Substance-Related Disorders
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
What is a substance use disorder?
when an individual uses more of the substance than they originally intended to and continue to use that substance despite experiencing significant adverse consequences.
types of dependence for substance use disorders
Physical dependence : changes in normal bodily functions—the user will experience withdrawal from the drug upon cessation of use.
Psychological dependence: an emotional, rather than physical, need for the drug and the drug is used to relieve psychological distress.
What is tolerance?
physiological dependence, and it occurs when a person requires more and more drug to achieve effects previously experienced at lower doses.
What is withdrawl?
a variety of negative symptoms experienced when drug use is discontinued.
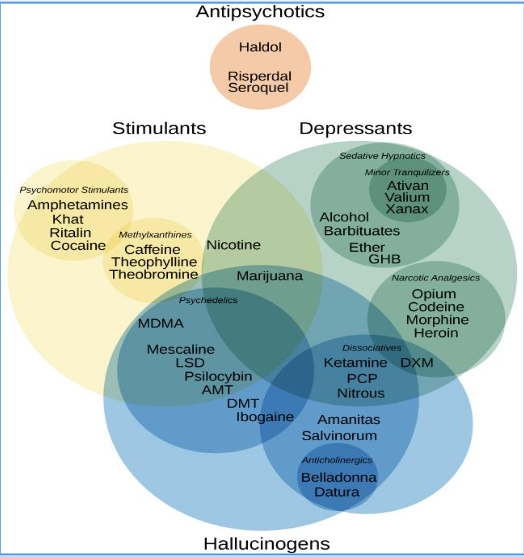
picture gives depiction of how all of the substances may or may not be intermingled based on usage
EtOH prevalence in the U.S.
30% of Americans meet DSM criteria for AUD in their lifetime
27% report binge drinking monthly
High association with accidents, suicide, homicide
Life expectancy: ~12 years shorter for people with alcohol dependence
How does EtOH affects the brain?
Low doses: activates dopamine in the mesolimbic pathway → pleasure
High doses: inhibits glutamate → poor judgment, lowered self-control
Can lead to brain shrinkage, impaired memory, and decision-making deficits
What are the short-term and long-term consequences of EtOH?
Short-Term:
Hangover (fatigue, nausea, anxiety)
Blackouts, risky behavior
Long-Term:
Liver cirrhosis (15–30% of heavy drinkers)
Malnutrition and gastrointestinal problems
Cognitive decline and brain damage
What is Fetal Alcohol Syndrome (FAS)?
Caused by alcohol consumption during pregnancy
Leads to: growth deficiencies, facial abnormalities, intellectual disability
CDC: “No safe amount of alcohol during pregnancy”
What is the DSM-5 Criteria for Alcohol Use Disorder?
A. 2+ of the following within 12 months (craving, unsuccessful attempts to cut down, role failures, tolerance, withdrawl)
B. Severity: Mild (2-3 symptoms), Moderate (4-5 symptoms), Severe (6+ symptoms)
Alcohol is often taken in larger amounts or over a longer period than was intended
There is a persistent desire or unsuccessful efforts to cut down or control alcohol use
A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
Craving, or a strong desire or urge to use alcohol
Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school or home
Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerated by the effects of alcohol
Important social, occupational, or recreational activities are given up or reduced becaue of alcohol use.
Recurrent alcohol use in situations in which it is physically hazardous
Alcohol use is continured despite knowledge of having a persistent or recurrent physical or psychological prblem that is likely to have been caused or exacerbated by alcohol
Tolerance, as defined by either of the follwoing
A need for markedly increased amounts of alcohol to achieve intoxication or desired effect
A markedly diminished effect with continued use of the same amount of alcohol
Withdrawl, as mainifested by either of the following
The characterisitic withdrawl syndrome for alcohol (refer to Criteria A and B of the criteria set for alcohol withdrawal)
Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
What are the biological causal factors to aEtOH lcohol use?
Pleasure Pathway (mesocorticolimbic pathway aka MCLP): Alcohol stimulates dopamine release
What are genetic vulnerability to EtOH use?
Having 1 alcoholic parent ↑ AUD risk significantly
Adoption studies support genetic influence
Alcohol flush reaction common in Asians → potential protective factor
What are the psychosocial causal factors of EtOH use?
Poor parental modeling and lack of monitoring
Psychological vulnerability: antisocial personality, depression, trauma history
Stress & Tension-Reduction Hypothesis: alcohol used to self-soothe
Expectancy Theory: beliefs that alcohol enhances social success, relaxation, and improved mood
What is the progression and course of EtOH use?
Early use → tolerance → dependence
Can begin in childhood or later life
Withdrawal symptoms include tremors, hallucinations, confusion (delirium tremens)
Chronic use → brain and liver damage, memory disorders (e.g., Korsakoff’s)
What is caused by Alcohol Amestic Disorder (Korsakoff’s Syndrome)?
Severe memory issues and confabulation
Due to thiamine (vitamin B1) deficiency
Can be reversed early with thiamine; may become irreversible if untreated
According to the DSM-5, how many criteria must be met within a 12-month period to be diagnosed with Alcohol Use Disorder?
A. At least 1
B. At least 2
C. At least 4
D. At least 6
B. At least 2
What is the main cause of alcohol amnestic disorder (Korsakoff’s syndrome)?
A. Chronic liver disease
B. A mutation in the dopamine receptor gene
C. Lack of vitamin B1 (thiamine)
D. Overactivation of the pleasure pathway
C. Lack of vitamin B1 (thiamine)
What are the interpersonal influences on EtOH abuse?
Excessive drinking can be reinforced within intimate relationships.
Spouses or close partners may unknowingly enable or promote alcohol use.
Relationship crisis (e.g., marital conflict) often trigger increases in drinking.
Family Dynamics:
Family factors (e.g., poor supervision, marital conflict, lack of cohesiveness) are linked to later alcohol use disorders.
What are the sociocultural factors of EtOH use?
Religious and cultural values (e.g., in Muslim, Mormon, and orthodox Jewish communities) limit alcohol use.
In contrast, European cultures often show higher rates of alcohol consumption.
Factors of College Binge Drinking
Approximately 80% of college students drink; half engage in binge drinking.
Binge drinking is associated with academic problems, and in some tragic cases, fatalities.
Examples: Incidents of alcohol poisoning among college students.
Reasons for Binge Drinking:
Expression of independence from parental influence.
Peer pressure, situational influences, and gender role expectations.
Beliefs about alcohol’s ability to enhance celebrations and social interactions.
What is the treatment for EtOH related disorders?
Many alcohol abusers are in denial; treatment is often sought only after “hitting bottom.”
Less than one-third of individuals with alcohol use disorders receive treatment.
Multidisciplinary Approach:
Combining medical, psychological, and environmental interventions is most effective.
Treatment goals include detoxification, behavioral change, and social reintegration.
Traditional vs. Controlled Drinking Approaches:
Traditional programs emphasize complete abstinence.
Some interventions (e.g., Brief Motivational Intervention, self-control training) aim at moderated or controlled drinking.
What are the medical and pharmacological treatments for EtOH use?
Initial focus on eliminating alcohol and managing withdrawal symptoms.
Use of benzodiazepines (e.g., Valium, diazepam) to reduce withdrawal risks (seizures, delirium).
Medications:
Antabuse (Disulfiram): Creates an aversive reaction if alcohol is consumed.
Naltrexone: Blocks alcohol’s pleasure-producing effects.
Acamprosate: Properties still under study; helps reduce heavy drinking.
What are some individual and group therapy options for EtOH treatment?
Cognitive-behavioral therapy (CBT) focuses on developing coping and stress-management skills.
Group therapy helps confront denial and facilitates learning through shared experiences.
DBT Skills (1:07)
What are some brief interventions for EtOH treatment?
Brief Motivational Intervention (BMI: 2:14): A short session that enhances self-regulation and readiness to change.
Computer-based self-control training programs have shown promise in reducing problem drinking.
What are the Cognitive-Behavioral Approaches for EtOH Relapse Prevention Strategies?
Planned relapse strategies help maintain confidence and prevent complete loss of self-efficacy.
Involvement of family members in relapse prevention can enhance long-term outcomes.
What is the Abstinence Violation Effect?
Minor transgressions may lead to feelings of failure, increasing the risk of full relapse.
Emphasizes the need for continuous self-monitoring and support.
What is the controlled drinking approach?
Suggests some individuals (often with less severe problems) can learn to moderate their intake.
What is the abstinence approach?
Emphasizes total cessation of alcohol use; favored by many self-help groups like AA.
What is Alcoholics Anonymous?
Founded in 1935; uses a 12-step program and emphasizes lifelong abstinence.
AA provides social support through group meetings, testimonials, and mutual help.
AA helps reduce personal responsibility by framing alcohol use disorder as a chronic condition.
Outcome studies are mixed due to methodological challenges; however, AA participation is associated with decreased drinking in both short- and long-term follow-up.
What are common Opiates?
opium, morphine, codeine, heroin, and methadone
What is the histoical context for Opium Abuse?
Opium has been used for centuries; morphine was widely used during the Civil War.
Heroin was developed from morphine and quickly became more potent and addictive.
How does someone use Opiates?
Opiates can be smoked, snorted, or injected (mainlining and skin popping).
Immediate Effects:
Users experience a rapid, intense “rush” (often compared to a sexual orgasm) followed by several hours of a “high” and subsequent negative phases.
What are the biological effects, withdrawl symptoms , and social/health impacts of Opiates?
Continued use (approximately 30 days) leads to physical dependence.
Tolerance increases over time; larger amounts are needed for the same effect.
Withdrawal Symptoms:
Can include runny nose, sweating, nausea, tremors, insomnia, and, in severe cases, delirium and cardiovascular collapse.
Withdrawal symptoms generally peak within 3–4 days and subside by days 7–8.
Social and Health Impacts:
Opiate addiction often leads to criminal behaviors and serious health issues (e.g., hepatitis from unsterile injection practices).
What are the neural bases for Opiate addiction?
Opiate Receptors: Opiates bind to receptors that regulate pleasure, pain, and breathing.
Dopamine Reward Pathway: Addiction is linked to dysfunction in the dopamine system—from the ventral tegmental area to the nucleus accumbens.
Reward Deficiency Syndrome: Individuals with genetic variations may find natural rewards less satisfying, predisposing them to seek external stimulation via drugs.
Other neurotransmitter systems (e.g., the opioid system) play key roles in the “liking” aspect of drug use.
What are the key chracteristics of Opiate Addiction?
High rates of comorbidity with other psychological disorders and substance abuse
Chronic nature of heroin and opioid use; persistence of cravings post-withdrawal
What are treatment straegies for opiate addicts?
Pharmacological Interventions:
Methadone maintenance programs
Buprenorphine as an effective alternative with fewer side effects
Psychological Interventions:
Behavioral therapies (counseling, group therapy)
Combined approach enhancing abstinence and cognitive function
What is the Historical Context for Stimulants?
Early uses in pre-Columbian cultures and later adoption in Western medicine (Freud, Conan Doyle, early Coca-Cola)
What are the pharmacodynamics of stimulants?
Blocks dopamine reuptake leading to increased synaptic dopamine
Results in euphoria, heightened energy, and temporary confidence
What are the treatment approaches to Stimulants?
Use of naltrexone and methadone to ease withdrawal symptoms
Efficacy of Cognitive Behavioral Therapy (CBT) and Contingency Management (CM) in reducing cocaine use
What are the effects and withdrawl symotoms of amphetamines?
Effects: Increased alertness, appetite suppression, but high potential for abuse and tolerance
Withdrawal: Symptoms include nausea, depression, and prolonged cognitive impairment
What are the effects and withdrawl symotoms of methamphetamines?
“Crystal meth” characteristics and ease of illicit manufacture
Rapid development of tolerance, brain changes, and severe psychiatric effects
High relapse rates post-treatment and challenges in achieving long-term abstinence
What are legal stimulants?
Caffeine and Nicotine
What are the effects, dependence, and treatments for nicotine?
Negative effects primarily intoxication (e.g., headache) rather than severe withdrawal
Nicotine:
High prevalence and early exposure
Strong physical and psychological dependence with withdrawal symptoms (irritability, anxiety, difficulty concentrating)
Treatment for Nicotine Dependence:
Nicotine replacement therapy (patches, gum, lozenges)
Behavioral interventions and counseling strategies
Emerging treatments (e.g., bupropion) and educational approaches
What are the pharmacological effects and withdrawl management of sedatives (barbiturates)
Act as depressants, inducing relaxation and sedation
Immediate effects: relaxation, sleep induction; higher doses can be lethal (respiratory depression)
Withdrawal Management:
Tapering doses to minimize dangerous withdrawal symptoms
Challenges with withdrawal: anxiety, tremors, insomnia, and possible delirium
What are hallucinogens?
Profound alterations in perception, mood swings, potential for traumatic “bad trips”
Long-term concerns: Flashbacks and persistent visual distortions
What are the different hallucinogen drug names?
LSD
Mescaline
Psilocybin:
Historically used in ceremonial contexts; alter sensory perception
Ecstasy (MDMA):
Combines hallucinogenic and stimulant properties
Euphoria, energy boost, but also risks such as hyperthermia and serotonin depletion leading to subsequent depression
What are the effects and treatment considerations for Cannabis?
Effects:
Mild euphoria, altered time perception, and enhanced sensory experience
Negative outcomes: Memory impairment, anxiety, and potential for withdrawal symptoms
Treatment Considerations:
Limited effectiveness of specific pharmacotherapies for cannabis dependency
Psychological interventions shown to reduce use; buspirone as a potential, modest aid
What is an overview of the DSM-5 Criteria for Gambling Disorder?
Persistent gambling despite significant negative consequences
Key symptoms: Escalating bets, preoccupation, chasing losses, and reliance on others for financial support
Epidemiology and Comorbidity:
Estimated prevalence of 1–2% in the adult population
High comorbidity with alcohol use disorders and personality disorders
What are the comorbidity and underlying mechansims for Pathological Gambling?
High rates of co-occurrence with substance abuse (e.g., alcohol, cocaine) and impulsivity
Severe gambling problems often seen in those with co-occurring substance disorders
Underlying Mechanisms:
Early trauma may contribute to impulsive, compulsive gambling behaviors
Recent research implicates brain regions tied to motivation, reward, and decision-making
Genetic factors and neurodevelopmental events during adolescence may play a role.
What is the overlaying substitle for substance abuse disorders?
disinhibited externalizing