BMS 595 L2 Quiz #4 body fluid compartments and blood
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
water moves through semi-permeable membranes of cells and from one compartment of body to another by a process called
Osmosis
In osmosis, The diffusion of water from regions of _______ concentration to regions of ________ concentration, along an osmotic gradient across a semi-permeable membrane.
higher, lower
True or False: chemical reactions of life take place in aqueous solutions
True
the dissolved substances in a solution refer to
solutes
water range for infants
75%
water range for men and women
50-60% and low as 45% in old age
Which parts of the body have the highest proportions of water
brain and kidneys 80-85%
True or False: Intracellular fluid (ICF) compartment in the human body is a system that includes all fluid enclosed in cells by their plasma membrane.
Hint think of inside of cell (intra-inside/ cellular-cell)
True
*also is the principle component of the cytosol/cytoplasm
This fluid compartment in the human body surrounds all cells in the body.
Extracellular Fluids (ECF)
Extracellular fluid compartment consist of:
Fluid component of the blood (plasma) and interstitial fluid (IF) that surrounds all cells not in the blood
Most of the water in the body is from what fluid compartment in the human body?
intracellular fluid (60%)
the second largest volume is interstitial fluid
True or False: the Extracellular Fluid include the cerebrospinal fluid that bathes the brain and spinal cord, lymph, the synovial fluid in joints, the pleural fluid in the pleural cavities, the pericardial fluid in the cardiac sac, the peritoneal fluid in the peritoneal cavity, and the aqueous humor of the eye.
True
Net filtration occurs near the arterial end of the capillary since capillary hydrostatic pressure (CHP) is greater than blood colloidal osmotic pressure (BCOP). There is no net movement of fluid near the midpoint of the capillary since CHP = BCOP. Net reabsorption occurs near the venous end of the capillary since BCOP is greater than CHP. This refer to what exchange?
Capillary Exchange
This disorder is the accumulation of excess water in the tissues; it's most common in soft tissues of the extremities and physiological causes are water leakage from blood capillaries
Edema
Blood is made up of:
plasma and formed elements
blood functions
transportation and heat regulation
Young adult male has approximately
5 liters of blood
blood volume varies
age; body type; sex; method of measurement
Formed elements are:
- Erythrocytes- Red Blood Cell (RBC)
- Platelets (Thrombocytes- not true cells)
- White Blood cells (leukocytes)
Description of what formed element:
Have no nucleus and shaped like tiny biconcave disks, anucleate disc
salmon colored
diameter: 7-8 micrometer
Do not contain ribosomes, mitochondria, and other organelles typical of most body cells
The primary component is hemoglobin (transport oxygen and carbon dioxide)
Most numerous of the formed elements
Red Blood Cell (RBC)
Function of what formed element
- critical role in transport of oxygen and carbon dioxide depends on hemoglobin
- carbonic anhydrase (CA)- enzyme that catalyzes a reaction joining carbon dioxide and water to form carbonic acid
- carbonic acid- dissociates and generates bicarbonate ions that will diffuse out to transport carbon dioxide in the blood plasma
Red Blood Cell (erythrocytes)
These are facts of a primary component in RBC -within each RBC are approximately 200 to 300 million molecules of _____
- made up of 4 globulin chains each attached to a heme group
- able to unite four oxygen molecules to form oxyhemoglobin to allow RBCs to transport oxygen where it is needed
- a male has a greater amount of hemoglobin than a female - Anemia - a decrease in number or volume of functional RBCs in a given unit of whole blood
hemoglobin
A decrease in number or volume of functional RBCs in a given unit of whole blood
Anemia
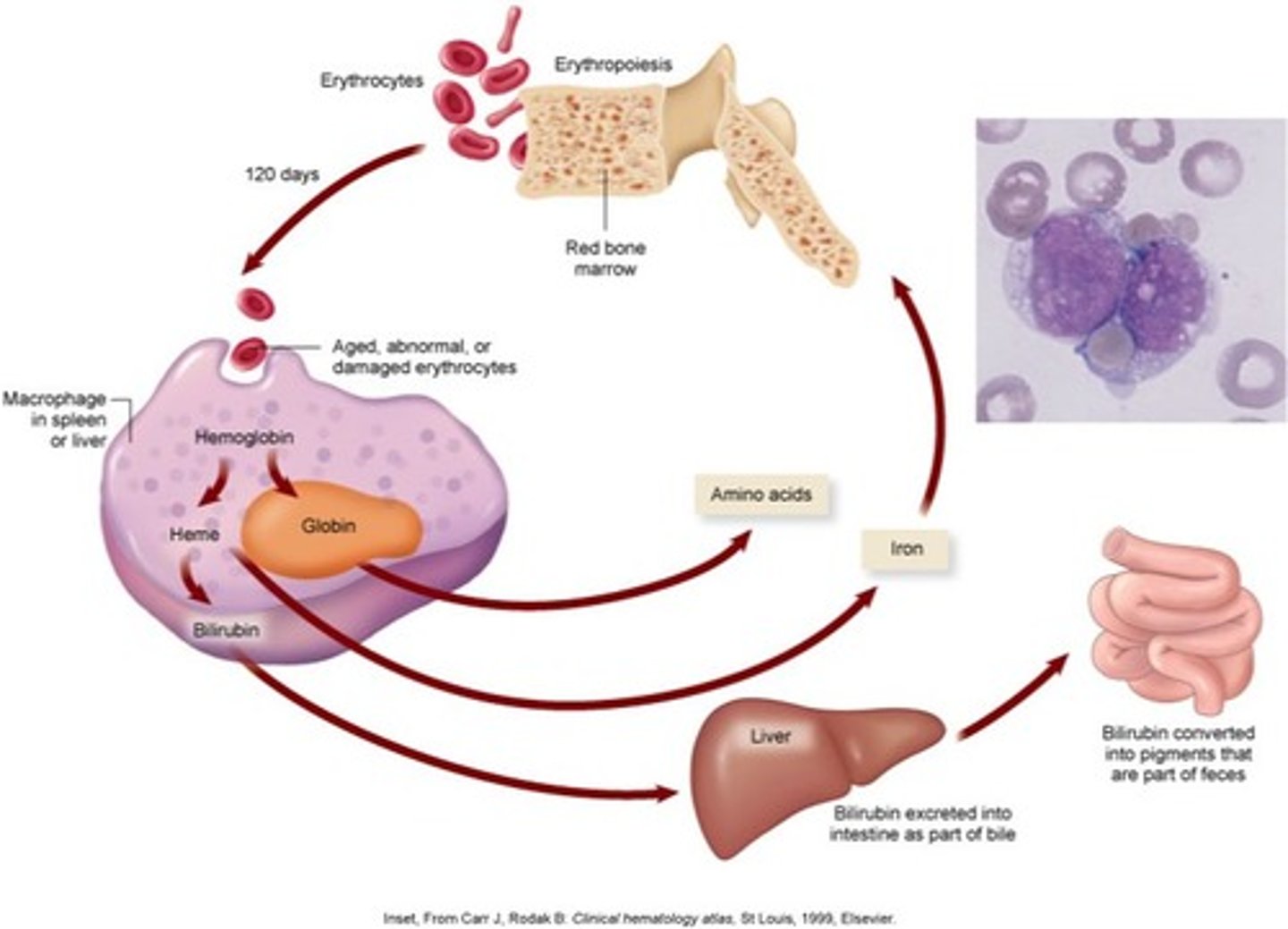
This is the process of Red Blood Cells begin in the red bone marrow as hematopoietic stem cells and goes through several stages of development to become erythrocytes
- maturation requires appro. 4 days
- RBC created and destroyed @ appro. 200 billion per day in adults
- homeostatic mechanisms operate to balance the number of cells formed against the number of cells destroyed
Erythropoiesis
Destruction of RBCs
- Life span of a circulating RBC averages 105 to 120 days
- Macrophage cells phagocytose the aged, abnormal, or fragmented RBCs
- Hemoglobin is broken down, and amino acids, iron, and bilirubin are released
white blood cells (leukocytes)
*reflected in picture and back of card
neutrophil- multi-lobed & bacterial or fungal infection; most common first responders to microbial infection
eosinophil- bi-lobed; parasitic infections/ allergic reactions (inflammatory)
basophil-bi-tri lobed & allergic/antigen response (release histamine causing vasodilation)
lymphocyte- deep staining, eccentric; includes B-cells, CD4+ Helper T cells & CD8+ cytotoxic T cells; operate primarily in the lymphatic system
monocyte- kidney shaped; phagocytosis of pathogens, presentation of antigens to T cells. eventually becoming tissue macrophages, which remove died cell debris and attack microorganisms
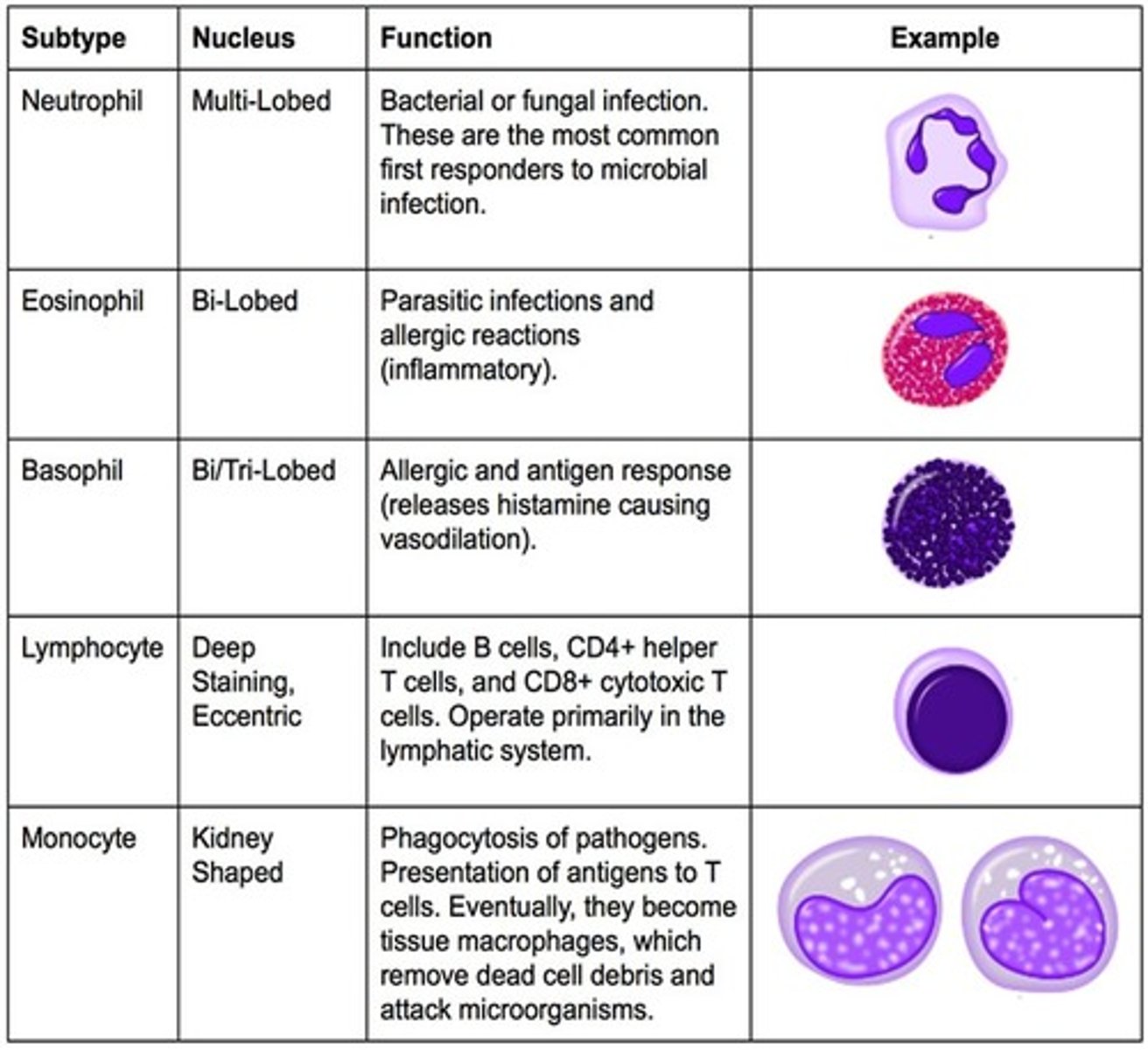
What type of white blood cell is this? kidney shaped; phagocytosis of pathogens, presentation of antigens to T cells. eventually becoming tissue macrophages, which remove died cell debris and attack microorganisms
monocyte
What type of white blood cell is multi-lobed & bacterial or fungal infection; most common first responders to microbial infection
neutrophil
What type of WBC is bi-lobed; parasitic infections/ allergic reactions (inflammatory)
basophil-bi-tri lobed & allergic/antigen response (release histamine causing vasodilation)
eosinophil
What type of WBC is deep staining, eccentric; includes B-cells, CD4+ Helper T cells & CD8+ cytotoxic T cells; operate primarily in the lymphatic system
lymphocyte
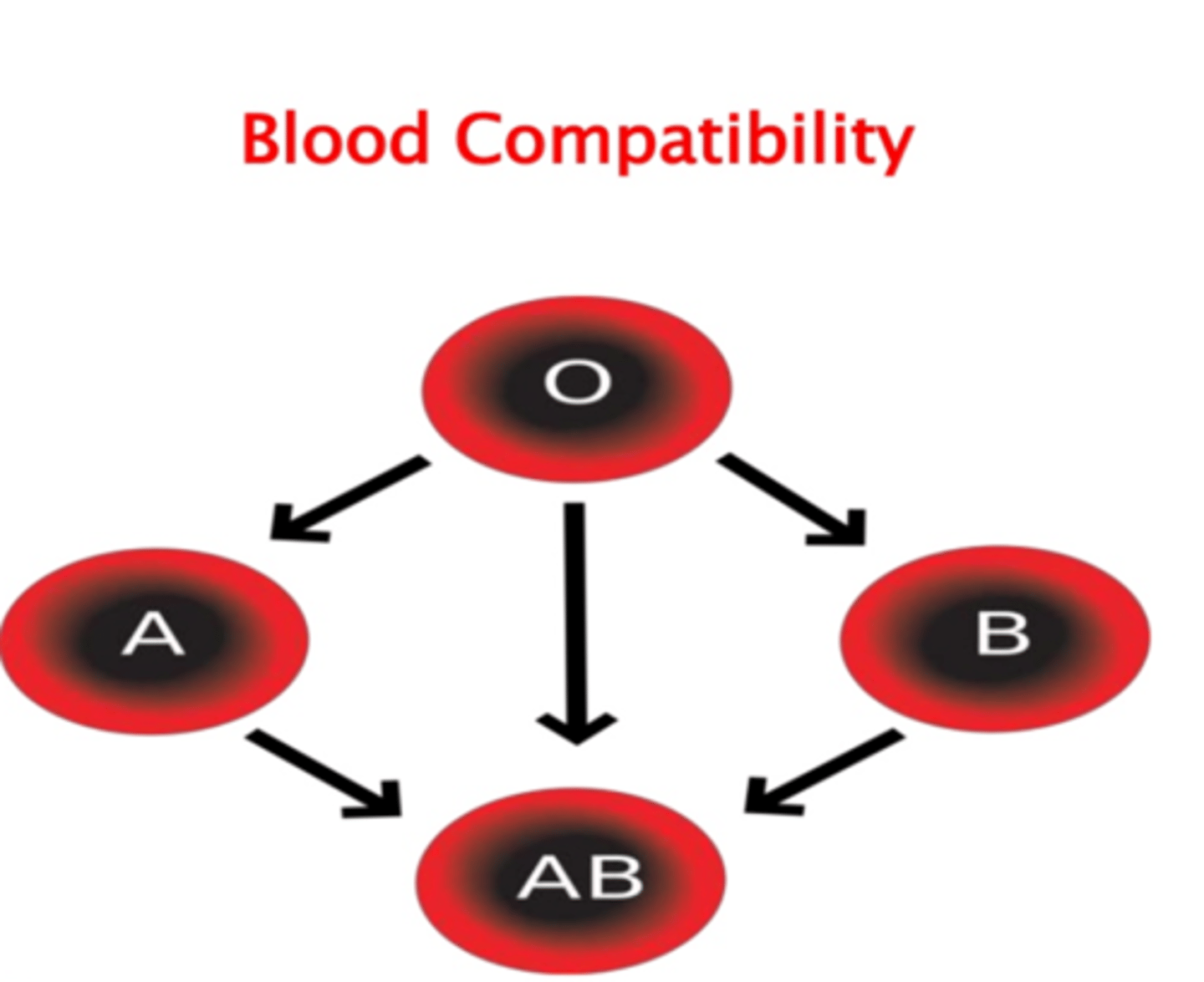
What blood type is the universal recipient because it has no RBC antibodies; this is also a rarer blood type?
Type AB
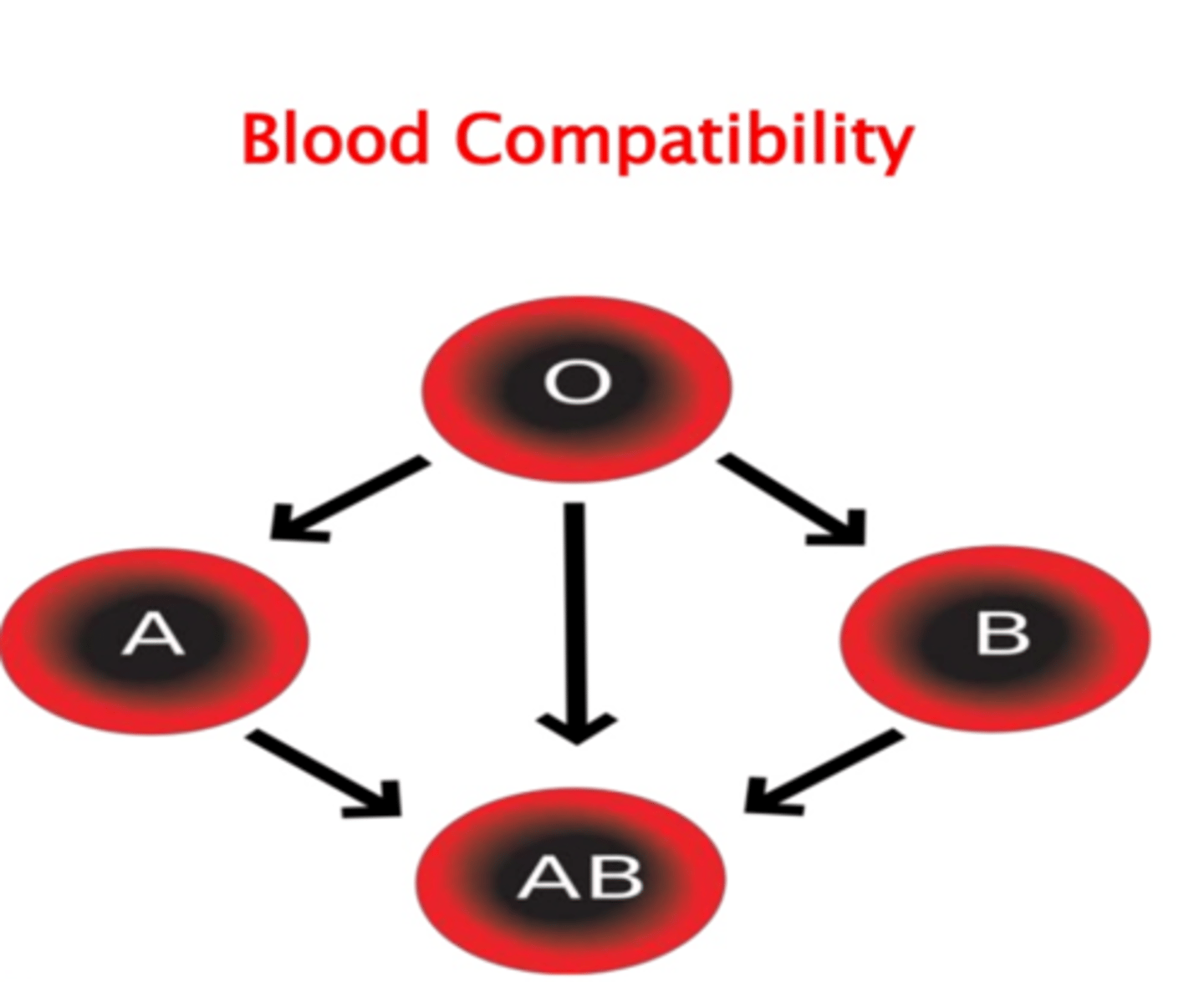
What blood type is the universal donor?
Type O
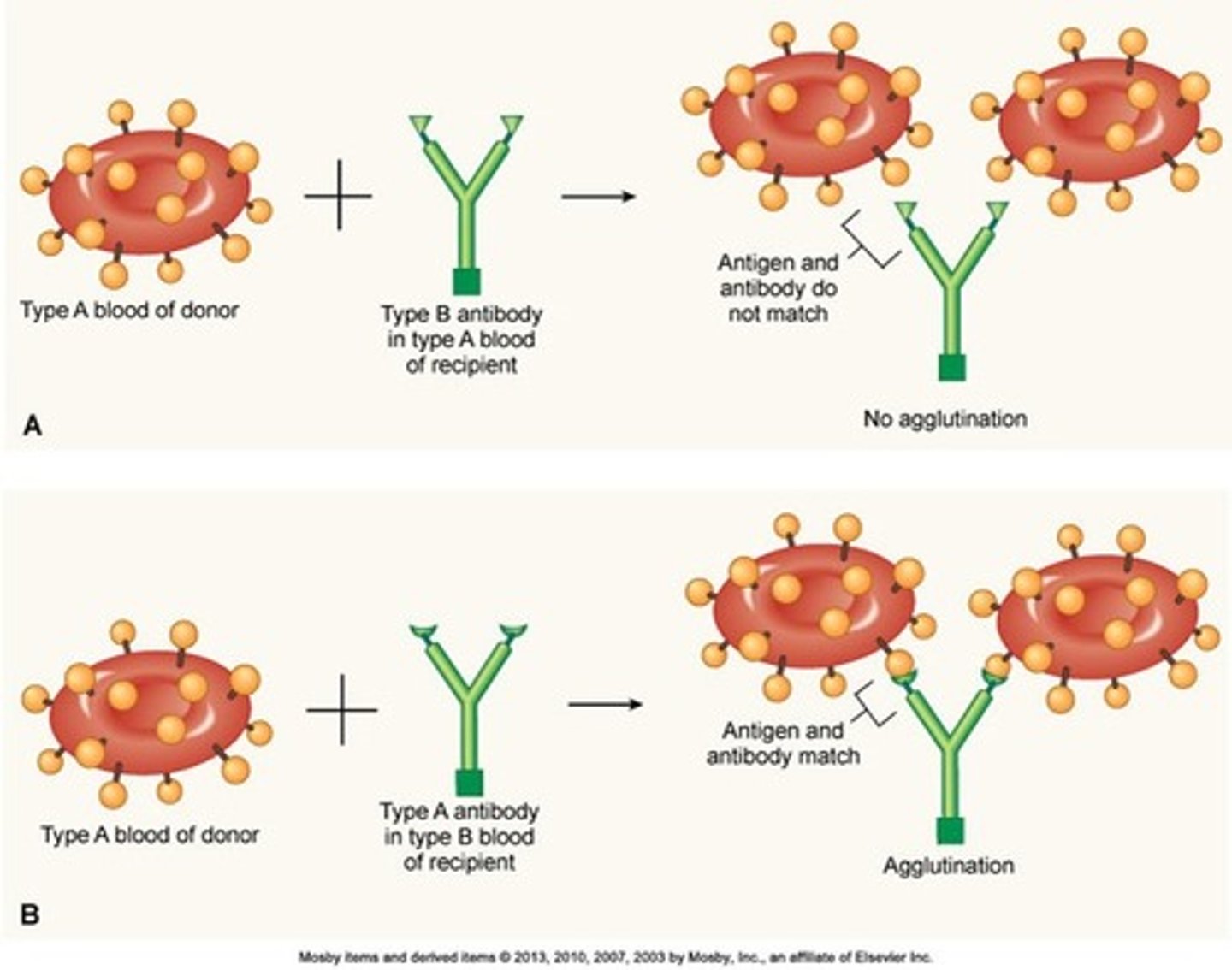
What happens when antibodies attack foreign RBCS; it is defined as the collection of separate particles like RBCs into clumps or masses; these events occur if an antigen is mixed with its corresponding antibody i.e when A antigen is mixed with anti-A antibody-essential giving a person w/ A blood (presenting A antigen) a transfusion of B blood (presenting Anti-A antibody)?
Agglutination
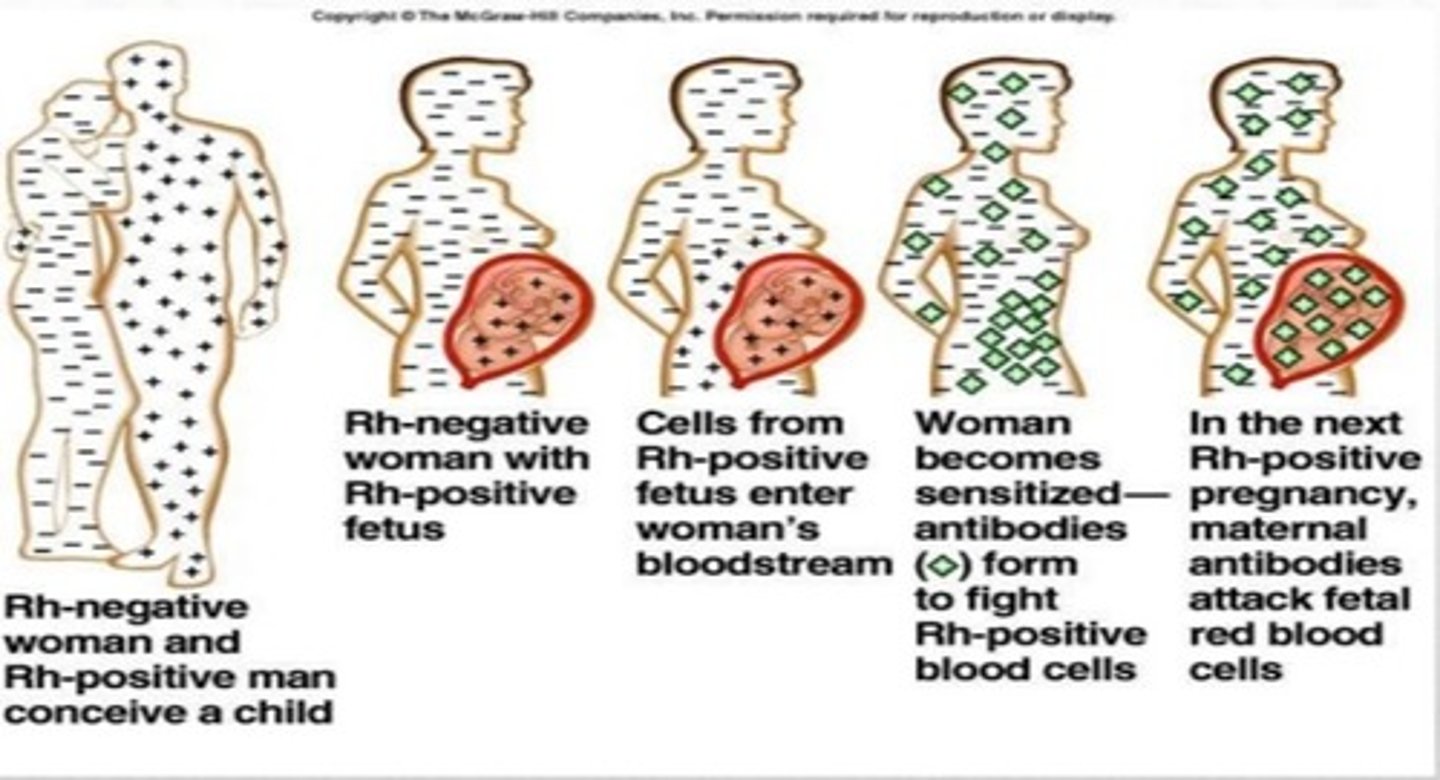
•Named for Rhesus Monkey
•3 genes, C, D, and E, each with two alleles
•DD, or Dd have D antigens on RBCs,
•Classified as Rh+
•Rh - lack D antigens
•Combined with ABO group to get Blood types like A positive or B negative
Rh Groups
What classifies an Rh-positive person versus an Rh-negative person?
The presence of a D antigen
What happens when a mother is Rh-negative is pregnant with an Rh-positive fetus?
•the mother is exposed to Rh-positive red blood cells and leads to maternal antibody production (IgG) against the foreign Rh antigen
•IgG can cross the placenta, subsequent pregnancy with Rh-positive fetus will result in fetal alloimmune-induced hemolytic anemia
Breakdown of red blood cells causes
elevation of bilirubin
hemolytic disease of the newborn (HDN)
•IgM does not cross placenta.
•Rh- mothers exposed to fetal Rh+ blood (often during delivery) may make anti-D IgG
• In subsequent pregnancies, anti-D IgG crosses the placenta causing hemolytic disease of the newborn (erythroblastosis fetalis) in the next fetus that is Rh+.
•Prevented by administration of RhoGAM to Rh - pregnant women during third trimester, which prevents maternal anti-Rh IgG production.
Rh - mothers have anti-D IgG only if previously exposed to Rh+ blood
A liquid part of blood; clear, straw-colored fluid; made up of 90% water and 10% solutes (Figure 20-20)
Solutes—6% to 8% of solutes are proteins, consisting of three main compounds
ØAlbumins—help maintain osmotic balance of the blood
ØGlobulins—essential component of the immunity mechanism
ØFibrinogen—key role in blood clotting
It's proteins have an essential role in maintaining normal blood circulation
Plasma
Coagulation
Mechanism of blood clotting- goal is to stop bleeding and prevent loss of vital body fluid in a swift and sure method; is; the classic theory is as follows:
- Classic theory of coagulation advanced in 1905; identified four components critical to coagulation:
-Prothrombin
-Thrombin
-Fibrinogen
-Fibrin
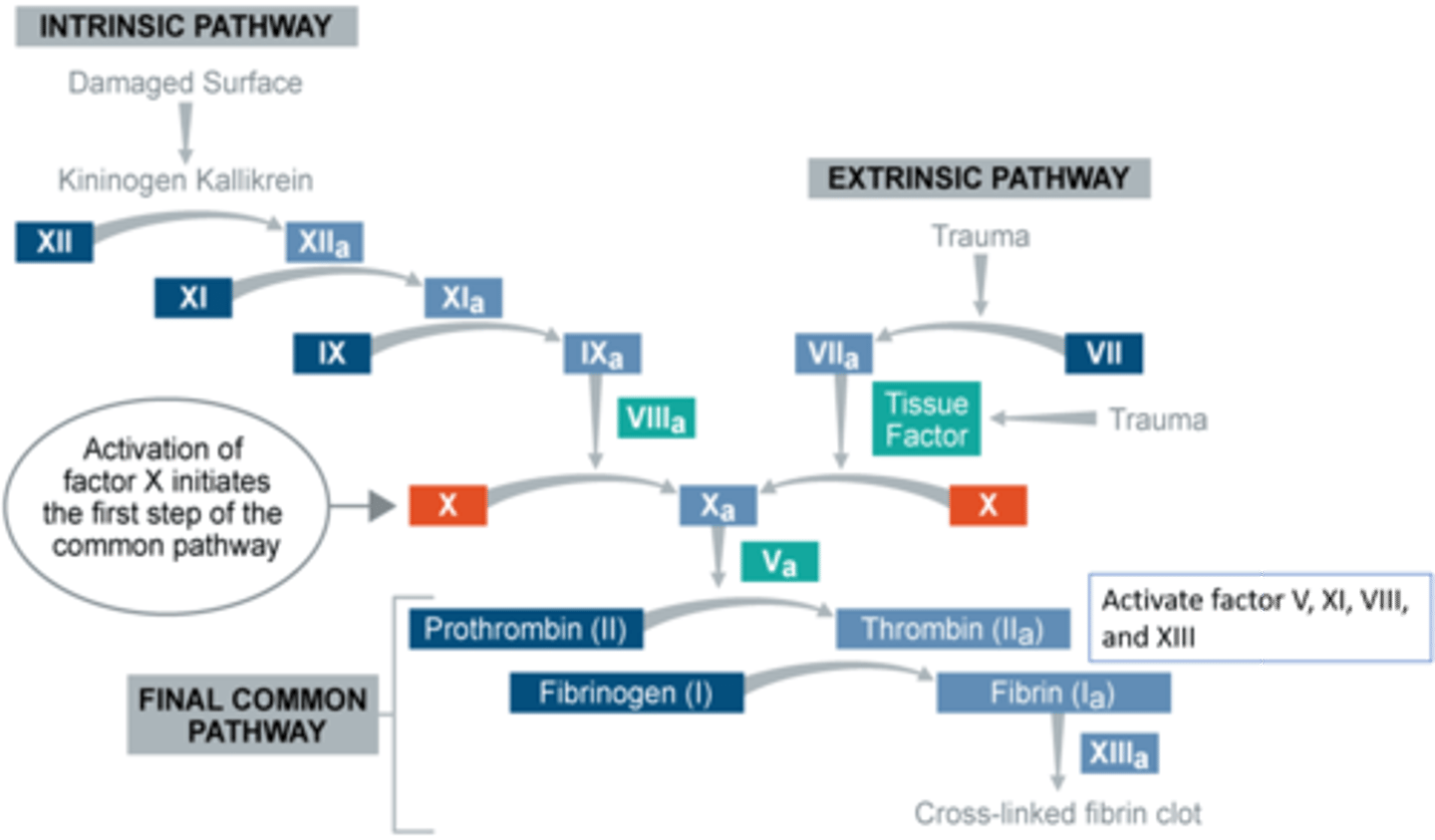
This process is the formation of blood clot that is more sophisticated and more durable repairs collectively; this process is sometimes characterized as a cascade because one events prompt the next in a multi-level waterfall; this result in the production of a gelatinous but robust clot made up of a mesh of fibrin-an insoluble filamentous protein derived from fibrinogen, the plasma protein introduced earlier—in which platelets and blood cells are trapped.
coagulation
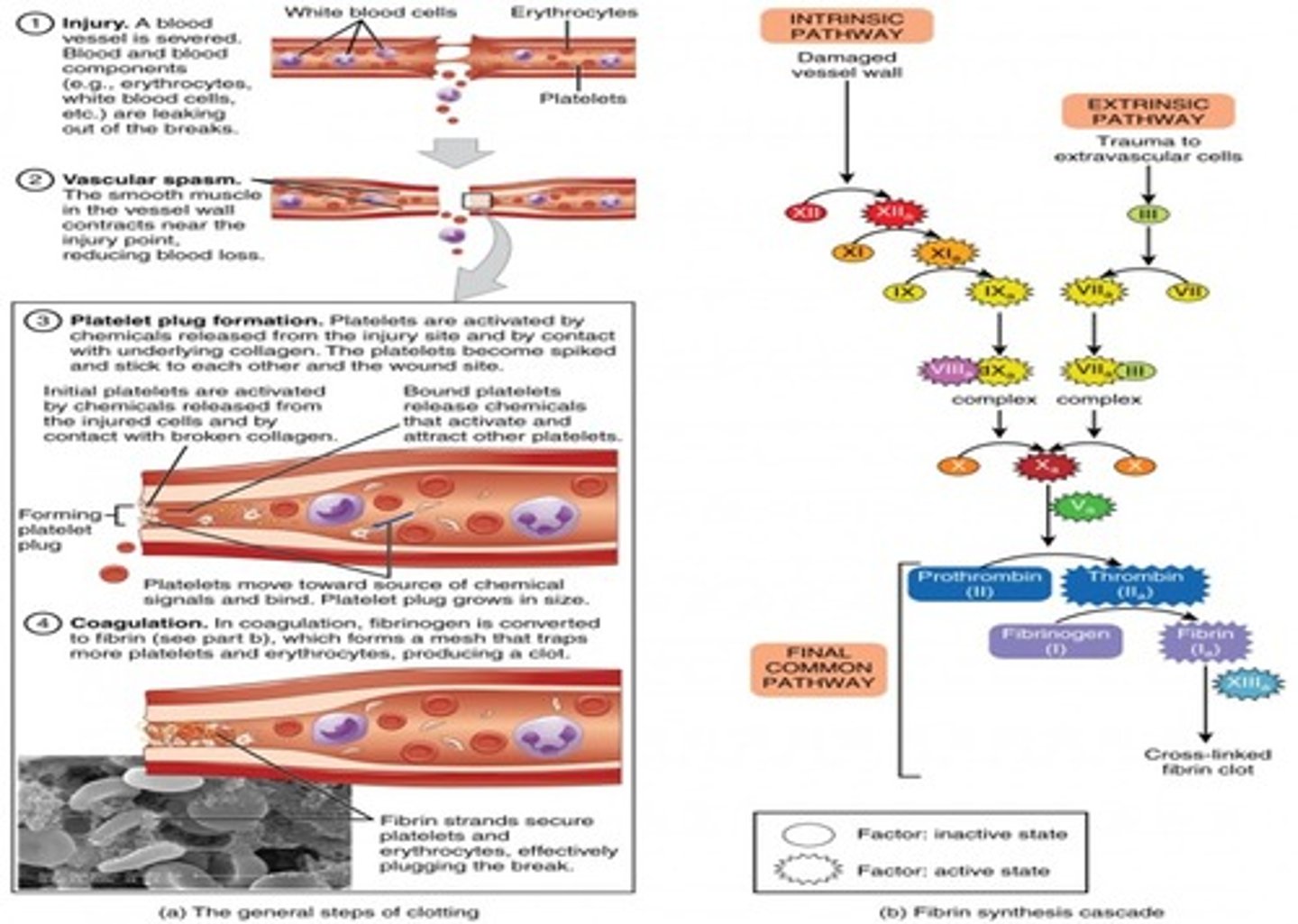
Mechanism of Coagulation (blood clotting)
ØStage 1- production of thromboplastin activator by either of the following:
ØChemicals released from damaged tissues (extrinsic pathway)
ØChemicals present in the blood (intrinsic pathway)
ØStage II - conversion of prothrombin to thrombin
ØStage III - conversion of fibrinogen to fibrin and production of fibrin clot
When a vessel is severed or punctured, or when the wall of a vessel is damaged this phenomenon occurs. In ___ ____, the smooth muscle in the walls of the vessel contracts dramatically. This response is believed to be triggered by several chemicals called endothelin's that are released by vessel-lining cells and by pain receptors in response to vessel injury.
This phenomenon typically lasts for up to 30 minutes, although it can last for hours.
vascular spasm
Formation of the Platelet Plug
A platelet plug can temporarily seal a small opening in a blood vessel
•In the second step, platelets, which normally float free in the plasma, encounter the area of vessel rupture with the exposed underlying connective tissue and collagenous fibers.
•The platelets begin to clump together, become spiked and sticky, and bind to the exposed collagen and endothelial lining. This process is assisted by a glycoprotein in the blood plasma called von Willebrand factor, which helps stabilize the growing platelet plug.
•As platelets collect, they simultaneously release chemicals from their granules into the plasma that further contribute to hemostasis. Among the substances released by the platelets are:
- adenosine diphosphate (ADP), which helps additional platelets to adhere to the injury site, reinforcing and expanding the platelet plug
- serotonin, which maintains vasoconstriction
- prostaglandins and phospholipids, which also maintain vasoconstriction and help to activate further clotting chemicals.
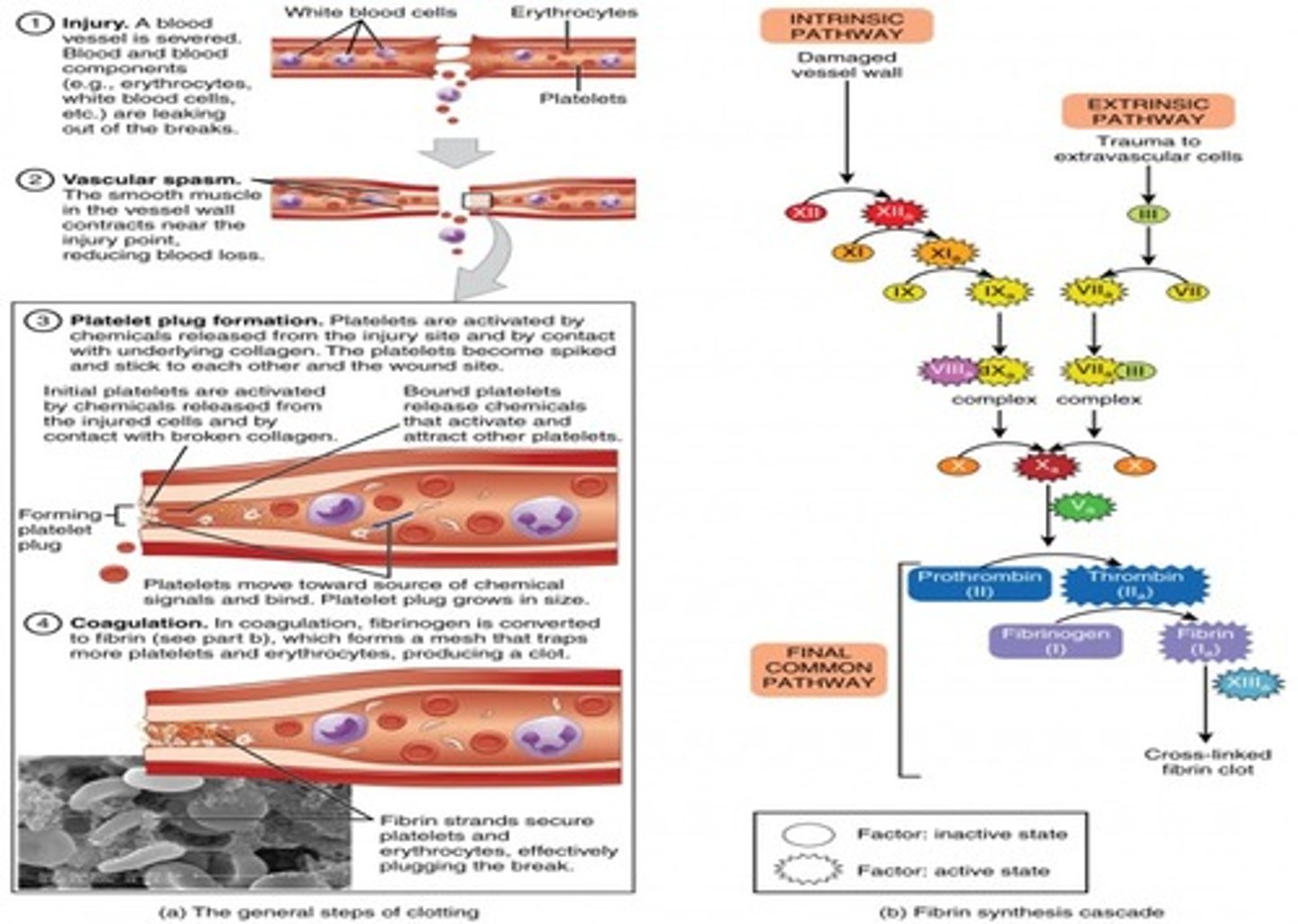
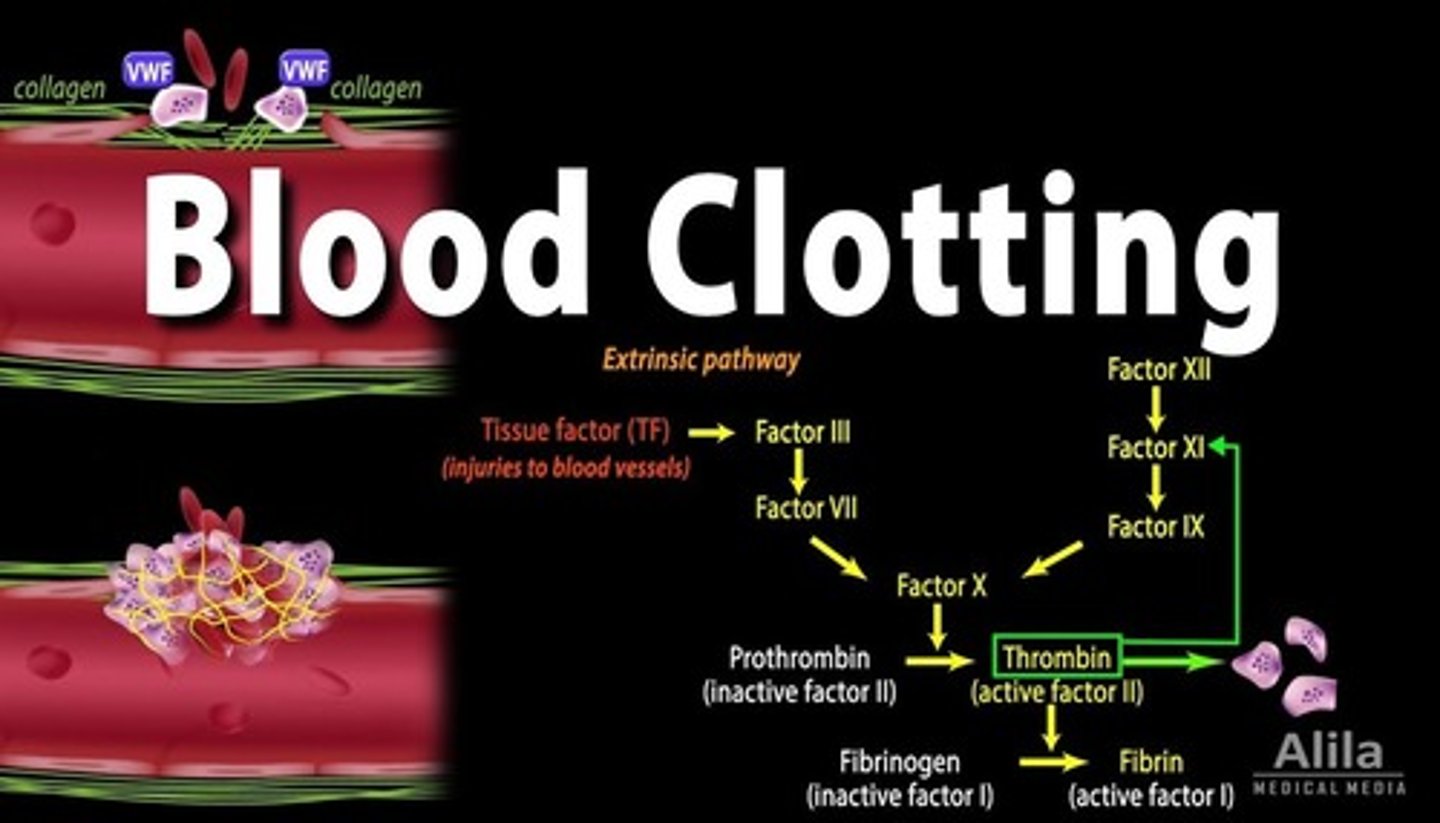
Coagulation Cascade Pathways
Factor Name and notes
I-Fibrinogen
II-Prothrombin. Popular with many other clotting factors. Probably the life and soul of the party.
III (tissue factor [TF]/ tissue thromboplastin) Tissue factor
IV (calicum ions Ca2+)-Calcium. Virtually never known as factor IV.
V ( Proaccelerin, labile factor, or platelet accelerator)-Best friends with factor X.
VI- A case of mistaken identity. Factor VI actually transpired to be just the active form of factor V.
VII- (Serum prothrombin conversion accelerator [SPCA]/ Stable factor)-Proconvertin. Popular with factor X.
VIII (antihemophilic factor [AHF])-Defective in hemophilia A, works as a team with factor IX *Von Willebrand Factor. Acts as a minder to factor VIII and helps platelets stick to things.
IX-(Plasma thromboplastin component [PTC]/ Christmas Factor)Factor VIII's best friend. Deficient in hemophilia B (Christmas disease).
X- (stuart factor, Stuart-Prower Factor, or thrombokinase)-Stuart-Prower factor. Works together with factor V in the central role of activating factor II.
XI-Plasma thromboplastin antecedent (PTA). Knows how to show factor IX a good time.
XII-Hageman factor/ glass factor *Prekallikrein. Likes to lavish attention on factor XII, when not attending to its own needs.
XIII-Fibrin stabilizing factor (FSF)
*High molecular weak kininogen. Cofactor in the activation of factors XI and XII and also prekallikrein.
![<p>Factor Name and notes</p><p>I-Fibrinogen</p><p>II-Prothrombin. Popular with many other clotting factors. Probably the life and soul of the party.</p><p>III (tissue factor [TF]/ tissue thromboplastin) Tissue factor</p><p>IV (calicum ions Ca2+)-Calcium. Virtually never known as factor IV.</p><p>V ( Proaccelerin, labile factor, or platelet accelerator)-Best friends with factor X.</p><p>VI- A case of mistaken identity. Factor VI actually transpired to be just the active form of factor V.</p><p>VII- (Serum prothrombin conversion accelerator [SPCA]/ Stable factor)-Proconvertin. Popular with factor X.</p><p>VIII (antihemophilic factor [AHF])-Defective in hemophilia A, works as a team with factor IX *Von Willebrand Factor. Acts as a minder to factor VIII and helps platelets stick to things.</p><p>IX-(Plasma thromboplastin component [PTC]/ Christmas Factor)Factor VIII's best friend. Deficient in hemophilia B (Christmas disease).</p><p>X- (stuart factor, Stuart-Prower Factor, or thrombokinase)-Stuart-Prower factor. Works together with factor V in the central role of activating factor II.</p><p>XI-Plasma thromboplastin antecedent (PTA). Knows how to show factor IX a good time.</p><p>XII-Hageman factor/ glass factor *Prekallikrein. Likes to lavish attention on factor XII, when not attending to its own needs.</p><p>XIII-Fibrin stabilizing factor (FSF)</p><p>*High molecular weak kininogen. Cofactor in the activation of factors XI and XII and also prekallikrein.</p>](https://knowt-user-attachments.s3.amazonaws.com/bb22206c-92eb-44a6-8907-1990a78bc18d.png)
coagulation cascade
•Factor X (stuart factor, Stuart-Prower Factor, or thrombokinase) is a critical component of the blood coagulation cascade; this factor is activated into factor Xa by factor IX (Plasma thromboplastin component [PTC]/ Christmas Factor; intrinsic) and factor VII (Serum prothrombin conversion accelerator [SPCA]/ Stable factor; extrinsic) ; factor Xa
Conditions that oppose clotting
ØClot formation in intact vessels is opposed
ØSeveral factors oppose clotting
- Perfectly smooth surface of the normal endothelial lining of blood vessels does not allow platelets to adhere
- Antithrombins—substances in the blood that oppose or inactivate thrombin; prevent thrombin from converting fibrinogen to fibrin; for example, heparin
Conditions that hasten clotting
ØRough spot in the endothelium
ØAbnormally slow blood flow
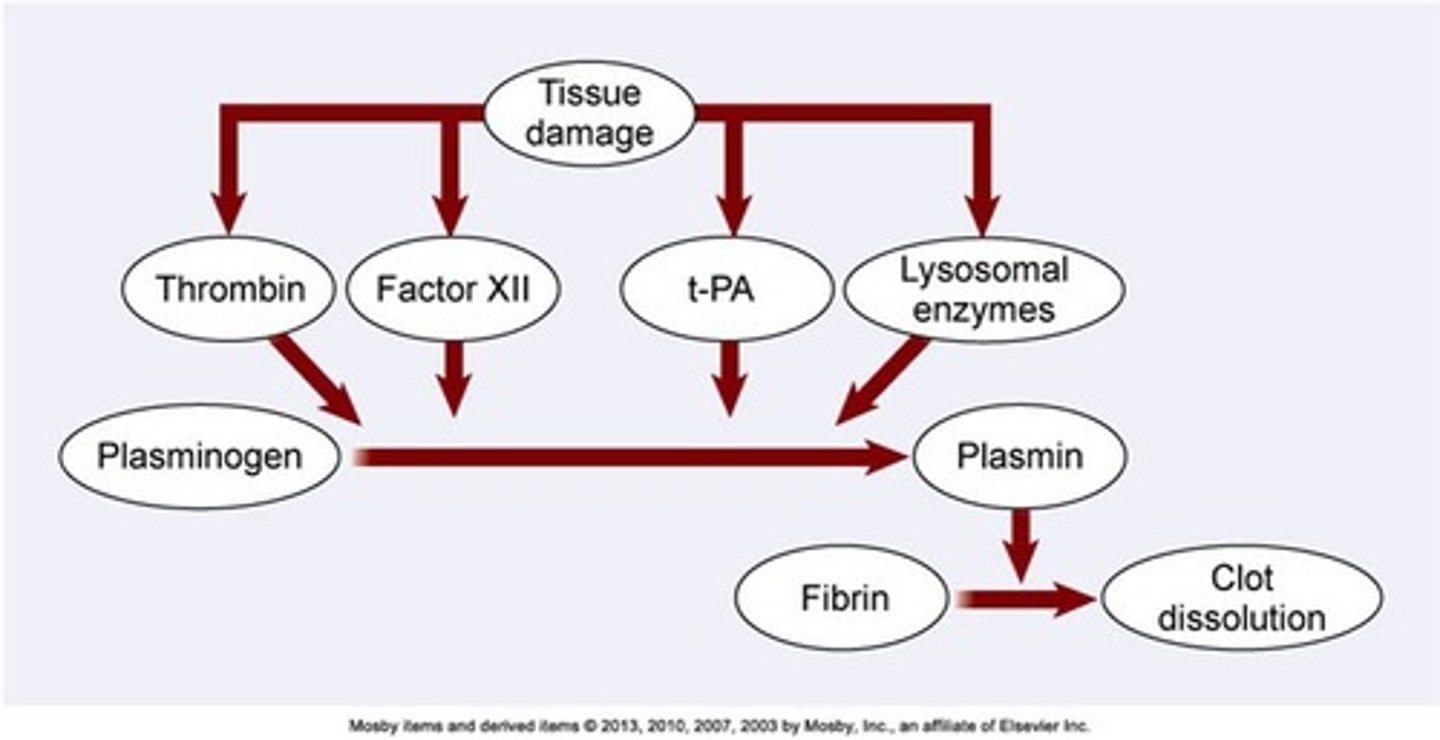
Clot dissolution
ØFibrinolysis - physiological mechanism that dissolves the clot once it has formed
ØPlasmin - enzyme in the blood that catalyzes the hydrolysis of fibrin, causing it to dissolve; it is activated by chemicals released from damaged cells and acts slowly to dissolve the clot
ØSubstances that generate plasmin can be used as a therapy to dissolve blood clots
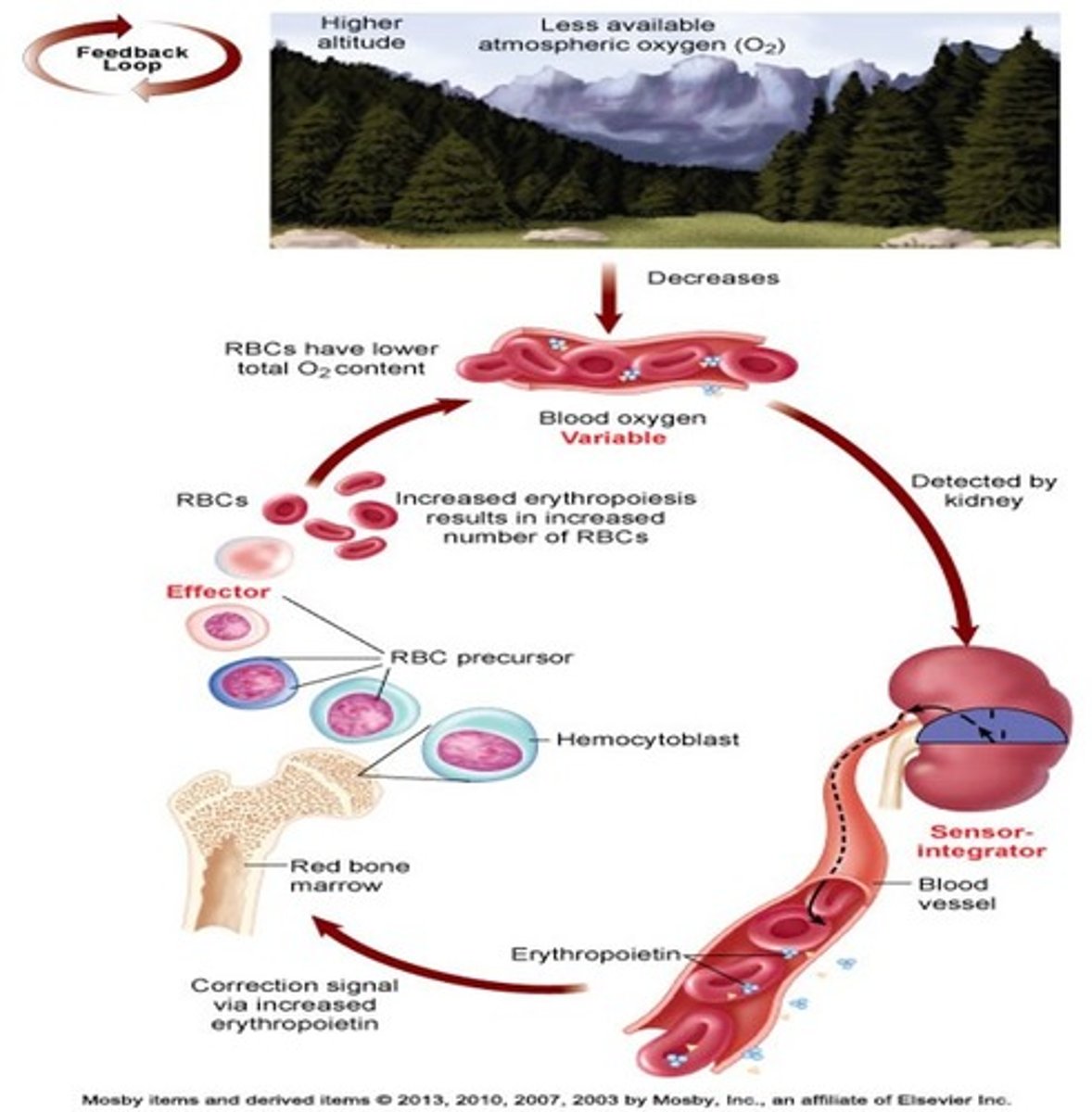
mechanism of higher altitude and the effects in the body from the less available atmospheric oxygen (O2)
low oxygen in RBC is detected by the kidney then the kidney release erythroprotein in the blood vessel afterwards the signal from the erythroprotein causes the bone marrow to produce hemocytoblast which is the precursor for erythrocytes (erythroblast) to compensate from the low oxygen in the atmosphere