carbohydrate metabolism
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
metabolism of carbs stage 1
occurs extracellularly in GI tract
Complex molecules → building block molecules → absorbed from the GI tract into circulation via F.D by GLUT 1-5 transporters
C-N and C-O bond broken (no C-C broken)
No energy produced
What enzyme breaks down starch and glycogen and what does it break it down into?
Amylase
starch/ glycogen → dextrins → monosaccharides
What type of enzymes are released by the small intestine? Give examples
Disaccharidases
lactase
Sucrase
Pancreatic amylase (break alpha-1,4 bonds)
Isomaltase (breaks alpha-1,6 bonds)
metabolism of carbs stage 2
Occurs intercellularly (in cytosol/ mitochondria)
Building block molecules → simpler molecules
C-C bond broken → some energy (ATP) produced
Oxidative (required coenzymes eg.NAD+ which gets reduced)
What are the functions of glycolisis?
yields NADH (used for reduction)
2 ATP Per mol glucose (exergonic reaction)
Produces C6 and 2 C3 (Pyruvate) intermediates
Lactate can be produced with low O2 from Pyruvate
Why is lactase production important and how is it removed?
Pyruvate is reduced to lactate
Regenerates NAD+ needed for glycolysis
Metabolised by liver and heart and disposed in the kidney
What are some important glycolysis intermediates?
Dihydroxyacetone phosphate (DHAP) → glycerol phosphate (lipid regulation ??)
1,3-BPG → 2,3-BPG (affects haemoglobin affinity)
What is the difference between hyperlactatemia and lactic acidosis?
Hyperlactatemia: conc of lactose 2-5mM (below renal threshold so no change in blood pH)
Lactic acidosis: >5mM of lactose (above renal threshold so blood pH decreases)
Function of Penrose phosphate pathway
Produce NADPH
(In RBC): maintaining free -SH (thiol) groups on cysteine residues (important in G6PDH deficiency)
Produces C5 ribsose sugar for synthesis of nucleotides
How can fructose and galactose be metabolised?
Fructose: converted to G-3-P and enters glycolisis pathway
Galactose: converted to G-1-P which is converted to G-6-P and enters glycolysis / can be converted to glycogen
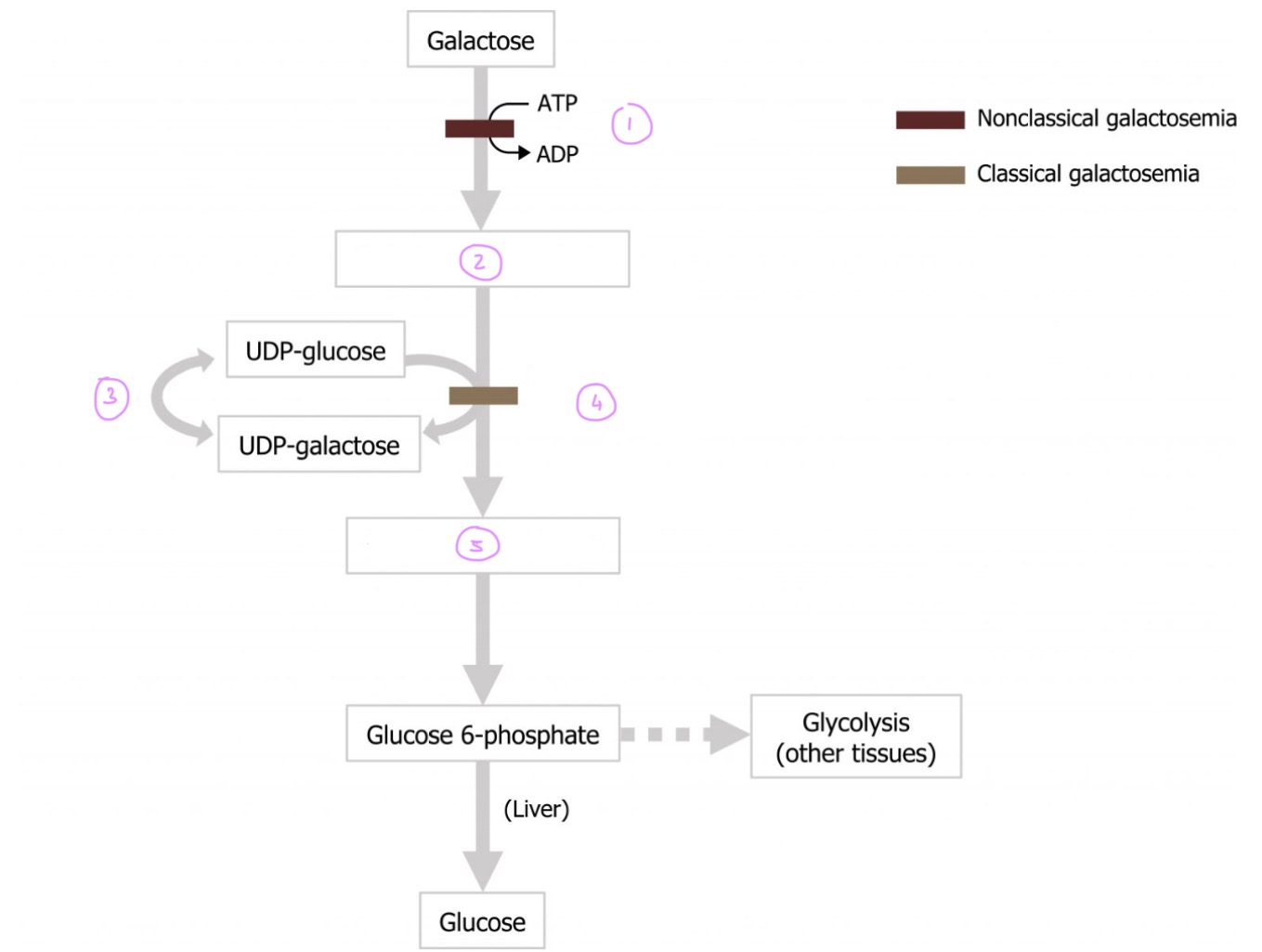
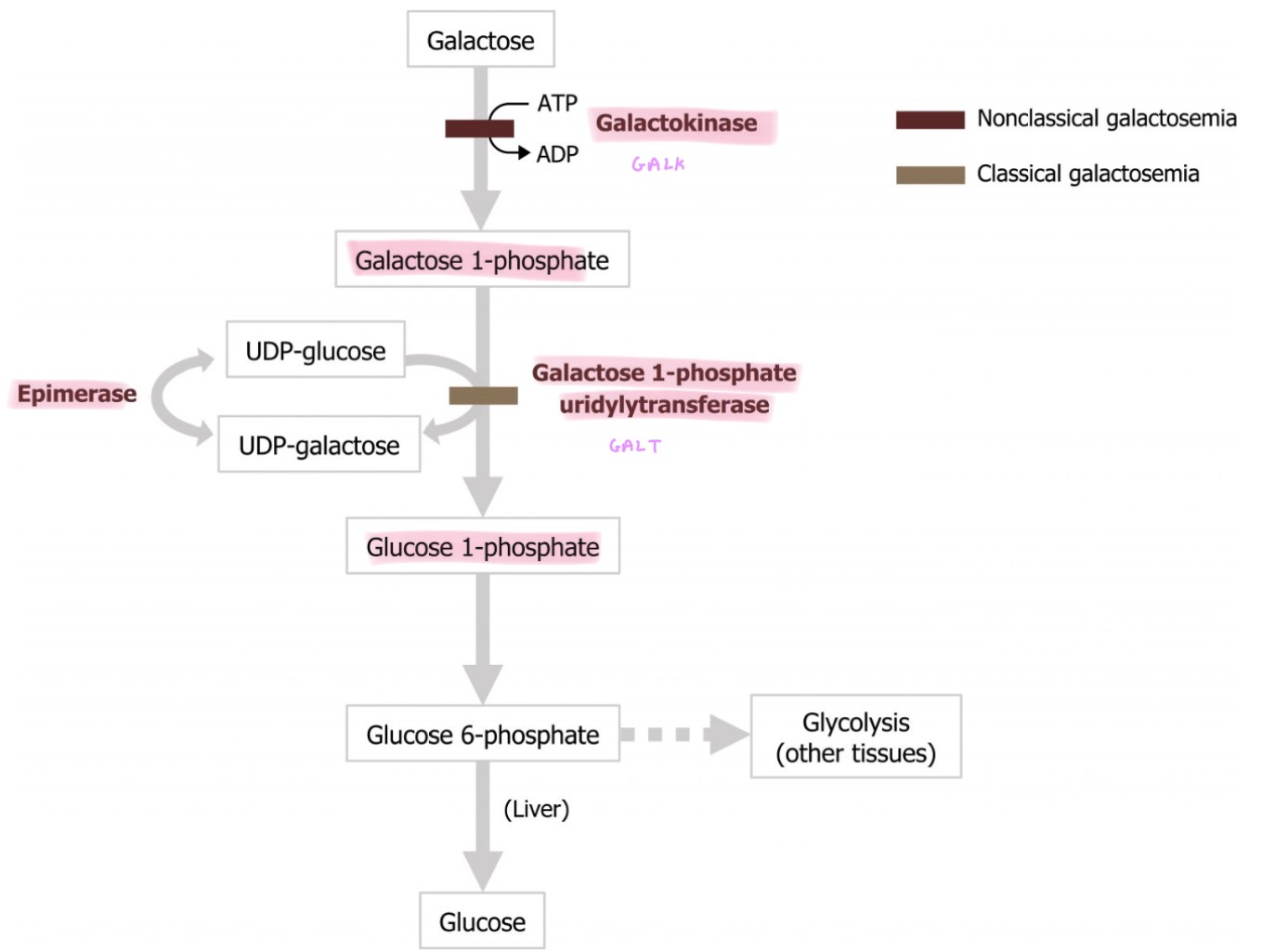
What is classical galactosaemia and what are the symptoms?
Deficiency In GALT → accumulation of galacticol which depletes NADPH from tissues
Symptoms: cataracts, glaucoma, damage to liver, brain and kidney
Treatment: non lactose diet
what is non-classical galactosaemia and what are its symptoms?
Deficiency in galactokinase (GALK)
Milder symptoms of cataracts, liver disease and delayed growth development
How is acetyl CoA made?
Pyruvate → acetate + CoA → acetyl CoA
(Releases CO2)
Enzyme: Pyruvate dehydrogenase(allosteric regulator)
What is Pyruvate dehydrogenase (PDH) activated by?
Pyruvate
NAD+
ADP
Insulin
Dephosphorylation
What is Pyruvate dehydrogenase (PDH) inhibited by?
acetyl CoA
NADH
ATP
phosphorylation
What is lactic acidemia Leigh’s disease?
Also know as Necrotising encephalopathy
Deficiency in PDH → high Pyruvate → high lactic acid → acidic blood
X-linked recessive
What does the TCA/ kerbs cycle produce?
1 ATP
3 NADH
1 FADH2
2 CO2
What are the intermediates of the TCA cycle used for?
C4-5: biosynthesis of non-Essential A.A eg. Succinate, fumerate
C4: Biosynthesis of human and glucose eg. Alpha-ketoglutaric acid
C6: Biosynthesis of fatty acids eg. Citric acid, isocitric acid
What regulated the TCA cycle?
ATP/ADP ratio (high ADP is a low energy signal → telling the body we need more energy)
NADH/NAD+ ratio (High NADH is a high energy signal → telling the body we don’t need more energy)
What is stage 4 and where does it happen?
Oxidative phosphorylation occurs on mitochondrial inner membrane Cristae)
Uses NADH + FADH2
What happens to the oxygen in oxidative phosphorylation?
O2 + 2H+ → 2H2O at the complex IV
How is ATP made in oxidative phosphorylation?
NADH + FADH are oxidised releasing H+ + e-
e- move down ETC releasing energy
Energy is used to pump H+ across
H+ move down conc gradient through ATP Synthase (complex V): ADP + H+ → ATP
how is mitochondrial deficiency bad?
loss of efficiency in ETC → less ATP
DNA mutations → abnormal components of respiratory chain
What types of poisons can stop oxidative phosphorylation?
Uncoupling agents (UCP 1-5) are important for heat production
Inhibitors of UCP 1-5: Inhibit transport of electrons so no ATP produced → no heat
How can cyanide poisoning affect the metabolism of carbs ?
?