A&P Quiz 10 (Ch 28 pt 2)
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
Male Accessory Glands
exocrine glands that secrete products into the ducts of the male reproductive tract
3 Accessory Glands of Male Reproductive System
seminal vesicles
prostate gland
bulbourethral glands
Seminal Vesicles
accessory gland of male reproductive system, sac-shaped glands, located next to the ampullae of the ducta deferentia, 5 cm long, tapers into a short excretory duct that joins the ampulla of the ductus deferens to form the ejaculatory duct, covered by fibrous connective tissue capsule containing smooth muscle cells
Prostate Gland
resembles a walnut, 4 cm long and 2 cm wide, located dorsal to the pubic symphysis at the base of the urinary bladder, surrounds the prostatic urethra and two ejaculatory ducts
Layers of Prostate Gland
consists of glandular and muscular tissue, covered by a fibrous connective tissue capsule containing distinct smooth muscle cells and many fibrous partitions that radiate into the prostate gland
Cells of Prostate Gland
muscular partitions are covered by columnar epithelial cells that secrete prostatic fluid
15-30 small prostatic ducts empty secretions into the prostatic urethra
Bulbourethral (Cowper) Gland
pair of small glands located near the membranous urethra, compound mucus gland, small ducts from each gland unite to form a single duct that empties into the spongy urethra and the base of the penis
Changes in Bulbourethral Gland Over Lifetime
young males: each gland is the size of a pea
decrease in size with age until they are almost impossible to detect in older males
Semen
composed of sperm cells and secretions from accessory glands
Percentages of Semen
60% of fluid is produced by the seminal vesicles
30% of fluid is produced by the prostate gland
5% of fluid is produced by the testes
5% of fluid is produced by the bulbourethral glands
Testes Contribution to Semen
produce sperm cells, secrete small amount of fluid to allow sperm cells to move through reproductive tract that also contains metabolic by products produced by the sperm cells
Sperm Cells
major components of testicular secretions
Bulbourethral Glands & Urethral Mucous Glands Contribution to Semen
produce alkaline mucous secretion just before ejaculation
Functions of Alkaline Mucous in Semen
lubricate the urethra for sperm movement
neutralize the acidic fluids in the spongy urethra
provide small amount of lubrication during intercourse
reduce vaginal acidity
Seminal Vesicles Contribution to Semen
produce thick mucus secretions that function in nourishment of sperm cells, coagulation of semen, and movement of sperm
3 Functions of Mucus Secreted by Seminal Vesicles
nourishment of sperm cells
coagulation of semen
movement of sperm
Nourishment of Sperm Cells
function of mucus secretion from seminal vesicles, fructose, citric acid, and other nutrients
Coagulation of Semen
function of mucus secretion from seminal vesicles, fibrinogen that is involved in a weak coagulation reaction immediately after ejaculation
Movement of Sperm
function of mucus secretion from seminal vesicles, prostaglandins stimulate uterine contractions to help move sperm through the female reproductive tract
Prostate Gland Contributions to Semen
produces thin milky alkaline secretion, fibrinolysin causes the mass of semen to dissolve to release sperm cells into the reproductive system
3 Functions of Prostate Gland Contributions to Semen
helps neutralize acidic urethral pH (with secretions from seminal vesicles, bulbourethral glands, and urethral mucous glands)
help neutralize acidic secretions of testes and vagina (with secretions from seminal vesicles)
important for transient coagulation of semen due to containing clotting factors that activate fibrinogen
Semen Sperm Count
normal sperm count ranges from 75-400 million sperm per milliliter of semen, normal ejaculation consists of 2-5 mL of semen, semen with highest sperm count is expelled first
Sperm After Ejaculation
sperm cells become motile after ejaculation (alkaline pH, nutrients, and removal of inhibitory substances from sperm cell surface increases motility), enzymes in acrosomal cap help digest a path through mucoid fluids of the female reproductive tract and through materials surrounding the oocyte
Control of Male Reproduction
under both hormonal and nervous control
5 Hormone Responses in Male Reproduction
development of reproductive structures
maintenance of their functional capacities
development of secondary sexual characteristics
control of sperm cell formation
influence sexual behavior
2 Neural Controls of Male Reproduction
sexual behavior
control the sex act
4 Male Reproductive Hormones
gonadotropin releasing hormone
luteinizing hormone
follicle-stimulating hormone
testosterone
(testes produce small amts of estrogen and progesterone)
GnRH in Males
stimulates large quantities of secretion of LH and FSH only when GnRH is produced in a series of pulses, secreted from hypothalamus
LH in Males
stimulates synthesis and secretion of testosterone, secreted from anterior pituitary
FSH in Males
supports spermatogenesis, secreted from anterior pituitary
Testosterone in Males
major male hormone secreted by the testes, supports spermatogenesis, stimulates development and maintenance of reproductive organs, causes development of secondary sexual characteristics
inhibits gnhr, lh, and fsh secretion through negative feedback
Regulation of Male Reproductive Hormone Secretion Involves
hypothalamus
pituitary gland
testes
Androgen
stimulates development of male reproductive structures and male secondary sexual characteristics
2 Conversions of Testosterone
some target cells (penis, scrotum) convert testosterone to dihydrotestosterone
other target cells (brain) convert testosterone to estrogen
Human Chorionic Gonadotropin (hCG)
gonadotropin-like hormone secreted by the placenta that stimulates the secretion and synthesis of testosterone by fetal testes
Puberty in Males Immediately After Birth
no stimulation is present and testes of newborn baby atrophy slightly and secrete only small amounts of testosterone
Males Before Puberty
gnhr release from hypothalamus is inhibited by small amounts of testosterone and other androgens
Puberty
age at which individuals become capable of sexual reproduction
Male Puberty
hypothalamus becomes less sensitive to inhibitory effect of androgens and gnhr secretion increases
gnhr increase lh and fsh secretion from anterior pituitary
fsh promotes sperm production
lh causes interstitial cells to secrete large amounts of testosterone
testosterone has negative feedback effect on gnrh but cannot completely suppress it after puberty
Androgen Production
produced by interstitial cells of testes, includes testosterone, small amounts of androgens are also produced by adrenal cortex and possibly the sustentacular cells
3 Effects of Testosterone
causes enlargement and differentiation of male genitals and reproductive system
necessary for sperm cell formation
affects development of secondary sexual characteristics
1-4 Male Secondary Sex Characteristics
growth of thicker, coarser, pigmented hair in pubic area extending up the linea alba, legs, chest, axillary region, face, back
coarser texture of the skin
darker skin color
increases secretion of sebaceous glands (face)
5-8 Male Secondary Sex Characteristics
hypertrophy of the larynx and reduction of tension on vocal folds
stimulates metabolism
increases erythropoietin production (increases rbc count)
minor mineralocorticoid-like effect causing na+ to be retained and increase body fluid volume
9-11 Male Secondary Sex Characteristics
promotes protein synthesis in most tissue- increasing skeletal muscle mass
growth of bone is stimulated as testosterone is converted to estrogen causing increased ca+2 deposition
sex hormones also stimulate ossification of the epiphyseal plate to stop growth
Testosterone in Male Sexual Behavior
require to initiate and maintain, enters cells in the hypothalamus and surrounding brain regions influencing their function resulting in sexual behavior, may depend on conversion of testosterone to other steroids (estrogen)
Testosterone Levels
stay consistent from puberty to age 40
slowly drop to about 20% of that amount by age 80
causes slow decline in sex drive and fertility
Male Sex Act
complete series of reflexes that result in erection of penis, secretion of mucus into the urethra, emission, ejaculation, orgasm, and resolution
Emission
discharge of all secretions from ducta deferentia into the urethra
Ejaculation
forceful expulsion of semen from urethra caused by contraction of the urethra, skeletal muscles in the pelvic floor, and muscles at the base of the penis
Orgasm
climactic sensation associated with ejaculation as a result of pleasurable sensation during the male sex act
Resolution
follows ejaculation and is characterized by flaccid penis, overall feeling of satisfaction, and inability to achieve erection and second ejaculation for a period of time
Sensory AP and Integration of Male Sex Act
initiated by a variety of sensor stimuli
sensory input is integrated in the sacral region of the spinal cord
input travels to the cerebrum for conscious sexual sensations
input from the cerebrum can reinforce the sacral reflexes but are not required for culmination of the male sex act
Male Sex Act with Spinal Cord Injury
male sex act can be performed by males with spinal cord injuries superior to the sacral region
Sensor Stimuli of Male Sex Act
rhythmic mechanical stimulation of the penis (glans penis) are extremely important for initiation of erection and ejaculation
stimulation of the surrounding tissue (scrotum, anal, perineal, and pubic regions)
engorgement of the prostate and seminal vesicles
mild irritation of the urethra (infection)
psychological stimuli (sight, sound, odor, thoughts) can also inhibit male sex act
Erection
first major component of male sec act, penis becomes enlarged and rigid, ap travels from the spinal cord via the pudenal nerve to the arteries of the erectile tissue, release of ach and nitric oxide cause smooth muscle to relax and blood vessels to dilate, other arteries constrict to shunt blood to the erectile tissue, blood filling the erectile tissue compresses the veins and partially occludes them, input comes from parasympathetic centers (s2-s4) or sympathetic centers (t2-l1) but parasympathetic input is normally more important
Parasympathetic AP in Male Sex Act
also cause mucous glands in the penile urethra and the bulbourethral glands to secrete mucus
Emission Steps
accumulation of sperm cells and secretion of the accessory gland in the urethra, sympathetic centers (T12-L1) are stimulated as the level of sexual tension increases, sympathetic AP cause peristaltic contractions of the reproductive ducts and stimulate seminal vesicles and prostate gland secretion, causes accumulation of semen in the prostatic urethra, produces sensory AP that pass via the pudendal nerves to the spinal cord, integration of sensory AP causes both sympathetic and somatic motor output
Ejaculation Steps
sympathetic AP cause internal urethral sphincter to constrict preventing mixing of semen and urine, somatic motor AP cause contraction of skeletal muscle of the urogenital diaphragm to contract, results in rhythmic contraction that forces semen out of the urethra
Female Reproductive System Consists of
ovaries
uterine tubes
uterus
vagina
external genital organs
mammary glands
Female Internal Reproductive Organs
in the pelvic cavity between the urinary bladder and rectum, uterus and vagina at the midline with ovaries on either side, held in place by a group of ligaments (broad ligament)
Broad Ligament
extension of peritoneum that spreads out on both sides of the uterus and attaches to the ovaries and uterine tubes
Ovaries
female gonads, small organs (2-3.5 cm long, 1-1.5 cm wide)
Mesovarium
peritoneal fold attached to each ovary on the posterior surface of the broad ligament
Suspensory Ligament
extends from mesovarium to the body wall
ovarian arteries, veins, and nerves travel with the suspensory ligament and enter the ovary through the mesovarium
Ovarian Ligament
attaches the ovary to the superior margin of the uterus
Ovarian (Germinal) Epithelium
visceral peritoneum covering ovary, composed of simple cuboidal epithelium
Tunica Albuginea
capsule of dense fibrous connective tissue directly below the ovarian epithelium
2 Regions of Ovary
cortex
medulla
Ovarian Cortex
dense outer portion, ovarian follicles containing oocytes distributed throughout the stroma
Ovarian Medulla
looser inner portion, blood vessels, lymphatic vessels, and nerves from mesovarium enter the medulla
Stroma
connective tissue of the ovary
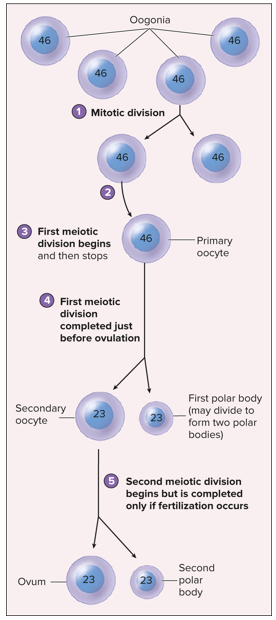
Oogenesis
production of gametes in females, begins before female is born, by the 4th month of development the ovaries have 5 million oogonia (cells from which oocytes develop), by birth many oogonia degenerate and the remaining ones have differentiated into cells that have begin meiosis, oogonia can form after birth from stem cells but for how long is unclear
Oogonia in Oogenesis
increase in number by mitosis during development, before birth most have differentiated into primary oocytes
Primary Oocytes in Oogenesis
diploid cells, begin meiosis i but stop at birth during prophase i
Oogenesis Continuation at Puberty
primary oocytes reenters and completes meiosis i just before ovulation, cytoplasm is not split evenly between two haploid cells, larger becomes secondary oocyte wile smaller becomes second polar body that can either degenerate or divide to produce second polar bodies that degenerate
Ovulation
release of the secondary oocyte from the ovary, secondary oocyte begins meiosis ii but stops in metaphase ii unless fertilization occurs
When does fertilization begin?
fertilization begins when sperm cells penetrates the cytoplasm of the secondary oocyte, secondary oocyte completes meiosis ii and divides unevenly, larger cell is ovum and smaller cell is a second polar body that degenerates
Oogenesis Diagram
Fertilization
23 chromosomes from the sperm cell nucleus join with 23 chromosomes from the oocytes to forma zygote, zygote has 23 pairs of (46) chromosomes and divided by mitosis to increase number of cells, 7 days after ovulation the mass of cells implants in the uterine wall, develops for 9 months to form a new individual
Follicle Development
ovarian follicles in the ovarian cortex, follicles contain developing primary oocytes, follicles develop as primary oocytes progress through meiosis i
Ovarian Cycle
reoccurring events that take place in the ovaries of sexually mature nonpregnant females, hormonally regulated
Primordial Follicle in Follicle Development
houses the primary oocytes at birth
Granulosa Cells
single layer of flat cells that surround the primary oocyte in the primordial follicle
Primary Oocytes in Follicle Development
2 million present at birth, decreases to 300,000-400,000 at beginning of puberty, about 400 primary oocyte complete development to secondary oocyte
Follicular Development at Puberty
some primordial follicles become primary follicles, oocyte enlarges, granulosa cells thicken and become cuboidal in shape and can increase in number of layers, formation of zona pellucida
Zona Pellucida
layer of clear material that is deposited around the oocyte during puberty when primordial follicles become primary follicles
Secondary Follicle in Follicular Development
about every 28 days hormonal changes stimulate primary follicles to continue to develop into secondary follicle, secondary follicle continues to enlarge to become a mature (graafian) follicle, oocyte is pushed to one side and lies in a mass of granulosa cells called the cumulus cells (cumulus oophorus)
Vesicles in Secondary Follicle
fluid filled spaces form among the granulosa cells when primary follicle develops into secondary follicle
Theca
capsule that forms around the follicle during development from primary to secondary, two layers
2 Layers of Theca
theca interna
theca externa
Theca Interna
layer of theca that surrounds the granulosa cells and synthesize ovarian hormones
Theca Externa
layer of theca that is primarily connective tissues and merges with the stroma of the ovary
Antrum
single fluid filled chamber created by the fusion of vesicles when secondary follicle develops into mature follicle
Follicular Development Diagram
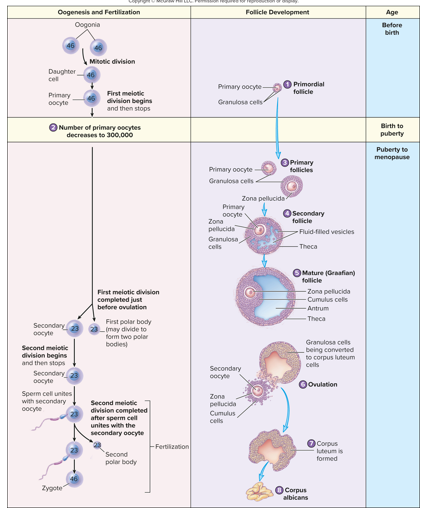
Mature Follicle in Follicular Development
forms a lump on the surface of the ovary, only one mature follicle undergoes ovulation and the rest degenerate (atresia)
ruptures during ovulation to release blood, follicular fluid, and oocyte surrounded by cumulus cells (corona radiata) into the peritoneal cavity
Corpus Luteum
endocrine structure produced by remains of follicle, convoluted appearance as a result of collapse, enlarges and remains active through the first trimester of pregnancy if it occurs (corpus luteum of pregnancy)
Luteal Cells
granulosa cells and theca interna that enlarge and secrete progesterone and smaller amounts of estrogen
Follicular Development if Pregnancy Does Not Occur
corpus luteum remains functional for 10-12 days and then begins to degenerate
decreasing progesterone and estrogen secretions
corpus albicans develops, shrinks, and eventually disappears (month to years)
Corpus Albicans
whitish structure that is produced as the connective tissue cells of the corpus luteum enlarge and become clear