Block 8: Week 1: The Menstrual Cycle
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
who mensurates?
females who are:
of post-pubertal age.
of pre-menopausal age.
who haven’t suffered POF (premature ovarian failure).
who are not severely under or overweight.
who are not pregnant.
what is premature ovarian failure?
menopause before age of 35,
can happen as early as 17
what is GnRH?
Gonadotropin Releasing Hormone - binds to GnRH receptors.
can GnRH cross the cell membrane? why? what does this mean?
NO - it is a neuropeptide and so can’t cross phospholipid membrane.
This means it can only act on cells which have the GnRH receptor!
what neuropeptide is involved in menstruation?
GnRH - Gonadotropin Releasing Hormone
what glycoproteins are involved in menstruation?
Luteinizing Hormone (LH).
Follicle Stimulating Hormone (FSH).
Chorionic Gonadotropin (CG).
are LH and FSH male or female hormones?
both! important in both men and women
what is common/different in LH/FSH/CG?
are heterodimers with a common alpha chain and unique beta chains
what is the common biochemical precursor to steroids?
cholesterol (not dietary cholesterol, cholesterol synthesised from acetate).
what are the 4 classes of steroids?
progestagens (21C).
androgens (19C).
oestragens (18C).
corticosteroids.
how are steroids classed?
based on number of carbons:
progestagens (21C).
androgens (19C).
oestragens (18C).
corticosteroids.
what type of receptor is needed for steroids?
nuclear receptor within the cell (CAN pass through membrane).
what factors regulate hormone concentration and activity?
receptor levels.
hormone production rate.
clearance rate.
binding proteins.
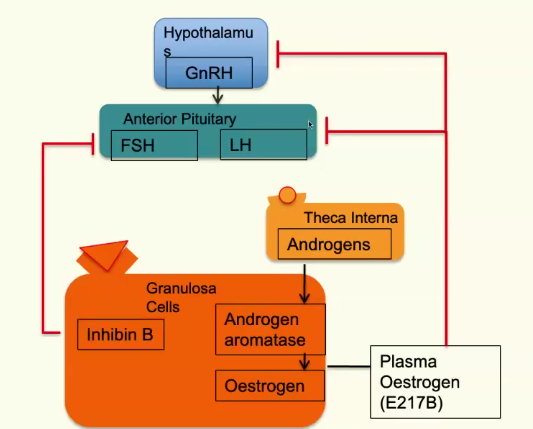
where does GnRH act? what does this cause?
on cells with its receptor in the anterior pituitary.
this causes FSH and LH release.
oogenesis: when is mitotic stage?
mitotic stages of oogenesis all completed by birth
oogenesis: when is first meiotic stage?
in fetal ovary, enters the first meiotic stage, forming germinal vesicles,
BUT reside as primary oocytes in the primordial follicle, surrounded by granulosa cells.
many primordial oocytes are lost shortly after birth.
when does meiosis restart in oogenesis?
restarts at puberty
what is cytodifferentiation? when does this happen?
go from primordial follicle to oocyte that can be fertilised.
completed in ovarian cycle
what makes up the primordial follicle?
1. The primordial oocyte
2. Single layer of granulosa cells – originate from celomic epithelium.
3. Mesenchymal cells – supporting cells
4. Surrounding membrane – theca cells.
how often do primordial follicles mature?
Every ~90 minutes, one of these follicles will develop and mature
how do we go from a primordial follicle to primary follicle?
primordial follicle will expand and get bigger - no changes besides this
how long to go from a primordial follicle to primary follicle?
over 70 days
what is theca?
outer layer of primary follicle differentiates, forming theca
what is follicular trickle?
primordial → primary → secondary (antral) follicles
what is atresia?
death of follicle
how is a tertiary (Pre-ovulatory) follicle formed?
FSH and LH prevents the atresia (death) of secondary follicle.
allows follicle to continue to grow to tertiary.
what is antrum?
fluid-filled cavity found within secondary (antral) follicle which will expand to form mature follicle after LH/FSH action.
what are the two phases of ovarian cycle?
follicular phase and luteal phase
when does follicular phase begin and end?
begins first day of menses and ends with ovulation.
simply, what is happening in follicular phase?
follicle is growing and developing over 14 days.
how often is GnRH released from hypothalamus?
pulse of GnRH released every hour.
where are LH receptors found?
on theca interna (membrane surrounding the follicle).
where are FSH receptors found?
granulosa cells (found one further in than theca cells in developing follicle).
when LH binds to LH receptors on theca interna, what is released?
androgens
when FSH binds to FSH receptors on granulosa cells, what is released?
androgen aromatase
what is the interaction between granulosa cells, theca interna, LH and FSH?
LH binds to theca interna, releasing androgens.
FSH binds to granulosa cells, releasing androgen aromatase.
androgen + androgen aromatase → oestrogen
how does oestrogen impact the hypothalamus?
oestrogen inhibits hypothalamus, preventing GnRH release and so inhibits LH/FSH release from anterior pituitary.
what is androgens impact on granulosa cells?
promote granlosa cells proliferation - follicle grows MORE, so more OESTROGEN.
what do granulosa cells release as follicle develops? what does this mean?
granulosa cells release AMH which prevents growth of neighbouring follicles.
dominant follicle persists at the expense of other follicles.
what change in LH occurs as oestrogen levels surge with dominant follicle growth?
Surge in oestrogen levels → oestrogen upregulates granulosa cells.
There is an increase in LH receptor expression.
This overcomes negative feedback on anterior pituitary, stimulating LH production.
LH surges and acts on theca cells and granulosa cells - OVULATION.
what happens once dominant follicle is established?
ovulation: progesterone is released, oestrogen is reduced.
what is LH role in oocyte maturation?
at LH surge with ovulation, oocyte resumes meiosis and undergoes “division” - nuclear maturation.
what is unique about the nuclear maturation of the oocyte?
it is unequal - most cytoplasm retained in secondary oocyte,
half of the chromosomes lost on 1st polar body.
second meiosis begins and oocyte arrests again at metaphase.
what happens to the cytoplasm during oocyte maturation?
cytoplasm is reorganised:
mitochondria relocate to periphery.
cortical granules migrate to periphery.
what happens to the granulosa cells during oocyte maturation?
granulosa cells undergo expansion to form cumulus cells.
when does luteal phase begin?
at ovulation when ruptured follicle forms corpus luteum
what are the key hormones in luteal phase?
oestrogen and progesterone.
LH and FSH decrease.
what are the phases of the uterine cycle?
menstrual phase.
proliferative phase.
secretory phase.
what happens in proliferative phase of uterine cycle?
endometrium and myometrium begins to regrow - oestrogen.
preparing for possible pregnancy.
cervical mucal secretions change.
what happens in secretory phase of uterine cycle?
blood supply to endometrial tissues remodeled.
cervical secretions change again.
supported by progesterone.
oestrogen types: 17-b-Estradiol vs Estrone vs Estriol?
different potencies:
17-b-Estradiol MOST - not found after menopause.
Estrone and Estriol lower - associated with menopause.
what is in the morning after pill?
very high progesterone to force menstruation
what is menorrhagia?
heavy periods
what are causes of menorrhagia?
may be normal.
first menses or towards menopause.
polycystic ovary syndrome (PCOS), fibroids, endometriosis, adenomyosis and pelvic inflammatory disease.
Von Willebrand disease.
anticoagulant medicines and chemotherapy medicines.
what are treatments of menorrhagia?
contraception, (e.g intrauterine system (IUS) or combined contraceptive pill).
drugs to reduce the bleeding (e.g tranexamic acid).
anti-inflammatory painkillers (e.g mefenamic acid or naproxen).
what are measures to see if periods are excessively heavy?
need to change your pad or tampon every 1 to 2 hours, or empty your menstrual cup more often than is recommended.
need to use 2 types of period product together, such as a pad and a tampon.
have periods lasting more than 7 days.
pass blood clots larger than about 2.5cm (the size of a 10p coin).
bleed through to your clothes or bedding.
avoid daily activities, like exercise, or take time off work because of your periods.
feel tired or short of breath a lot.