Inpatient Management of Hyperglycemia and Hypoglycemia (Wang)
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
What blood glucose level is considered to be hyperglycemia?
≥ 140 mg/dL
Hyperglycemia is associated with increased morbidity and mortality, why?
Increased infections
Longer hospital and ICU length of stay
What are the three levels of hypoglycemia?
Level 1: blood glucose < 70 mg/dL and ≥ 54 mg/dL
Level 2: blood glucose < 54 mg/dL
Level 3: a severe event characterized by AMS and / or physical functioning that requires assistance from another person for recovery (irrespective of glucose level)
How does acute kidney injury (AKI) lead to hypoglycemia?
AKI can result in decreased clearance of renally-excreted oral diabetic agents and insulin
What are the renally-excreted oral diabetic medications?
Metformin
Sulfonylureas
DPP-4 Inhibitors
SGLT -2 Inhibitors
TZDs
Alpha-Glucosidase Inhibitors
What is “stress“ hyperglycemia and causes it?
It causes an increase in gluconeogenesis
It is caused by hypoxia, hemorrhage, sepsis, shock, surgery, trauma
What is the difference between enteral nutrition and parenteral nutrition?
Enteral: Method used to provide calories and nutrients directly into the GI tract
Parenteral: Method used to provide calories and nutrients directly into the bloodstream
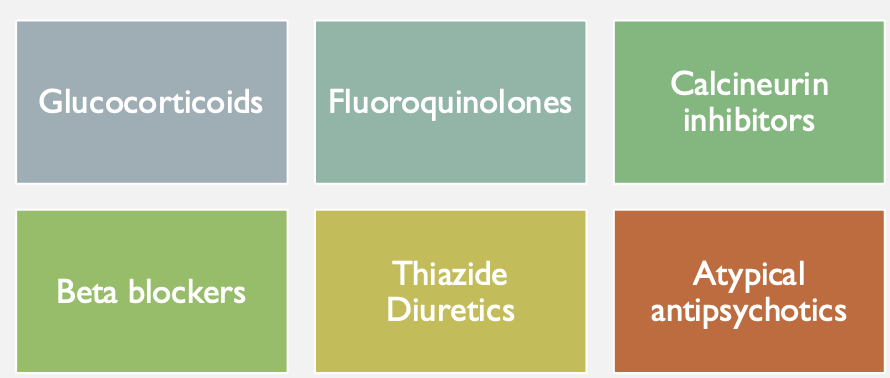
Which medications affect glucose levels?
See image
When should an A1C test be performed on hospitalized patients?
On all patients with diabetes or hyperglycemia (BG >140 mg/dL) if no A1C result is available from the last 3 months
What is the glycemic goal for the majority of non-critically ill and critically ill patients?
140-180 mg/dL
What is the glycemic goal for selected critically ill patients?
110-140 mg/dL
Who are selected critically ill patients for tighter glycemic control?
Patients with a high risk for hyperglycemia-related complications, recent major surgery, or a history of hyperglycemia
What is the risk associated with tighter glycemic control?
Greater risk of hypoglycemia
What is basal insulin?
Insulin needed to control gluconeogenesis, even when the patient is not eating
What is correctional insulin?
Insulin given to lower high blood glucose to a specific target range
What is nutritional insulin?
Insulin needed to cover carbohydrate intake from food, IV fluids with dextrose, tube feeds, or TPN
What is the difference between a basal + bolus regimen and a sliding scale?
Basal + bolus: Mimics normal insulin profile
Sliding scale: The intensity of it is selected based on the patient’s insulin sensitivity and specific glycemic goals
When should insulin be initiated in non-critically ill hospitalized patients?
For persistent hyperglycemia (minimum of two BG ≥180 mg/dL within 24 hours)
What is the preferred insulin treatment for non-critically ill hospitalized patients who are NPO or have poor oral intake?
Basal insulin OR basal + bolus insulin
What is the preferred insulin treatment for non-critically ill hospitalized patients with adequate nutritional intake?
Basal + bolus + prandial (nutritional) insulin
What should be avoided when treating hospitalized patients with insulin?
Avoid using only correctional (sliding scale) insulin without basal insulin
What does the Rabbit 2 trial claim?
Avoid use of only correctional (sliding-scale) insulin
What is the purpose of continuous IV insulin infusions?
To deliver insulin directly into the bloodstream, achieving specific glycemic goals while avoiding hypoglycemia
Where are continuous IV insulin infusions typically used?
In the ICU setting with q1h glucose checks
How is the infusion rate adjusted during continuous IV insulin infusions?
Based on glycemic fluctuations
What software system can assist with glucose management during continuous IV insulin infusions?
EndoTool
How do you calculate the total daily dose (TDD) for SQ insulin when transitioning from an IV drip?
Find the average insulin infusion rate, multiply by 24 to get 24h insulin utilization, and then calculate 80% of that value for the 24h SQ insulin requirement
When should SQ basal insulin be given when transitioning from an IV insulin drip?
Give SQ basal insulin 2 hours before stopping the insulin drip to avoid rebound hyperglycemia
What should be done with renally-excreted oral diabetic medications in hospitalized patients?
Hold these medications while the patient is hospitalized
When can metformin be resumed post-contrast administration?
Wait at least 48 hours before resuming metformin
When should SGLT2 inhibitors be initiated or continued in hospitalized patients?
In patients with T2DM hospitalized with heart failure, after recovery from the acute illness
How is hypoglycemia treated in asymptomatic/responsive patients?
15-20 grams of oral carbohydrates or D50W 50 mL IV push if NPO
How is hypoglycemia treated in symptomatic/non-responsive patients?
D50W 50 mL IV push or Glucagon 1 mg IM if no IV access is available