Mycology Week 1
1/172
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
173 Terms
5 types of microorganisms
helminth, virus, protozoan, bacterium, fungus
nomenclature
Genus species
Symbiotic Relationships
mutualism, commensalism, parasitism
mutualism
both partners benefit, example: intestinal bacteria help synthesize vitamins K and B
commensalism
one partner benefits while the other is unaffected, example: barnacles on whales, flora living on skin
parasitism
one partner benefits at the expense of the other, example: fungi that infect and feed on host organisms, pathogenic infection
anatomical barriers as ecosystem
the skin and mucous membranes are anatomical barriers to infection, but they also give a foundation for microbial ecosystems that support beneficial microbial communities.
normal microbiota (flora)
populations of microbes that are routinely found growing in/on a healthy personand play essential roles in digestion, immunity, and preventing pathogenic infections. They help maintain homeostasis in the host.
resident flora
populations of microbes that permanently inhabit a specific area of the body, contributing to health and immune function. it can change with diet, age, antibiotic use, stress, illness, and environemental factors
transient flora
form short associations and are replaced
sterile body fluids
CSF, pleural fluid, peritonial fluid, synovial fluid, pericardial fluid, blood, bone and marrow, urine in the bladder
protectie role of normal microbiota
covering binding sites for pathogenic attachment, consumption of available nutrients, producing toxic compounds like antibiotics
infection
when a microbe has a parasitic relationship with the host. sometimes the host doesn’t always notice symptoms (asymptomatic/subclinical)
infectious disease
when an infection results in disease
symptoms
felt by the patient, examples: pain and nausea
signs
observable effects through examination, examples: rash, pus, swelling
colonization
when a microbe can successfully establish on a host and grow, but it does not automatically mean there will be disease or infection
primary infection
the initial disease that may occur after infection
secondary infection
can happen as a result of a primary disease, example: secondary bacterial pneumonia can occur after an influenza infection
pathogen
a microbe that can cause disease in an otherwise healthy person
opportunistic pathogen
a microbe that causes disease when the host’s immune system is down, can be a part of the normal flora or a common microbe
true pathogen
microbes that cause disease in healthy people
virulence
describes how capable a pathogen is at causing disease, highly virulent means they have high pathogenicity
transmissible or communicable disease
can be spread from host to host, or indirectly through a vector
infectious dose
the minimum number of organisms required to establish infection
incubation
time between the introduction of a microbe and the onset of symptoms
illness
after incubation, signs and symptoms occur
convalescence
recovery, but the host may still be contagious
acute illness
rapid onset of symptoms that last a short time, immunity is established after, examples: common cold, flu, pneumonia, bronchitis, strep throat, UTIs
chronic illness
symptoms develop slowly and persist, examples: HIV/AIDS, hepatitis C, chronic kidney disease, heart disease, rheumatoid arthritis
latent illness
the infection never goes away and can be reactivated later in life, example: shingles, herpes, HIV, hepatitis B (HBV)
Koch’s Postulate
how to prove that a certain pathogen is the cause of a disease.
the microbe must be present in every case
the microbe must be isolated as pure culture from the diseased host
the same disease must occur when introduced to a susceptible experimental host
the microbe must be recovered from the experimental host
virulence factor
anything that a microbe produces that allows it to cause disease by infection, examples: toxins, enzymes, surface structures
molecular Koch’s Postulate
virulence factor should be found in pathogenic strain
a cloned virulence gene should make a non-pathogenic strain become pathogenic, and disrupting the virulence gene should reduce pathogenicity
virulence genes have to be expressed during disease
antibodies and immune cells against virulence gene should be effect at disrupting disease
mechanisms of pathogenicity
ways that pathogens are able to evade the immune system, examples: attaching to host cells, intracellular survival, invasion, toxin production, immune evasion (capsules or antigenic variation)
fungi
eukaryotic, single-celled or multinucleate organisms, eat through decomposing and absorbing organic material in which they grow
types of fungi
yeast, mold, mushrooms
clinical mycology overview
identification of pathogenic fungi
cultures are held for 4 weeks
macroscopic and microscopic observations are done
macroscopic observations of fungi
growth rate, colony structure, surface and reverse color
microscopic observations of fungi
lactophenol cotton blue staining to observe hyphae, spores, phialides, budding yeast
KOH prep to make fungi more observable
india ink for cryptococcus (can’t penetrate the capsule)
yeast overview
unicellular
budding
white and round colonies
found on fruit or skin
used for alcohol and baking
can cause infections
mold overview
has multicellular filaments (hyphae)
can make sexual or asexual spores
fuzzy colonies with many differing colors
found in dark humid places
cheese production
antibiotic production (penicillium)
can cause allergic reactions and respiratory illness
yeast budding
bud = blastospore
pseudohyphae = long chains of blastospores that are attached
bud scars form
mycelium
the root-like structure of fungi, made up of thin branching filaments called hyphae
mushroom
when conditions are right mycelium can form fruiting bodies which are referred to as the mushroom
vegetative mycelium
non-reproductive part of mycelium that grows underground or in organic matter to absorb nutrients
aerial mycelium
reproductive and asexual spore-forming, it grows above the substrate surface
hypha
a long, branching filamentous cell, many hyphae make the mycelium, it is the basic cellular unit of filamentous fungal structures
classification of hyphae
septate or nonseptate
morphology: nodular, root-like (rhizoid), racquet, pectinate, or spiral
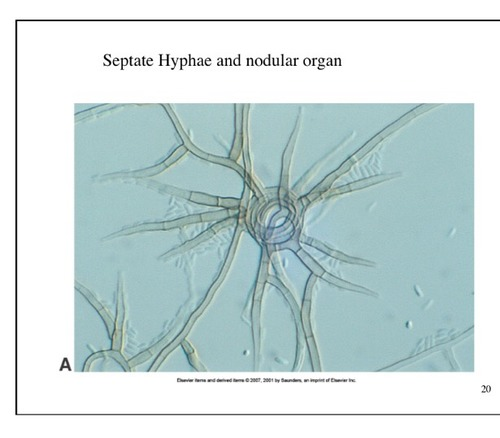
what type of hyphae is this
nodular

what type of hyphae is this
rhizoid

what type of hyphae is this
racquet

what type of hyphae is this
pectinate

what type of hyphae is this
spiral
dimorphic fungi
a type of fungi that can exist as either mold (filamentous form) or yeast, typically depending on temperature, carbon dioxide, or nutrients
thermal dimorphism
pathogenic fungi that change form based on temperature, mold in cold (soil) and yeast in warm (human body), examples: histoplasma, coccidioides, blastomyces
subcellular structures of fungi
capsule (in some)
cell wall
cell membrane
cytoplasm
nucleus
nuclear membrane
nucleolus
ER
mitochondria
vacuoles
capsule
made of polysaccharides and found in some fungi, antiphagocytic, Cryptococcus neoformans (encapsulated yeast), virulence factor that can cause chronic infections
cell wall
antigenic (can trigger immune response), multilayered (90% polysaccharides and 10% proteins and glycoproteins), provides shape and strength (protection from osmotic shock)
major polysaccharides of fungal cell wall
polymer = chitin, monomer = N-acetyl glucosamine
cellular membrane
bilayered, phospholipids and sterols (ergosterol and zymosterol), protects cytoplasm, controls solute concentrations, facilitates capsule and cell wall synthesis
types of spores
sexual, asexual, parasexual (genetic exchange)
types of sexual spores
zygospore
ascospore
basidiospore
oospore
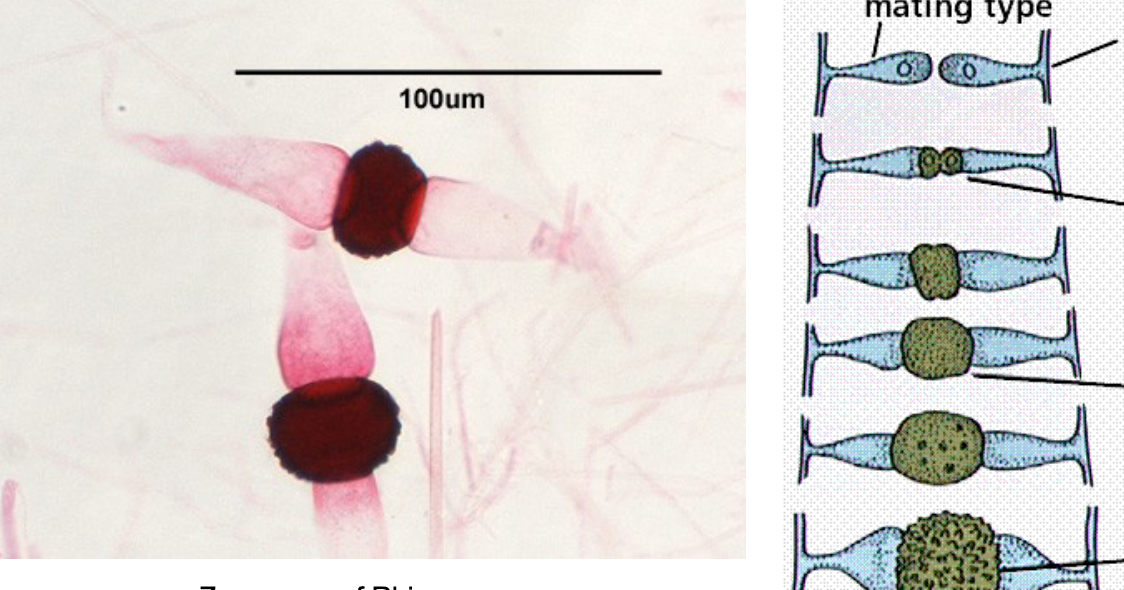
what type of sexual spore is this
zygospore
zygospore
fusion of 2 haploid cells, diploid nucleus, thick-walled, can remain dormant for extended times, mating between + and - hyphae
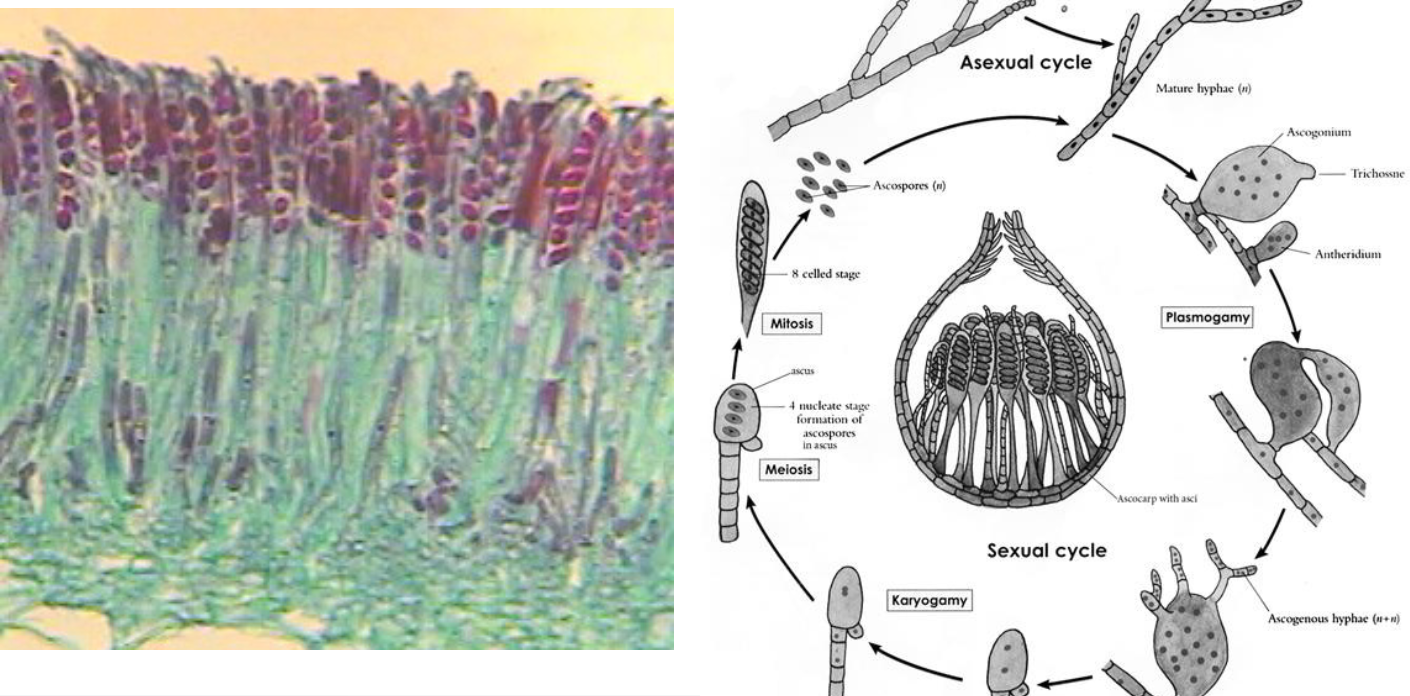
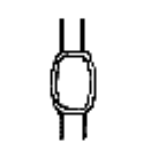
what type of sexual spore is this
ascospore
ascospore
like a bag of spores, formed in an ascus (sac-like cell)

what type of sexual spore is this
basidiospore
basidiospore
spores formed at the ends of club-shaped cells called basidium

what type of sexual spore is this
oospore
oospore
thick-walled, egg-like
asexual spores
sporangiospores
arthrospores
blastospores
chlamydospores
macroconidium
microconidium
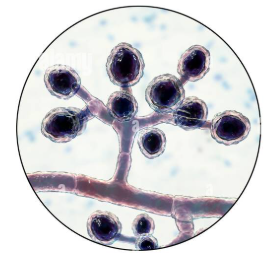
sporangiospores
endogenous, formed within a sporangium, the protoplasm cleaves around the nuclei
conidia
exogenous, mostly at the tip of supporting hyphae called conidiophores
blastic conidia
1st cell enlarges, 2nd septum forms
thallic conidia
1st septum forms, 2nd cell enlarges
what type of asexual spore is this
arthrospore
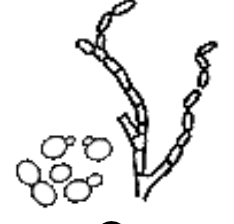
what type of asexual spore is this
blastospore
what type of asexual spore is this
chlamydospore

what type of asexual spore is this
macroconidia
what type of asexual spores is this
microconidia
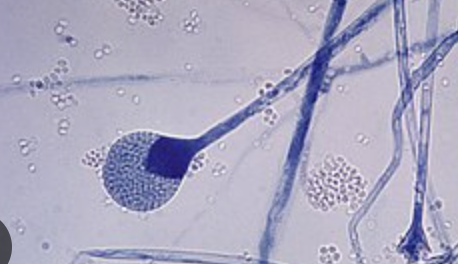
what type of asexual spore is this
sporangiospore
arthrospores
formed by fragmenting specialized hyphal cells, rectangular
blastospores
budding in yeast, like Candida
chlamydospores
thick-walled, single celled, long-surviving, formed when vegetative cells contract
macroconidia
multi-celled, can have irregular shapes
microconidia
single-celled
mycosis
fungal infection
types of mycoses
superficial mycosis
cutaneous mycosis
subcutaneous mycosis
systemic (disseminated) mycosis
others
dermatophytosis (skin, hair, nails)
zygomycosis
yeasts
opportunistic mycosis (contaminants)
pneumocystosis
superficial mycosis
outermost layers of epidermis called the stratum corneum
cutaneous mycosis
in the dermis layer (underneath epidermis)
subcutaneous mycosis
in deeper layers of connective tissue, under the skin, hypodermis layer
systemic (disseminated) mycosis
spread from the respiratory system to multiple organ systems
specimen from humans
sputum (phlegm), vaginal, urine, tissues, blood, exudates, pus, drainage, skin, hair, nails
direct specimen staining/examination
india ink preparations
gram stain procedure/calcofluor white
periodic acid-Schiff, hematoxylin and eosin, calcofluor white
gomori methenamine silver GMS stain
giemsa stain
india ink
distinguishing encapsulated yeast (Cryptococcus neoformans) in CSF, blue
what specimen are gram stain/calcofluor white used for
analyzing materials from mucous membranes, body fluids, urines, pink or purple
calcofluor white stain
observing fluorescent fungal elements in tissue, sputum, body fluids, skin scrapings, and corneal scrapings, example: C. albicans germ tubes
periodic acid-Schiff (PAS) stain
detects polysaccharides and therefore fungal walls, skin scrapings and tissue sections, pink color
gomori methenamine silver GMS
outlines fungi in deep black and the background green, on tissue sections, historically used with Pneumocystis jiroveci