Stages of Tissue Healing & Phases of Rehab
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What is the timeline of the acute stage of healing? (Reaction and inflammation)
4-6 days (<1 week)
What are some clinical signs someone is in the acute stage of tissue healing?
Pain at rest
Pain with ROM before tissue resistance (empty end feel)
Loss of function
Impaired movements
Muscle guarding.
What is the timeline of the subacute stage of healing? (Proliferation, repair, and healing)
~10-17 days (ie. 2-3 weeks after the injury) .
Up to 6 weeks or longer depending on the tissue involved, extent of injury, and the patient demographics/characteristics.
This stage is divided into early and late sub-acute phases.
What occurs to inflammation during the subacute stage of healing?
Progressively decreases and eventually will be absent.
What is the clinical sign of the subacute stage of tissue healing?
No pain at rest
Pain with ROM when available tissue resistance is met (has an end feel)
Pain when tissue is stretched or stressed beyond tolerance.
Muscles may test weak
Function is limited by pain or weakened tissue.
Pain is typically at moderate levels during movement and should be decreasing as time progresses.
What is the timeline of the chronic stage of healing? (maturation and remodeling)
6 months-1 year
Often divided into early and late phases.
Is there still inflammation in the chronic stage of tissue healing?
No, it should be absent.
What are the clinical signs of the chronic stage of tissue healing?
Pain may be present after tissue resistance is met or at the end of available ROM (anatomic limit) or with stretching tight structures.
Contractures or adhesions may be present limiting ROM
Ongoing weakness, poor endurance, or poor neuromuscular control may limit function.
*Pain is usually mild at this stage and is improving as time progresses.
What is the 4th stage of tissue healing?
Chronic inflammation or pain
What typically causes the 4th stage of tissue healing to occur?
The connective tissue is repeatedly stressed beyond the ability to repair itself and the inflammation process is perpetuated.
What are the clinical symptoms of the chronic inflammation/pain stage of tissue healing?
Symptoms of increased pain, swelling, and muscle guarding that lasts more than several hours after activity.
May also complain of increased stiffness after periods of rest, loss of ROM 24 hrs after activity, with possible progressive loss of ROM if irritation persists.
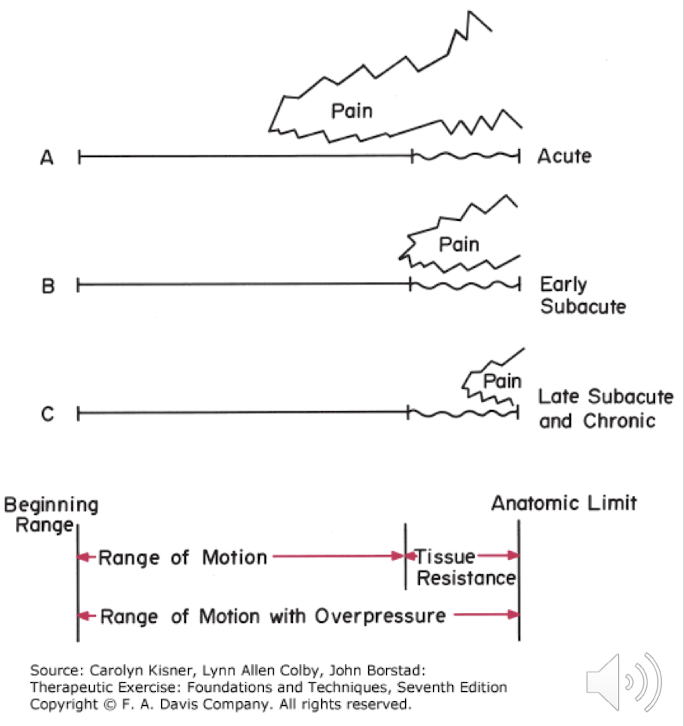
Explain the relationship between ROM, pain, and the stages of tissue healing.
Acute stage
The pain begins before the available tissue resistance and at rest.
Pain begins before way before anatomic limit.
Early subacute stage
Pain is synchronous with encountering tissue resistance at the end of available ROM.
Pain occurs only when the newly developing tissue is stressed beyond its tolerance or when tight tissue is stressed
Late subacute and chronic stage
A stretch pain may be felt when testing tight structures at the end of their available range
What is phase 1 of rehabilitation called?
Maximum protection
What impairments are seen in phase of the rehabilitation process?
Inflammation
Pain at rest
Edema
Muscle spasm
Impaired movements
Restricted use of associated areas
Explain the PT interventions that will be used if someone is in phase 1 of rehabilitation.
The PT interventions will be directly related to the impairments the patient presents with (up to 1 week post-injury)
What does the plan of care consist of in phase 1 of rehabilitation?
Educate the patient
Recovery time, assistive devices, sleep, etc.
Control pain, edema, and spasms.
Ice, compression, elevation, gentle massage for spasms, grade 1-2 joint mobilizations.
Maintain soft tissue and joint integrity and mobility.
PROM with no reproduction of pain, isometrics with no increase in pain, E-stim
Maintain integrity and function of associated areas (prevent negative effects of immobilization)
Aerobic exercise depending on the proximity to the concerned area, gait training with assistive device, AROM/AAROM in joints around concerned area.
What are contraindications during phase 1 of rehab?
Stretching and resistance exercises should NOT be performed at the site of inflamed or swollen tissue.
What is phase 2 of rehabilitation called?
Moderate protection/controlled motion
What impairments are present with phase 2 of rehab?
Pain when end of available ROM is reached/resistance met
Swelling still apparent but decreasing
Loss of ROM
May have contracture
Muscle weakness from pain or limited use
Restricted ADL’s and IADL’s
Explain the plan of care during phase 2 of rehab
Educate the patient
Review anticipated recovery time, how PT can help, etc.
Promote healing of injured tissues
Monitor response of tissue with exercise prescription, decrease intensity or ROM if pain or inflammation occurs. Continue with joint protection or AD until no longer needed.
Restore soft tissue and joint integrity and mobility
AAROM of involved area that is within limits of pain, increase mobility of scar, progressively increase mobility of related structures if limited ROM is due to tightened structures, joint mobs (gr. 1-4), PNF stretching
Develop neuromuscular control, muscular endurance, and strength in involved and related muscles (restore full and pain-free ROM)
Progress to multi-stage isometrics and initiate AROM when pain free and motion ha improved.
Maintain integrity and function of associated areas
Continue with aerobic exercise as tolerated, progressive and resistive exercises of uninvolved area.
When is discomfort a red/yellow flag during phase 2 of rehab?
Discomfort will occur as level is progressed, but it should not last more than a couple of hours.
What is phase 3 of rehab called?
Minimum to no protection (return to function)
What are some impairments seen in phase 3 of rehab?
Soft tissue and or joint contractures and adhesions that limit normal ROM or accessory mobility, decreased muscle performance, decreased usage of involved part, loss in participation.
Should there be signs of inflammation in phase 3 of rehab?
No