Aspiration of gastric contents
Pulmonary contusion
Near drowning
Toxic inhalation injury
Indirect lung injury
Sepsis
Severe trauma
Multiple bone fractures
Flail chest
Head trauma
Burns multiple transfusion
Drug overdose
Pancreatitis
Post cardiopulmonary bypass
ARDS Pathophysiology
Inflammation
Injury to the alveolar capillary membrane
Severe ventilation - perfusion mismatch occurs
Alveolar collapse
Lung compliance decreased (the ability the lungs can stretch)
Loss of surfactant
ARDS: Clinical manifestations
Resembles severe pulmonary edema
Rapid onset dyspnea
Less than 72 hours after the precipitating event
Arterial hypoxemia (manifests)
Visible bilateral infiltrates (xray)
Decreased pulmonary compliance: stiff
Recovery: oxygenation and CXR improve, better lung compliance
ARDS: Assessment
Develops over 48-72 hours
Crackles
Rapid onset dyspnea
Arterial hypoxemia: refractory to oxygen therapy
White patches on CXR
Pulmonary Edema or ARDS
Brain natriuretic peptide (BNP)
ARDS: Management
Intubate/Mechanical Ventilation
PEEP to improve oxygenation
Low tidal volumes (bc alveoli are filled with fluid)
Vasopressor therapy
Fluid volume
Nutrition
Pharmacology
Sedatives, analgesics, neuromuscular blockage, inhaled nitric oxide heliox
Specialty bed/pronation
ECMO therapy
Used in severe cases of ARDS/COVID 19/Sepsis
Open heart surgery
VV mode (venus system)
General for lungs
VA mode (arterial system and venous)
For lungs and heart
Multiple additional sub settings
Gas exchange machine
Decannulation
Clots
Infection
Fluid compromise/ must have anticoagulation
Applies in every case where blood is taken outside the body
Oxygen
Room air is 21% oxygen
Oxygen is a drug
Obtain an order for the least amount of oxygen to stabilize the patient
Each L of O2 SpO2 goes up about 4%
Many devices are used
Be careful when giving oxygen to COPD patients
Oxygen toxicity
40 is the goal
Should not be weaning anyone over 40% oxygen
Emergency airway management
Upper airway obstruction has multiple causes
Food, vomitus, angioedema (swelling of throat, typically caused by anaphylaxis or medication i.e. ace inhibitors), altered LOC, loss of tone (pharyngeal muscle, tongue) post stroke
Vomiting, place the HOB up to a high Fowlers, turn the patient’s to the side, and suction out the mouth with a rigid catheter (aka Yankhower)
Airway management devices: Advanced airways
Oral airway
Nasal airway
Laryngeal mask airway (LMA)
Done in field, not done in ICU (not common)
Tracheostomy
Reserved for those who have been intubated (ETT) for more than 2-3 weeks
Endotracheal tube (ETT)
Mechanical ventilation
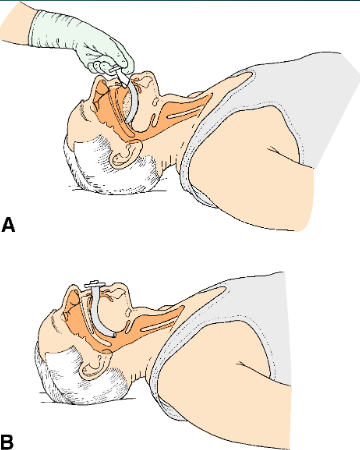
Oral airway
(often used with unconscious patients)
Need to be very careful with oral cleaning, be aware of placement and proper cleaning to prevent VAP (ventilation acquired pneumonia)
Sized from mouth to corner of jaw
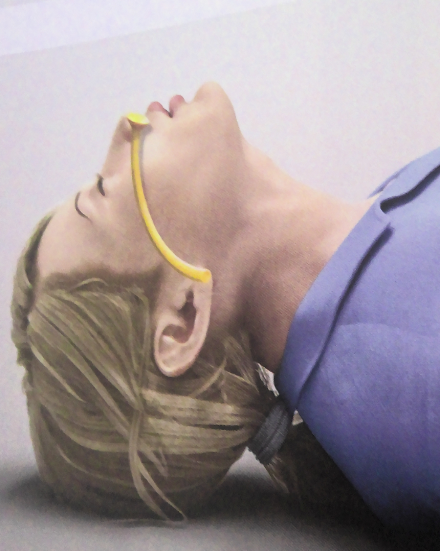
Nasal airway
Sized from nose to earlobe
Goes in bevel facing septum
Clean as ordered, can remove to wash and replace
Endotracheal tube (ETT)
Is an issue if patient removes newly placed tube, need to get help and inform physician to replace/see if there was any damage done
If established tube pops out can clean with sterile water/saline and replace, need to notify physician
Note diameter of tube (9/10 7 or 7.5 size, depending on size of patient)
Usually is 20-21 sonometers
Nutrition
Want to get dietitian involved, need calories
Need to adjust feed to accommodate for comorbidities/existing conditions (i.e. diabetes)
Recommend placing NG tube as well
Only require 1 CXR, pt is still sedated
Have physician change order/contact pharmacy for oral to NG meds if needed
Cough reflex suppressed
Family education, cannot eat or drink
Need to figure out a form of communication
Lavage sparingly
Suction as needed, excessive suction can cause more secretions

Ventilator bundle
GI prophylaxis
DVT prophylaxis
raise HOB to 30-45 degrees
oral care, chlorohexidine
sedation vacation, let them relax
Ventilator management
Oxygen is a drug use as little as possible
Above 50% can lead to oxygen toxicity
PEEP can be used as additional therapy. Using PEEP decreases venous return to the heart
Can help need less oxygen
Sedation is used to decrease WOB, BMR and agitation
Match to RASS score
Alarms
High: will go off with cough, biting tube, thick secretions/plugs, drop a lung
Low: usually on weaning trial, not exhaling enough, something has disconnected
Ventilator bundle
Endotracheal intubation
Placement of a tube (usually orally)
To provide a patent airway for mechanical ventilation
Removal of secretions
Inserted by the provider or a respiratory therapist
Nurses gather the proper equipment
Sedation
Monitor pulse oximetry.
Three point check: right lung, left lung and stomach (if stomach is getting bigger, might be in the wrong place)
Capnography, Xray
Advanced Airway: Risk Benefit - Advantages
Patent airway
Mechanical ventilation
Need to be sedated
Suctioning
Decreased work of breathing
Improved oxygenation
Rest muscles
Goal is <50% oxygenation
Advanced Airway: Risk Benefit - Disadvantages
Discomfort
Cough and swallowing reflex are depressed
Secretions become thicker
Increased risk of aspiration
Ventilator associated pneumonia (VAP)
Tracheostomy
Bypass the upper airway (obstruction)
Bypasses dead space
Allow removal of secretions
Permit long-term mechanical ventilation
Limited aspiration of oral secretions
To replace an endotracheal tube
Less complications
More comfortable
Types
Cuffless: lot of secretions, long term
Cuffed
Fenestrated: can eat and drink, maybe speak
Surgical procedure
Ventilation can be well controlled
Can be done in ICU, if complicated move to OR
Indwelling tube inserted into the trachea
Tracheostomy
Temporary or permanent
Secured by ties around the patients neck
Check back for fungal rash
Tracheostomy: Complications
Bleeding, pneumothorax, aspiration, subcutaneous or mediastinal emphysema, laryngeal nerve damage, posterior tracheal wall penetration
False passage
Medical emergency if patient pulls out tube within 10 days of operation
Tracheostomy: Long term complications
Airway obstruction infection, rupture of the innominate artery, dysphagia, fistula formation, tracheal dilation, and tracheal ischemia and necrosis
Inner cannula needs to be changed once a shift
Tracheostomy: Nursing Management
Requires continuous monitoring and assessment
Especially in the beginning
Comes with rigid operator, used to help with placement need to be placed in a biohazard bag with pt name and taped to wall
Have access to 10cc syringe in case need to add some air
Have bag valve mask in room (amboo)
Early interventions
Proper suctioning trach care once a shift, change/clean inner cannula
HOB at 30 degrees
Analgesia, sedatives
Extra trach at bedside, rigid obturator in plastic bag secured over client’s head
With name on it
Administer O2 and humidified warm air
Maintain cuff pressure
Suction
Maintain skin integrity around tracheostomy
Auscultate lung sounds
Monitor for infection
Use sterile technique when suctioning, teach care
Change inner cannula at least once every shift
Keep the tracheostomy ties snug
Mechanical ventilation
Oxygenate the blood for patient with poor ventilation
Control respirations during surgery (sedated, paralyzed)
Rest respiratory muscles
Indications
Decreased PaO2
Increased PaCO2
Persistent acidosis
Treat respiratory failure
Compromised airway
Classification of Ventilation (machine)
[works by volume or pressure or combination of]
Negative pressure [iron lung]
Positive pressure
Volume cycled, pressure cycled, flow cycle, time cycled
Non invasive
External: BiPAP, CPAP
BiPAP good for COPD, works on 2 levels, O2 and CO2
Modes (how the machine will ventilate)
Assist control (AC): complete/total ventilative support
Intermittent Mandatory Ventilation (IMV)
Stacking of breaths, bad not allowing breaths in between
Synchronous (SIMV)
Machine will hold off if senses breath in between
Doesn’t stack
Contrast positive airway pressure (CPAP)
Better for blowing off CO2
Pressure support (PS)
Weaning modality/used for extubating
Used with CPAP to take people off vent
Mechanical Ventilation Overview
Ventilator settings (prescriber orders)
Mode (AC, CPAP)
Respiratory rate (RR)
Tidal volume (TV or Vt)
PCV uses pressure
Fractional inspired oxygen (FiO2)
Positive-end expiratory pressure (PEEP)
Used to give less O2 (as little as possible)
Negative pressure ventilator
Exert negative pressure on the external chest
“Pulls” at lungs/chest wall
“Iron lung”
Chest cuirass
Positive pressure ventilators
Most common
Exerts positive pressure on the airway (push air in)
Force alveoli to expand during inspiration
Expiration occurs passively
Advanced airway required (ETT, Trach)
Classified by the method of ending the inspiratory phase of respiration
Volume cycled, pressure cycled, high frequency cycled
Noninvasive positive pressure ventilation (mask)
BiPAP (non-invasive)
treats CO2 and O2 levels
Prone to skin breakdown
Need skin protection for bridge of nose and forehead
Do not restrain hands, if patient vomits they need to be able to pull it off
Volume Cycled Ventilation mode
Most common
Volume of air is preset
Volume is relatively constant
395-400
Once the volume is delivered, the inspiration stops
High Frequency Oscillatory Ventilator
[needs to be sedated and paralyzed, for ARDS]
Very high respiratory rate
180-900 breaths/minute
Very low tidal volume
Need CO2 monitoring
High airway pressure
Small pulses of oxygen enriched air
Open the alveoli
Atelectasis, ARDS
Lung protective
From pressure injury
Noninvasive Positive Pressure Ventilation (NIPPV)
Use of face mask or other devices to maintain a seal and permit ventilation
Indications
Respiratory failure
Pulmonary edema
COPD
Sleep related disorder
Continuous positive airway pressure (CPAP)
O2 and airway issue
Bi-Level positive airway pressure (BiPAP)
Inspiration and exhalation pressure
CO2 removal
O2 administration
Ventilator Modes
How breaths are delivered:
Assist control (AC) sometimes called CMV
Synchronized intermittent mandatory ventilation (SIMV)
Gets O2 and PEEP but only gets tidal volume when they pull
Pressure control ventilation
Preset pressure and kick off
Constant Positive Airway Pressure (CPAP)
Can be used on mask and vent
Pressure support (PS)
Used together with CPAP
Offsets narrow diameter of endotracheal tube
Positive End expiratory pressure (PEEP)
AC (assist controlled)
Also known as Controlled mandatory ventilation (CMV)
Provides full ventilator support
Preset tidal volume, RR
If patient initiates a breath before the preset rate, the ventilator will deliver the preset volume and “assist” the breath
Every breath (machine or patient) will receive the preset volume
SIMV (Synchronized Intermittent Mandatory Ventilation)
Machine delivers a preset tidal volume and rate
Spontaneous breaths can occur
Between machine breaths the patient can determine own tidal volume, no assist
Senses breath and holds back
Machine senses the patient breath and will not initiate a machine breath in opposition of the patient breath (synchronized)
“Bucking the vent” is decreased
Pressure Controlled Ventilation mode PCV
Delivers inspiration until it reaches a preset pressure then kicks off
Major limitations
Volume delivered is varied (tidal volume)
Volume delivered depends on patient’s airway resistance and compliance
Alterations in tidal volume can compromise ventilation
Pressure Support Ventilation (PSV)
[weaning mode]
Machine applies a pressure to the airway throughout the patient triggered breath
Decreased resistance in the ETT and machine tubing
Decreased work of breathing for the patient
Offsets pressure of narrow tube (feeling)
PS is reduced as patient’s strength increases
PEEP
Positive end expiratory pressure
Pushes air in
Positive pressure maintained by the ventilator at the end of expiration
Increase functional residual capacity
Opens collapsed alveoli
Improves oxygenation and allows for lower FiO2%
Can be used in liu of O2
Complications: decreased venous return to the heart and barrow trauma and danger of pneumothorax
CPAP
Continuous positive airway pressure
Positive pressure applied throughout the respiratory cycle to a spontaneously breathing patient
Can decrease need for oxygen therapy
Administered via ETT, trach, or external mask
Patient must breathe spontaneously
This can be a weaning mode (invasive) or a therapy (non-invasive)
Mechanical Ventilation: Care of Patients
Assessment of the patient
In depth respiratory assessment including all indicator of oxygenation status
Comfort
Bundle
Turning and positioning
Coping, emotional needs
Communication
Yes or no questions, alphabet board, writing, etc.
Mechanical Ventilation: Ventilator settings
Initial ventilator settings are determined by the provider and set by the respiratory therapist
Set tidal volume
Set rate (12-16 bpm)
Set oxygen level
Set mode (AC)
Set PEEP (5-15cm H2O)
Mechanical Ventilation: Goals
Optimal gas exchange
Attainment of optimal mobility
Absence of trauma or infection
Adjustment to nonverbal methods of communication
Alphabet board
blinking/pointing
Mechanical Ventilation: Exchanging Gas Exchange
Monitoring ABGs and SPO2
Do not suction right before ABG
Auscultate lung sounds posteriorly
Back side first
Judicious use of analgesics use RASS parameters
Monitor fluid balance
I&O: either zero or slightly negative (more output than input)
Promoting effective airway clearance
Assess lung sounds every 4hrs
Measure to clear airway
Suctioning, CPT, position changes, promoting early mobility
Humidification (HME)
Medication’s sedatives, pain control, antibiotics
Optional mobility
Physical deconditioning and prolonged motor weakness accompanying critical illness have profound and lasting consequences
Early mobility is facilitated by change in intensive care unit culture
Preventing Trauma
Ventilator Associated Pneumonia (VAP)
Daily interruption of sedation
Daily readiness to extubate
DVT and PUD (peptic ulcer disease) prophylaxis
Daily oral care with Chlorhexidine
Every 4hrs and PRN oral care
Elevation of HOB about 30 degrees
Hand washing protocol
Weaning
Process of gradual withdrawal from dependence upon the ventilator
Successful weaning is a collaborative process (between nurse, PT, provider)
Criteria for weaning
Patient preparation
Methods of weaning
CPAP trial (1hr)
Make sure they are able to maintain their airway
Extubation requirement RR <30, tidal volume >300
Rest (few days)
Ambulation
Lower O2 concentration
Monitor SpO2
Do ABGs
Rapid shallow breathing index, low number is good (<105)
PaFIO2 ratio: low is bad
Extubation
Extubation is described as the discontinuation of an artificial airway
Indication for its original placement no longer exists
Extubation Criteria
Guidelines of adequate pulmonary mechanical function includes
A successful weaning trial minimum 30 min
Rapid shallow breathing index less than 105
Normal ABG for that patient
Awake alert and able to support their own airway
Afebrile, minimal secretions
Chronic ventilation
When continuous mechanical ventilation is required
Conditions such as stroke and spinal cord injury
Chronic stable illnesses, such as neuromuscular disorders and chest wall deformities, and/or advanced age
Chronic illness that requires recurrent ICU hospitalization
May require frequent repeated treatments with mechanical ventilation and repeated attempts to wean from mechanical ventilation
Terminal Wean
Palliative wean
Need to explain to family that dropping stats is normal, can be a difficult situation
The removal of ongoing ventilator support is a necessary evil when these devices are hindrances to ending life rather than sustaining a manageable quality of life for a patient
Patient wishes
Pain free and free of respiratory distresses
Make sure they are not air hungry
Make sure they are comfortable
Hospice care and Palliative care
All hospice care is palliative care
Not all palliative care is hospice care
Palliative care focuses on symptom management in serious illness and can last for prolonged time
Hospice care is an option when death is expected within 6 months
Psychosocial and Regulatory issues
Methods of stating end-of-life preferences
Advanced directives (enshrined by law)
DNR
Medical durable power of attorney/ Health care proxy/ Living Will
Patient has to be incapacitated to take effect
Will see health care proxy most often
POLST/ MOLST (in NYS it’s a MOLST)
Goes into effect as soon as it is signed by physician
Travels with patient to every facility
Signing as a witness for informed consent
Cultural awareness
Autonomy, double affect and coercion
Autonomy: patient has right to make their own medical decision s
Double affect: an action caused unintended consequence detrimental to patient life
Coercion: comes off as a “threat”
Communication
Confronting death is emotionally difficult
Poor communication is the #1 problem vocalized by families
Skill development
Families and clients often have an impossible choice to make
Therapeutic and non-therapeutic communication
Therapeutic: active listening
Non therapeutic: false reassurances
Spiritual care fostering hope
Spirituality (may or may not contain elements of religion)
Religion
Spiritual assessment is on your nursing assessment
Hope fostering categories
Love of family and friends; faith; setting goals; staying independent; positive relationships with clinicians; humor; uplifting memories; personal characteristics
Hope hindering categories
Abandonment, isolation, uncontrolled pain/discomfort, devaluation of personhood
Managing Physiologic Responses to Terminal Illness
Pain
Is preventable or treatable
Assess pain using facility’s pain scale tools
Use smallest dose possible to alleviate symptoms
Inability to communicate pain should not be mistaken for lack of pain, neither should be sleeping
Helpful medications in managing terminal illness
Opioids (can be given SL, oral, or PR)
Morphine sulfate (oral Roxinol)
Decreased air hunger (sensation of being SOB)
Lowers pain
Lowers BP and may depress respirations
GI motility, Establish bowel regime
Colase or laxatives (to keep them regulated/ address constipation)
Reversal agent: Narcan (Nalaxone)
Benzodiazepines
Ativan, Xanax
Anxiety can increase WOB
Reversal agent: Romazicon (Flumazenil)
Physiological responses to terminal illness
Dyspnea is the uncomfortable awareness of breathing and is very prevalent at end of life
Feeling of can’t get enough air
NOT necessarily associated with tachypnea, diaphoresis or cyanosis
Assess by patient report using a scale of 0-10
Manage anxiety
Low flow O2, movement of air (fan), low dose opioids
1/2L to 1L of O2
Reduce demand, energy conservation
Cluster care for less strain
Impaired secretions at the end of life
Reassure the family that increased secretions are normal at end of life
Educate the family on how to differentiate increased secretions from dyspnea
Medication for secretions (oral)
Atropine PO or SL
Glycopyrrolate
Hyoscyamine
Scopolamine patch
Depression
Depression should not be ignored
Depression can be treated with medications, but therapeutic blood levels often take time to achieve the desired results
Delirium and Depression
A disturbance in consciousness, attention, awareness, and cognitive capacity. It is rapid in its onset and different from dementia
Delirium is often related to underlying treatable condition s
New medication
Impaction
Full bladder
Pain
Sleep deprivation/change of environment
change/disturbance in general [changes in meds, treatment, routine (family visits)]
Grief and mourning and palliative sedation
Unbiased care
Ethical dilemma withdrawing of care
Decision making capacity
Palliative sedation is different from euthanasia