MSK - Bullous Skin disorders
1/54
Earn XP
Description and Tags
1. Describe the typical clinical presentation, risk factors, pathophysiology, diagnostic features, and treatment of dermatitis herpetiformis. 2. Describe the typical clinical presentation, risk factors, pathophysiology, diagnostic features, and treatment of bullous pemphigoid 3. Describe the typical clinical presentation, risk factors, pathophysiology, diagnostic features, and treatment of pemphigoid vulgaris.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
What Are Bullous Skin Disorders? 3 reasons they are caused
Bullae are fluid-filled blisters >1 cm in diameter, relative to vesicles that are less than 1 cm
infection, mechanical stress, or a malfunctioning immune system
common autoimmune bullous (blistering) disorders
pemphigus vulgaris, bullous pemphigoid, and dermatitis herpetiformis
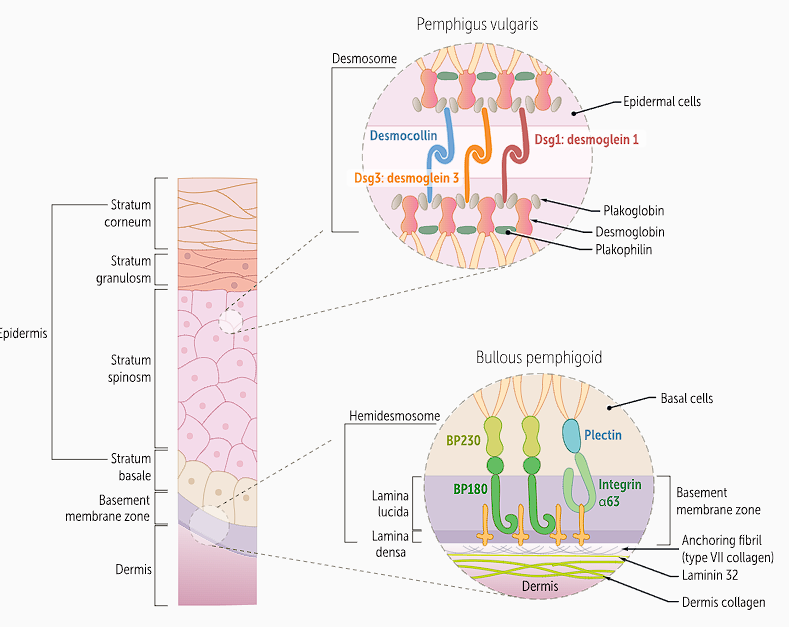
Different involvement in skin and autoantibodies for different proteins
Pemphigus Vulgaris (PV)
autoimmune skin disorder that causes intraepithelial blisters in skin and mucous membranes, effecting mainly people 50-60 y/o and males + females equally
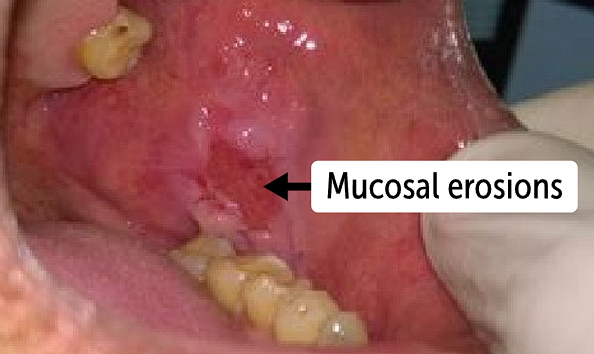
Pemphigus vulgaris affects both
the skin and mucous membranes. Mucosal blisters rupture easily, so patients present with painful and erythematous eroded lesions
PV - Patients can have skin involvement with
flaccid blisters with an erythematous base
When blisters rupture, they cause painful, bleeding lesions
Patients with PV will have a ___________ sign
positive Nikolsky sign, which is a skin finding in which the affected epidermis separates from the underlying dermis with a light touch
Lesions are usually nonpruritic
most common site of involvement for PV
oral cavity, which is where initial disease presents
Other affected mucosal sites are conjunctiva, nose, esophagus, vagina and anus
Disease will progress from mucosal signs to skin, including the scalp, face, neck, axilla, groin and trunk
Risk factors for PV
Genetics - Ashkenazi Jew, Indian, Middle Eastern, White - increased risk
Patients with HLA-DR4 and DR14 are at increased risk
Cause of pemphigus vulgaris
our body’s immune system makes a mistake and attacks cells of the mucous membranes and the skin, specifically the proteins in upper layers of the skin.
UV radiation and thiol drugs like captopril and penicillamine will be associated with PV
How Does Pemphigus Vulgaris Develop?
PV is mediated by immunoglobulin G (IgG) autoantibodies against the protein desmoglein 1 and 3, which is part of a desmosome responsible for adhesion between keratinocytes in the epidermis.
Desmoglein 1 and 3 are cadherin molecules
Mucocutaneous PV has both desmoglein 1 and 3 while mucosal-dominant PV only has antibodies for desmoglein 3
Destruction of desmoglein causes acantholysis which is
separation of keratinocytes from the stratum spinosum layer of the epidermis
The blisters from PV are thinly walled and flaccid, so they end up rupturing easily
Layers of the dermis
Stratus corneum where there’s 10-30 layers of dead keratinocytes
Outermost layer of the epidermis.
Cells: Flattened, dead keratinocytes (corneocytes) filled with keratin, surrounded by lipids.
Stratum lucidum only seen in thick skin,
Thin, transparent layer above the granulosum.
Cells: Densely packed, dead keratinocytes with eleidin (a keratin-rich protein).
Stratum spinosum - Above the basal layer.
Keratinocytes here are linked by strong desmosomes, giving a “spiny” look under the microscope.
Provides mechanical strength, starts keratin production, contains Langerhans cells for immune defense.
Stratum granulosum (granular layer)
Above the spinosum.
Keratinocytes become flattened and packed with keratohyaline granules.
Function of keratohyaline granules:
Contain proteins (profilaggrin, loricrin) that bundle keratin filaments together.
Strengthen and toughen the cells.
Help form the waterproof barrier of skin as cells transition into the outer stratum corneum.
Stratum basale is the deepest epidermal layer, containing basal keratinocytes (stem cells), melanocytes and Merkel cells
Constant cell division → produces new keratinocytes; anchors epidermis to dermis; provides pigmentation and sensation.
Diagnosis is by clinical history and physical examination and confirmed by laboratory investigations
Clinical assessment - take history of skin and mucosal involvement and a positive Nikolsky sign on examination of blisters supports
Testing for Pemphigus V
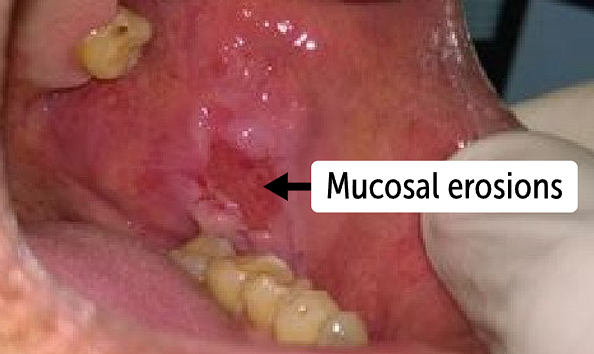
Serology testing for ELISA and IF test - test for IgG abs for desmoglein 1 and 3 and against circulating epithelial antigens
Biopsy to test lesions and lesion around skin — biopsy includes histology and direct IF
Treat pemphigus vulgaris aggressively - what is first line
Systemic steroid therapy w or w/o immunosuppresion is first line
Use immunosuppression as adjunct for steroids to reduce dependency - azathioprine, mycophenolate mofetil immunosuppresants
Azathioprine is cytotoxic and mycophenolate will inhibit immune cell function
If disease is chronic or refractory, try
rituximab or IVIG (IV immunoglobulin)
Rituximab is a monoclonal antibody against to target Cd20 on B cells
Pemphigus vulgaris is a very serious and potentially fatal disease.
most common causes of death are infections and metabolic disturbances.
With proper treatment, mortality drops to 10%. It should be noted that mild disease, however, may resolve spontaneously. The disease is prone to recurrence.
Bullous pemphigoid (BP)
autoimmune skin disorder that causes subepithelial blisters in mucous membranes and skin due to antibodies attacking hemidesmosomal proteins
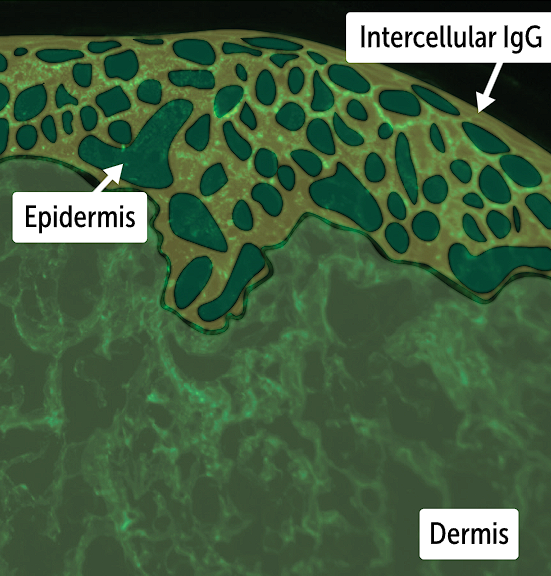
Prodomal phase of BP last weeks to months
presents with urticaria-like lesions, which are erythematous, pruritic, and edematous wheals.
bullae seen on the skin in bullous pemphigoid are severely pruritic 1- to 3-cm blisters on an erythematous base. These bullae are tense and therefore negative for the Nikolsky sign.
Unlike PV that is positive but when eroded blisters rupture, they are similar to PV with moist, erythematous base and crust formation
The clinical presentation that stands out for BP is its
prodromal phase with itchy urticarial lesions that progress to tense blisters
Lesions of BP that can occur anywhere on the skin however they are often seen in
abdomen, groin, and flexors of extremities, oral lesions are less common, more likely in pemphigus vulgaris than bullous pemphigoid with negative Nikolsky sign
Genetics are involved as European people older than 60 have increased risk, also there is
HLA-DQB1 that is associated with BV
What Causes Bullous Pemphigoid? (4 and 2 drugs as examples)
Environmental factors, drugs, infections, dipeptidyl peptidase 4 inhibitors (DPP-4) that treat diabetes like linagliptin and vildagliptin can all cause BP
Environmental factors - BP
mechanism of antigen cross-reactivity are contributors to bullous pemphigoid
Certain infections and drugs can cause BP.
This is a result of cross-reactivity of antibodies against infectious antigens or drugs with antigens in the basement membrane zone
Antibodies attack antigens in basement membrane
Some infections that can cause bullous pemphigus
Infections from hepatitis B, hepatitis C, Helicobacter pylori, Toxoplasma gondii, and cytomegalovirus
How Does Bullous Pemphigoid Develop?
autoantibodies against the hemidesmosomes, which attach keratinocytes to the cells of the epithelial basement membrane
inflammatory damage that impacts connection between stratum basale of epidermis and underlying basement membrane
Blisters are tense because damage is deeper in epidermis, so the skin layer above is thicker and less likely to rupture
Common hemidesmosome proteins targeted in _______ ; BP180 and BP230
Bullous pemphigoid ; which are the BP antigen 180 and BP antigen 230 (BP230)
BP180 is the main transmembrane protein that adheres basal keratinocytes in the stratum basalis layer of the epidermis to the basement membrane;
BP230 is an intracellular protein that links the intermediate filaments to hemidesmosomes.
Bullous pemphigoid diagnosis is by clinical history and physical examination and confirmed with laboratory investigations. - what sign is negative (what does that relate to) and what is spared in this disorder
a history of tense skin bullae associated with pruritus and mucosal sparing in a relatively older patient.
Negative Nikolsky sign
Lab workup for bullous pemphigus - what will you find, what are the methods
Blood sample for ELISA or indirect immunofluorescence
Can biopsy blisters (lesions) and perilesional tissue for histology and direct immunofluorescence
WIll find linear deposition pattern of IgG in basement membrane along with C3 complement deposition, also linear

How Do We Treat Bullous Pemphigoid?
Bullous pemphigoid is far less serious than PV. Therefore, BP treatment is less aggressive. It is important to control the cause of BP (eg, medication like the diabetes liptin medications, infection)
BP180 (hemidesmosome in stratus basal) and 230 (intracellular linker of IF to hemidesmosome)
Meidcations for BP
Topical steroids are the cornerstone of BP treatment and are usually sufficient on their own.
Oral steroids may be used if topical application is not available or not practical.
Tetracycline antibiotics are steroid-sparing drugs that also can be used for treating BP.
In refractory disease, immunosuppressant therapy (eg, azathioprine (purine analog that stops DNA/RNA synthesis and prolif of lymphocytes), mycophenolate mofetil(immunosuppresent by stoping IMP-dehydrogenase for stopping lymphocyte proliferation) or IVIG may be used.
Skin care for BP can prevent infections and reduce pain
Lesions should be cleaned with antiseptic solution.
Open erosions should be covered with dressing.
Puncturing blisters is controversial as it provides comfort to the patient but increases the risk of infection
Dermatitis Herpetiformis (DH)
autoimmune skin disorder that causes blisters due to gluten sensitivity
not like celiac because there aren’t antibodies formed to gluten
Celiac disease
Celiac involved development of antibodies (IgA) against tissue transglutaminase
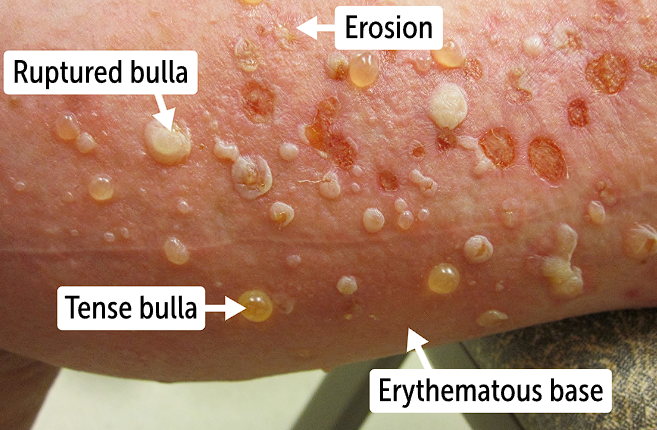
Presentation of dermatitis herpeformis
clusters of severely pruritic papules and vesicles on the skin.
Vesicles are fluid filled like bullae, just smaller
Vesicles will clump together and looks like herpes
in DH, lesions usually are distributed
symmetrically in groups over extensor surfaces such as shoulders, elbows, knees, and buttocks
the lesions are fleshy or erythematous in color
Patients will scratch lesions cause erosions and excoriations of the lesions

oral involvement is rare, when it does occur - in DH
there are erythematous vesicles or erosions
in DH, GI issues can also occur bc of gluten sensitivity
including cramping pain, diarrhea, and constipation
DH lesion type and appearance
DH presents with grouped papules and vesicles that give patients a burning and stinging sensation
Risk factors for DH
DH is associated with certain HLA genes, including HLA-DQ2 or DQ8
Related to the autoimmune response to gliadin proteins (glycoprotein in gluten of wheat)
What HLA subtypes are associated with PV, BP and DH
PV —> HLA-DR4 and HLA-DR14
BP —> HLA-DQB1
DH —> HLA-DQ2 and HLA-DQ8
DH development
Gluten allergy
Gliadin is peptide in gluten that is released in digestive tract when food is broken down
Gliadin will become deaminated by the tissue transglutaminase in intestines, which will cause gliadin to bind to HLA-DQ2 or HLA-Dq8 molecules
HLA, gliadin and T cells, B cells - DH
HLA-DQ8 and HLA-DQ2 will be where deaminated gliadin in intestine will bind, and that will cause recruitment and activation of helper T cells
These T cells will induce inflammation and expose tissue transglutaminase antigens to B cells
B cells start producing IgA abs to tissue transglutaminase and epidermal transglutaminase, which will for complexes
IgA and epidermal transglutaminase
they deposit within the dermal papillae and cause immune damage, leading to inflammation and blistering.
On histology, you will see neutrophilic microabscesses within the dermal papilla.
dermal papilla is in epidermis-dermis junction, extending into epidermis and are finger like projections
What layers of epidermis are impacted in PV, BP and DH
PV —> stratum spinosum
BP —> stratum basal and connective tissue below
DH —> dermal papillae
Diagnosis for DH
Dermatitis herpetiformis diagnosis is confirmed with a biopsy of the perilesional skin
Characteristic lesions and histopathology
excoriated papules, erosions, and crusts — remember that they are itchy so patients scratch for erosion to occur
Histopathology reveals infiltration of neutrophils with incipient formation of papillary microabscesses and dermal-epidermal separation
direct IF of DH will show what type of deposits where
IgA granular deposits at basement membrane
The are specific to tissue transglutamaniase and enzyme transglutaminase due to inflammation that causes release of self antigens
gliadin binds to HLA-DQ2 or DQ8
DH - Tests that can support the diagnosis include histopathology and serology
Biopsy of skin lesion can be done with light microscopy
Histology shows PMN infiltrates, papillary infiltrates, papillary micro abscesses and sub-epidermal blisters
Serology testing will have positive IgA antibodies circulating, which are sensitive of endomysium, tissue and/or epidermal transglutaminase
Treatment for Dermatitis herpetiformis - first line
The first-line treatment for dermatitis herpetiformis is a gluten-free diet (GFD) with or without dapsone therapy
Dapsone is an antibiotic
Can also give topical steroids w/ or w/o oral antihistamines to manage pruritis
DH is a chronic disease with multiple relapses, triggered by
gluten consumption or discontinuation of dapsone
A 35-year-old Indian man presents to the clinic with blisters that are easily eroded with gentle rubbing of the skin. He stated that the lesions started within the oral cavity before involvement of his chest area. This patient most likely has antibodies to a protein with which of the following functions?
Adheres basal keratinocytes in the stratum basalis layer
Cell-to-cell adhesion between keratinocytes in the stratum spinosum
Deaminates and forms covalent bonds with gliadin
The correct answer is cell-to-cell adhesion between keratinocytes in the stratum spinosum (B). This patient has pemphigus vulgaris, which is mediated by IgG autoantibodies against desmoglein 3 (and 1), a protein part of a structure (desmosome) that mediates cell-to-cell adhesion. BP180 is a transmembrane protein that adheres to basal keratinocytes in the stratum basalis layer (A), and antibodies against this protein are the cause of bullous pemphigoid. Tissue transglutaminase deaminates and forms covalent bonds with gliadin (C). BP230 links the intermediate filaments to hemidesmosomes (D).
A 45-year-old man of northern European descent presents to the emergency department complaining of diarrhea that started months ago. He reported his symptoms are associated with wheat ingestion. On careful examination, you noticed grouped small papules and vesicles on his elbows, which he reveals to be severely pruritic. Which of the following tests will most likely be positive in this patient?
Antinuclear antibodies
Anti-Scl 70 antibodies
IgA tissue transglutaminase
Thyroid peroxidase antibodies
The correct answer is IgA tissue transglutaminase (C). Activated B cells produce antibodies against tissue transglutaminase after ingestion of gluten-containing foods such as wheat. It is thought celiac disease and dermatitis herpetiformis share the same pathogenesis. Antinuclear antibodies (A) are positive in patients with systemic lupus erythematosus. Anti-Scl 70 antibodies (B) are positive in patients with scleroderma. Thyroid peroxidase antibodies (D) are positive in patients with Hashimoto disease.
A 60-year-old woman of European descent presents to the clinic with bullae of 1-3 cm that are tense and severely pruritic with an erythematous base. She stated that the lesions started a few weeks ago with hives on the skin that progressed to the lesions described. Which of the following drugs can be a cause of this condition?
Doxycycline
Linagliptin
Lisinopril
Metformin
The correct answer is linagliptin (B). There are data supporting drugs of class dipeptidyl peptidase 4 inhibitors (DPP-4 inhibitors that treat diabetes like linagliptin and vildagliptin) causing drug-induced bullous pemphigoid. Doxycycline (A) is an antibiotic, lisinopril (C) is an antihypertensive drug, and drug. None of these three drugs are associated with bullous pemphigoid.