LF264 Lecture 10 - Oral Tolerance
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
What sort of immune response do enteric pathogens induce? How do they do this?
- Cause a local inflammatory response
- Pattern recognition receptors (PRRs), e.g toll-like receptor (TLRs), are important
- Ligation of TLR stimulates release of cytokines/chemokines which attract monocytes (come into tissue are differentiate into macrophages), eosinophils and T cells out of the blood and the release of antimicrobial peptides
--> TH17 will release IL-17 and help with attraction of neutrophils and help to maintain the integrity of the epithelial barrier
- Resident dendritic cells in tissue are also attracted
--> Stimulation of costimulatory molecules on the dendritic cells overcomes their normally relatively unresponsive, 'lazy' state in the gut
--> Leads to activation of T cells and then B cells
--> Also happens within Peyer's patches
How do commensal organisms and enteric pathogens in the gut differ?
- Enteric pathogens induce inflammation
- Commensal organisms do not induce inflammation
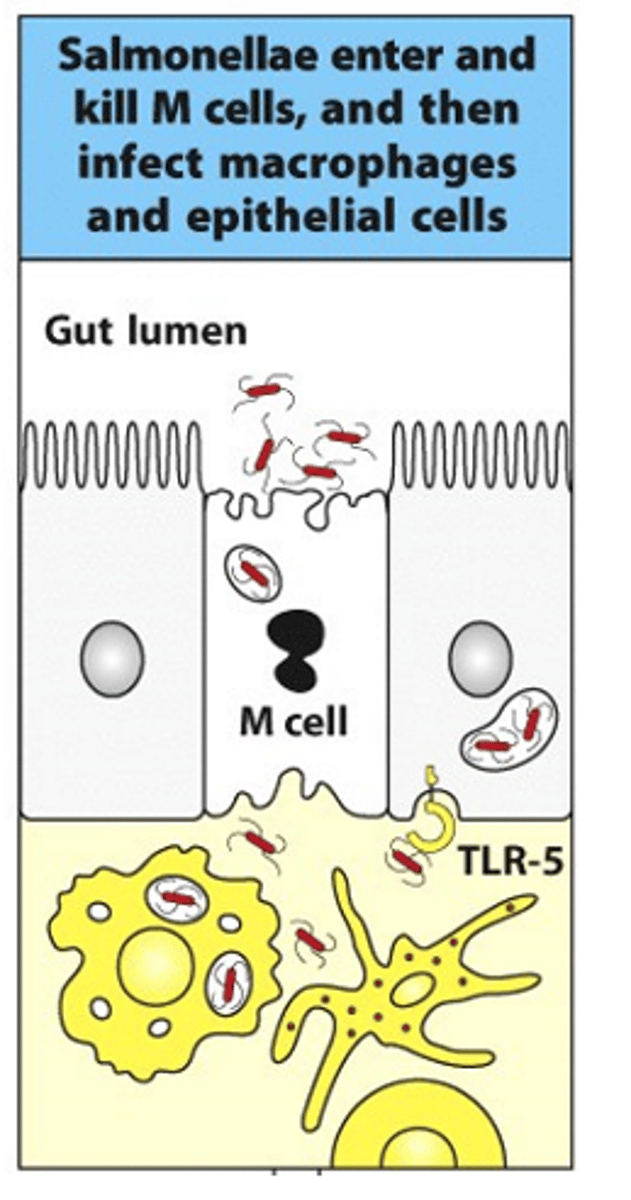
How does Salmonella act in the gut?
- Salmonella targets M cells
- M cells bring antigens/pathogens into underlying tissues
- Salmonella targets M cells and gets brought into the underlying tissues
- Can then infect macrophages and activate them
- Have to go through the process of generating TH1 response that activates macrophages to manage/destroy infection
- Once inside gut, can interact with TLRs on the surface of the epithelial cells and get ingested into macrophages to produce an established infection
What must the mucosal response to infection be?
- Major role of mucosal immmunity = to protect against a huge variety of enteric pathogens
- Response must be able to recognise and respond to any pathogen, but must not produce same response to harmless antigens (e.g food) or commensal organisms
- Mucosal immune response has to balance these competing demands
What are the majority of antigens found in the GI tract?
- Majority of antigens are either from food or commensal organisms
What is oral tolerance?
- Food/commensal organisms do not raise an immune response
- This is called oral tolerance
What can we try and do with oral tolerance?
- Can try to harness it to treat autoimmune diseases, e.g allergy
- Tried to do it with people allergic to peanuts but doesn't work very well
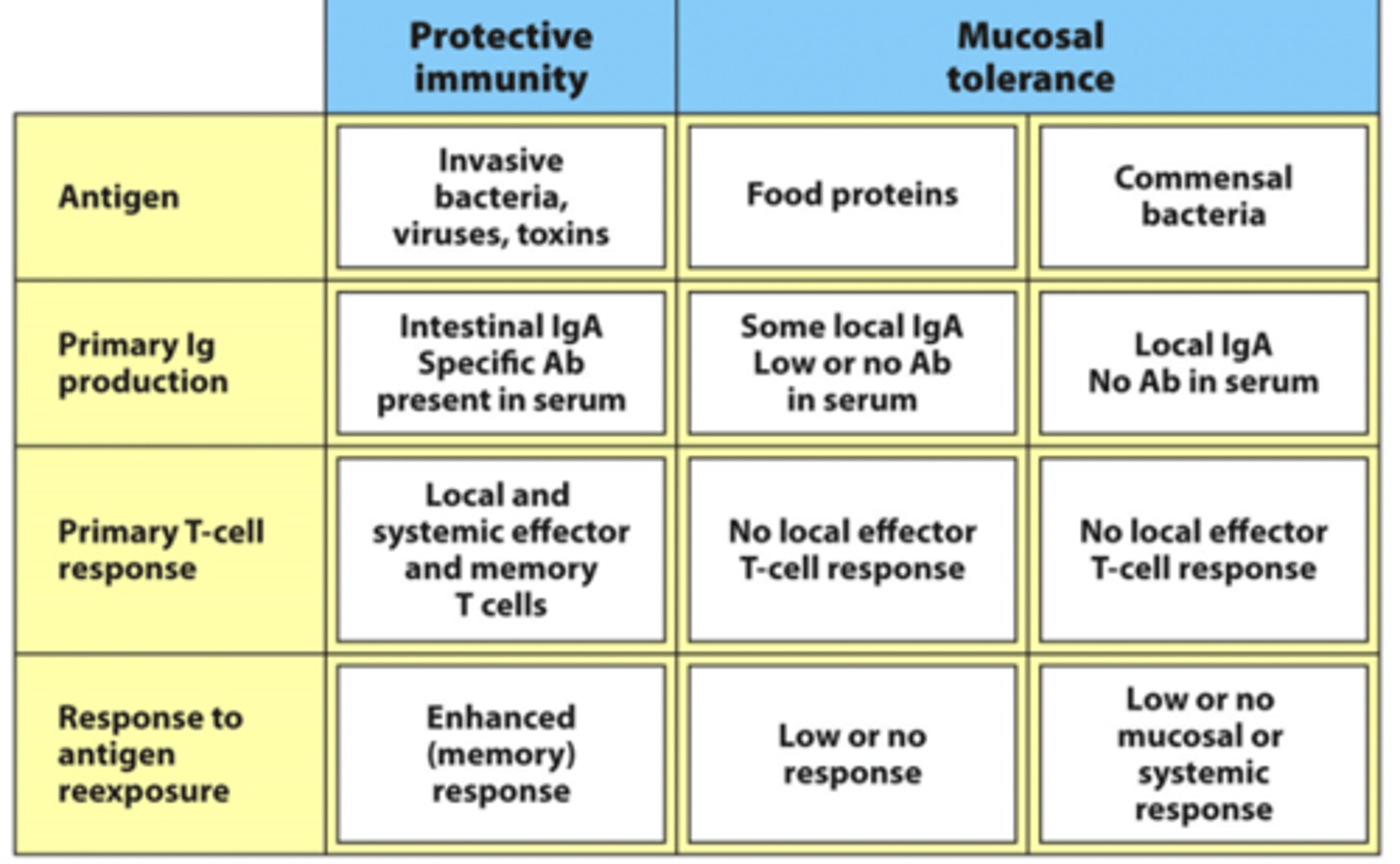
What is balanced in the mucosal immune system?
- Protective immunity
- Mucosal tolerance
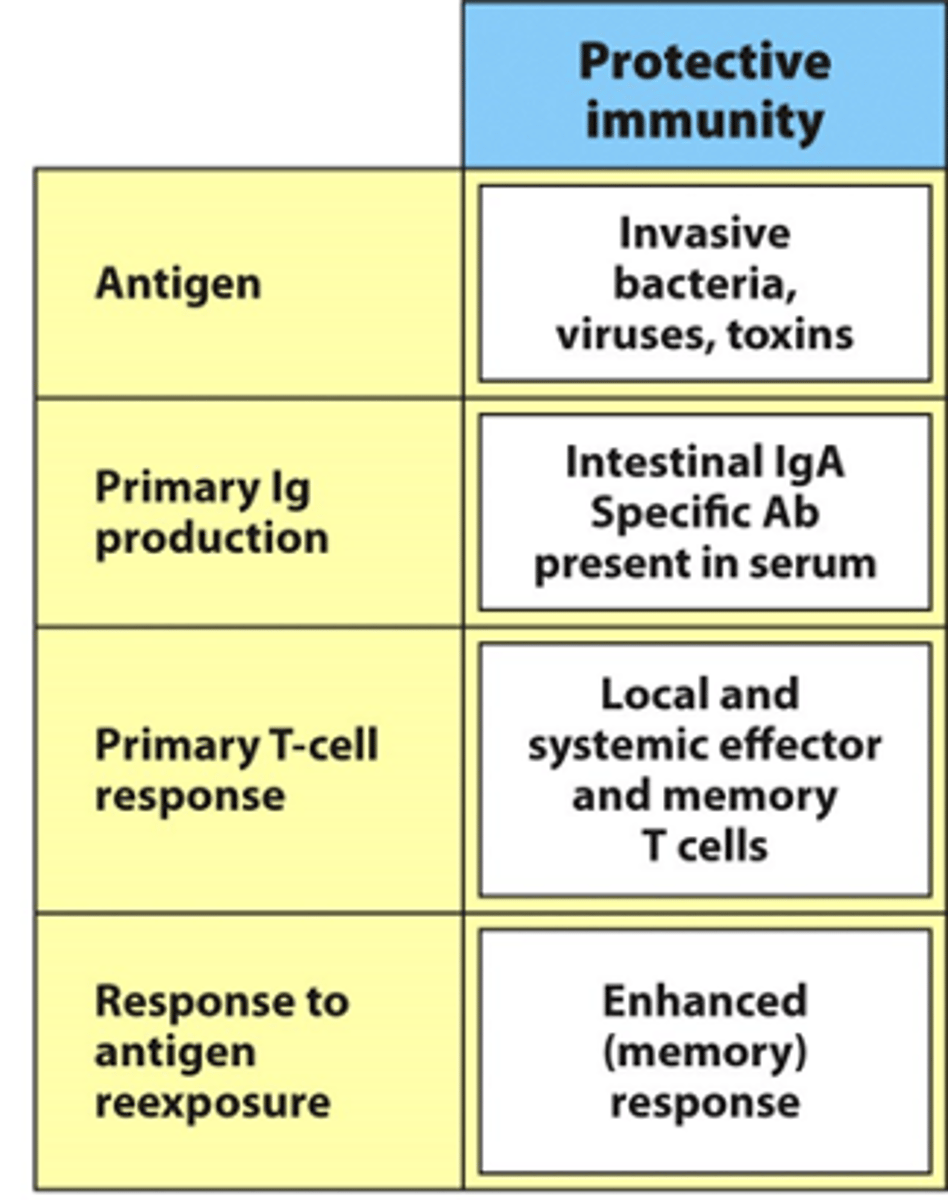
What is the protective immunity in the gut in response to? Describe the antibody production here and the T cell response
- Protective immunity = from invasive bacteria/viruses/toxin
--> Invasive as they need to 'muscle' their way in through the commensal organisms
- Produce IgA in response to this
--> If we generate really good protective immunity in the mucosa, we want to protect the mucosal surface and provide more systemic immune response too
--> Want to make sure antibodies can be present in serum too so also make lots of IgG for in the serum (systemic protection)
- Primary T cell is quite local and systemic
--> Includes memory cells so enhanced, quicker response next time
What is the mucosal tolerance in the gut in response to? Describe the antibody production here and the T cell response
- Mucosal tolerance = from food proteins and commensal bacteria
- Very local/low levels of IgA here to keep these antigens in check
- IgA will still bind to/target commensal organisms
--> Ties them up in big complexes to prevent them from coming in and causing an immune response
- No local effector T cell response
- Low/no mucosal/systemic response to these antigens
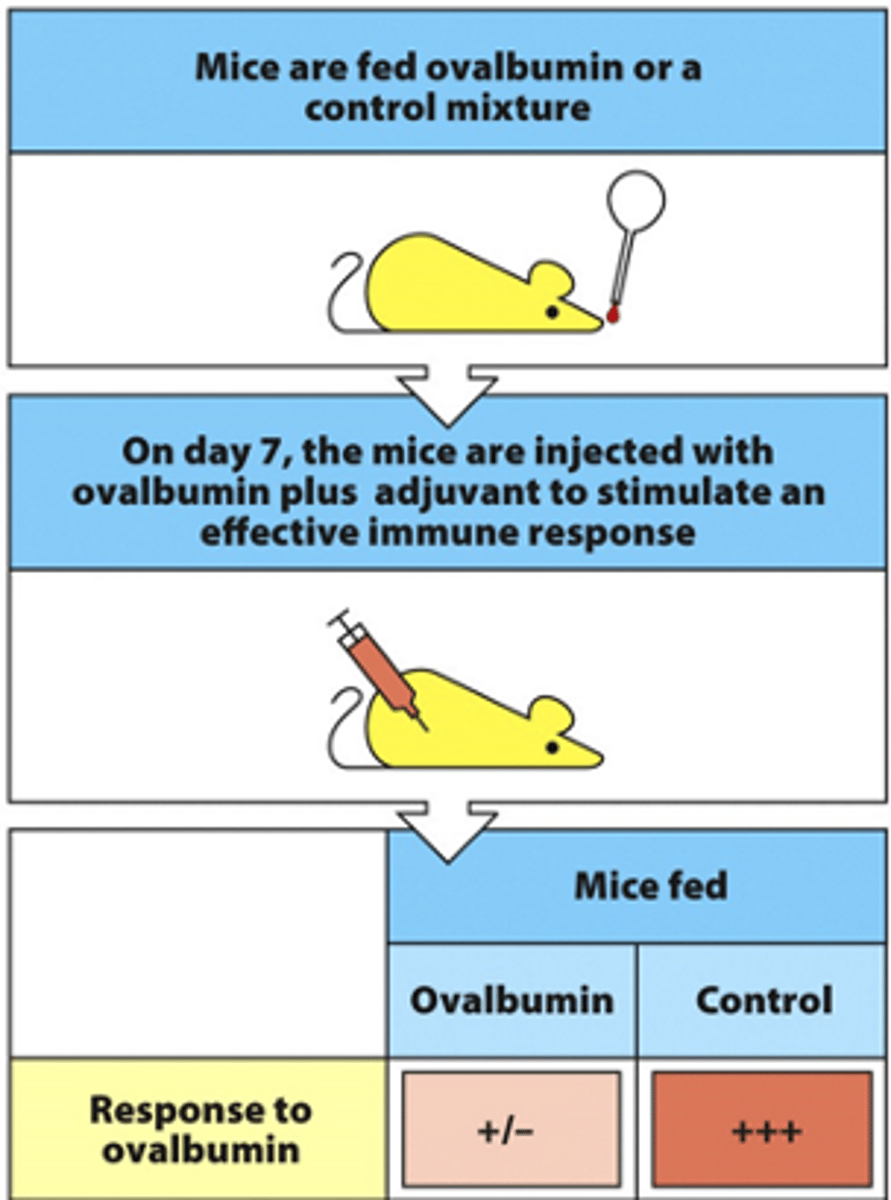
Describe how oral tolerance was demonstrated in mice
- Tester group of mcie are fed ovalbumin orally
- Control group of mice are fed a different protein orally
- Fed daily
- On day 7, mice are injected (through intramuscular) with ovalbumin attached to adjuvant (adjuvant enhances the immune response) --> this is the antigen
--> Mice that were fed ovalbumin had very limited response to this antigen
--> Mice that were not fed ovalbumin had massive response to the antigen
- If you introduce small amounts of the antigen orally, can create a small tolerance to this antigen not only in the gut but also systemically through the whole body
What is C. diff? Does it have a vaccine?
- C. diff = hospital acquired infection
- Quite fatal
- No vaccines available
--> If you want to create a vaccine for something that targets the gut mucosa, want to create a vaccine that produces protection in the gut, e.g oral vaccine
--> Need to overcome oral tolerance to be able to make oral vaccines
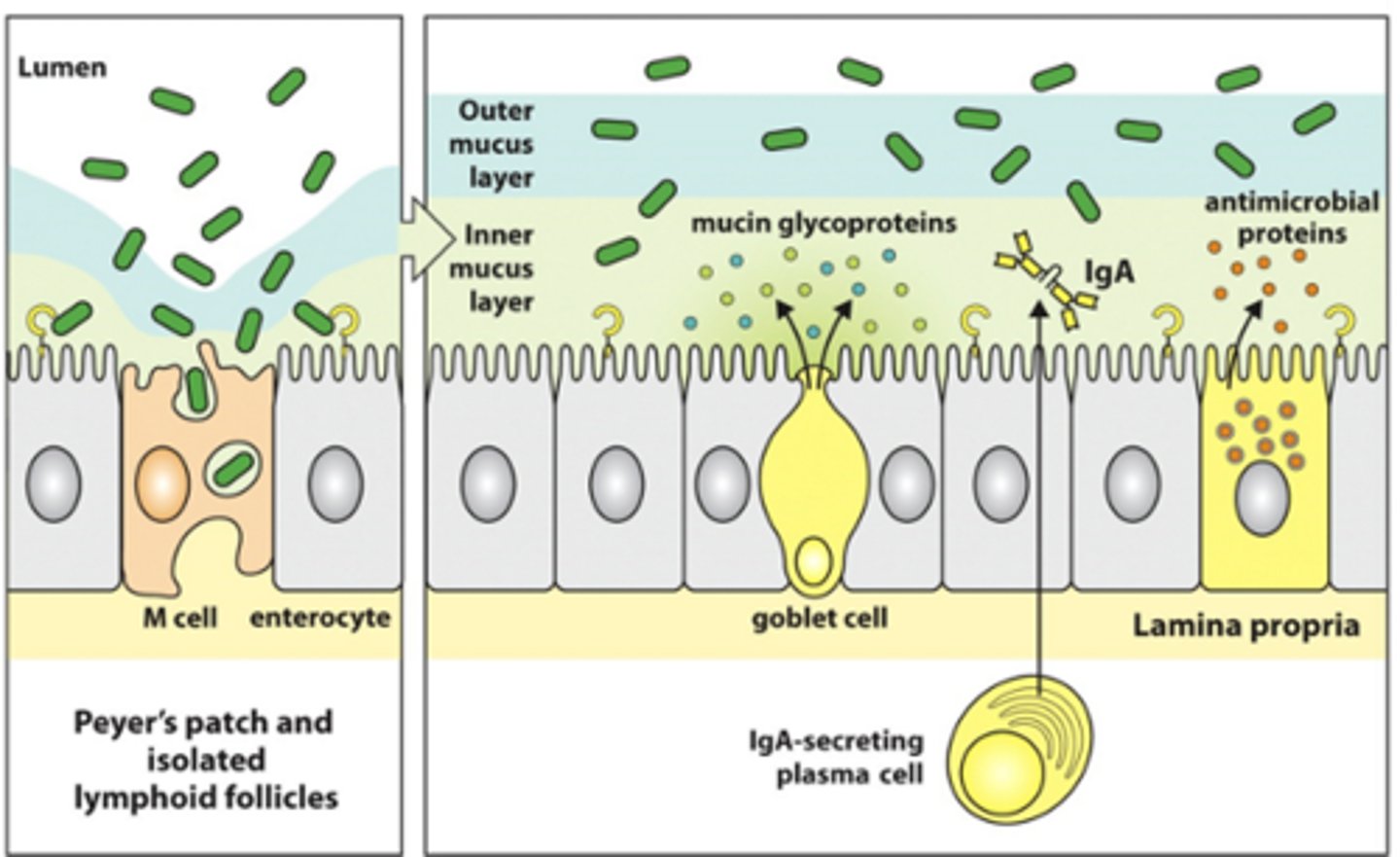
What happens in the presence of commensal organisms in the gut? Describe the general responses and structures involved in preventing an immune response to them
- Have Peyer's patches and isolated lymphoid follicles scattered in the gut
- Have commensal bacteria coming in through M (microfold) cells
- This generates a low level IgA response from B cells
- Don't want too much bombardment of this system
--> Can inhibit this
--> Have TLRs that recognise the antigen and so the antigen can enter the underlying tissues through the enterocytes as well as the M cells
- Have physical barriers:
--> 2 layers of mucus (inner and outer layers) that have slightly different viscosities
--> Goblet cells produce mucus (mucin polypeptides)
--> Have paneth cells that secrete antimicrobial proteins
- IgA forms dimer and enter lumen to tie up commensal organisms and stops them from getting through into the tissues
- Overall role: stops overstimulation by vast amounts of commensal organisms and inhibit potential pathogens from becoming established here
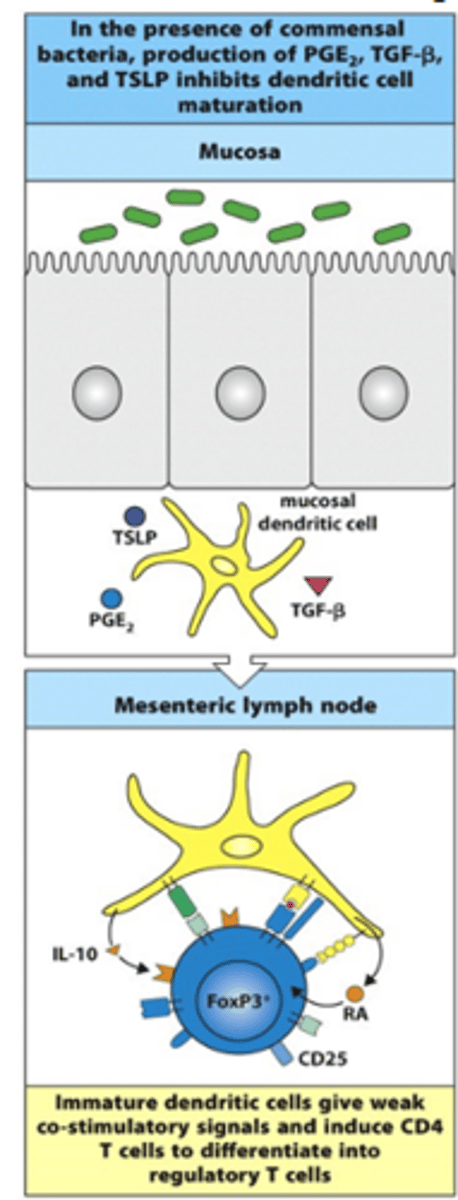
What sorts of T cells are produced in response to commensal organisms? Describe the process
- In the presence of commensal bacteria, PGE2, TGF-beta and TSLP are produced
--> This inhibits dendritic cell maturation
--> Generates/maintains the sleep state of the dendritic cell
- In mesenteric lymph node:
--> Immature dendritic cells give weak co-stimulatory signals (e.g IL-10, CD25, RA) and induce CD4+ T cells to differentiate into Treg cells (Foxp3+ cells)
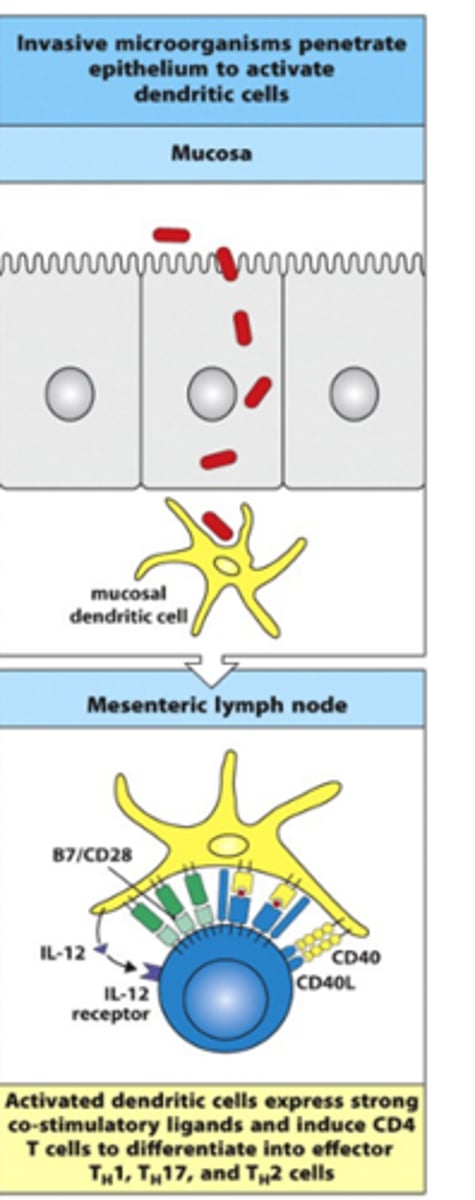
What sorts of T cells are produced in response to invasive microorganisms? Describe the process
- Invasive microorganisms penetrate the epithelium/come in through M cells to activate dendritic cells
- Dendritic cell takes in pathogen, processes and puts out on MHCII
--> Recognises PAMPs through PRRs and snaps dendritic cell out of 'lazy' state
--> Danger signals on APC are upregulated
--> Expresses co-stimulatory signals, e.g B7/CD28, IL-12, CD40
--> Activation of T cells depends on the cytokine signal released
- Induce CD4+ T cells to differentiate into effector TH1, TH17 and TH2 cells
Why don't food and commensal organisms produce an immune response?
- Commensal organisms and food antigens do not carry the danger signals recognised by TLRs on the surface of macrophages and dendritic cells (PAMPs)
--> They do not stimulate an inflammatory response which is necessary to generate an immune response
- Commensal gut flora also inhibit the activation of dendritic cells, by production of molecules like prostaglandin
--> These cells give out weak co-stimulatory signals to CD4+ T cells making them differentiate into Treg cells and preventing them from activating to TH1 or TH2 cells
- Regulatory CD4+ T cells generate anti-inflammatory cytokines and stimulate an anti-inflammatory local IgA response by class switching
How can oral tolerance by useful in the medical environment?
- Production of oral/mucosal tolerance increases levels of TGF-beta which has many immunosuppressive properties
- Generation of mucosal tolerance in animal models of inflammatory disease has protective properties for that disease, e.g experimentally induced arthritis and encephalomyelitis
- This raises the possibility of using induced oral tolerance in treatment of human inflammatory disease, though trials have not been very promising for the treatment of established disease